Professional Documents
Culture Documents
TMP B3 DB
Uploaded by
FrontiersOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TMP B3 DB
Uploaded by
FrontiersCopyright:
Available Formats
The devil in the details: public health and depression
Andreas Vilhelmsson
Journal Name: Frontiers in Public Health
ISSN: 2296-2565
Article type: Opinion Article
Received on: 02 Sep 2014
Accepted on: 29 Sep 2014
Provisional PDF published on: 29 Sep 2014
www.frontiersin.org: www.frontiersin.org
Citation: Vilhelmsson A(2014) The devil in the details: public health and
depression. Front. Public Health 2:192.
doi:10.3389/fpubh.2014.00192
Copyright statement: 2014 Vilhelmsson. This is an open-access article distributed
under the terms of the Creative Commons Attribution License (CC
BY). The use, distribution and reproduction in other forums is
permitted, provided the original author(s) or licensor are
credited and that the original publication in this journal is cited,
in accordance with accepted academic practice. No use,
distribution or reproduction is permitted which does not comply
with these terms.
This Provisional PDF corresponds to the article as it appeared upon acceptance, after rigorous
peer-review. Fully formatted PDF and full text (HTML) versions will be made available soon.
Epidemiology
- 1 -
The devil in the details: public health and depression 1
2
Andreas Vilhelmsson
1
* 3
4
1
Department of Clinical Sciences, Division of Social Medicine and Global Health, 5
Faculty of Medicine, Lund University, Sweden 6
7
*Corresponding author 8
9
10
Email addresses: 11
AV: andreas.vilhelmsson@med.lu.se 12
13
14
15
- 2 -
Abstract 1
2
Background: Mental disorders, especially depression, have been increasingly 3
described as a growing burden to global public health. This description is, however, 4
not without controversy, and some scholars are skeptical of how, for instance, 5
depression is viewed as an increasing widespread ill health problem. 6
Discussion: While public health medicine has long engaged in strategies of disease 7
prevention and health promotion, more individualized practices of risk are argued to 8
have become a central dimension of the politics of life in the twenty-first century. By 9
trying to assess potential risk factors for disease and disorders at earlier stages, the 10
concepts of illness and risk may become increasingly blurred. Non-medical problems 11
have become medical ones with risking leading to overdiagnosis and overtreatment as 12
the definition of what constitutes an abnormality gets increasingly broader. If normal 13
events are misdiagnosed as depression, this will risk leaving those who are depressed 14
untreated (extended waiting lists to health care, wrong medications or lack of 15
resources) and thereby create undertreatment and overtreatment simultaneously. 16
Summary: For the sake of public health, arguments for increased diagnosis must 17
therefore be related to a possible danger of medicalizing social problems and life 18
crises. By including people with mild problems in estimates of mental illness, we risk 19
losing support for treating those people who have legitimate disorders. 20
Keywords: Depression; Medicalization; Mental Disorders; Overdiagnosis; 21
Overtreatment; Public Health 22
23
24
- 3 -
Background 1
Mental disorders have been increasingly portrayed by the World Health Organization 2
(WHO) and health researchers as a growing burden to global public health [1-5]. Just 3
the sheer economic impact of mental disorders is significant; it is expected to cost 4
almost a third of the projected US$47 trillion incurred by all non-communicable 5
diseases by 2030 [6]. American and European research indicated in 2005 that 26-27% 6
of the adult population suffers from a diagnosable mental disorder, representing over 7
57 million Americans and almost 83 million Europeans [7-8]. The European research 8
was later revised in 2011 to 38% (approximately 160 million Europeans) by including 9
mental diagnoses usually not analyzed in these kinds of studies, such as insomnia and 10
alcoholism [9]. In Sweden as well as other countries, milder mental symptoms are 11
now being frequently reported as common occurrences [10-11], especially among 12
youth and the elderly [12-13]. These milder symptoms are increasingly becoming 13
highlighted as important; research (for example, Swedish and American) have 14
suggested that early mental ill health can predict more severe mental illness and 15
mental disorders (such as major depression) later in life [14-16] and even premature 16
death [17]. It is, therefore, often argued that early signs of mental ill health need to be 17
acknowledged and treated to prevent the onset of mental disorders [14-16, 18-21]. 18
Depression is the most common of the affective disorders, which are defined as 19
disorders of mood rather than disturbances of thought or cognition [22]. Depression is 20
estimated to have a point prevalence of about 5% in the general population, and a 21
lifetime risk of about 15% [23]. Globally, more than 350 million people of all ages are 22
believed to suffer from depression [24]. Just in the European Union a yearly 23
prevalence of 6.9% of depression is estimated to affect 30.3 million inhabitants [9]. 24
- 4 -
Overall, the WHO now ranks depression as one of the most burdensome diseases in 1
the world, and the organization has for some time projected and warned that 2
depression is predicted to be the highest-ranking disease problem in the developed 3
world by 2020 [1-2]. 4
5
This description is, however, not without controversy, and some scholars are skeptical 6
of how, for instance, depression is viewed as an increasing widespread ill health 7
problem [25-29]. The aim of this article is to discuss some of these issues. 8
9
Discussion 10
The anatomy of public health 11
As Dubos argues in his classic book Mirage of Health, the myths of Hygeia and 12
Asclepius symbolize the never-ending oscillation between two different points of 13
view in medicine: health as the natural order of things and health as something to be 14
restored by correcting an imperfection [30]. The modern followers of Hygeia can be 15
understood as practitioners of public health and the medical professionals as followers 16
of Asclepius [31]. It is sometimes argued that with the exception of the specialties of 17
public health and family medicine, the focus of modern medicine is mainly on the 18
individual patient, rather than relating their situation to their families, communities or 19
the wider society [32]. However, while public health medicine has long engaged in 20
strategies of disease prevention and health promotion, more individualized practices 21
of risk are argued to have become a central dimension of the politics of life in the 22
twenty-first century [33]. Increasingly we have come to regard simply being at risk of 23
future disease as being a disease in its own right [28]. Diagnostic labels now go 24
beyond disease itself to include risk factors for disease, sometimes giving rise to a 25
- 5 -
new source of social identity, namely a pre-disease [34]. This is what critics argue is 1
underway with the introduction of preconditions for major depression in DSM-5 [35]. 2
Focusing on preconditions for disease may further increase what the German 3
sociologist, Ulrich Beck, has called the risk society [36] and in a global approach 4
world risk society [37]; a society structured through individualization where a social 5
crisis appears as an individual crises, no longer perceived in terms of their rootedness 6
in the social realm. Thinking of depression in terms of risk is related to the 7
problematization of depressive illness in the population and as a public health issue 8
[38]. But by trying to assess potential risk factors for disease and disorders at earlier 9
stages, the concepts of illness and risk may become increasingly blurred [39]. 10
11
The ghost in the machine 12
A medical diagnosis is perhaps most readily recognized as the official label that 13
classifies disease as a medically-related problem, and is the foundation from which 14
sense-making and experiences are crafted [34]. A diagnosis can validate a patients 15
perception of her symptoms by giving her experience a name, and equally, it can 16
pathologize routine lived experience, such as fluctuations in ones mood [40]. Medical 17
encounters usually take place within a system where diagnostic handbooks and short 18
form tests are used as a fast way of judging a persons health status, a system that 19
allows and encourages doctors to swiftly choose a diagnosis without a comprehensive 20
investigation of the whole situation surrounding the patient. As argued, for instance 21
by psychiatrist David Healy, guidelines and protocols are now part of an 22
industrialization of health care as he calls it [41]. This is not the purpose for which 23
these handbooks were intended. The DSM was issued as a manual for guiding 24
decisions regarding diagnosis, but has more often been used as a steering document 25
- 6 -
for diagnosis. For instance, it is stated in the DSM-IV that, It is important that DSM- 1
IV not to be applied mechanicallyand are not to be used in a cookbook fashion (p. 2
xxxii) [42]. By using the DSM as a fast track to diagnosis one may end up with a 3
problem with not just overdiagnosis, but also overtreatment. In the medical encounter 4
the doctor may judge it to be more dangerous not to treat someone who may prove to 5
be ill than to treat them when actually there is no need to do so, and as a precaution 6
and in fear of relapse recommend long-term use of medicines [43]. Research has 7
suggested that the act of prescribing in itself might also suggest a biological basis for 8
a problem [44], and that it appears that doctors are less willing to consider nondrug 9
treatments if drug therapy is available, even when there is no evidence that 10
pharmacotherapy is superior [45]. 11
12
Risk of overdiagnosis and overtreatment 13
One pathway to overdiagnosis can be through disease boundaries being widened and 14
treatment thresholds lowered to a point where a medical label and subsequent therapy 15
may cause people more harm than good [28]. This broadening of diagnostic criteria is 16
argued to reflect medicalization as much as discovery of previously undetected sick 17
people [35, 46-49]. Non-medical problems have become medical ones with risking 18
leading to overdiagnosis and overtreatment as the definition of what constitutes an 19
abnormality gets increasingly broader [50]. 20
Concern for the harm and costs of overdiagnosis and overtreatment is now gaining 21
momentum, as the discussion of risk assessment and suggestions of pre-disease 22
progress in the scientific debate [51-52]. Missed, delayed, or incorrect diagnoses can 23
lead to inappropriate patient care, poor patient outcomes and increased costs [53]. In 24
- 7 -
the United States it has been estimated that between $158 billion and $226 billion was 1
wasted on overtreatment in 2011 [54], and that the cost of medicalization in 2005 2
corresponded to almost 4% of the total domestic expenditures on health care that year, 3
or $77 billion [55]. Thus, overdiagnosing depression just in case or because of a 4
risk assessment may take its toll both health-wise and financially. One study found 5
overdiagnosis and overtreatment of depression to be common in community settings 6
in the U.S. [56]. 7
Whether the public benefits from taking more and more medicines for increasingly 8
broadly defined disease is open to serious question. Critics like Marcia Angell argues 9
for instance that one could make a strong argument that Americans with minor 10
ailments suffer more from overmedication, and all the side effects and drug 11
interactions that go with it, than from undermedication [48]. Thus, overdiagnosing 12
depression just in case or because of a risk assessment may take its toll both health- 13
wise and financially. 14
15
The devil in the details 16
Maybe, the devil is in the details. The one in four figure for mental illness 17
prevalence, widely quoted as it is, has an unclear origin [57]. Is it even reasonable that 18
27% of the American and European population is estimated to suffer from mental 19
disorders (or 38% Europeans depending on how many disorders are included)? Or 20
that approximately 8.5% of the Nordic population is prescribed antidepressant 21
medication? [58]. Or does it instead tell us something about the contemporary global 22
community and our view of health and ill health? Pharmaceutical companies have for 23
some time been accused of disease mongering [28, 59], whereby a new condition 24
- 8 -
is promoted as a major public health problem in order to create a market for treatment, 1
often without the publics knowledge, sometimes referred to as the public 2
healthification of social problems [60]. And there is also the issue of alleged 3
financial ties between the members of the DSM panels and the pharmaceutical 4
industry [61-62] but also between industry and doctors responsible for clinical 5
practical guidelines for other medical conditions as well [63]. 6
If normal events are misdiagnosed as depression, this will risk leaving those who are 7
depressed untreated (extended waiting lists to health care, wrong medications or lack 8
of resources) and thereby create undertreatment and overtreatment simultaneously. If 9
depression is going to be viewed as a growing public health problem, there needs to 10
be a distinction between ill health problems that are medical problems and those that 11
are not. 12
13
Summary 14
It is evident that there are conflicting views regarding the officially proclaimed 15
widespread existence of mental disorders, and depression in particular. One the one 16
hand, we face descriptions of a growing public health burden and risk, but on the 17
other hand we have descriptions of overdiagnosis and overtreatment. Certainly, from a 18
public health perspective anyway, a medical approach to mental disorders would be 19
troublesome, since increasing medicalization furthermore risks individualizing mental 20
problems that may have other sources and thereby moves the focus away from the 21
social and political context of ill health, for instance poverty and inequality. For the 22
sake of public health, arguments for increased diagnosis must therefore be related to a 23
possible danger of medicalizing social problems and life crises. By including people 24
- 9 -
with mild problems in estimates of mental illness, we risk losing support for treating 1
those people who have legitimate disorders. 2
3
Competing interests 4
The author declares: that no support was given from any organisation for the 5
submitted work; that there are no financial relationships with any organisations that 6
might have an interest in the submitted work; that no other relationships or activities 7
exist that could have influenced the submitted work. 8
Acknowledgements 9
The author would like to thank Anna Meeuwisse, Lund University, and Tommy 10
Svensson, Linkping University for providing valuable comments on previous 11
versions of the manuscript. AV is a researcher with the Department of Clinical 12
Sciences, Division of Social Medicine and Global Health at Lund University. 13
14
15
References 16
1. World Health Organization (WHO): Mental health: new understanding, new 17
hope. Geneva; 2001. 18
2. World Health Organization (WHO): Promoting mental health: concepts, 19
emerging evidence, practice: a summary report / a report from the World 20
Health Organization, department of mental health and substance abuse in 21
collaboration with the Victorian health promotion foundation (VicHealth). 22
Geneva; 2004. 23
- 10 -
3. World Health Organization (WHO): The global burden of disease: 2004 1
update. Geneva; 2008. 2
4. Cassano P, Fava M: Depression and public health: an overview. J 3
Psychosom Res 2002, 53:849-57. 4
5. Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, 5
Charlson FJ, Norman RE, Flaxman AD, Johns N, Burstein R, Murray CJL, 6
Vos T: Global burden of disease attributable to mental and substance use 7
disorder: findings from the Global Burden of Disease Study 2010. Lancet 8
2013, 382:1575-1586. 9
6. Bloom DE, Cafiero ET, Jan-Llopis, Abrahams-Gessel S, Bloom LR, Fathima 10
S, Feigl AB, Mowafi M, Pandya A, Prettner K, Rosenberg L, Seligman B, 11
Stein AZ, Weinstein C: The global economic burden of noncommunicable 12
diseases. Geneva: World Economic Forum; 2011. 13
7. Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE: Prevalence, 14
severity, and comorbidity of 12-month DSM-IV disorders in the National 15
Comorbidity Survey Replication. Arch Gen Psychiatry 2005, 62:617-627. 16
8. Wittchen H-U, Jacobi F: Size and burden of mental disorders in Europe - a 17
critical review and appraisal of 27 studies. Eur Neuropsychopharmacol 18
2005, 15:357-376. 19
9. Wittchen H-U, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jnsson B, 20
Olesen J, Allgulander C, Alonso J, Faravelli C, Fratiglioni L, Jennum p, Lieb 21
R, Maercker A, van Os J, Preisig M, Salvador-Carulla L, Simon R, 22
Steinhausen HC: The size and burden of mental disorders and other 23
disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 2011, 24
21:655-679. 25
- 11 -
10. Stefansson C-G: Major public health problems - mental ill-health. Scand J 1
Public Health 2006, 34(Suppl 67):87-103. 2
11. Danielsson M, Berlin M: Health in the working-age population. Health in 3
Sweden: The National Public Health Report. Scand J Public Health 2012, 4
40(Suppl 9):72-94. 5
12. Lager A, Berlin M, Heimerson I, Danielsson M: Young people's health. 6
Health in Sweden: The National Public Health Report 2012. Scand J 7
Public Health 2012, 40(Suppl 9):42-71. 8
13. Lennartsson C, Heimerson I: Elderly people's health. Health in Sweden: 9
The National Public Health Report 2012. Scand J Public Health 2012, 10
40(Suppl 9):95-120. 11
14. Breslau N, Roth T, Rosenthal L, Andreski P: Sleep disturbance and 12
psychiatric disorders: a longitudinal epidemiological study of young 13
adults. Biol Psychiat 1996, 39:411-418. 14
15. Chang PP, Ford DE, Mead LA, Cooper-Patrick L, Klag MJ: Insomnia in 15
young men and subsequent depression. Am J Epidemiol 1997, 146:105-114. 16
16. Ringbck Weitoft G, Rosn M. Is perceived nervousness and anxiety a 17
predictor of premature mortality and severe morbidity? A longitudinal 18
follow up of the Swedish survey of living conditions. J Epidemiol 19
Community Health 2005, 59:794-798. 20
17. Gale CR, Batty GD, Osborn DP, Tynelius P, Whitley E, Rasmussen F: 21
Association of mental disorders in early adulthood and later psychiatric 22
hospital admissions and mortality in a cohort study of more than 1 million 23
men. Arch Gen Psychiatry 2012, 69(8):823-831. 24
- 12 -
18. Goodwin R, Olfson M: Treatment of panic attack and risk of major 1
depressive disorder in the community. Am J Psychiatry 2001, 158:1146- 2
1148. 3
19. Koivumaa-Honkanen H, Honkanen R, Viinamki H, Heikkil K, Kaprio J, 4
Koskenvou M: Life satisfaction and suicide: a 20-year follow-up study. Am 5
J Psychiatry 2001, 158:433-439. 6
20. Stein MB, Fuetsch M, Mller N, Hfler M, Lieb R, Wittchen HU: Social 7
anxiety disorder and the risk of depression. Arch Gen Psychiatry 2001, 8
58:251-256. 9
21. Wittchen H-U, Beesdo K, Bittner A, Goodwin RD: Depressive episodes.- 10
evidence for causal role of primary anxiety disorders? European 11
Psychiatry 2003, 18:384-393. 12
22. Rang HP, Dale MM, Ritter JM, Flower RJ: Rang and Dale's pharmacology. 13
Edinburgh: Churchill Livingstone; 2007. 14
23. Lnnqvist J: Major psychiatric disorders in suicide and suicide attempters. 15
In Oxford textbook of suicidology and suicide prevention: a global approach. 16
Edited by Wasserman D, Wasserman C. Oxford: Oxford University Press; 17
2009:275-286. 18
24. Depression. [www.who.int/mediacentre/factsheets/fs369/en/index.html#]. 19
25. Busfield J: Mental illness. Cambridge: Polity Press; 2011 20
26. Healy D: Pharmageddon. Berkeley and Los Angeles: University of California 21
Press; 2012. 22
27. Horwitz AV, Wakefield JC: Loss of sadness: how psychiatry transformed 23
normal sorrow into depressive disorder. Oxford: Oxford University Press; 24
2007. 25
- 13 -
28. Moynihan R, Doust J, Henry D: Preventing overdiagnosis: how to stop 1
harming the healthy. BMJ 2012, 344:e3502. 2
29. Rose N: Disorders without borders? The expanding scope of psychiatric 3
practice. BioSocieties 2006, 1:465-484. 4
30. Dubos R: The mirage of health: utopias, progress, and biological change. 5
New Brunswick: Rutgers University Press; 1959 [1987]. 6
31. Garrett L: Betrayal of trust. The collapse of global public health. New York: 7
Hyperion; 2000. 8
32. Helman C: Culture, health and illness. Oxford: Oxford University press; 2007. 9
33. Rose N: The politics of life itself. Biomedicine, power, and subjectivity in the 10
twenty-first century. Princeton and Oxford: Princeton University Press; 2007. 11
34. Jutel A, Nettleton S: Towards a sociology of diagnosis: reflections and 12
opportunities. Soc Sci Med 2011, 73:793-800. 13
35. Frances A: The first draft of DSM-V. BMJ 2010, 340:492. 14
36. Beck U: Risk society: towards a new modernity. London: Sage Publications; 15
1992. 16
37. Beck U: World risk society. Cambridge: Polity Press; 1999. 17
38. Heln I: The depression paradigm and beyond: the practical ontology of 18
mood disorders. Science Studies 2011, 24(1):81-112. 19
39. Conrad P: The medicalization of society. On the transformation of human 20
conditions into treatable disorders. Baltimore: The Johns Hopkins University 21
Press; 2007. 22
40. Ebeling M: 'Get with the Program!': Pharmaceutical marketing, symptom 23
checklists and self-diagnosis. Soc Sci Med 2011, 73:825-832. 24
- 14 -
41. Healy D: Medical partisans? Why doctors need conflicting interests. Aust 1
NZ J Psychiat 2012, 46(8):704-707. 2
42. American Psychiatric Association, APA: Diagnostic and Statistical Manual of 3
Mental Disorders. Fourth Edition. Text revision. Washington DC: American 4
Psychiatric Association; 2000. 5
43. Busfield J: 'A pill for every ill': Explaining the expansion in medicine use. 6
Soc Sci Med 2010, 70:934-941. 7
44. Cohen CI: The biomedicalization of psychiatry: a critical overview. 8
Community Mental Health Journal 1993, 29(6):509-521. 9
45. Lexchin J: Lifestyle drugs: issues for debate. CMAJ 2001, 164(10):1449- 10
1451. 11
46. Wakefield JC: The concept of mental disorder: diagnostic implications of 12
the harmful dysfunction analysis. World Psychiatry 2007, 6:149-156. 13
47. Wakefield JC, Schmitz MF, First MB, Horwitz AV: Extending the 14
bereavement exclusion for major depression to other losses. Arch Gen 15
Psychiatry 2007, 64:433-440. 16
48. Angell M: The truth about the drug companies: how they deceive us and what 17
to do about it. New York: Random House; 2004. 18
49. Goldacre B: Bad Pharma: how drug companies mislead doctors and harm 19
patients. London: Fourth Estate; 2012. 20
50. Welch G, Schwartz L, Woloshin S: Overdiagnosed: making people sick in the 21
pursuit of health. Boston: Beacon Pres; 2011. 22
51. Godlee F: Preventing overdiagnosis. BMJ 2012, 344:e3783. 23
52. Sheldon T: Reserve antidepressants for cases of severe depression, Dutch 24
doctors are told. BMJ 2012, 344:e4211. 25
- 15 -
53. McDonald KM, Matesic B, Contopoulos-Ioannidis DG et al: Patient safety 1
strategies targeted at diagnostic errors: a systematic review. Ann Intern 2
Med 2013, 158:381-389. 3
54. Berwick DM, Hackbarth AD: Eliminating waste in US health care. JAMA 4
2012, 307(14):1513-1516. 5
55. Conrad P, Mackie T, Mehrotra A: Estimating the costs of medicalization. 6
Soc Sci Med 2010, 70(12):1943-1947. 7
56. Mojtabai R: Clinician-identified depression in community settings: 8
concordance with structured-interview diagnoses. Psychother Psychosom 9
2013, 82:161-169. 10
57. Ginn S, Horder J: "One in four" with a mental health problem: the 11
anatomy of a statistic. BMJ 2012, 344:e1302. 12
58. Vilhelmsson A: Depression and antidepressants: a Nordic perspective. 13
Front Public Health 2013, 1:30. 14
59. Moynihan R, Heath I, Henry D: Selling sickness. The pharmaceutical 15
industry and disease mongering BMJ 2002, 324:886-91. 16
60. Meyer IH, Schwartz S: Social issues as public health: promise and peril. 17
Am J Public Health 2000, 90(8):1189-1191. 18
61. Cosgrove L, Krimsky S, Vijayaraghavan M et al: Financial ties between 19
DSM-IV panel members and the pharmaceutical industry. Psychother 20
Psychosom 2006, 75:154-160. 21
62. Cosgrove L, Krimsky S: A comparison of DSM-IV and DSM-5 panel 22
members' financial associations with industry: a pernicious problem 23
persists. PLoS Med 2012, 9(3):e1001190. 24
- 16 -
63. Neuman J, Korenstein D, Ross JS et al: Prevalence of financial conflicts of 1
interest among panel members producing clinical practical guidelines in 2
Canada and United States: cross sectional study. BMJ 2011, 343:d5621. 3
4
You might also like
- tmpF178 TMPDocument15 pagestmpF178 TMPFrontiersNo ratings yet
- Tmp1a96 TMPDocument80 pagesTmp1a96 TMPFrontiersNo ratings yet
- Tmpa077 TMPDocument15 pagesTmpa077 TMPFrontiersNo ratings yet
- tmp998 TMPDocument9 pagestmp998 TMPFrontiersNo ratings yet
- tmpE3C0 TMPDocument17 pagestmpE3C0 TMPFrontiersNo ratings yet
- tmp27C1 TMPDocument5 pagestmp27C1 TMPFrontiersNo ratings yet
- tmp3656 TMPDocument14 pagestmp3656 TMPFrontiersNo ratings yet
- tmpA7D0 TMPDocument9 pagestmpA7D0 TMPFrontiersNo ratings yet
- tmp96F2 TMPDocument4 pagestmp96F2 TMPFrontiersNo ratings yet
- tmp97C8 TMPDocument9 pagestmp97C8 TMPFrontiersNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- IB Final ShellDocument25 pagesIB Final ShellsnehakopadeNo ratings yet
- The Problem of Units and The Circumstance For POMPDocument33 pagesThe Problem of Units and The Circumstance For POMPamarendra123No ratings yet
- Dryer Regenerative Blower Purge DBP 02250195 405 R00 PDFDocument84 pagesDryer Regenerative Blower Purge DBP 02250195 405 R00 PDFjennyNo ratings yet
- LECTURE NOTES-EAT 359 (Water Resources Engineering) - Lecture 1 - StudentDocument32 pagesLECTURE NOTES-EAT 359 (Water Resources Engineering) - Lecture 1 - StudentmusabNo ratings yet
- ომარ ხაიამი - რობაიები (პარალელური ტექსტები)Document31 pagesომარ ხაიამი - რობაიები (პარალელური ტექსტები)გენო მუმლაძეNo ratings yet
- L04-課文單片填空 (題目) (Day of the Dead)Document3 pagesL04-課文單片填空 (題目) (Day of the Dead)1020239korrnellNo ratings yet
- Dissertation Topics Forensic BiologyDocument7 pagesDissertation Topics Forensic BiologyHelpMeWriteMyPaperPortSaintLucie100% (1)
- Vaccination Schedule in Dogs and CatsDocument3 pagesVaccination Schedule in Dogs and CatsAKASH ANANDNo ratings yet
- Đề ANH chuyên 5Document7 pagesĐề ANH chuyên 5Phạm Ngô Hiền MaiNo ratings yet
- STR Mpa-MpmDocument8 pagesSTR Mpa-MpmBANGGANo ratings yet
- PV2R Series Single PumpDocument14 pagesPV2R Series Single PumpBagus setiawanNo ratings yet
- Unknown Facts About Physicians Email List - AverickMediaDocument13 pagesUnknown Facts About Physicians Email List - AverickMediaJames AndersonNo ratings yet
- Hospital - Data Collection & Literature StudyDocument42 pagesHospital - Data Collection & Literature StudyNagateja MallelaNo ratings yet
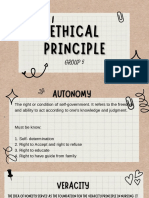
- Group 5 - Ethical PrinciplesDocument11 pagesGroup 5 - Ethical Principlesvirgo paigeNo ratings yet
- Aromatic Electrophilic SubstitutionDocument71 pagesAromatic Electrophilic SubstitutionsridharancNo ratings yet
- Argumentative Essay Research PaperDocument5 pagesArgumentative Essay Research PaperJadNo ratings yet
- Schedule NDocument3 pagesSchedule Nmittal kelaNo ratings yet
- Safety AuditDocument9 pagesSafety AuditRobena Nagum BagasNo ratings yet
- Power Divider and Combiner: EE403-Microwave Engineering MTC, EE Dep., Electromagnetic Waves GroupDocument52 pagesPower Divider and Combiner: EE403-Microwave Engineering MTC, EE Dep., Electromagnetic Waves GroupHabibat El Rahman AshrafNo ratings yet
- Impression TakingDocument12 pagesImpression TakingMaha SelawiNo ratings yet
- BV DSG eDocument18 pagesBV DSG eIulianIonutRaduNo ratings yet
- Tackling Food Inflation: Ashwinkumar Kokku - 67 Malcolm Pinto - 89 Samir Vele - Nitin JadhavDocument9 pagesTackling Food Inflation: Ashwinkumar Kokku - 67 Malcolm Pinto - 89 Samir Vele - Nitin JadhavMalcolm PintoNo ratings yet
- B1 Pendent SprinklerDocument2 pagesB1 Pendent SprinklerDave BrownNo ratings yet
- Mdp36 The EndDocument42 pagesMdp36 The Endnanog36No ratings yet
- MPERSDocument1 pageMPERSKen ChiaNo ratings yet
- Mobrey CLT PDFDocument18 pagesMobrey CLT PDFAnonymous Oydnu9No ratings yet
- White Vaseline: Safety Data SheetDocument9 pagesWhite Vaseline: Safety Data SheetHilmi FauziNo ratings yet
- Flores V PinedaDocument10 pagesFlores V Pinedacha chaNo ratings yet
- Total Elbow Arthroplasty and RehabilitationDocument5 pagesTotal Elbow Arthroplasty and RehabilitationMarina ENo ratings yet
- Ventura 4 DLX ManualDocument36 pagesVentura 4 DLX ManualRoland ErdőhegyiNo ratings yet