Professional Documents
Culture Documents
OECD
Uploaded by
VimuvimCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
OECD
Uploaded by
VimuvimCopyright:
Available Formats
Prekliniske dokumentasjonsstudier
og forventet kvalitet
Katrine W Rustad
LINK Medical Research
Norsk Biotekforum, 13.februar 2012
Outline
Preclinical safety studies
Regulatory guidelines
Good Laboratory Practice (GLP)
Purpose of GLP
OECD principles of GLP
Why, how and when are preclinical safety studies
performed?
Preclinical
research and
development
Clinical research
and development
Short-term
Long-term
Phase 1
Phase 2
Phase 3
MAA/NDA
review
Post-marketing
surveillance
Phase 4
Animal
testing
Adverse
reaction
reporting
File submission Approval
Initial
synthesis
Guidelines
FDA (US Food and Drug Administration)
EMA (The European Agency for the Evaluation of
Medicinal Products)
OECD (Organization for Economic Co-operation and
Development)
ICH (International Conferences of Harmonisation)
Guidelines
cont.
ICH topics divided into 4 major categories:
S=Safety topics, relating to in vitro and in vivo preclinical
studies
Carcinogenicity Studies
Genotoxicity Studies
Toxicokinetics and Pharmacokinetics
Toxicity Testing
Reproductive Toxicology
Biotechnological Products
Pharmacology Studies
Immunotoxicology Studies
Q=Quality topics, relating to chemical and pharmaceutical Quality
Assurance
E=Efficacy topics, relating to clinical studies in human
Guidelines
cont.
ICH topics divided into 4 major categories:
M= Multidisciplinary Topics i.e. cross-cutting topics
M1: Medical terminology
M2: Electronic standards for transmission of regulatory
information
M3: Timing of Pre-clinical Studies in Relation to Clinical
Trial
o M3(R2):
Guidance on Non-Clinical Safety Studies for the Conduct of
Human Clinical Trials and Marketing Authorization for
Pharmaceuticals
M4: The Common Technical Document (CTD)
M5: Data elements and standard for drug dictionaries
Good Laboratory Practice (GLP)
FDA reported that a number of preclinical laboratory
studies which had been performed to investigate the
toxicity of novel compounds were deficient in a variety
of ways
The problem was sufficiently serious to warrant the
introduction of legislation which should prevent future
deficiencies
The first proposals for GLP were made by FDA in 1976
and finally published as law in 1979
Purpose of GLP:
Quality
generate scientific data that comply with regulatory
authorities requirements with respect to quality
Reliability of safety data
data submitted to regulatory authorities are a true
reflection of the results obtained during the study
Human safety
data can be relied upon when making risk/safety
assessments
GLP is not:
GLP can become confused with the standards of
laboratory safety
wearing appropriate gloves, glasses and clothing to
handle materials safely
GLP is not laboratory work in general!
Good Laboratory Practice (GLP)
Planned
Performed
Monitored
Recorded
Reported
Archived
(ref. OECD GLP Principles)
GLP is a quality system concerned with the organizational process
and the conditions under which nonclinical health and
environmental safety studies are:
OECD Principles of GLP include:
Ensure test facility fulfill GLP requirements:
suitable labs
essential equipment and material available
adequate, competent study personnel
Must have knowledge in those parts of GLP applicable to
their involvement in study
Record raw data promptly and accurately in accordance
with GLP
Responsible for quality of raw data
GLP principles:
Quality assurance program:
Assure QA responsibility performed in accordance with
GLP:
Verify and document study plan performed in
accordance with GLP
Conduct inspections to determine if study conducted in
accordance with GLP
Inspect final report to confirm that methods,
procedures, observation are accurate and completely
described
Reported results accurately and completely reflect raw
data of study
Sign a GLP statement in final study report incl. type and
date of inspections were reported to management and
study director
GLP principles:
Standard operating procedure (SOP):
Appropriate and technically validated SOPs should be
available for, but not limited to the following categories:
Test and reference items
Apparatus, material, reagents and solutions
Computerised systems
Record keeping, reporting, storage and retrieval
Test system
QA procedures
GLP principles:
Facilities for Test and Reference Items:
Should be separate rooms/areas for receipt and storage of
test item and reference items
To prevent contamination or mix-ups
Mixing of the test item with vehicle
Test and Reference Items
Receipt, handling, sampling and storage
Labelling, expiry date, storage conditions, stability
Characterisation:
Identity (batch number), purity, composition,
concentration
GLP principles:
Performance of the study:
Appoint Study Director (SD)
Documented approval of study plan issued by SD
Study Director Responsibilities:
single point of study control
responsible for overall conduct of the study
issue protocol, QA involvement, ensure computerised
systems are validated, documentation of raw data,
final report and archiving
Principle Investigator Responsibilities
Responsible for delegated phase of the GLP study in
multi-site studies
GLP principles:
Test System Facilities:
Suitable rooms/areas available
Biological:
Newly arrived animals should be isolated until health
status evaluated
Maintain record of source, date and conditions at arrival
Should be acclimatised to the environment for an adequate
period before first adminstration of test item
All info needed to properly identify test system should
appear on their housing during the conduct of the study
During use, housing for test systems should be cleaned
and sanitised at appropriate intervals
Bedding for animals should be changed as required by
sound husbandry practice
GLP principles:
Storage/archiving of records and reports:
secure storage and retrieval of study plan, raw data,
final reports, sample of test item and specimens
GLP inspections:
All labs having GLP accreditation will be inspected
GLP inspection include a general review of the quality system
in the lab and an audit of selected GLP studies
Report will be sent to the lab and to the authority
Common findings/deviations:
Report not in accordance with raw data
Unauthorized corrections in raw data
Implementation of protocol deviations without amendment
Procedures not done in accordance with SOP/no SOP
established
Incomplete traceability of sample (receipt, storage, time,
temp)
Archiving routine
Why, How and When are
preclinical toxicology and
pharmacology studies performed?
Why perform toxicology studies?
To be as sure as possible (within reasonable limits)
that the products we develop are not harmful to man
at clinically relevant doses
To fulfill the regulatory requirements for registration of
new products
To identify possible risk parameters that need to be
followed-up in clinical studies
How to perform toxicology studies?
Single dose toxicity (rat and dog)
Repeat dose toxicity (rat and dog)
Local tolerance (rabbit)
Genetic toxicity, in vitro + in vivo (rat)
Reproductive toxicology
Carcinogenicity
All studies are conducted according to GLP
Single dose toxicity studies
Investigate the toxic effect of a single high dose of the
product
Single dose via intended clinical route
Minimum 3 doses + control
2 species: rodent + non-rodent
14 Days observation (clinical signs)
Body weight
Necropsy
Target organ weight
Target organ histology
Repeat dose toxicity studies
The drug may not produce immediate toxic effects
Delayed effects due to accumulation of the drug in
animals
2 species: rodent + non-rodent
Toxicokinetics required to document exposure and aid
to interpretation
Recovery period to investigate reversibility of findings
Repeat dose toxicity studies
cont.
Clinical signs
Food consumption
Water consumption
Ophthalmology
Body weight
Antibody determination
Clinical pathology
-clinical chemistry
-haematology
-urinalysis
Anatomic pathology
-organ weight
-macroscopic
-microscopic
Observations, analysis and measurements:
Irritation & Local tolerance studies
Local tolerance
-Intravenous
-Intraarterial
-Paravenous
-Subcutaneous
-Intramuscular
Irritation
-Skin
-Eye
Ascertain that medicinal products are tolerated at sites
in the body which may come in contact with the product
as a result of its administration in clinical use
Genotoxicity
In vivo and in vitro tests for detection of compounds
that induce genetic damage directly or indirectly
Compounds positive in these tests may have the
potential of inducing cancer and/or heritable effects
A battery of tests is necessary to assess the genotoxic
potential of a compound
Genotoxicity
cont.
The recommended standard test battery:
A test for gene mutation in bacteria (Ames test)
An in vitro test with cytogenetic evaluation of
chromosomal damage with mammalian cells or an
in vitro mouse lymphoma tk assay (MLA test)
An in vivo test for chromosomal damage using
rodent hematopoietic cells (micronucleus test)
Reproductive toxicology
Study for effects on fertility and early embryonic
development to implantation
Study for effects on pre- and postnatal
development, including maternal function
Carcinogenicity
The need for carcinogenicity studies:
- Expected clinical use is continuous > 6 months
The rodent bioassays are amongst the most costly
elements in preclinical testing, in terms of time and
resources
Chronic studies (usually 2 years)
Over 1000 animals used per drug
Pharmacology studies
Pharmacology studies can be divided into three
categories
Primary pharmacodynamic:
studies on the mode of action and/or effects of a
substance in relation to its desired therapeutic
target
Secondary pharmacodynamic:
studies on the mode of action and/or effects of a
substance not related to its desired therapeutic
target
Safety pharmacology studies:
Performed according to GLP
Safety Pharmacology Core Battery
Purpose to investigate the effects of the test substance on vital
organs or systems (acutely critical for life):
Cardiovascular system:
Blood pressure, Heart rate, electrocardiogram (ECG)
Telemetry study (dog)
Respiratory system:
Respiratory rate and other measures of respiratory
function (rat)
Central nervous system:
Motor activity, Behavioral changes, Coordination,
Sensory/motor reflex responses, Body temperature
Modified Irwin screen test (rat)
QT prolongation
Delayed ventricular repolarization
Drug induced cardiac arrhythmia recognized as a major hurdle
in development of new drugs
Most common problem is:
acquired long QT syndrome caused by drugs that block the
myocardial Herg potassium channel
delay cardiac repolarization
increase the risk of torsades de pointes arhythmia
Testing of compounds for interactions with the hERG channel
allows the identification of potential risk of QT prolongation in
humans
hERG assay, in vitro electrophysiology study
whole-cell patch-clamp technique
Safety margins
Need a margin of safety for each drug product
Safety margin:
Multiples of the clinical dose dose to be used in
human studies that have been tested in preclinical
safety studies
No observed effect level (NOEL):
The highest dose tested in an animal species with
no detected effects
FDA recommendation:
the no-observed-adverse-effect level (NOAEL) in
toxicity studies in suitable animal species to be at
least one hundred times (100x) greater than the
maximal mass dose to be used in human studies
Clinical trials
Phase I - Human Pharmacology Studies
- to evaluate PK and tolerance in healthy volunteers
Phase II - Therapeutic Exploratory Studies
-to explore efficacy and safety in patients
Phase III - Therapeutic Confirmatory Studies
- to confirm efficacy and safety in patients
Phase IV Therapeutic use
-to study the safety after drug has been released on the market
When to perform preclinical studies?
Timing of studies in relation to
clinical trials
ICH M3:
timing of preclinical studies in relation to clinical trials
recommended preclinical safety studies needed to
support clinical trials
duration of preclinical safety studies
When to perform preclinical studies?
Timing of studies in relation
to clinical trials
Before Phase I:
Single dose toxicity
Repeat dose toxicity
Local tolerance
Genotoxicity
in vitro mutagenicity & clastogenicity
Safety pharmacology
PK & TK
appropriate information by the time Phase I is
completed
When to perform preclinical studies?
Timing of studies in relation
to clinical trials
Before Phase II:
Repeat dose toxicity (dependent on duration)
Genotoxicity
complete standard battery
Before Phase III:
Repeat dose toxicity (dependent on duration)
Before New Drug Application (NDA):
Carcinogenicity studies (unless cause for concern)
not required for all pharmaceuticals
may be conducted post-approval for
pharmaceuticals treating serious diseases
Summary and conclusion:
Preclinical toxicological studies:
Single dose toxicity (rat and dog)
Repeat dose toxicity (rat and dog)
Local tolerance (rabbit)
Genotoxicity (in vitro and in vivo)
Safety pharmacology core battery:
Combined respiratory and cardiovascular study in
conscious (telemetered) dogs
Irwin screen test (rat)
hERG assay (in vitro)
Summary and conclusion:
Preclinical safety studies have to be performed prior
to clinical trials in order to fulfil regulatory
requirements
All safety studies are conducted according to GLP
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- OECD Guidance Document 39Document71 pagesOECD Guidance Document 39VimuvimNo ratings yet
- Root Traits and Phenotyping Strategies FDocument22 pagesRoot Traits and Phenotyping Strategies FVimuvimNo ratings yet
- Registration in Rest of WorldDocument40 pagesRegistration in Rest of WorldVimuvimNo ratings yet
- Low Cost Tissue CultureDocument102 pagesLow Cost Tissue Culturepossibilistic67% (3)
- Sop ElisaDocument4 pagesSop ElisaVimuvimNo ratings yet
- Health Effects Test Guidelines: OPPTS 870.7800 ImmunotoxicityDocument12 pagesHealth Effects Test Guidelines: OPPTS 870.7800 ImmunotoxicityVimuvimNo ratings yet
- List of Preclinical Services: 07/07/14 Liveon Biolabs Pvt. Ltd. ConfidentialDocument5 pagesList of Preclinical Services: 07/07/14 Liveon Biolabs Pvt. Ltd. ConfidentialVimuvimNo ratings yet
- SSR Marker ListDocument1,660 pagesSSR Marker ListVimuvim100% (1)
- Liveon Biolabs Pvt. Ltd.Document14 pagesLiveon Biolabs Pvt. Ltd.VimuvimNo ratings yet
- Plant BiochemistryDocument116 pagesPlant BiochemistrySerkalem Mindaye100% (2)
- Patterning Chromatin: Form and Function For H2A.Z Variant NucleosomesDocument6 pagesPatterning Chromatin: Form and Function For H2A.Z Variant NucleosomesVimuvimNo ratings yet
- Reactive Oxygen SpeciesDocument29 pagesReactive Oxygen SpeciesVimuvimNo ratings yet
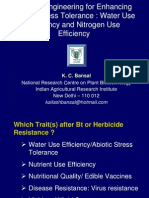
- Dr. K C BansalDocument28 pagesDr. K C BansalVimuvimNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Complications of Insulin TherapyDocument16 pagesComplications of Insulin TherapyIngrid NicolasNo ratings yet
- Multiple Personality Disorder: Is It Fact or Fiction?: Deguzman 1Document10 pagesMultiple Personality Disorder: Is It Fact or Fiction?: Deguzman 1Eliza Philline De GuzmanNo ratings yet
- APA Practice Guideline For The Treatment of Patients With Substance Use DisordersDocument276 pagesAPA Practice Guideline For The Treatment of Patients With Substance Use DisordersRaja Ahmad Rusdan MusyawirNo ratings yet
- PRE Test 1Document15 pagesPRE Test 1Naomi VirtudazoNo ratings yet
- Theraputic Guidelines Version 3 - 2019 PDFDocument163 pagesTheraputic Guidelines Version 3 - 2019 PDFPulkit Kinra83% (6)
- Essential Questions in Paediatrics For MRCPCH v2 PDFDocument208 pagesEssential Questions in Paediatrics For MRCPCH v2 PDFa4aboo100% (11)
- Modifiers-Table 122015 2Document25 pagesModifiers-Table 122015 2khatNo ratings yet
- Energy Drinks Are Bad RealDocument4 pagesEnergy Drinks Are Bad RealMadihi NorhadiNo ratings yet
- 2004 NEJM Photosensitivity NEJ 2004Document7 pages2004 NEJM Photosensitivity NEJ 2004Alma EscobarNo ratings yet
- McWilliams Center For Counseling, Inc. Community Support Office - 438Document2 pagesMcWilliams Center For Counseling, Inc. Community Support Office - 438James BennettNo ratings yet
- Knowledge, Attitude and Practices Towards Breast Feeding Among Lactating Mothers in King George Hospital, A Tertiary Care CenterDocument10 pagesKnowledge, Attitude and Practices Towards Breast Feeding Among Lactating Mothers in King George Hospital, A Tertiary Care CenterIJAR JOURNALNo ratings yet
- Comparative Efficacy and Acceptability META-ANALYSIS 2015Document11 pagesComparative Efficacy and Acceptability META-ANALYSIS 2015Alexandra CastellanosNo ratings yet
- Occupational Health Form: General DetailsDocument2 pagesOccupational Health Form: General DetailsKhushal khanNo ratings yet
- DKA Handout1Document59 pagesDKA Handout1aleNo ratings yet
- Case Study 5 Dengue Fever CorrectedDocument13 pagesCase Study 5 Dengue Fever CorrectedyounggirldavidNo ratings yet
- ANMDocument13 pagesANMhiiihhhhhhhhNo ratings yet
- Treatment Modalities Applicable To The Psychiatric ClientDocument53 pagesTreatment Modalities Applicable To The Psychiatric Clientnickybore100% (1)
- Skull Fracture Vs SuturesDocument6 pagesSkull Fracture Vs Suturesmohit372No ratings yet
- EASL-GL Benign Tumor LiverDocument13 pagesEASL-GL Benign Tumor LiveroliviaNo ratings yet
- OS Pharmacy L III - IVDocument125 pagesOS Pharmacy L III - IVashagrie67% (3)
- Mental Rubrics by Farookh MasterDocument589 pagesMental Rubrics by Farookh MasterPranesh Peter91% (22)
- Anesthesia For The Pet Practitioner (Banfield, 2003 Edition) PDFDocument125 pagesAnesthesia For The Pet Practitioner (Banfield, 2003 Edition) PDFKatarina SimicicNo ratings yet
- TramadolDocument2 pagesTramadolJordanne EtisNo ratings yet
- Medical Biotechnology Multiple Choice Question (GuruKpo)Document13 pagesMedical Biotechnology Multiple Choice Question (GuruKpo)GuruKPO91% (11)
- HIV Drug Chart (2021)Document1 pageHIV Drug Chart (2021)savNo ratings yet
- Case Study On Acute PyelonephritisDocument85 pagesCase Study On Acute Pyelonephritissanutulsi100% (23)
- Insights and Images: Vascular Channel Mimicking A Skull FractureDocument2 pagesInsights and Images: Vascular Channel Mimicking A Skull Fracturethariq mubarakNo ratings yet
- Feeling GreatDocument243 pagesFeeling GreatSunny LamNo ratings yet
- 11 Human Body SystemDocument3 pages11 Human Body SystemCris EnriquezNo ratings yet
- Lesson Plan On Post Natal ExercisesDocument11 pagesLesson Plan On Post Natal Exercisesvarshasharma0593% (15)