Professional Documents
Culture Documents
9592
Uploaded by
irmawatig0 ratings0% found this document useful (0 votes)
42 views9 pagesbyg
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentbyg
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
42 views9 pages9592
Uploaded by
irmawatigbyg
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 9
Original Article
PATTERNS OF DRUG THERAPY AMONG DIABETIC HYPERTENSIVE PATIENTS WITH OTHER
COMPLICATIONS
DR. ZAKIA HUSSAIN
1
, DR. AMTUL SANA
2
, SALAHUDDIN MOHAMMED
*3
, MOHAMMED ABDUL RAZZAQ
Received: 19 Apr 2014 Revised and Accepted: 19 May 2014
ABSTRACT
Objectives: There are many variations in prescribing patterns of Diabetes mellitus with hypertension which requires lifelong treatment as
enormously increased the burden of chronic diseases and needs much care while choosing drugs. In a tertiary care centre, prescribing pattern are
powerful tools to ascertain the role of drugs in society. Hence, there is a need for appropriate, safe, effective and economical study to find out the
patterns of drug therapy among diabetic hypertensive patients with other complications.
Methods: Retrospective, randomized and non-interventional study design was conducted from April 2012 to September 2012 at a 600 bedded
multispecialty tertiary care teaching hospital in south India.The collected data are thoroughly analysed and prescriptions were checked for
appropriateness. For easy sorting all data obtained were entered into Microsoft Excel 2000 and cross-checked for accuracy. The data collected were
analysed to obtain averages, percentages and standard deviations. The data were grouped on the bases of age, gender, fasting blood glucose, blood
pressure, co morbidities, various classes of drugs and analysed for significance.
Results: Patterns of drug therapy among Diabetic hypertensive patients with other complications was observed in 117 subjects, out of which males
are more affected than females in the age group of 50-60 years. The most common drug administered for Diabetes was Metformin whereas for
hypertension, Telmisartan was administered. There was a positive relationship between fasting blood glucose and systolic blood pressure.
Conclusion: Lacuna in the present prescribing pattern is underutilization of diuretics. Further studies from time to time are required in drug
utilization pattern and standard treatment guidelines to be circulated among practicing physicians. Our study was done for a short period of time
and the number of patients studied was low. Hence, similar studies covering large number of patients are needed to confirm our findings.
4
College of Health Sciences, Department of Pharmacy, Mizan Tepi University, Mizan Teferi, Ethiopia, Malla Reddy College of Pharmacy,
Dhulapally, Secunderabad. Deccan School of Pharmacy, Kanchanbagh, Hyderabad
Email: salahuddin_pharma48@yahoo.com
Keywords: Diabetes Mellitus, Hypertension, Drug Utilization, JNC VII, Treatment.
INTRODUCTION
Diabetes mellitus (DM) is group of common metabolic disorders that
share the phenotype of hyperglycaemia which are caused by a
complex interaction of genetics and environmental factors. In the
United States, DM is the leading cause of end-stage renal disease
(ESRD), traumatic lower extremity amputations, and adult
blindness. It also predisposes to cardiovascular diseases. With an
increasing incidence worldwide, DM will be a leading cause of
morbidity and mortality for the foreseeable future. The treatment
goal for DM is to prevent mortality and complications by
normalizing blood glucose level. But blood glucose level might be
increased despite of appropriate therapy in patients leading to
diabetic complications, such as disturbances in fat metabolism,
nerve damage, and eye disease [1-5].
The common causes of diabetic complication are poor control of
diabetes either due to non-adherence, poor attitude towards the
disaease and its complications, unhealthy diet and insufficient
physical activity and due to poor managment by the health care
professionals [6-8] Despite this complications diabetes can
predispose the individual for differentinfections [9-13]. The final
outcome of diabetes is disability, and/or [9-13] indirect (costs of
hospitalizations, loss of vision, lower extremity amputations, kidney
failure, and cardiovascular events)[14,15].
Thus, prevention is cost effective than treatment and managment of
diabetic complications[16,17] Though this is the case in many parts
of the world especialy in developed countries [8,16,18], to our
knowledge comprehensive study is lacking in our country except on
patterns of drug therapy and some on prevalence of
complications[11]. Different studies infact of different
methodological quality [19] have documented the complications of
diabetes in different setups including hospitals and community
[11,20,21] on attitude of patients [7,22-24] and adherence
patterns[25-28]. These all can lead to death though one affects the
other[6,9]. Diabetes and its complications are among common
reasons for inpatient patient admissions acounting for about
4.4%[6] of total admissions leading to to about 3.4%[29] to 32.5%
[9] total deaths.
.
The prevalence of chronic complications varies
from 52.0% to 74.2%[11, 12, 20, 30]. The common chronic
complications were erectile dysfunction 64% [31], visual
disturbance (33.8%[11]), Cardiovascular disorders (30.1%[30])
though hypertension alone was 68%[32], neuropathy (29.5%[11]),
and nephropathy (15.7%[11]).
.
Negative attitude of patients towards diabetes managments such as
dietary modifictaions, excersise, and insulin therapy are common
and ultimately canlead to diabeic complications[33]
Likewise acute complications had
similar trend which ranges 30.5% among which DKA was 71%
followed by hypoglycemia 19.4% but Hyperosmolar Hyper-glycemic
State was insignificant[11]. The common risk factors for occurence
of complications were gender [7], longduration with diabetes[12],
poor and inadequate glycemic control[21], negative attitude towards
diabetes[21,22] poor treatment adherence [25]and poor knowledge
about the disease and its managment[21,22].
.
. About 18% of
patients percieve that balanced diet low in sugar/sweets is
important for diabetes control while 52% thought that only sweets
should be stopped [22]. Negative attitude can be developed due to
various reasonsone of which is lack of education [34]. Thus, better
under-standing of perceptions and attitudes among both patients
and providers is needed to guide initiatives to improve the
management of diabetes[19,27]. Though diabetes is fatal disease, of
our knowlege there are no comprehensive studies conducted in the
study area. Thus, this study is aimed indeterming the prescription
pattern in type-2 diabetes mellitus with coexisting hypertension,
prevelence of diabetes related complications and related risk factors,
International Journal of Pharmacy and Pharmaceutical Sciences
ISSN- 0975-1491 Vol 6, Issue 6, 2014
Innovare
Academic Sciences
Mohammed et al.
Int J Pharm Pharm Sci, Vol 6, Issue 6, 270-277
271
identifying the prescribing errors; and treatment adherence as per
the JNC VII guidelines with its related barriers in the hospital.
MATERIALS AND METHODS
The intended work can be divided into the following steps.
Step 1: To collect randomly the prescriptions of patients diagnosed
with diabetes.
Step 2: To separate the prescriptions prescribing Anti Diabetic
Drugs and the ones without anti diabetic Drugs.
Step 3: To divide the prescriptions into various groups according to
the following: Age and Sex of patient and diseases associated with DM.
Step 4: To statistically analyse the prescriptions on the following
aspects:
Demographic Characters of Patients.
Showing incidence of DM according to sex.
Showing incidence of DM according to different age groups.
Analysis of Prescription in DM with respect to dosage forms.
Analysis of prescription showing incidence with other diseases.
Distribution of drugs in different categories based on ATC
classification.
Patterns of utilization of Major Pharmacological Drug classes.
Step 5: To analyses the frequency of diseases associated with DM
statistically and the drugs according to their pharmacological categories.
Location
The study was conducted in the medical outpatient and inpatient wards
of Malla reddy hospital, jeedimetla, in Andhra Pradesh state. It is a 600
bedded tertiary care teaching hospital located at Hyderabad, the hospital
is a unique and well known for its services to people who came from
various parts of city. The institution excels in diverse specialties like
general medicine, general surgery, obstetrics, genecology, paediatrics,
orthopaedics, neurology, neurosurgery, radiology, cardiology,
cardiothoracic surgery, pulmonology, gastroenterology, nephrology,
ENT, dental surgery an department of physical rehabilitation. The
hospital is well equipped with modern diagnostic facilities like 64 slice
CT scan, 1.5 tesla MRI scan, ultrasound sonography, ECG, tread mill, echo
colour Doppler etc. the hospital also have well equipped twelve hi-tech
operation theatres, medicine intensive care unit, coronary care unit,
catheterization laboratory performing diagnostic cardiac catheterisaion,
ballonvalvuloplasty, coronary stenting and haemodialysis.
Study design
It was a retrospective randomized non interventional study
Study period
Data was collected from April 2012 to September 2012 in between 9
am to 4 pm in the departments of general medicine, general surgery
and ophthalmology.
Inclusion criteria:
All diabetic patients who have registered in the outpatient and
inpatient departments.
Prescriptions of patients with at least one Antidiabetic drug
Exclusion criteria:
Paediatric patients and pregnant women.
Patients who were not willing to disclose their information
Data collection
A data collection format was designed to aid collection of data as
shown in annexure I.
Case notes
Data on sex, age, groups of medicines prescribed, number of
prescriptions and number of medicines occurring per prescription
were obtained.
Data analysis
The collected data were thoroughly analyzed and prescriptions were
checked for appropriateness. For easy sorting, all data obtained
were entered into Microsoft Excel 2000 and cross-checked for
accuracy. The data collected were analyzed to obtain averages,
percentages and standard deviations.
Ethical issues
Permission was sought and obtained from the Malla Reddy hospital
before commencement of study.
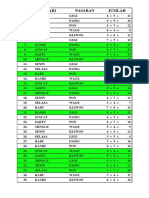
Fig. 1: Age as a factor
RESULTS AND DISCUSSION
Out of 117 diabetic patients, 43.6% were females (51) and 56.4%
were males (66). Males were more sufferers than females. out of all
the patients, 5 patients were in the age group 30-40 years (4.3%),
29 patients were in the age group 40-50 years (24.8%), 47 patients
were in the age group 50-60 years (40.2%), 26 patients were in the
age group of 60-70 years (22.2%) and 10 patients were in the age 70
years and above (8.6%). The more number of patients were in the
age group 50-60 years may be because of sedentary life style and
obesity. These demographic characteristics related to age and
gender were shown in the figure number 1.
Table 1: Comparison of age, weight and mean fasting blood sugar levels among hypertensive and non-hypertensive diabetes mellitus
patients
Characteristics HDM NHDM P Value
Age (Years) 54.3 (10.6) 51.08(12.44) 0.358
Weight(Kg) 61.48 (9.84) 60.29(7.02) 0.17
Mean FPG (mmol/L) 162.2(54.98) 176.75(66.5) 0.316
Age as a Factor
No of
Females
No of
Males
Total
Mohammed et al.
Int J Pharm Pharm Sci, Vol 6, Issue 6, 270-277
272
When compared to hypertensive diabetes mellitus patients with
non-hypertensive diabetes mellitus patients, latter were having
higher mean fasting blood sugar levels (176.75 > 162.2). Mean age of
hypertensive diabetes mellitus was 54.3 years slightly greater than
that of non-hypertensive diabetes mellitus patients (51.08 years).
The mean weight of hypertensive diabetes mellitus patients was
61.48kg and that of non-hypertensive diabetes mellitus patients was
found to be 60.29kg. The data with standard deviations and
significance values were shown in the table no. 1.
Fig. 2: Preferred route of administration of drugs in
prescription
Oral route (88.58%)was most preffered than compared to
parenteral route(11.43%) for diabetic patients . this my be due to
ease of administration, availability of drugs. This data were shown in
figure no. 2. The average number of medications per prescription
was found to be 4.77.
Fig. 3: Analysis of prescription showing with other diseases
While analysing the prescriptions showing incidence with other
diseases it was clear that hypertension was the most prevalent
disease (87.83%), which was associated with diabetes and followed
by eye disorders like retinopathy, cataract (9.57%), kidney diseases
like nephropathy, chronic kidney disease (7.83%), respiratory
diseases like asthma (6.96%), gastro intestinal tract disorders like
cholelithiasis (6.96%), anaemia (3.48%).This was shown in the
figure no.3.
Fig. 4: Relationship between blood pressure and blood sugar
The systolic blood pressures of diabetic hypertensive patients were
categorized into five groups i.e 130-140, 140-150, 150-160, 160-170
and 170 and above. The mean fasting blood sugars of the patients
under each group were calculated and depicted in the figure no.4.
Fig. 5: Analysis of Diabetic hypertensive prescriptions based on
gender
While analysing diabetic hypertensive patients prescriptions it was
found to be patients with age 50-60 years were more in number (40
patients consisting of 39.54% females and 39.66% males), followed
by patients with age 60- 70 years (25 patients consisting of 18.61%
females and 29.32% males).this was shown in the figure no. 5.560
drugs were prescribed for 117 diabetic patients were categorised
into 14 classes as per ATC classification as shown in annexure II.
This was shown in the table no 2. The classes of drugs which were
included in the various categories of ATC classification were
analysed and tabulated. The main pharmacological drug classes
involved with diabetes mellitus prescriptions were found to be A, C
%Age
oral
88.58
89%
%Age
parenteral
11.43
11%
Preferred route of administration
oral parenteral
Analysis of prescription showing with
other diseases
only DM
DM+HTN
Dm+eye
DM+Kidney
DM+Aneamia
DM+Respiratory
DM+GIT
130-140 140-150
150-160160-170
170
F
a
s
t
i
n
g
b
l
o
o
d
g
l
u
c
o
s
e
l
e
v
e
l
i
n
m
g
/
d
l
Systolic blood pressure in mm of Hg
Analysis of Diabetic hypertensive
prescriptions based on gender
%age of
females
%age of
males
Mohammed et al.
Int J Pharm Pharm Sci, Vol 6, Issue 6, 270-277
273
and M. Most frequently were the drugs for GIT and metabolism
(47.86%), followed by drugs for cardio vascular diseases (18.75%)
and drugs for musculo-skeletal system (8.93%). This data were
shown in the table no. 3.
Table 2: Anatomical, Therapeutic and Chemical Classification of Drugs
A Drug for GIT and Metabolism
T.Metformin HCL T.PioglitazoneT.Ondansetron
T.AtorvastatinT.PantaprazoleT.itopride
T.RabeprazoleT.Glimepiride Vitamins
Insulin injT.Glimepiride+metformin
B Drugs for treatment of disorders of blood and blood sugar forming organs
T.AsprinT.EnoxaparineT.Clopidogrel
T.clopidogrel+AspirinInj.Heparin
C Drugs for cardiovascular diseases
T.MetoprololT.AmlodipineInj.furosemide
T.NifedipineT.MetolazoneT.Prazosin
T.CarvedilolT.isosorbidedinitrateT.Clonidine
T.NebivololT.TelmisartanT.Enlapril
T.Perindopril
D Dermatological drugs
G Drugs for urinary system and sex hormones
H Hormones for systemic use except sex hormones
J Anti-infections drug for systemic use
Inj.Ceftriaxone Na Inj.Amikacin Inj. metronidazole
L Antineoplastic and immunomodulating
M Drugs for musculoskeletal system
T.paracetamolT.Paracetamol+tramadolT.Hyoscine butyl Br
T.Ibuprofen+paracetamolT.paracetamol+aceclofenac sodium
T.Calcium citrate T.Dicycloverine HCL
N Drugs for nervous system
T.PregabalinT.AmitryptylineT.Alprazolam
P Drugs for parasitic infections
T.Amoxycillin+Clavulanic acid T.Piperacillin NA +tazobactam
T.LevofloxacinT.CefiximeT.Azithromycin
T.Artesunate+Mefloquine
R Drugs for respiratory system
T.Monteleukast+ LevocetrizineT.Cetrizine HCL
T.FlunerazineT.Doxofylline
T.CyproheptadineHCl+ Tricholinecitrate+sorbital Na
S Drugs for ears and nose
V Various others
Table 3: Analysis of drugs based on ATC Clasification
Drug class(based on ATC Classification) Frequency %
A Drug for GIT and Metabolism 268 47.86
B Drugs for treatment of disorders of blood and blood sugar
forming organs
49 8.75
C Drugs for cardiovascular diseases 105 18.75
D Dermatological drugs - -
G Drugs for urinary system and sex hormones - -
H Hormones for systemic use except sex hormones - -
J Anti-infections drug for systemic use 27 4.83
L Antineoplastic and immunomodulating agents - -
M Drugs for musculoskeletal system 50 8.93
N Drugs for nervous system 10 1.79
P Drugs for parasitic infections 36 6.43
R Drugs for respiratory system 15 2.68
S Drugs for ears and nose - -
V Various others - -
Table 4: Analysis of anti hypertensive drug combinations
Combinations of anti-hypertensive drugs Frequency
ARBS+Betablockers 2
CCBS +Beta blockers 2
ACE + Diuretics 0
ACE+CCBS 2
ACE+Beta blockers 2
CCBS+Diuretics 3
ARBS+Betablockers+ CCBS+Diuretics 3
Mohammed et al.
Int J Pharm Pharm Sci, Vol 6, Issue 6, 270-277
274
By analysing anti hypertensive drugs based on systolic blood
pressure, T. Telmisartan was prescribed to all categories of SBP
more number of times. For the SBP category 150-160mm of Hg
T.Amplodipine was prescribed more number of times next to the
T.telmisartan. T.Nebivolol and T.Enalapril were prescribed only for
two patients. This data were shown in the Figure no. 7.
Fig. 6: Utilisation of antihypertensive drugs in diabetic
hypertensive patients
Out of 100 drugs prescribed for diabetic hypertensive patients most
commonly used category of drugs were angiotensin receptor
blockers (41%), calcium channel blockers (21%) and beta blockers
(13%). Most commonly prescribed drug was telmisartan. Diuretics,
alpha blockers and ACE inhibitors were rarely prescribed. This
data were shown in the figure no. 6.
Fig. 7: Analysis of Anti hypertensive drug patterns based on
systolic blood pressure.
Out of the combinations drugs used for treatment of hypertension,2
patients received angiotensin receptor blocker and beta blockers, 2
patients received calcium channel bolckers and beta blockers, 2
patients received ACE inhibitors and calcium channel blockers, 2
patients received ACE inhibitors and beta blockers, 3 patients
received calcium channel blockers and diuretics, 3 patients received
angiotensin receptor blocker + beta blockers + calcium channel
blockers + diuretics. This data were shown in the table no. 4. By
analysing the anti-hypertensive drugs based on diastolic blood
pressure (DBP), T.Telmisartan was prescribed for more number of
times in the DBP level 100-110 mm of Hg than other drugs.
T. Nebivolol and T. Enalapril were prescribed only in the category
DBP 90-100 mm of Hg. This data were shown in the Figure no. 8.
Fig. 8: Analysis of Anti hypertensive drug patterns based on
diastolic blood pressure.
Fig. 9: Preferred medications in DM (N=111 drugs)
S
y
s
t
o
l
i
c
b
l
o
o
d
p
r
e
s
s
u
r
e
F
r
e
q
u
e
n
c
y
Analysis of Anti hypertensive drug
patterns based on systolic blood pressure.
D
i
a
s
t
o
l
i
c
b
l
o
o
d
p
r
e
s
s
u
r
e
F
r
e
q
u
e
n
c
y
Analysis of Anti hypertensive drug
patterns based on diastolic blood
pressure
Preferred medications in DM
Insulin oral hypoglycemic agents
Mohammed et al.
Int J Pharm Pharm Sci, Vol 6, Issue 6, 270-277
275
Fig. 10: Utilisation of anti-diabetic drugs in diabetic patients
(N=111)
The anti-diabetic drugs prescribed for the patients include T. glimepiride
+ metformin, T. Pioglitazone, T. Metformin, T. Glimepiride, Inj. Insulin.
Out of this most commonly prescribed drug was T. Metformin HCL
(49%). The data were shown in the Fig. 10.
Out of 111 anti-diabetic drugs, 79 were oral anti diabetic agents
(71.18%) and parenteral insulin injection constituted 32(28.83%).
And the data were tabulated and depicted in the figure no.9.By
analysing the Anti diabetic drugs based on Fasting blood glucose
levels, T. Metformin was prescribed for more times in the category
120-130mg/dl than other drugs. T.Pioglitozone was prescribed only
two categories i.e 140-150 and 220-230 mg/dl for only two times.
T.Glimepride and metformin was prescribed to the category 140-150
mg/dl for only two times. This data were shown in the figure no.11.
The drugs used for infections in diabetic hypertensive patients were
inj. Ceftriaxone Na (16%), inj. Metronidazoe (13%), inj. Amikacin
(14%), T. Amoxycilln+ clavulanic acid (17%), T.levofloxacin (10%),
tab. Cefixim (13%), T. Azithromycin (6%), T. Piperacilline Na +
tazobactam (8%), T. Artesunate+ mefloquine (3%). This data were
shown in the figure no. 12.
Fig. 11: Analysis of Anti-diabetic drugs based on fasting blood
sugar level.
Fig. 12: Diabetes mellitus and anti-infective drugs (N=63)
Prescribing Errors
The following Prescribing errors were found in the study Untreated
Hypertension: For 9 subjects who were having their blood pressure
greater than 140/90mm of Hg, there was no anti-hypertensive drug
prescribed.
Contraindicated drug prescribed: Metoprolol was prescribed for 1
subject suffering from Asthma. Illegible handwriting was observed
in the prescription. Wrong route of administration: An Injection
Insulin was prescribed for oral route.
Abbreviations
WT Weight
HT Height
IBW Ideal Body Weight
BP Blood Pressure
Series1
Insulin inj
28.83
29%
Series1
T.Glimepe
ride+metf
ormin
3.61
4%
Series1
T.Pioglita
zone
5.41
5%
Series1
T.Glimepi
ride
12.62
13%
Series1
T.Metfor
min HCL
49.55
49%
Utilisation of antidiabetic drugs
Insulin inj
T.Glimeperide+metformin
F
r
e
q
u
e
n
c
y
Fasting blood sugar in mg/dl
Prescription pattern analysis of
antidiabetic drugs based on fasting
blood sugar
Mohammed et al.
Int J Pharm Pharm Sci, Vol 6, Issue 6, 270-277
276
Chol Cholesterol
Cl Chlorine
Na Sodium
K Potassium
Zn Zinc
DM Diabetes Mellitus
HTN Hypertension
HDM Hypertensive Diabetes Mellitus
NHDM Non Hypertensive Diabetes Mellitus
ATC Anatomical, Therapeutical and Chemiacal Classification
Temp/ T Temperature
GRBS Glucose random blood sugar
FBS Fasting blood sugar
PPBS Post prandial blood sugar
SBP Systolic blood pressure
DBP Diastolic blood pressure
ADA American diabetes association.
DPP Dipeptidyl peptidase.
GLP Glucagon like peptide
FDA Food and Drug Administration
CNS Central Nervous System
RAAS Renin Angiotensin Aldosterone system
NSAIDs Non Steroidal Anti-inflammatory disease.
SNS Sympathetic Nervous System
VSMC Vascular Smooth Muscle Cell
CO Cardiac Output
HR Heart rate
SVR Sustained Virologic Response
CHF Congestive Heart Failure
CV Cardio Vascular
MI Myocardial Infarction
CCF Congestive Cardiac Failure
COPD Chronic obstructive Pulmonary Disease.
GERD Gastro-esophageal reflux disease
SIADH Syndrome of inappropriate secretion of anti-diuretic hormone
Br Asthma Bronchial Asthma
SSS Sick sinus syndrome
SEAR South East Asia region
SLE Systemic lupus erythematous
BPH Benign prostatic hyperplasia.
HDL High density lipid
LDL Low density lipid
BMI Body mass index
JNC Joint National committee
GDM Gestational diabetes mellitus
TZN Thiazolidinedione
TG Triglycerides
BUN Blood urea nitrogen
DM Diabetes Mellitus
ECG Electro cardiogram
CT Computer Tomography
ENT Ear, Nose, Throat
UTI Urinary tract infection
GIT Gastrointestinal tract
LVF Left Ventricular failure
Vit Vitamins
WHO World Health Organization
NCDs Non communicable Diseases
SD Standard Deviation
CCB Calcium channel blocker
ACE Angiotensin Converting Enzyme
I.V Intra Venous
I.M Intra muscular
Inj. Injection
OD once a day
BID Twice a Day
TID Thrice a day
QID Four times a Day
PO Per Oral
HS On bed time
Stat Immediate
HCTZ Hydrochlorothiazide
ARB Angiotensin II receptor blocker
OAs Oral agents.
Mohammed et al.
Int J Pharm Pharm Sci, Vol 6, Issue 6, 270-277
277
CONCLUSION
Hypertension is associated with diabetes largely independent of
gender. 50-60 year age group patient have 40% risk to get diabetes.
Hypertension is part of the metabolic syndrome, with a prevalence as
high as 87.83% in patients who have type 2 diabetes. This study has
shown Metformin as the predominantly prescribed oral
hypoglycaemic drug in both combination and monotherapy. In the
sulfonylureas, Glimepiride is the most predominantly prescribed drug.
Telmisartan is prescribed for hypertension in majority of the patients.
We have found prescribing errors like untreated indication,
prescribing contraindicated drugs and illegible handwriting and
route of administration. The adherence to the JNC VII Guidelines was
good except in case of diuretics. Lacuna in the present prescribing
pattern is underutilization of diuretics. Further studies from time to
time are required in drug utilisation pattern and standard treatment
guidelines to be circulated among practicing physicians. Our study
was done for a short period of time and the number of patients
studied was low. Hence, similar studies covering large number of
patients are needed to confirm our findings.
REFERENCES
1. Longo D, Fauci A, Kasper D, Hauser S, Jameson J, Loscalzo J.
Harrisons: principles of internal medicine2008.
2. Katon W, Lin EH, Simon G, Ludman E, Oliver M. KorffMV,
Potentially modifiable factors associated with disability among
people with diabetes. Psychosom Med 2005;67(2):233-40.
3. Rimm EB, Chan J, Stampfer MJ, Colditz GA, Willett WC.
Prospective study of cigarette smoking, alcohol use, and the
risk of diabetes in men. BMJ (Clinical research ed.)
1995;310(6979):555-9.
4. Wise PH, Edwards FM, Craig RJ, Evans B, Murchland JB,
Sutherland B, et al. Diabetes and associated variables in the
South Australian Aboriginal. Australian and New Zealand
journal of medicine 1976;6(3):191-6.
5. Emanuele NV, Swade TF, Emanuele MA. Consequences of
alcohol use in diabetics. Alcohol health and research world
1998;22(3):211-9.
6. Ajayi EA, Ajayi AO. Pattern and outcome of diabetic admissions
at a federal medical center: a 5-year review. Annals of African
medicine 2009;8(4):271-5.
7. Fitzgerald JT, Anderson RM, Davis WK. Gender differences in
diabetes attitudes and adherence. The Diabetes educator
1995;21(6):523-9.
8. Sharma R, Grover VL, Chaturvedi S, J. Recipe for diabetes
disaster: a study of dietary behaviors among adolescent
students in South Delhi, India. Int Dev Ctries. Alcohol health
and research world 2011;31
9. Chijioke A, Adamu AN, Makusidi AM. Mortality pattern among
type 2 diabetes patients in Ilorin, Nigeria.JEMDSA. Alcohol
health and research world 2010;15(2 SRC - GoogleScholar):1-4.
10. Yadav R, Tiwari P, Dhanaraj E. Risk factors and complications
of type 2 diabetes in Asians. CRIPS.2008; 9(2):8-12.
11. Worku D, Hamza L, Woldemichael K. Patterns of diabetic
complications at jimma university specialized hospital,
southwest ethiopia. Ethiopian journal of health sciences
2010;20(1):33-9.
12. Roaeid RB, Kablan AA. Diabetes mortality and causes of death
in Benghazi: a 5-year retrospective analysis of death
certificates. Eastern Mediterranean health journal = La revue
de sante de la Mediterranee orientale = al-Majallah al-sihhiyah
li-sharq al-mutawassit 2010;16(1):65-9.
13. Holewski JJ, Moss KM, Stess RM, Graf PM, Grunfeld C.
Prevalence of foot pathology and lower extremity
complications in a diabetic outpatient clinic. Journal of
rehabilitation research and development 1989;26(3):35-44.
14. Triplitt CL, Reasner CA, Isley WL, Dipiro JT, Talbert RL, Yee GC.
Pharmacotherapy: A pathophysiologic approach, 7th
edition2008. 1285-320
15. Rayappa PH, Raju KNM, Kapur A, Bjork S, Sylvest C, Kumar
KMD. Economic cost of diabetes care the Bangalore urban
district diabetes study. Int J Diab Dev Countries 1999;19
16. Herman WH, Urbanski P, Wolf AM. Cost effectiveness issues of
diabetes prevention and treatment [Internet]. Newsflash.
[citedMar14].Availablefrom: http://www.dce.org/links/spring
_Newsflash_cost.htm2014.
17. Williamson DF, Vinicor F, Bowman BA, Centers For Disease C,
Prevention Primary Prevention Working G. Primary prevention
of type 2 diabetes mellitus by lifestyle intervention:
implications for health policy. Annals of internal medicine
2004;140(11):951-7.
18. Skovlund SE, Peyrot M, A. The Diabetes Attitudes, Wishes, and
Needs (DAWN) Program. Approach to Improving Outcomes of
Diabetes Care. Diabetes Spectrum 2005;18
19. Vermeire E, Royen PV, Coenen S, Wens J, Denekens J. The
adherence of type 2 diabetes patients to their therapeutic
regimens: a qualitative study from the patients perspective.
Practical Diabetes Int 2003;20.
20. Khazai MH, Khazai B, Zargaran Z, Moosavi Z, Khadivi Z, Arya. F.
Diabetic complications and risk factors in recently diagnosed
type ii diabetes: a case-control study. Alcohol health and
research world 2006;2.
21. Khattab M, Khader YS, Al-Khawaldeh A, Ajlouni K. Factors
associated with poor glycemic control among patients with
type 2 diabetes. Journal of diabetes and its complications
2010;24(2):84-9.
22. Gul N. Knowledge, attitudes and practices of type 2 diabetic
patients. Journal of Ayub Medical College, Abbottabad : JAMC
2010;22(3):128-31.
23. Eldarrat AH. Diabetic patients: their knowledge and perception
of oral health. The Libyan journal of medicine 2011;6.
24. Anderson RM, Donnelly MB, Dedrick RF. Measuring the
attitudes of patients towards diabetes and its treatment.
Patient education and counseling 1990;16(3):231-45.
25. Clark EV. How language acquisition builds on cognitive
development. Trends in cognitive sciences 2004;8(10):472-8.
26. Hermanns N, Mahr M, Kulzer B, Skovlund SE, Haak T. Barriers
towards insulin therapy in type 2 diabetic patients: results of
an observational longitudinal study. Health and quality of life
outcomes 2010;8:113.
27. Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR,
Skovlund SE. Psychosocial problems and barriers to improved
diabetes management: results of the Cross-National Diabetes
Attitudes, Wishes and Needs (DAWN) Study. Diabetic medicine
: a journal of the British Diabetic Association
2005;22(10):1379-85.
28. Lin EHB, Von Korff M, Ciechanowski P, Peterson D, Ludman EJ,
Rutter CM, et al. Treatment adjustment and medication
adherence for complex patients with diabetes, heart disease,
and depression: a randomized controlled trial. Annals of family
medicine 2012;10(1):6-14.
29. Bradshaw PT, Ibrahim JG, Gammon MD. A Bayesian
proportional hazards regression model with non-ignorably
missing time-varying covariates. Statistics in medicine
2010;29(29):3017-29.
30. Liu Z, Fu C, Wang W, Xu B. Prevalence of chronic complications
of type 2 diabetes mellitus in outpatients-a cross-sectional
hospital based survey in urban China [Internet]. Health and
Quality of Life Outcomes, [cited Mar 14]. Available from
[http://www.hqlo.com/content/8/1/62]2014.
31. Peter J, Riley CK, Layne B, Miller K, Walker L. Prevalence and
risk factors associated with erectile dysfunction in diabetic
men attending clinics in Kingston, Jamaica. Journal of
Diabetology. 2 2012;2
32. Raval A, Dhanaraj E, Bhansali A, Grover S, Tiwari P. Prevalence
& determinants of depression in type 2 diabetes patients
in a tertiary care centre. The Indian journal of medical research
2010;132:195-200.
33. Mukhopadhyay P, Paul B, Das D, Sengupta N, Majumder R.
Perceptions and practices of type II diabetes: A cross-sectional
study in tertiary care hospital in Kolkata. Int. J. Diab.
Dev.Countries. 2010;30 (3):143-149.
Mohammed et al.
Int J Pharm Pharm Sci, Vol 6, Issue 6, 270-277
278
34. Ajayi IO, Arije A, Ekore JO, J. EkoreRI, Attitude; diabetic foot
care, education; knowledge; Type 2 diabetes mellitus. Afr
Health Care FamMed 2010;2.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- DEPO IGD 03 - BMHP BDocument1 pageDEPO IGD 03 - BMHP BirmawatigNo ratings yet
- DEPO IGD 03 - BMHP ADocument4 pagesDEPO IGD 03 - BMHP AirmawatigNo ratings yet
- ASPAKalkes Merged PDFDocument55 pagesASPAKalkes Merged PDFirmawatigNo ratings yet
- Antiseptik Saluran Terinfeksi Cresotin Liquid IIDocument2 pagesAntiseptik Saluran Terinfeksi Cresotin Liquid IIirmawatig0% (1)
- BAPAKDocument1 pageBAPAKirmawatigNo ratings yet
- Suratbedaran IaiDocument1 pageSuratbedaran IaiirmawatigNo ratings yet
- B GutDocument2 pagesB GutirmawatigNo ratings yet
- CAN'T FIGHT THIS FEELING (Reo Speedwagon)Document23 pagesCAN'T FIGHT THIS FEELING (Reo Speedwagon)irmawatigNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- HitchjikersGuide v1Document126 pagesHitchjikersGuide v1ArushiNo ratings yet
- Snowflake Core Certification Guide Dec 2022Document204 pagesSnowflake Core Certification Guide Dec 2022LalitNo ratings yet
- God Whose Will Is Health and Wholeness HymnDocument1 pageGod Whose Will Is Health and Wholeness HymnJonathanNo ratings yet
- CASE: Distributor Sales Force Performance ManagementDocument3 pagesCASE: Distributor Sales Force Performance ManagementArjun NandaNo ratings yet
- 2011 06 13-DI-PER8-Acoustic Insulation Catalogue-Rev 01Document12 pages2011 06 13-DI-PER8-Acoustic Insulation Catalogue-Rev 01Tien PhamNo ratings yet
- Komatsu Hydraulic Excavator Pc290lc 290nlc 6k Shop ManualDocument20 pagesKomatsu Hydraulic Excavator Pc290lc 290nlc 6k Shop Manualmallory100% (47)
- Value Chain AnalaysisDocument100 pagesValue Chain AnalaysisDaguale Melaku AyeleNo ratings yet
- Internship Report On A Study of The Masterbranding of Dove: Urmee Rahman SilveeDocument45 pagesInternship Report On A Study of The Masterbranding of Dove: Urmee Rahman SilveeVIRAL DOSHINo ratings yet
- Research On Goat Nutrition and Management in Mediterranean Middle East and Adjacent Arab Countries IDocument20 pagesResearch On Goat Nutrition and Management in Mediterranean Middle East and Adjacent Arab Countries IDebraj DattaNo ratings yet
- Solution Document For Link LoadBalancerDocument10 pagesSolution Document For Link LoadBalanceraralNo ratings yet
- RPS Manajemen Keuangan IIDocument2 pagesRPS Manajemen Keuangan IIaulia endiniNo ratings yet
- Vocabulary Inglés.Document14 pagesVocabulary Inglés.Psicoguía LatacungaNo ratings yet
- Pudlo CWP TDS 2Document4 pagesPudlo CWP TDS 2azharNo ratings yet
- Review of Related LiteratureDocument9 pagesReview of Related LiteratureMarion Joy GanayoNo ratings yet
- Solved SSC CHSL 4 March 2018 Evening Shift Paper With Solutions PDFDocument40 pagesSolved SSC CHSL 4 March 2018 Evening Shift Paper With Solutions PDFSumit VermaNo ratings yet
- 2U6 S4HANA1909 Set-Up EN XXDocument10 pages2U6 S4HANA1909 Set-Up EN XXGerson Antonio MocelimNo ratings yet
- Jesus Hold My Hand EbDocument2 pagesJesus Hold My Hand EbGregg100% (3)
- Living in IT Era OutputDocument6 pagesLiving in IT Era OutputDanica Rose SaludarNo ratings yet
- Case 3 GROUP-6Document3 pagesCase 3 GROUP-6Inieco RacheleNo ratings yet
- Surefire Hellfighter Power Cord QuestionDocument3 pagesSurefire Hellfighter Power Cord QuestionPedro VianaNo ratings yet
- Chapter 14ADocument52 pagesChapter 14Arajan35No ratings yet
- Operations Management Final Exam Solutions CourseraDocument2 pagesOperations Management Final Exam Solutions Courseratheswingineer0% (5)
- NURS FPX 6021 Assessment 1 Concept MapDocument7 pagesNURS FPX 6021 Assessment 1 Concept MapCarolyn HarkerNo ratings yet
- Bio Lab Report GerminationDocument10 pagesBio Lab Report GerminationOli Damaskova100% (4)
- Intimate TemporalitiesDocument12 pagesIntimate TemporalitiesmittentenNo ratings yet
- Adrenal Cortical TumorsDocument8 pagesAdrenal Cortical TumorsSabrina whtNo ratings yet
- Agrarian ReformDocument40 pagesAgrarian ReformYannel Villaber100% (2)
- Quizo Yupanqui StoryDocument8 pagesQuizo Yupanqui StoryrickfrombrooklynNo ratings yet
- Propht William Marrion Branham Vist IndiaDocument68 pagesPropht William Marrion Branham Vist IndiaJoshuva Daniel86% (7)
- WIKADocument10 pagesWIKAPatnubay B TiamsonNo ratings yet