Professional Documents
Culture Documents
Endo Questions
Uploaded by
Arwa0 ratings0% found this document useful (0 votes)
117 views7 pagesendocrinology Questions
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentendocrinology Questions
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
117 views7 pagesEndo Questions
Uploaded by
Arwaendocrinology Questions
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
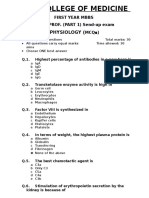
Endocrinology Questions
1. Hypopituitarism in adults leads to all of the
following EXCEPT
a. Failure to produce sex steroids and
gametes
b. Hypogonadism and infertility
c. Loss of secondary sex characteristics
in the male
d. Amenorrhea in the female
e. Inability to regulate glucose
2. Adrenal crisis is precipitated by all the
following EXCEPT
a. Prolonged suppressive
glucocorticoid therapy without
proper coverage in periods of
recovery of the pituitary adrenal
axis
b. Acute illness without recognition of
the lack of cortisol
c. Pituitary apoplexy
d. Growth hormone replacement in a
patient with unrecognized ACTH
deficiency
e. Head injury
3. Which of the following anatomical parts of
the adrenal gland produce aldosterone
a. Zona Fasciculata
b. Zona Reticularis
c. Zona Glomerulosa
d. All of the above
e. None of the above
4. Concerning the adrenal gland negative
feedback loop, identify the true statement
a. Cortisol promotes release but not the
synthesis of ACTH
b. Cortisol stimulates synthesis and
release of the CRH
c. CRH stimulates release of ACTH
d. AVP and CRH stimulate release of
ACTH
e. All of the above are true
5. In primary failure of the adrenal gland, the
etiology can be
a. infiltrative destruction of the gland
itself
b. Pituitary apoplexy
c. Meningococcemia.
d. Cortisol level is low
e. ACTH levels are high
6. Which of the following has NOT been
associated with primary gland failure
a. AIDS
b. Metastatic malignancy
c. Mutation of the ACTH gene
d. Pituitary/hypothalamic radiation
e. None of the above
7. In secondary adrenal gland failure:
a. There is no hyperpigmentation
b. ACTH levels are low
c. CRH levels are low
d. Aldosterone is still produced
e. All of the above are true
8. Secondary adrenal gland failure can be due
to all of the following EXCEPT
a. Pituitary tumors
b. Hypothalamic disease
c. Irradiation of the hypothalamus
d. Head injury
e. Diabetes
9. In tertiary adrenal gland failure
a. ACTH release from the pituitary gland
will be suppressed by exogenous cortisol
a. ACTH release occurs but lacks a
diurnal rhythm
b. CRH levels are high
c. Cortisol levels are high
d. Aldosterone levels are high
10. Clinical signs of adrenal gland failure
are
a. Hypernatremia
b. Hyperglycemia
c. Low calcium
d. Lymphocytosis
e. Constipation
11. Primary adrenal gland deficiency
clinically results in all of the following
EXCEPT
a. Inability to tan
b. Increased libido in the female
c. Abdominal striae
d. Oral mucosa
hyperpigmentation
e. Low blood pressure
12. Meningococcemia can result in
a. Paradoxical regeneration of the
adrenal gland after surgical
removal
b. Waterhouse Frederichson
syndrome
c. Resistance to ACTH stimulation
of the zona glomerulosa
d. Direct sensitization of CRH to
the zona fasciculata
e. Increased cortisol feedback to the
pituitary gland to block cortisol
release.
13. Management of adrenal crisis includes
all of the following EXCEPT
a. IV access
b. Chem 7
c. Measurement of CRH levels
d. ACTH test
e. Measurement of cortisol level
14. Cushing syndrome is caused by all of the
above EXCEPT
a. Excessive levels of cortisol
b. Pituitary adenoma
c. Deficiency in ACTH
d. Increase in CRH
e. All of the above
15. Clinical features of Cushing syndrome
include all of the following EXCEPT
a. Weight loss
b. Violaceous cutaneous striae
c. Thin skin
d. Buffalo hump
e. Moon face
16. Clinical features of Cushing syndrome
include all of the following EXCEPT
a. Thick skin
b. Muscle weakness
c. Hirsutism
d. Clitoris hypertrophy
e. Striae distensae
17. Clinical signs of Cushings disease
include all of the following EXCEPT
a. Moon face
b. Absence of thirst
c. Normal menstrual periods
d. Personality changes
e. Fatigability / Weakness
18. Orthopedic problems in Cushing Disease
include
a. Osteoporosis
b. Vertebral Collapse
c. Both of the above
d. None of the above
19. The definitive test in the diagnosis of
Cushing disease is
a. 1 mg Dexamethasone
suppression test
b. Serum cortisol test
c. 2 mg Dexamethasone
suppression test
d. Measurement of CRH levels
e. None of the above
20. In Cushing disease secondary to an
adrenal tumor
a. ACTH levels are normal
b. ACTH levels are high
c. Cortisol levels are low
d. CRH levels are low
e. None of the above
21. Cushing disease treated with surgical
adrenalectomy secondary to pituitary
tumor has the following characteristics
a. ACTH levels are high
b. Patients require lifelong
replacement of both
glucocorticoids and
mineralocorticoids
c. ACTH levels are low
d. Both of the above
e. None of the above
22. Nelson syndrome features all of the
following EXCEPT
a. Excess of cortisol levels
b. Increased alpha-MSH.
c. Increased CRH levels
d. Increased ACTH levels
e. Tongue is normal
23. Hypoaldosteronism
a. May be independent of cortisol
deficiency
b. Renin levels may be low
c. May occur after heparin
administration
d. May present with postural
hypotension
e. All of the above
24. Concerning hypoaldosteronism
a. Cortisol is the treatment of
choice
b. Conn syndrome may result from
over treatment of
hypoaldosteronism
c. Results from an increase in
angiotensin I conversion to
angiotensin II
d. Is precipitated by pituitary
apoplexy
e. Fludrocortisone 0.10 mg is an
effective medical treatment
25. Which of the following may be a sign of
primary hyperaldosteronism
a. Diastolic hypertension without
edema
b. Hypokalemia
c. Polyuria
d. Metabolic acidosis
e. All of the above
26. Secondary aldosteronism can be due to
a. Renal artery stenosis
b. Malignant hypertension
c. Heparin administration
d. Radiation as the definitive
therapy
e. None of the above
27. Treatment for bilateral adrenal
hyperplasia includes
a. Absence of salt restriction as a
mode of therapy
b. Surgery to correct the underlying
defect
c. Spironolactone
d. None of the above
e. All of the above
28. Pheochromocytoma
a. Results in the feeling of
impending doom
b. Presents with painful extremities
c. Causes frequent diarrhea
d. Is often associated with obesity
e. Presents with hypotension
29. Paroxysmal symptoms of a
pheochromocytoma include
a. Hypotension
b. Ulcers on the pretibial surface of
both legs
c. Respiratory failure
d. Acute exacerbations of pain in
the great toe
e. Sweating
30. Which of the following is associated
with pheochromocytoma
a. Thyroid medullary cancer
b. Astrocytoma
c. Glioblastoma
d. Liver failure
e. Spontaneous fractures of the base
of the 5
th
metatarsal bone
31. Concerning the treatment of a
pheochromocytoma:
a. Surgery is a treatment of choice
b. Radiation therapy is
contraindicated
c. Alpha adrenergic blockers are
often deleterious
d. Beta blockers are contraindicated
e. Salt restriction is imperative
32. Systemic manifestation of MEN II
syndrome which includes a
pheochromocytoma are
a. Lichen amyloidosus
b. Weight gain
c. Bradycardia
d. Decreased urine output
e. Increased appetite
33. The diagnosis of diabetes can be made
with which of the following
a. A fasting blood glucose of 125
b. Random sugar of > 200 with
symptoms of diabetes
c. A 2hr blood glucose of > 180
during an oral GTT
d. Ketones in urine
e.
34. Concerning diabetes
a. Insulin is released from the alpha
cells in the liver
b. Insulin is synthesized in the beta
cells of the pancreas
c. C peptide is made in a ratio of
1: 2 to the insulin molecule
d. Insulin is active immediately
upon release without any further
enzymatic action needed for it to
become metabolically active.
e. Retinal detachment occurs early
in the disease process.
35. In diabetic ketoacidosis, the most
important initial therapy (after the
ABCs) is :
a. Insulin
b. Potassium
c. Fluids
d. Magnesium
e. Bicarbonate
36. Glucose should be administered to a
patient in DKA when the glucose levels
approaches
a. 50
b. 100
c. 150
d. 250
e. 400
37. Insulin should be administered in a
patient with DKA
a. As long as the patient is ketotic
b. Only until the glucose falls
below 200
c. Until the patient is transferred
from the ER to the ICU
d. As long as the patient is
hypokalemic
e. Until the patient is euglycemic
38. Which of the following hormones
opposes insulin action
a. Growth hormone
b. Epinephrine
c. Cortisol
d. Glucagon
e. All of the above
39. Diabetic ketoacidosis is associated with
a. Decreased gluconeogenesis
b. Increased glycogenolysis
c. Ketone formation
d. No change in insulin levels
e. Hyponatremia
40. Symptoms of diabetic ketoacidosis
include all of the following EXCEPT
a. Polyuria
b. Shortness of breath
c. Well hydrated mucosa
d. Kussmaul respirations
e. Altered mental status
41. Precipitating events of diabetic
ketoacidosis are
a. Hypoglycemia
b. Infection
c. Medical compliance
d. Low HBA1c levels
e. Well controlled diabetes
42. Laboratory findings in diabetic
ketoacidosis include
a. Low glucose levels
b. Absence of ketones in the urine
c. Hypermagnesemia
d. Hyperphosphatemia
e. Acidosis
43. Diabetic ketoacidosis gives a strongly
positive nitroprusside test due to
a. Acetoacetate
b. Beta hydroxybutyric acid
formation
c. Acetone
d. Glucose
e. Insulin
44. The nitroprusside test becomes more
positive as you are (correctly) treating
the patient with DKA. This is because
a. total ketone bodies increase as
effective therapy is initiated
b. Beta hydroxybutyric acid
(negative on nitroprusside test) is
converted to acetoacetate which
(positive on nitroprusside test).
c. Acetone formed as the final
oxidation product is strongly
reactive with nitroprusside
d. A fourth yet unknown ketone
body is produced which give a
positive nitroprusside test
e. Insulin which is given to the
patient in DKA is strongly
reactive with nitroprusside.
45. Bicarbonate is not given routinely to a
patient with DKA because
a. Cerebral edema occurs
commonly
b. The patient will produce their
own bicarbonate as they are
given insulin and fluids
c. There is decreased tissue
oxygenation as the HbO
2
curve
shifts to the left
d. It promotes hyperkalemia
e. It increases CSF pH
46. A patient who develops a nonketotic
hyperglycemic state (coma) will have
a. A low glucose level
b. Severe ketoacidosis
c. Hyposmolality
d. Pre-renal azotemia
e. Arterial pH less than 7.00
47. The most important treatment for NKHC
(non ketotic hyperosmolar state/coma)
is:
a. Fluids
b. Insulin
c. Potassium
d. Magnesium
e. Bicarbonate
48. Which of the following infections in
chronic diabetes results in malignant
external otitis?
a. Escherichia coli
b. Pseudomonas aeruginosa
c. Mycoplasma pneumoniae
d. Hemophiles Influenzae
e. Enterococcus
49. Which of the following is a significant
complication in diabetics
a. Rhinocerebral mucormycosis
b. Clostridium difficile colitis
c. Osteomyelitis
d. Optic neuritis
e. Endophthalmitis
50. In thyroid regulation
a. TRH is synthesized by the pituitary
b. TSH is synthesized by the
hypothalamus
c. Thyroid hormone inhibits release of
TSH but not TRH
d. T4 is less potent than T3
e. TSH stimulates TRH release
51. Comparing T4 vs T3
a. T3 is bound to prealbumin
b. The half life of T3 is longer than T4
c. T3 binds less to the receptor than does T4
d. T4 is more potent than T3
e. T3 is formed by peripheral conversion of
T4 to T3
52. Symptoms of hypothyroidism include
a. Hoarse voice
b. Cold intolerance
c. Constipation
d. Amenorrhea
e. All of the above
53. Signs of hypothyroidism include
a. Puffy face / hands and feet
b. Delayed DTR
c. Carpal tunnel syndrome
d. Alopecia
e .All of the above
54. Treatment of hypothyroidism
a. May unmask adrenal insufficiency
b. Is associated with pseudotumor cerebri in
children
c. May need to be increased in pregnancy
d. Includes daily doses of levothyroxine
e. All of the above
55. Hyperthyroidism symptoms include
a. Irritability
b. Cold intolerance
c. Increased appetite
d. Constipation
e. Bradycardia
56. Hyperthyroidism signs include
a. Weight gain
b. Cold skin
c. Normal menstrual periods
d. Increased perspiration
e. Slow heart rate
57. Physical signs of hyperthyroidism include
which of the following
a. Pretibial myxedema
b. Puffy face
c. Increased nail growth
d. Yellow teeth
e. Hyperpigmentation on the oral
mucosa
58. Precipitating events of thyroid storm
include
a. Infection
b. CVA
c. DKA
d. Emotional stress
e. All of the above
59. Treatment of thyroid storm includes
a. Propylthiouracil
b. Potassium iodide
c. Propranolol
d. Dexamethasone
e. All of the above
60. All of the following are symptoms of
thyroid eye disease
a. Diplopia
b. Proptosis
c. Lid lag /retraction
d. Conjunctival injection / chemosis
e. All of the above are true
Endocrinology Answers
1. e
2. d
3. c
4. c
5. a (c can also be correct)
6. d
7. e
8. e
9. a
10. d
11. a, b, & c
12. b
13. c
14. c
15. a
16. a
17. c
18. c
19. c
20. d
21. a & b
22. a
23. e
24. e
25. a, b, & c
26. a
27. b
28. a
29. e
30. a
31. a
32. a
33. b
34. b
35. c
36. d
37. a
38. e
39. c
40. c
41. b
42. e
43. a
44. b
45. c
46. d
47. a
48. b
49. a
50. d
51. e
52. e
53. e
54. e
55. a & c
56. d
57. a
58. e
59. e
60. e
You might also like
- Selected Topics in the History of Biochemistry. Personal Recollections. Part IIIFrom EverandSelected Topics in the History of Biochemistry. Personal Recollections. Part IIIRating: 1 out of 5 stars1/5 (1)
- 015 Physiology MCQ ACEM Primary EndocrineDocument11 pages015 Physiology MCQ ACEM Primary Endocrinesandesh100% (1)
- Handbook of Endocrine Research TechniquesFrom EverandHandbook of Endocrine Research TechniquesFlora de PabloNo ratings yet
- Endicrine MCQ-QuestionsDocument4 pagesEndicrine MCQ-QuestionsThe White Army100% (1)
- Endocrinology 2015-2016 CM 377Document45 pagesEndocrinology 2015-2016 CM 377Daniel ArseniNo ratings yet
- Noor Endocrinologybase. FINALDocument62 pagesNoor Endocrinologybase. FINALschool adressNo ratings yet
- بايو بيبر 1 د.جميلة السمهريDocument8 pagesبايو بيبر 1 د.جميلة السمهريOzgan SüleymanNo ratings yet
- MCQ On VitaminsDocument5 pagesMCQ On VitaminsNikhil raj Yadav100% (1)
- 15 Lecture 3 Endo 2 Tutorial PDFDocument2 pages15 Lecture 3 Endo 2 Tutorial PDFFafa MusNo ratings yet
- Book Back MCQDocument51 pagesBook Back MCQClinton ThomasNo ratings yet
- Endocrinology Best RDocument27 pagesEndocrinology Best RfrabziNo ratings yet
- Diabetes MellitusquestionsDocument3 pagesDiabetes Mellitusquestionscubicj100% (1)
- Endo Main Base LvivtechDocument103 pagesEndo Main Base LvivtechGiridhar SolasaNo ratings yet
- MCI Screening Test 2005Document46 pagesMCI Screening Test 2005Iboyaima SinghNo ratings yet
- Endocrine SystemDocument51 pagesEndocrine SystemMahenor Emad100% (1)
- MCQ ChoDocument31 pagesMCQ Choامجد حسين جواد كاظمNo ratings yet
- MCQS CNS PathologyDocument14 pagesMCQS CNS PathologyFourth YearNo ratings yet
- MCQ On EndocrinologyDocument19 pagesMCQ On Endocrinologyolayemi mariam0% (1)
- Nelson MCQ Fluid TherapyDocument10 pagesNelson MCQ Fluid TherapyBelinderjit Kaur100% (2)
- Physiology MOCK MCQ Exam September 2012Document33 pagesPhysiology MOCK MCQ Exam September 2012mee youNo ratings yet
- DM Questions For IM ResDocument2 pagesDM Questions For IM ResAj BrarNo ratings yet
- En-Metabolism LipidicDocument25 pagesEn-Metabolism LipidicCristina THCSNo ratings yet
- Pathology BDocument5 pagesPathology Bttdjhg2p6kNo ratings yet
- Urinary Tract ReviewDocument12 pagesUrinary Tract ReviewJessica MooreNo ratings yet
- Kidney Q BankDocument12 pagesKidney Q Bankattia arshadNo ratings yet
- TextDocument14 pagesTextOdigo OfujeNo ratings yet
- LO9&10Document13 pagesLO9&10Nine AranasNo ratings yet
- Coordination System Encircle The Best Answer of The Following QuestionsDocument13 pagesCoordination System Encircle The Best Answer of The Following Questionsnon elfNo ratings yet
- Revision MCQsDocument6 pagesRevision MCQswiamNo ratings yet
- Physiology Final Exams JULY 8, 2020Document17 pagesPhysiology Final Exams JULY 8, 2020Ndor BariboloNo ratings yet
- ch20-22 - Probleme SetDocument8 pagesch20-22 - Probleme SetReese VespertineNo ratings yet
- Questions Examples - Old Curriculum PDFDocument10 pagesQuestions Examples - Old Curriculum PDFaminata6No ratings yet
- First Part Exam - March 2021Document28 pagesFirst Part Exam - March 2021hassan mohamedNo ratings yet
- 00018Document92 pages00018Fernandez-De Ala NicaNo ratings yet
- Class Notes On Questionnaires For Pharmacology in The Gastrointestinal TractDocument12 pagesClass Notes On Questionnaires For Pharmacology in The Gastrointestinal TractMarqxczNo ratings yet
- MCQ Bleeding Disorders 2nd Year2021Document6 pagesMCQ Bleeding Disorders 2nd Year2021sherif mamdoohNo ratings yet
- A. Ground Nut Oil B. Palm Oil C. Margarine D. Soya Bean OilDocument8 pagesA. Ground Nut Oil B. Palm Oil C. Margarine D. Soya Bean Oildrpnnreddy100% (1)
- 3 Metabolism of Proteins & Amino AcidsDocument79 pages3 Metabolism of Proteins & Amino AcidsYashfa YasinNo ratings yet
- Biochemisrty Question Bank-1Document51 pagesBiochemisrty Question Bank-1Abd El-Rahman Salah0% (1)
- Aiims BiochemDocument39 pagesAiims Biochemshalialoo22No ratings yet
- Phys - Mcqs - Endocrine - Gastroenterology 123Document41 pagesPhys - Mcqs - Endocrine - Gastroenterology 123Syeda AlizaNo ratings yet
- Renal Path Q'sDocument20 pagesRenal Path Q'skank_sNo ratings yet
- 4 2 PDFDocument9 pages4 2 PDFMahtab KhalifpourNo ratings yet
- MCQSDocument25 pagesMCQSkays30002403No ratings yet
- 1st Year Sendup MCQsDocument8 pages1st Year Sendup MCQsTARIQNo ratings yet
- Biochemistry MLT EXAMDocument8 pagesBiochemistry MLT EXAMLeonel NkwetiNo ratings yet
- Pharmacology Qs Form BookDocument55 pagesPharmacology Qs Form Bookraamki_99No ratings yet
- Endocrinology BDocument5 pagesEndocrinology BTricia Aquino100% (1)
- Biochem 2Document7 pagesBiochem 2Aleena KarimNo ratings yet
- 4 - Biochemistry MCQs GlycolysisDocument7 pages4 - Biochemistry MCQs Glycolysissherazahmedroy0% (1)
- MCQ - 1 (1) - 1Document5 pagesMCQ - 1 (1) - 1marwaNo ratings yet
- MCQs On CVS Pharmacology by Medical Study CenterDocument47 pagesMCQs On CVS Pharmacology by Medical Study CenterLin YunNo ratings yet
- حالات سكرDocument13 pagesحالات سكرNada AliNo ratings yet
- MCQs Pharmacology - Series III-ADocument13 pagesMCQs Pharmacology - Series III-Asidharta_chatterjee100% (1)
- Kenya Medical Training College: Department of Clinical MedicineDocument12 pagesKenya Medical Training College: Department of Clinical MedicineAlvin Omondi100% (1)
- Biochemistry MCQS - VitaminsDocument3 pagesBiochemistry MCQS - VitaminsRati PotateNo ratings yet
- (D) All TheseDocument4 pages(D) All TheseYahya Daham Zafeer SakhrNo ratings yet
- 2nd MB Resit 2019 Respiration QuestionsDocument5 pages2nd MB Resit 2019 Respiration Questionsada100% (1)
- 017 Pathology MCQ ACEM Primary GITDocument3 pages017 Pathology MCQ ACEM Primary GITRebeenMustafaNo ratings yet
- Metabolism MCQ ADocument0 pagesMetabolism MCQ ASurajit BhattacharjeeNo ratings yet
- Histology of Lower GITDocument27 pagesHistology of Lower GITArwa100% (2)
- Module 17 GITDocument112 pagesModule 17 GITArwaNo ratings yet
- Introduction To Nervous SystemDocument30 pagesIntroduction To Nervous SystemArwaNo ratings yet
- Multiple Choice Questions: Patterns of Chromosome InheritanceDocument10 pagesMultiple Choice Questions: Patterns of Chromosome InheritanceArwaNo ratings yet
- 30 Clinical Cases From EmedicineDocument103 pages30 Clinical Cases From EmedicineBahi Alastal100% (3)
- Notes On EmbryologyDocument30 pagesNotes On EmbryologyArwa100% (9)
- ABC of BurnsDocument37 pagesABC of Burnsiraklisd100% (2)
- Normal Laboratory ValuesDocument2 pagesNormal Laboratory ValuesArwaNo ratings yet
- Abuse and Neglect of Children and The ElderlyDocument27 pagesAbuse and Neglect of Children and The ElderlyArwaNo ratings yet
- Principles of Forensic MedicineDocument206 pagesPrinciples of Forensic MedicineArwa100% (3)
- Cigarette Smoking and Lung CancerDocument24 pagesCigarette Smoking and Lung CancerIndonesia TobaccoNo ratings yet
- JETIR1904787Document3 pagesJETIR1904787RONAL SALAS CONTRERASNo ratings yet
- Carcinoma of Prostate: Dr. Saadat Hashmi Consultant UrologistDocument48 pagesCarcinoma of Prostate: Dr. Saadat Hashmi Consultant UrologistMuhammad ArsalNo ratings yet
- 004 Torillo v. LeogardoDocument2 pages004 Torillo v. LeogardoylessinNo ratings yet
- 250 Watt Solar Panel SpecificationsDocument2 pages250 Watt Solar Panel Specificationsfopoku2k20% (1)
- AASHTO Digital Publications: Instructions Located HereDocument2 pagesAASHTO Digital Publications: Instructions Located HereMinn LwinNo ratings yet
- 4 26 12Document9 pages4 26 12stevenscreekNo ratings yet
- DolphinsDocument1 pageDolphinsDebra OkwuziNo ratings yet
- Intermediate Home/Office Electrical/Electronic Equipment ServicingDocument53 pagesIntermediate Home/Office Electrical/Electronic Equipment ServicingSha Tu BolaNo ratings yet
- Cde-Class II Amalgam Restorations-31!12!14Document36 pagesCde-Class II Amalgam Restorations-31!12!14Archita KureelNo ratings yet
- Eaton 092394 T5B 3 7 E en - GBDocument6 pagesEaton 092394 T5B 3 7 E en - GBJorge AmayaNo ratings yet
- Leviticus 12 Pulpit Commentary Homiletics PDFDocument16 pagesLeviticus 12 Pulpit Commentary Homiletics PDFEmiel AwadNo ratings yet
- Public Places 9 & 10Document2 pagesPublic Places 9 & 10kaka udinNo ratings yet
- Instructions For Assembling Your Owners ManualDocument8 pagesInstructions For Assembling Your Owners ManualJim PowersNo ratings yet
- Review of Documents On Seismic Strengthening of Existing BuildingsDocument12 pagesReview of Documents On Seismic Strengthening of Existing Buildingsm7j7a7No ratings yet
- CSEB Korba THERMAL POWER PLANT Mechanical Training ReportDocument20 pagesCSEB Korba THERMAL POWER PLANT Mechanical Training Reporthaxxo24No ratings yet
- 1198-Article Text-5716-1-10-20221219Document9 pages1198-Article Text-5716-1-10-20221219Hendarko AriNo ratings yet
- Components of FitnessDocument3 pagesComponents of Fitnessapi-3830277100% (1)
- Growing Lavender For OilDocument4 pagesGrowing Lavender For OilAsim Serifovic100% (1)
- Am Jf211 - Jul 04Document4 pagesAm Jf211 - Jul 04ilham_metallurgy6744No ratings yet
- SWT Nedelka Cartagena enDocument2 pagesSWT Nedelka Cartagena enChristian Lazo FerreyraNo ratings yet
- Air Compressor: TopicDocument17 pagesAir Compressor: TopicManuel GuerreroNo ratings yet
- Pin ContentDocument20 pagesPin ContentSwetha100% (2)
- DGMS Final ReportDocument15 pagesDGMS Final ReportMaverickNo ratings yet
- Introduction HmoleDocument32 pagesIntroduction HmoleBrian Montales BaggayanNo ratings yet
- Nutrients: Dietary Fiber, Atherosclerosis, and Cardiovascular DiseaseDocument11 pagesNutrients: Dietary Fiber, Atherosclerosis, and Cardiovascular Diseasemichael palitNo ratings yet
- Recipe For SuccesDocument27 pagesRecipe For Successtefany alvarezNo ratings yet
- Experiment-3: Study of Microstructure and Hardness Profile of Mild Steel Bar During Hot Rolling (Interrupted) 1. AIMDocument5 pagesExperiment-3: Study of Microstructure and Hardness Profile of Mild Steel Bar During Hot Rolling (Interrupted) 1. AIMSudhakar LavuriNo ratings yet
- Hide and DrinkDocument562 pagesHide and DrinkMao Lee100% (1)
- Valerie Tillard Murder: Probable CauseDocument11 pagesValerie Tillard Murder: Probable CauseLeigh EganNo ratings yet
- Primary Health Care: Mr. John Michael M. Pitoy, B.S.N., R.NDocument44 pagesPrimary Health Care: Mr. John Michael M. Pitoy, B.S.N., R.NJohn Michael Manlupig Pitoy100% (9)
- Summary of Mary Claire Haver's The Galveston DietFrom EverandSummary of Mary Claire Haver's The Galveston DietRating: 5 out of 5 stars5/5 (1)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 4.5 out of 5 stars4.5/5 (3)
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingFrom EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingRating: 4 out of 5 stars4/5 (3)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeFrom EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNo ratings yet
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthFrom EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthRating: 4 out of 5 stars4/5 (6)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeFrom EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeRating: 4 out of 5 stars4/5 (3)
- Glucose Revolution: The Life-Changing Power of Balancing Your Blood SugarFrom EverandGlucose Revolution: The Life-Changing Power of Balancing Your Blood SugarRating: 5 out of 5 stars5/5 (351)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouFrom EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNo ratings yet
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyFrom EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyNo ratings yet
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainFrom EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainRating: 3.5 out of 5 stars3.5/5 (38)
- Molecules of Emotion: Why You Feel the Way You FeelFrom EverandMolecules of Emotion: Why You Feel the Way You FeelRating: 4 out of 5 stars4/5 (128)
- Keto Friendly Recipes: Easy Keto For Busy PeopleFrom EverandKeto Friendly Recipes: Easy Keto For Busy PeopleRating: 3.5 out of 5 stars3.5/5 (2)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsFrom EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsRating: 4 out of 5 stars4/5 (49)
- How Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseFrom EverandHow Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseRating: 4.5 out of 5 stars4.5/5 (84)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeFrom EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeRating: 4 out of 5 stars4/5 (3)
- The End of Craving: Recovering the Lost Wisdom of Eating WellFrom EverandThe End of Craving: Recovering the Lost Wisdom of Eating WellRating: 4.5 out of 5 stars4.5/5 (81)
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomFrom EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomRating: 4 out of 5 stars4/5 (1)
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthFrom EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthNo ratings yet
- The Whole Body Reset: Your Weight-Loss Plan for a Flat Belly, Optimum Health & a Body You'll Love at Midlife and BeyondFrom EverandThe Whole Body Reset: Your Weight-Loss Plan for a Flat Belly, Optimum Health & a Body You'll Love at Midlife and BeyondRating: 4.5 out of 5 stars4.5/5 (28)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeFrom EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeRating: 5 out of 5 stars5/5 (1)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisFrom EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisRating: 3 out of 5 stars3/5 (2)
- The Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodFrom EverandThe Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodNo ratings yet
- Ultrametabolism: The Simple Plan for Automatic Weight LossFrom EverandUltrametabolism: The Simple Plan for Automatic Weight LossRating: 4.5 out of 5 stars4.5/5 (28)