Professional Documents
Culture Documents
Drug Study (FINAL)
Uploaded by
iamjenivicOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Study (FINAL)
Uploaded by
iamjenivicCopyright:
Available Formats
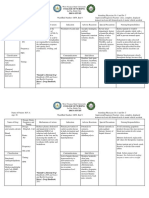
DRUG MECHANISM OF
ACTION
INDICATION CONTRAINDICATIONS ADVERSE EFFECTS
AND SIDE EFFECTS
NURSING
RESPONSIBILITIES
Generic Name
Potassium
Chloride
Brand Name
Kalium Durule
Classification
Electrolyte
Sub
Classification
Dosage
1 tab
Route
oral
Frequency
Every 8 hours
Form
Tablet
Color
White
Principal
intracellular cation
of most body
tissues participates
in a number of
physiologic
processes
maintaining
intracellular
tonicity;
transmission of
nerve impulses,
contraction of
cardiac, skeletal,
and smooth muscle;
maintenance of
normal renal functi
on; also plays a role
in carbohydrate
metabolism and
various enzymatic
reactions.
Prevention
and
correction of
potassium
deficiency;
when
associated
with
alkalosis,
use potassium
chloride;
when
associated
acidosis,
use potassium
acetate bicarb
onate, citrate,
or gluconate.
Contraindicated
with allergy to
tartrazine, aspirin (t
artrazine is found in
some preparations
marketed as Kaon-
Cl, Klor-Con);
therapy with
potassium-sparing
diuretics or
aldosterone-
inhibiting agents;
severerenal impair
ment with oliguria,
anuria, azotemia;
untreated
Addisons disease;
hyperkalemia;
adynamiaepisodica
hereditaria; acute
dehydration; heat
cramps; GI
disorders that delay
passage in the GI
tract.
Use cautiously
with cardiac
disorders,
especially if treated
with cardiac
glycosides,
pregnancy and
lactation.
Adverse Effects:
Dermatologic:
Rash
GI: Nausea,
vomiting,
diarrhea, abdomina
l discomfort, GI
obstruction, GI
bleeding,
GI ulceration or
perforation.
Hematologic:
Hyperkalemia-
increased serum
potassium, ECG
changes (peaking
of T waves, loss of
P waves,
depression of ST
segment,
prolongation of
OTC interval).
Local: Tissue
sloughing, local
necrosis,
local phlebitis, and
venospasm with
injection.
Side Effects:
Confusion,
anxiety, feeling
Consider the 10
Golden Rights of
administering
medication
Arrange for serial
serum potassium
levels before and
during therapy
Administer oral
drugs after meals
or with food and a
full glass of water
to decrease GI
upset.
Caution patient
not to chew or
crush tablet; have
patient swallow
tablet whole.
Caution patient
that expanded wax
matrix capsules
will be found in
stool.
Caution patient
not to use salt
substitutes.
Ask the patient to
have periodic
blood tests and
medical
evaluation.
Tell the patient to
report tingling of
like you might
pass out
Uneven heartbeat
Extreme thirst,
increased urination
Leg discomfort
Muscle weakness
or limp feeling
Numbness or
tingly feeling in
your hands or feet,
or around your
mouth
Severe stomach
pain, ongoing
diarrhea or
vomiting
Black, bloody, or
tarry stools; or
Coughing up blood
or vomit that looks
like coffee grounds
hands or feet,
unusual tiredness
or weakness,
feeling of
heaviness in the
legs, severe
nausea, vomiting,
abdominal pain,
black or tarry
stool.
DRUG MECHANISM OF
ACTION
INDICATION CONTRAINDICATIONS ADVERSE
EFFECTS AND SIDE
EFFECTS
NURSING
RESPONSIBILITIES
Generic
Name
Metronidazole
Brand Name
Flagyl
Classification
Amebicide,
Antibacterial,
Antibiotic,
Antiprotozoal
Sub
Classification
Dosage
500mg/tablet
Route
Oral
Frequency
Thrice a day
(TID)
Form
Tablet
Color
White
Bactericidal:
inhibits DNA
synthesis in
specific
(obligate)
anaerobes,
causing cell
death;
antiprotozoal-
trichomonacidal
, amebicidal:
Biochemical
mechanism of
action is not
known.
Acute infection
with susceptible
anaerobic bacteria
Acute intestinal
amebiasis
Amebic liver
abscess
Trichomoniasis
(acute and partners
of patients
undergoing
colorectal surgery
Unlabeled uses:
Prophylaxis for
patients
undergoing
gynecologic,
abdominal surgery,
hepatic
encephalopathy,
Crohns disease;
antibiotic-
associated pseudo
membranous
colitis, treatment
of Gardnerella
vaginalis,
giardiasis (use
recommended by
the CDC); infected
decubitus ulcers;
perioral dermatitis
Contraindicated
with
hypersensitivity to
metronidazole;
pregnancy ( do not
use for
trichomoniasis in
first trimester)
Use continuously
with CNS diseases,
hepatic diseases,
candidiasis
(moniliasis), blood
dyscrasias,
lactation.
Adverse Effect:
CNS:
Headache,
dizziness,
ataxia,
vertigo,
incoordiantio
n, insomnia,
seizures,
peripheral
neurophaty,
fatigue
GI:
Unpleasant
metallic taste,
anorexia,
nausea,
vomiting,
diarrhea, GI
upset, cramps
GU: Dysuria,
incontinence,
darkening of
the urine
Local:
Thrombophle
bitis (IV);
redness,
burning,
dryness, and
skin irritation
(topical)
Others:
Severe,
Consider the
10 Golden
Rights of
administering
medication
Tell the
patient to
take full
course drug
therapy; take
the drug with
food if GI
upset occur.
Tell the
patient not to
take alcohol
(beverages or
preparations
containing
alcohol,
cough
syrups) for
24-72 hr of
drug use;
severe
reactions may
occur.
Caution the
patient that
their urine
may be
darker in
color than
usual; this is
expected
disulfiram-
like
interaction
with alcohol,
candidiasis
(superinfectio
n)
Side Effects:
Numbness or
tingling in
your hands or
feet;
White patches
or sores
inside your
mouth or on
your lips;
Pain or
burning when
you urinate;
Diarrhea that
is watery or
bloody;
Vision
problems,
pain behind
your eyes;
Trouble
concentrating,
slurred
speech, mood
or behavior
changes,
tremors,
muscle
twitching,
Tell the
patient that
they may
experience
this side
effects like:
Dry mouth
with strange
metallic taste
(frequent
mouth care,
sucking
sugarless
candies may
help); nausea,
vomiting,
diarrhea (eat
frequent
small meals)
Tell the
patient to
report severe
GI upset,
dizziness,
unusual
fatigue or
weakness,
fever, chills.
seizure
(convulsions);
Fever, chills,
muscle pain,
confusion,
headache,
sore throat,
neck stiffness,
increased
sensitivity to
light,
drowsiness,
nausea and
vomiting; or
Severe skin
reaction --
fever, sore
throat,
swelling in
your face or
tongue,
burning in
your eyes,
skin pain,
followed by a
red or purple
skin rash that
spreads
(especially in
the face or
upper body)
and causes
blistering and
peeling.
DRUG MECHANISM
OF ACTION
INDICATION CONTRAINDICATIONS ADVERSE EFFECTS AND
SIDE EFFECTS
NURSING
RESPONSIBILITIES
Generic Name
Metoclopramide
Brand Name
Reglan
Classification
Antiemetic,
Dopaminergic
blocker, GI
stimulant
Sub
Classification
Dosage
1 ampule
Route
Parenteral
Frequency
TID/ q6
Form
Liquid ampule
Color
Clear
Stimulates
motility of
upper GI
tract without
stimulating
gastric,
biliary, or
pancreatic
secretions,
appears to
sensitize
tissues to
action of
acetylcholin
e, relaxes
pyloric
sphincter
which when
combined
with effects
on motility,
accelerates
gastric
emptying
and
intestinal
transit; little
effect on
gallbladder
or colon
motility;
increases
lower
esophageal
sphincter
pressure;
Relief
symptoms of
acute and
recurrent
diabetic
gastroparesis.
Short term
therapy (4-
12weeks) for
adults with
symptomatic
gastro
esophageal
reflux who fail
to respond to
conventional
therapy
Prophylaxis of
postoperative
nausea and
vomiting when
nasogastric
suction is
undesirable
Contraindicated
with allergy to
metaclopramide, GI
hemorrhage,
mechanical
obstruction or
perforation;
pheochromocytoma
(may cause
hypertensive
crisis); epilepsy.
Use continuously
with previously
detected breast
cancer (one third of
such tumors are
prolactin
dependent);
lactation,
pregnancy; fluid
overload; renal
impairment.
Adverse Effects:
CNS: Restlessness,
drowsiness, fatigue,
lasitudes, insomnia,
extrapyramidalreact
ion, parkinsonism-
like reactions,
akathisia, dystonia,
myoclonus,
dizziness, anxiety
CV: Transient
hypertension
GI: Nausea,
diarrhea
Side Effects:
tremors, or restless
muscle movements
in your eyes,
tongue, jaw, neck,
arms, or legs
mask-like
appearance of the
face
very stiff (rigid)
muscles, high
fever, sweating,
confusion, fast or
uneven heartbeats,
tremors, feeling
like you might pass
out
depressed mood,
thoughts of suicide
Consider the 10
Golden Rights of
administering
medication
Asses if the
patient has
historyof
allergies
tometocloprami
de.
Monitor BP
carefully during
IVadministratio
n.
Monitor
extrapyramidal
reactions and
consultphysician
if they occur.
Monitor patients
with diabetes,
arrange for
alteration in
insulin dose or
timing ifdiabetic
control is
comprisedby
alterations in
timing of food
absorption.
Keep
diphenhydramin
e injection
readily available
in case
extrapyramidal
has sedative
properties,
induces
release of
prolactin.
or hurting yourself
hallucinations,
anxiety, agitation,
jittery feeling,
trouble staying still
swelling, fluid
retention
jaundice (yellowing
of your skin or
eyes)
seizure
(convulsions)
Less serious side effects
may include:
feeling restless,
drowsy, tired, or
dizzy
headache, sleep
problems
(insomnia)
nausea, vomiting,
diarrhea
breast tenderness or
swelling
changes in your
menstrual periods
urinating more than
usual
reaction occur
(50mg IM)
Have
phentolamine
readily available
in case of
hypertensive
crisis (most
likely to occur
with
undiagnosed
pheochromocyto
ma)
Do not use
alcohol, sleep
remedies, or
sedatives;
serious sedation
could occur.
Tell the patient
that they may
experience these
side effects:
drowsiness,
dizziness (do
not drive or
perform other
task that
requires
alertness);
restlessness,
anxiety,
depression,
headache,
insomnia
(reversible);
nausea, diarrhea.
Tell the patient
to report
involuntary
movement of
the face, eyes, or
limbs, severe
depression, and
severe diarrhea.
DRUG MECHANISM
OF ACTION
INDICATION CONTRAINDICATIONS ADVERSE EFFECTS AND
SIDE EFFECTS
NURSING
RESPONSIBILITIES
Generic
Name
Furosemide
Brand Name
Lasix
Classification
Loop
Diuretics
Sub
Classification
Dosage
10mg
Route
Parenteral
Frequency
STAT
Form
Liquid ampule
Color
Clear
Inhibits
reabsorption of
sodium chloride
from the
proximal and
distal tubules
and ascending
limb of the loop
of Henle,
leading to a
sodium-rich
diuresis.
Oral, IV:
Edema
associatedwit
h heart
failure,
cirrhosis,rena
l disease.
IV: acute
Pulmonary
Edema
Oral:
hypertension
Contraindicated
with allergy to
furosemide,
sulfonamides,
allergy to tartrazine
(in oral solution);
anuria, severe renal
failure; hepatic
coma; pregnancy;
lactation.
Use cautiously with
SLE, gout, diabetes
mellitus.
Adverse Effects:
CNS: dizziness,
vertigo, paresthesias,
xanthopsia, weakness,
headache, drowsiness,
fatigue, blurred vision,
tinnitus, irreversible
hearing loss
CV: orthostatic
hypotension, volume
depletion, cardiac
arrhythmias,
thrombophlebitis
Dermatologic:
photosensitivity, rash,
pruritus, urticaria,
purpura, exfoliative,
dermatitis, erythema
multiforme
GI: nausea, anorexia,
vomiting, oral and
gastric irritation,
constipation, diarrhea,
acute pacreatitis,
jaundice
GU: polyuria, nocturia,
glycosuria, urinary
bladder spasm.
Hematologic:
leukopenia, anemia,
thrombocytopenia, fluid
and electrolytes
imbalance,
hyperglycemia,
hyperuricemia
Consider the
10 Golden
Rights of
administering
medication
Profound
dieresis with
water and
electrolyte
depletion can
occur, careful
medical
supervision is
required.
Administer
with food or
milk to prevent
GI upset.
Reduce dosage
if given with
other anti
hypertensive;
readjust
dosage
gradually as
BP responds.
Give early in
the day so that
increase
urination will
not disturb
sleep.
Do not mix
parenteral
solution with
highly acidic
Others: Muscle cramps
and muscle spasm
Side Effects:
Common side effects of
furosemide:
low blood pressure
dehydration
electrolyte depletion
(for example, sodium,
potassium)
Less common side effects
include :
jaundice,
ringing in the ears
(tinnitus)
sensitivity to light
(photophobia)
rash
pancreatitis
nausea
diarrhea
abdominal pain
dizziness
Increased blood sugar
increase uric acid level
salutions with
pH below 3.5
Do not expose
to light, which
may discolor
tablets or
solution; do
not use
discolored
drug or
solution.
Discard
diluted
solutions after
24 hr.
Measure and
record weight
to monitor
fluid change
Arrange to
monitor serum
electrolytes,
hydration,
liver and renal
function.
Arrange with
potassium rich
diet or
supplemental
potassium as
needed.
Tell the patient
that they may
experience this
side effects:
increased
volume and
frequency of
urination;
dizziness,
feeling faint on
arising,
drowsiness
(avoid rapid
position
changes;
hazardous
activities, like
driving and
consumption
of alcohol);
sensitivity to
sun light( use
sun glasses,
wear
protective
clothing, or
use sunscreen;
increased thirst
(suck on
sugarless
lozenges; use
frequent
mouth care);
loss of body
potassium(a
potassium rich
diet or
potassium
supplement
will be
needed).
Tell the patient
to report loss
or gain of
more than
1.5kg in 1 day,
swelling in the
ankle or
fingers,
unusual
bleeding or
bruising,
dizziness,
trembling,
numbness,
fatigue, muscle
weakness or
cramps.
DRUG MECHANISM
OF ACTION
INDICATION CONTRAINDICATIONS ADVERSE EFFECTS
AND SIDE EFFECTS
NURSING
RESPONSIBILITIES
Generic Name
Omeprazole
Brand Name
Zefxon
Classification:
Antisecretory
drug
Proton pump
inhibitor
Sub
Classification
Dosage
40mg
Route
Parenteral
Frequency
twice a day (BID)
Form
Powder in vial,
diluted with
sterile water
Color
Cloudy
Gastric acid
pump inhibitor
suppresses
gastric acid
secretion by
specific
inhibition of
the hydrogen
potassium
ATPase
enzymes
system at the
secretory
surface of the
gastric parietal
cells; blocks
the finalstep
acid
production.
Short term
treatment of
active
duodenal ulcer.
Treatment of
heartburn or
symptoms of
GERD
Short term
treatment of
active benign
gastric ulcer
GERD, severe
erosive
esophagitis,
poorly
responsive
symptomatic
GERD
Long term
therapy:
treatment of
pathologic
hypersecretory
conditions
(Zollinger
Ellisons
syndrome,
multiple
adenomas,
systemic
mastocytosis)
Eradication of
H. pylori with
amoxicillin or
metronidazole
Contraindicated
with
hypersensitivity to
Omeprazole or its
components
Use cautiously with
pregnancy,
lactation
Adverse Effects:
CNS: headache,
dizziness,
asthenia, vertigo,
insomnia, apathy,
anxiety,
paresthesias,
dream
abnormalities
Dermatologic:
rash,
inflammation,
urticaria, pruritus,
alopecia, dry skin.
GI: diarrhea,
abdominal pain,
nausea, vomiting,
constipation, dry
mouth, tongue
atrophy
Respiratory: URI
symptoms, cough,
epistaxis
Others: cancer in
preclinical studies,
back pain, fever
Side Effects:
Dizziness (avoid
driving or
performing
hazardous tasks)
headache (request
medications)
Consider the 10
Golden Rights
of administering
medication
Assess other
medications
patient may be
taking for
effectiveness
and interactions
(especially
those dependent
on cytochrome
P450
metabolism or
those dependent
on acid
environment for
absorption).
Monitor
therapeutic
effectiveness
and adverse
reactions at
beginning of
therapy and
periodically
throughout
therapy.
Assess GI
system: bowel
sounds every
8hours,
abdomen for
pain and
swelling,
and
clarithromycin
nausea
vomiting
diarrhea (maintain
proper nutrition)
symptoms of URI
cough (do not self-
medicate; consult
with your health
care provider if
uncomfortable).
appetite loss.
Monitor hepatic
enzymes: AST,
ALT, increased
alkaline
phosphatase
during
treatment.
Tell the patient
to report if
experiencing
this side effects:
dizziness,
headache,
nausea,
vomiting,
diarrhea.
DRUG MECHANISM
OF ACTION
INDICATION CONTRAINDICATIONS ADVERSE EFFECT
AND SIDE EFFECT
NURSING
RESPONSIBILITIES
Generic Name
Ambroxol HCL
Brand Name
Ambrolex
Classification
Mucolytic
Sub
Classification
Dosage
75mg
Route
Oral
Frequency
Once a day
Form
Capsule
Color
Half white and
half green
It makes phlegm
in the airways
thinner and less
sticky. It does this
by increasing the
body's natural
production of
surfactant. This
contributes to a
secretomotoric
effect: it helps the
cilia - tiny hairs
that line the
respiratory tract -
to transport the
phlegm out of the
lungs.
Adjuvant therapy in
patients with abnormal,
viscid, or in spissated
mucous secretions in
acute and chronic
broncho pulmonary
diseases, and in
pulmonary
complications of cystic
fibrosis and surgery,
tracheostomy, and
atelectasis.
There is no absolute
contraindication but in
patient with gastric
ulceration relative caution
should be observed.
Adverse Effect:
Occasional
gastrointestinal
side effects may
occur but these
are almost
invariably mild
Rashes
Fatigue
Dry mouth
Rhinorrhea
Constipation
Dysuria
Contact
dermatitis
Consider the 10
Golden Rights of
administering
medication
Monitor S/Sx of
aspiration of
excess secretions
and for
bronchospasm.
Have suction
apparatus
immediately
available.
Tell the client to
report difficulty
with clearing the
airway or any
other respiratory
distress.
Tell the client to
report if
experiencing this
side effects: GI
upset, rashes,
fatigue, dry mout.
DRUG MECHANISM
OF ACTION
INDICATION CONTRAINDICATIO
NS
ADVERSE EFFECT
AND SIDE EFFECTS
NURSING
RESPONSIBILITIES
Generic Name
Cefuroxime Sodium
Brand Name
Zinacef
Classification
Antibiotic,
Cephalosporin
Sub Classification
Second generation
Dosage
750mg
Route
Parenteral
Frequency
q8
Form
powder in vial,
diluted with sterile
water
Color
Bactericidal:
inhibits synthesis
of bacterial cell
wall, causing cell
death.
Lower
respiratory
infections
caused by S.
pneumonia, S.
aureus, E. coli,
Klebsiella
pneumonia, H.
influenza, S.
pyogenes
Dermatologic
infections
caused by S.
aureus, S.
pyogenes, E.
coli, K.
pneumonia,
Enterobacter
UTIs caused
by E. coli, K.
pneumonia
Uncomplicated
and
disseminated
gonorrhea
caused by N.
gonorrhoeae
Septicimia
caused by S.
Contraindicate
d with allergy
to
cephalosporins
or penicillins
Use
continuously
with renal
failure,
lactation,
pregnancy
Side Effects
Diarrhea, stomach
upset
Difficulty of
breathing
Anusual tiredness
or fatigue
Pain at injection
site
Adverse Effect:
CNS: headache,
dizziness,
lethargy,
paresthesias
GI: nausea,
vomiting,
diarrhea,
anorexia,
abdominal pain,
flatulence,
pseudomenbranou
se colitis,
hepatotoxicity
GU:
Nephrotoxicity
Hematologic:
Consider the 10
Golden Rights of
administering
medication
Determine history
of hypersensitivity
reactions
to cephalosporins,
penicillins, and
history of
allergies,
particularly to
drugs, before
therapy is initiated.
Lab tests: Perform
culture and
sensitivity tests
before initiation of
therapy and
periodically during
therapy if
indicated. Therapy
may be instituted
pending test
results. Monitor
periodically BUN
and creatinine
clearance.
Do skin test before
Light yellow
pneumonia, S.
aureus, E. coli,
K pneumonia,
H. influenza
Meningitis
caused by S.
pneumoniae,
H. influenza,
S. aureus, N.
meningitides
Bone and joint
infections due
to S. aureus
Perioperative
prophylaxis
Treatment of
acute bacterial
maxillary
sinusitis in
patients 3-mo
12yr
Bone marrow
depression
Hypersensitivity:
ranging from rash
to fever to
anaphylaxis;
serum sickness
reaction
Local: pain,
abcess at injection
site, phlebitis,
inflammation of
IV site
Others:
superinfection,
disulfram- like
reaction with
alcohol
administering the
drug
Inspect IV
injection sites
frequently for
signs of phlebitis.
Monitor for
manifestations of
hypersensitivity.
Discontinue drug
and report their
appearance
promptly.
Monitor I&O rates
and pattern:
Especially
important in
severely ill
patients receiving
high doses. Report
any significant
changes.
Tell the client to
report loose stools
or diarrhea
promptly.
Tell the client to
avoid alcohol
while taking this
drug and for 3days
after because
severe reaction
often occurs.
DRUG MECHANISM OF
ACTION
INDICATION CONTRAINDICATIO
NS
ADVERSE
EFFECTS AND
SIDE EFFECTS
NURSING
RESPONSIBILITIES
Generic Name
Paracetamol
Brand Name
Biogesic
Classification
Non- narcotic
analgesic,
Antipyretic
Sub
Classification
Dosage
300mg
Route
P.O
Frequency
PRN
Form
Ttablet
Color
Orange
Decreases
fever by a
hypothalamic
effect leading
to sweating
and
vasodilation
Inhibits
pyrogen effect
on the
hypothalamic-
heat-regulating
centers
Inhibits
CNS prostagla
ndin synthesis
with minimal
effects on
peripheral pros
taglandin synth
esis
Does not cause
ulceration of
the GI tract
and causes no
anticoagulant
action
Control of pain
due to headache,
earache,
dysmenorrhea,
arthralgia,
myalgia,
musculoskeletal
pain,
arthritis, immuni
zations, teething,
tonsillectomy
Reduce fever in
viral
and bacterial infe
ctions
As a substitute
for aspirin in
upper GI disease,
bleeding
disorders clients
in anticoagulant
therapy and
gouty arthritis
Anemia, cardiac
& pulmonary
disease. Hepatic
or severe renal
disease.
Liver toxicity
(hepatocyte
necrosis) may
occur with
doses not far
beyond labeled
dosing.
Side Effects:
Minimal GI
upset,
methemoglo
binemia,
hemolytic
anemia,
neutropenia,
thrombocyto
penia,
pancytopenia
,
leucopenia,ur
ticaria, CNS
stimulation,
hypoglycemi
c coma,
jaundice,
glissitis,
drowsiness,
liver damage
Adverse Effect
Allergic skin
reactions &
GI
disturbances.
Consider the 10
Golden Rights of
administering
medication
Monitor CBC,
liver and renal
functions.
Assess for fecal
occult blood and
nephritis.
Tell the patient to
avoid using OTC
drugs
with Acetaminoph
en
Tell the patient to
take the drug with
food or milk to
minimize GI upset.
Tell the client to
report N&V.
cyanosis, shortness
of breath and
abdominal pain as
these are signs of
toxicity.
Tell the client to
report paleness,
weakness and heart
beat skips
Tell the client to
report abdominal
pain, jaundice,
dark urine,
itchiness or clay-
colored stools.
Tell the client that
Phenmacetin may
cause urine to
become dark
brown or wine-
colored.
Tell the client to
report pain that
persists for more
than 3-5 days
Tell the client that
this drug is not for
regular use with
any form of liver
disease because it
might cause further
damage.
DRUG MECHANISM
OF ACTION
INDICATION CONTRAINDICATIO
NS
ADVERSE EFFECT
AND SIDE EFFECT
NURSING
RESPONSIBILITIES
Generic Name
Aminoleban
Brand Name
Classification
V06DD - Amino
acids, incl.
combinations with
polypeptides ; Used
as general nutrients.
Sub Classification
Dosage
500mg
Route
Parenteral
Frequency
q8
Form
Liquid
Color
Clear
Given to
normalize
the amino
acid,
carbohydr
ates, fats,
vitamins
and
minerals
in the
plasma
Hepatic
encephalopathy
due to acute or
chronic liver
diseases & of -
ve nitrogen
balance when
adequate
nutrition PO or
gastro duodenal
tube is
impossible or
undesirable.
Patient with
abnormal amino
acid metabolism
(since the infuse
amino acids are
not adequately
metabolized,
the patient
clinical
condition may
be worsened.)
Severe renal
disorders
Adverse Effect:
Cardiovascular:
Chest discomfort,
& palpitation.
Hypersensitivity:
rare skin
eruptions
Gastrointestinal:
occasional nausea
and vomiting
Others:
occasional chills,
fever, headache
Side Effects:
Hypoglycemia
may occur and
hyperammonemia
has been reported.
Hypersensitivity
reactions such as
skin rash may
occur rarely.
Nausea, vomiting,
chest discomfort
and palpitations
may occur
infrequently.
Large doses and
rapid
Consider the 10
Golden Rights of
administering
medication
Asses patients
condition before
starting the
therapy.
Be alert to
adverse reaction.
Monitor patient
temperature.
If GI reaction
occur monitor
patient
hydration.
Tell the patient
to report if felt
this side effects:
nausea,
vomiting, chest
discomfort,
palpitation occur.
administration
may lead to
acidosis.
Chills, fever and
headache may
infrequently
occur.
DRUG MECHANISM OF
ACTION
INDICATION CONTRAINDICATI
ONS
ADVERSE EFFECT
AND SIDE EFFECTS
NURSING
RESPONSIBILITIES
Generic Name
Sinutab extra-
strength
Brand Name
Sinutab Forte
Classification
phenylpropanola
mine,
combinations ;
Belongs to the
class of systemic
sympathomimeti
c preparations
used as nasal
decongestant
Sub
Classification
Dosage
1 cap
Route
oral
Frequency
TID
Form
Capsule
Color
Red and yellow
Sinutab Extra-
Strength is a
fixed-dose
combination
capsule containing
the following 3
active ingredients:
Phenylpropanola
mine HCl (PPA)
or Phenylephrine:
A systemic
decongestant to
relieve clogged
nose and sinuses.
Chlorphenamine
Maleate or
Phenyltoloxamine
Citrate: An
antihistamine/anti
allergy.
Paracetamol: A
pain killer, as well
as an antipyretic
(for fever).
Temporary
relief of sinus
headache;
promote nasal
and sinus
drainage; help
relieve runny
nose, facial
pain, malaise
and fever often
associated with
colds,
influenza,
acute and
chronic
sinusitis,
allergic rhinitis
(hay fever) and
vasomotor
rhinitis.
Patients who
are
hypersensiti
ve or allergic
to any of the
components
of Sinutab
Extra-
Strength.
Unless
otherwise
advised by a
physician,
during
pregnancy
and
lactation,
patients with
severe
kidney
disease or
who are
taking other
medications
containing
PPA.
Adverse Effect:
chest pain, rapid
pulse, fast or
uneven heart
rate;
confusion,
hallucinations,
severe
nervousness;
tremor, seizure
(convulsions);
easy bruising or
bleeding,
unusual
weakness;
little or no
urinating;
nausea, pain in
your upper
stomach,
itching, loss of
appetite, dark
urine, clay-
colored stools,
jaundice
(yellowing of
your skin or
eyes); or
Dangerously
high blood
pressure (severe
headache,
blurred vision,
buzzing in your
ears, anxiety,
Consider the 10
Golden Rights of
administering
medication
Tell the patient not
take more of this
medication than is
recommended. An
overdose of
acetaminophen can
damage your liver
or cause death.
Instruct the patient
that this
medication could
not use if she/he
are allergic to
acetaminophen,
chlorpheniramine,
or
pseudoephedrine.
Inform patient that
she need to avoid
drinking alcohol. It
may increase your
risk of liver
damage while
taking
acetaminophen,
and can increase
certain side effects
of
chlorpheniramine.
Explain to the
patient that theres
a side effects that
chest pain,
shortness of
breath, uneven
heartbeats,
seizure).
Side Effect:
dizziness,
drowsiness;
mild headache,
blurred vision;
dry mouth,
nose, or throat;
constipation;
feeling nervous;
sleep problems
(insomnia);
she may
experience upon
taking the
medication such as
blurred vision or
impair your
thinking or
reactions.
If other unwanted
effects not
previously listed
occur, consult a
physician.
DRUG MECHANISM OF
ACTION
INDICATION CONTRAINDICATION
S
ADVERSE EFFECTS
AND SIDE EFFECTS
NURSING
RESPONSIBILITIES
Generic Name
Ketorolac
Tromethamine
Brand Name
Toradol
Classification
nonsteroidal anti-
inflammatory
agents, nonopioid
analgesics
Sub Classification
pyrroziline
carboxylic acid
Dosage
30 mg
Route
Parenteral
Frequency
q8
Form
Liquid ampule
Color
Clear
Inhibits
prostaglandin
synthesis,
producing
peripherally
mediated
analgesia.
Also has
antipyretic and
anti-
inflammatory
properties.
Therapeutic
Effects:
Decreased pain.
Short-term
manageme
nt of pain
(not to
exceed 5
days total
for all
routes
combined).
Contraindicated
in:
Hypersensitivity
Cross-sensitivity
with other
NSAIDs may exist
Pre- or
perioperative use
Known alcohol
intolerance
(injection only)
Perioperative pain
from coronary
artery bypass graft
(CABG) surgery .
Use Cautiously
in:
Cardiovascular
disease or risk
factors for
cardiovascular
disease (may risk
of serious
cardiovascular
thrombotic events,
myocardial
infarction, and
stroke, especially
with prolonged
Adverse Effects:
CNS:
drowsiness,
abnormal
thinking,
dizziness,
euphoria,
headache.
Respiratory:
asthma,
dyspnea.
CV: edema,
pallor,
vasodilation.
GI: GI
bleeding,
abnormal taste,
diarrhea, dry
mouth,
dyspepsia, GI
pain, nausea.
GU: oliguria,
renal toxicity,
urinary
frequency.
Dermatologic:
exfoliative
dermatitis,
Stevens Johnson
Syndrome, toxic
Consider the 10
Golden Rights of
administering
medication
Assessment
Patients who have
asthma, aspirin-induced
allergy, and nasal polyps
are at increased risk for
developing
hypersensitivity reactions.
Assess for rhinitis,
asthma, and urticaria.
Pain: Assess pain (note
type, location, and
intensity) prior to and 1-2
hr following
administration.
Lab Test
Considerations: Evaluate
liver function tests,
especially AST and ALT,
periodically in patients
receiving prolonged
therapy. May cause
levels.
tell the patient that it
may cause prolonged
bleeding time that may
persist for 24-48 hr
following discontinuation
of therapy.
Inform the patient that
it may cause BUN,
serum creatinine, or
use)
History of GI
bleeding
Renal impairment
(dosage reduction
may be required)
necrolysis
pruritus,
purpura,
sweating,
urticaria.
Hematology:
prolonged
bleeding time.
Local: injection
site pain.
Neurology:
paresthesia.
Misc: allergic
reactions
including,
anaphylaxis
Side Effects:
chest pain,
weakness,
shortness of
breath, slurred
speech,
problems with
vision or
balance;
black, bloody,
or tarry stools;
coughing up
blood or vomit
that looks like
coffee grounds;
swelling or
rapid weight
potassium concentrations.
.
Implementation
Do not confuse Toradol
(ketorolac) with Torecan
(thiethylperazine) or
tramadol (Ultram).
Administration in
higher-than-recommended
doses does not provide
increased effectiveness but
may cause increased side
effects. Duration of
ketorolac therapy, by all
routes combined, should
not exceed 5 days Use
lowest effective dose for
shortest period of time.
Coadministration with
opioid analgesics may
have additive analgesic
effects and may permit
lower opioid doses. .
PO: Ketorolac therapy
should always be given
initially by the IM or IV
route. Use oral therapy
only as a continuation of
parenteral therapy.
injection, 0.9%
NaCl.
Patient/Family
Teaching
Instruct patient
on how and when
to ask for pain
gain;
urinating less
than usual or
not at all;
nausea, stomach
pain, low fever,
loss of appetite,
dark urine, clay-
colored stools,
jaundice
(yellowing of
the skin or
eyes);
fever, sore
throat, and
headache with a
severe
blistering,
peeling, and red
skin rash;
the first sign of
any mouth sores
or skin rash, no
matter how
mild;
pale skin, easy
bruising, severe
tingling,
numbness, pain,
muscle
weakness; or
fever, headache,
neck stiffness,
chills, increased
sensitivity to
light, purple
spots on the
skin, and/or
medication.
Instruct patient
to take medication
exactly as directed.
Take missed doses
as soon as
remembered if not
almost time for
next dose. Do not
double doses. Do
not take more than
prescribed or for
longer than 5 days.
May cause
drowsiness or
dizziness. Advise
patient to avoid
driving or other
activities requiring
alertness until
response to the
medication is
known.
Caution patient
to avoid the
concurrent use of
alcohol, aspirin,
NSAIDs,
acetaminophen, or
other OTC
medications
without consulting
health care
professional.
Advise patient
to inform health
care professional
of medication
regimen prior to
seizure
(convulsions).
Less serious side
effects may include:
upset stomach,
mild nausea or
vomiting,
diarrhea,
constipation;
mild heartburn,
stomach pain,
bloating, gas;
dizziness,
headache,
drowsiness;
sweating; or
ringing in your
ears.
treatment or
surgery.
Advise patient
to consult health
care professional if
rash, itching,
visual
disturbances,
tinnitus, weight
gain, edema, black
stools, persistent
headache, or
influenza-like
syndrome (chills,
fever, muscle
aches, pain)
occurs. .
Evaluation/Desire
d Outcomes
Decrease in
severity of pain.
Patients who do
not respond to one
NSAID may
respond to another.
DRUG MECHANISM OF
ACTION
INDICATION CONTRAINDICATIO
NS
ADVERSE EFFECTS
AND SIDE EFFECTS
NURSING
RESPONSIBILITIES
Generic Name
Perindopril
Brand Name
Coversyl plus
Classification
Antihypertensive
Sub
Classification
ACE Inhibitor
Dosage
1 cap
Route
oral
Frequency
BID
Form
Tablet
Color
White
Antihypertensive
.
Pharmacology:
Perindopril is an
ACE-inhibitor
that works by
widening the
blood vessels,
which makes it
easier for the
heart to pump
blood through
them.
Indapamide is a
diuretic that
causes an
increase in the
amount of urine
produced.
Each of the
active ingredients
of Coversyl Plus
reduces blood
pressure and
work together to
control blood
pressure.
Treatment
of essential
hypertensio
n
Allergy to
perindopril or
other ACE-
inhibitors, or to
indapamide or
any other
sulfonamides.
History or
presence of
wheezing,
swelling of the
face or tongue,
intense itching
or severe skin
rashes with
previous ACE-
inhibitor
treatment, or
other
circumstances
(eg,
angioedema).
Severe liver
diseases or if
suffering from
hepatic
encephalopathy
; severe kidney
disease, or on
dialysis; low or
high blood
potassium;
Adverse Effect:
CNS: dizziness,
asthenia, sleep
disorder,
paresthesia,
depression,
somnolence,ner
vousness,
headache.
CV: palpitati
ons, edema,
chest pain, ab
normal ECG.
EENT:rhinitis,
sinusitis, ear
infection,
pharyngitis,
tinnitus.
GI: dyspepsia,
diarrhea,
abdominalpain,
nausea, vomi
ting, flatulenc
e.
GU: proteinur
ia, urinarytrac
t infection, m
alesexual
dysfunction,
menstrual
disorder.
Consider the 10
Golden Rights of
administering
medication
Assess patients
condition.
Dont let the
patient to take this
if she has an
allergy to
penidopril. And if
she has a history of
wheezing, swelling
of the face or
tongue, intense
itching or severe
skin rashes.
Explain to patient
what was the
medication for,
and what are the
side effects that
she may encounter.
Instruct the patient
to consult her
doctor if she
experiencing
unwanted effect.
untreated
decompensated
heart failure
(severe water
retention,
difficulty in
breathing);
children.
Use in
pregnancy &
lactation: Cove
rsyl Plus should
not be used
during the first
3 months of
pregnancy and
must not be
taken from the
4th month of
pregnancy.
When
pregnancy is
planned or
confirmed, the
switch to an
alternative
treatment
should be
initiated as soon
as possible.
Do not take
Coversyl Plus if
breastfeeding.
Musculoskele
tal: back
pain,
hyperonia,
neck pain,
joint pain,
myalgia,
arthritis, arm or
leg pain
Respiratory:
cough, upper
respiratory
infection
Skin: Rash
Other: viral
infection,
injury, seasonal
allergy
Side Effect:
Cough, often
described as dry
and irritating,
shortness of
breath,
discomfort on
exertion.
Headache,
dizziness,
vertigo, pins
and needles.
Changes in the
rhythm or rate
of the heart
beat, fast or
irregular heart
beat
Stroke,
myocardial
infarction,
angina pectoris
(a feeling of
tightness,
pressure or
heaviness in the
chest).
Feeling tired or
lethargic.
Tinnitus
(persistent noise
in the ears),
vision
disturbances.
Hypotension,
flushing,
impaired
peripheral
circulation, nose
bleeds.
Nausea,
vomiting, taste
disturbances,
indigestion,
diarrhoea,
constipation or
stomach pain.
Muscle cramps.
Rash, pruritus
(itching).
Eosinophilic
pneumonia.
Hepatitis.
Renal failure.
Bleeding or
bruising more
easily than
normal caused
by a low blood
platelet count ,
frequent
infections such
as fever, severe
chills, sore
throat or mouth
ulcers caused by
a lack of white
blood cells,
pancytopenia (a
rare type of
anaemia).
Decreased
blood sugar
levels.
Fainting.
You might also like
- Collection of Questions From Previous HAAD ExamsDocument34 pagesCollection of Questions From Previous HAAD ExamsRehan Usman83% (29)
- Drug Study-Med WardDocument2 pagesDrug Study-Med WardErnest Brian FernandezNo ratings yet
- Drug Study: Davao Doctors College General Malvar ST., Davao City Nursing ProgramDocument3 pagesDrug Study: Davao Doctors College General Malvar ST., Davao City Nursing ProgramJear RomeroNo ratings yet
- FlecainideDocument3 pagesFlecainideAlexandra AntondyNo ratings yet
- Ertapenem (Invanz)Document1 pageErtapenem (Invanz)Adrianne BazoNo ratings yet
- Drug StudyDocument11 pagesDrug StudyKimberly Ann MendozaNo ratings yet
- Drug Study (AFP)Document10 pagesDrug Study (AFP)Summer SuarezNo ratings yet
- Drug StudyDocument11 pagesDrug StudyMichelle TamorNo ratings yet
- Name of Drug Content Class and Mechanism of Action (MOA) Indication/s Contraindication/s Side Effects (Pere System) Nursing ConsiderationsDocument8 pagesName of Drug Content Class and Mechanism of Action (MOA) Indication/s Contraindication/s Side Effects (Pere System) Nursing ConsiderationsJustin John NavarroNo ratings yet
- Drug StudyDocument12 pagesDrug StudyFiela De VillaNo ratings yet
- Drug Study For PneumoniaDocument15 pagesDrug Study For PneumoniaPrincess Pauline Abrasaldo100% (1)
- Drug Study (Room 104)Document4 pagesDrug Study (Room 104)Maeshe Pryll TanamorNo ratings yet
- Drug StudyDocument49 pagesDrug StudyMitz BaldizarNo ratings yet
- Drug 101Document12 pagesDrug 101Alyzza DagoyNo ratings yet
- Drug StudyDocument12 pagesDrug StudyAngeli A EstilloreNo ratings yet
- TramadolDocument2 pagesTramadoldwightciderNo ratings yet
- College of Nursing: Cebu Normal UniversityDocument5 pagesCollege of Nursing: Cebu Normal UniversityChelsea WuNo ratings yet
- Duavent Drug Study - CunadoDocument3 pagesDuavent Drug Study - CunadoLexa Moreene Cu�adoNo ratings yet
- Drug Study 1Document15 pagesDrug Study 1Czarina Isabela TuazonNo ratings yet
- Drug StudyDocument4 pagesDrug StudyLene ThereseNo ratings yet
- Generic (Trade Name) Dosage / Frequency Classification Indication Contraindication Side Effects Nsg. ResponsibilitiesDocument4 pagesGeneric (Trade Name) Dosage / Frequency Classification Indication Contraindication Side Effects Nsg. Responsibilitiesliesel_12100% (1)
- Zolpidem TartrateDocument2 pagesZolpidem TartrateAndrea Huecas TriaNo ratings yet
- Nursing Drug Study (Albendazole)Document6 pagesNursing Drug Study (Albendazole)Kristel Diane RidaoNo ratings yet
- Drug StudyDocument14 pagesDrug StudyWendy EscalanteNo ratings yet
- Losartan Plus HydrochlorothiazideDocument18 pagesLosartan Plus Hydrochlorothiazidegmsanto7No ratings yet
- Drug StudyDocument34 pagesDrug Studypoleene de leonNo ratings yet
- Drug Name Generic Name Classification Mechanism of Action Indication Contra Indication/precautions Adverse Effect Dosage Nursing InterventionsDocument4 pagesDrug Name Generic Name Classification Mechanism of Action Indication Contra Indication/precautions Adverse Effect Dosage Nursing InterventionsTedd CamilingNo ratings yet
- Iron SucroseDocument3 pagesIron SucroseAtul KumarNo ratings yet
- Metoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDocument9 pagesMetoclopramide: GIT Regulators, Antiflatulents & Anti-Inflammatories Antiemetics See Available Brands of MetoclopramideDominique RamosNo ratings yet
- Drug StudyDocument23 pagesDrug StudyampalNo ratings yet
- Drug StudyDocument12 pagesDrug StudyAdrianPaul Dela CruzNo ratings yet
- Dynastat: What Is in This LeafletDocument4 pagesDynastat: What Is in This LeafletBenj GilbuenaNo ratings yet
- Drug StudyDocument33 pagesDrug Studyjefwy8No ratings yet
- Drug Ferrous SulfateDocument1 pageDrug Ferrous SulfateSrkocherNo ratings yet
- Drug Card PradaxaDocument2 pagesDrug Card PradaxaBen0% (1)
- Drug Study EditedDocument5 pagesDrug Study EditedfabtaciousVeelaNo ratings yet
- Drug StudyDocument3 pagesDrug StudyKervin TalledoNo ratings yet
- Ds in Delivery RoomDocument11 pagesDs in Delivery RoomArian May MarcosNo ratings yet
- Tetanus Immune Globulin: Deanzel Jade TrazonaDocument9 pagesTetanus Immune Globulin: Deanzel Jade TrazonaIrene Grace BalcuevaNo ratings yet
- Drug Study-Sodium BicarbonateDocument7 pagesDrug Study-Sodium BicarbonateTrisha Faye OrtegaNo ratings yet
- Lasix - Drug StudyDocument2 pagesLasix - Drug StudyRosalinda PerigoNo ratings yet
- Drug Study For SLEDocument28 pagesDrug Study For SLERomwella May AlgoNo ratings yet
- Drug Study - CapDocument5 pagesDrug Study - CapABARAJNo ratings yet
- Drug StudyDocument9 pagesDrug StudyLynel Joy JamotilloNo ratings yet
- Drug Study....Document5 pagesDrug Study....Maria Jelyn SarmientoNo ratings yet
- "Uterine Leiomyoma " A Case Study: Saint Mary's University School of Health and Natural SciencesDocument75 pages"Uterine Leiomyoma " A Case Study: Saint Mary's University School of Health and Natural SciencesKyla CarbonelNo ratings yet
- Mindanao State University - Iligan Institute of Technology Student: ALEXA MURIEL L. MOZAR Section: BLOCK 261Document2 pagesMindanao State University - Iligan Institute of Technology Student: ALEXA MURIEL L. MOZAR Section: BLOCK 261Alexandra AntondyNo ratings yet
- Drug Study DulcolaxDocument2 pagesDrug Study DulcolaxReisha Fungo0% (1)
- MannitolDocument3 pagesMannitolAlexandra AntondyNo ratings yet
- Drug StudyDocument6 pagesDrug StudyBadeth BustamanteNo ratings yet
- Drug StudyDocument3 pagesDrug Studyanon_11638632No ratings yet
- Duodenal UlcerDocument4 pagesDuodenal UlcerLourenz BontiaNo ratings yet
- Indacaterol GlycopyrroniumDocument1 pageIndacaterol GlycopyrroniumNeulAskiel FloresNo ratings yet
- Drug Study: CNS: DizzinessDocument1 pageDrug Study: CNS: Dizzinessmarsh155No ratings yet
- Drug Study KeterolacDocument2 pagesDrug Study KeterolacKillerBall RegioNo ratings yet
- Drug Study RifampicinDocument1 pageDrug Study RifampicinEphraim MaravillaNo ratings yet
- Diagnostics - Nursing ResponsibilitiesDocument9 pagesDiagnostics - Nursing ResponsibilitiesCarmellaDawn100% (3)
- Name of Drug Action Indication Contra-Indication Side Effects Nursing ConsiderationsDocument11 pagesName of Drug Action Indication Contra-Indication Side Effects Nursing ConsiderationsMalou SanNo ratings yet
- Drug StudyDocument10 pagesDrug StudyHelen ReonalNo ratings yet
- CVA Drug StudyDocument51 pagesCVA Drug StudyKarel LuNo ratings yet
- Final SCIDocument65 pagesFinal SCIiamjenivicNo ratings yet
- Time Trends in The Prevalence of Atherosclerosis: A Population-Based Autopsy Study in March 2011Document5 pagesTime Trends in The Prevalence of Atherosclerosis: A Population-Based Autopsy Study in March 2011iamjenivicNo ratings yet
- Acute GastroentiritisDocument1 pageAcute GastroentiritisiamjenivicNo ratings yet
- Gordons Functional Health PatternDocument8 pagesGordons Functional Health PatterniamjenivicNo ratings yet
- Huerto, Coleen Comelle I. Pancreatic Cancer May Be Identified by Molecular Marker From Pancreatic 'Juices'Document3 pagesHuerto, Coleen Comelle I. Pancreatic Cancer May Be Identified by Molecular Marker From Pancreatic 'Juices'iamjenivicNo ratings yet
- NCP 1Document7 pagesNCP 1Roldan VidadNo ratings yet
- Anti Protozoal DrugssssDocument37 pagesAnti Protozoal DrugssssKrizia mae LaureanoNo ratings yet
- Vaginitis ACOG 2006Document17 pagesVaginitis ACOG 2006xiomara andrea rios coquecoNo ratings yet
- Case P On Lung AbscessDocument20 pagesCase P On Lung AbscessanShUl 002100% (1)
- Chin 2001Document13 pagesChin 2001zaheerbdsNo ratings yet
- Obat - BMDocument50 pagesObat - BMNovita PermataNo ratings yet
- Blastocystis: To Treat or Not To Treat.: InvitedarticleDocument6 pagesBlastocystis: To Treat or Not To Treat.: Invitedarticlepavaroti37No ratings yet
- NCP DrugDocument13 pagesNCP DrugMhar CamposanoNo ratings yet
- Regañon - Rle Case # 1Document22 pagesRegañon - Rle Case # 1Darla Janyll RegañonNo ratings yet
- Guideline Antibiotic RationalDocument35 pagesGuideline Antibiotic RationalIstianah EsNo ratings yet
- Odontogenic Infections: Ickman Setoaji W, DRG., MMDocument66 pagesOdontogenic Infections: Ickman Setoaji W, DRG., MMAmeliza Putri AlindNo ratings yet
- Sush PMBDocument38 pagesSush PMBAnindaNo ratings yet
- Detailed Drug StudyDocument5 pagesDetailed Drug StudyKarl Vincent SosoNo ratings yet
- Drug StudyDocument6 pagesDrug StudyArdrina SappariNo ratings yet
- What Is Bacterial Vaginosis and What Are The Symptoms?Document3 pagesWhat Is Bacterial Vaginosis and What Are The Symptoms?Mymy SofiNo ratings yet
- 2012 Aug IMG Poster 165760a SepsisDocument1 page2012 Aug IMG Poster 165760a SepsisTeng Huei LeeNo ratings yet
- Characterization and Treatment of Recurrent Bacterial VaginosisDocument9 pagesCharacterization and Treatment of Recurrent Bacterial VaginosisKhusnul Eka PratiwiNo ratings yet
- Myoma Final Power PointDocument45 pagesMyoma Final Power Pointicesexy100% (1)
- ORNIDAZOLEDocument9 pagesORNIDAZOLEroopendramauryaNo ratings yet
- Fire Belly ToadsDocument12 pagesFire Belly ToadsAmy Thomas StanislawskiNo ratings yet
- Guidelines For Office Gynecology in JapanDocument17 pagesGuidelines For Office Gynecology in JapanKatherine ZevallosNo ratings yet
- Manual of Obstetrics, 8e (Jun 25, 2014) - (1451186770) - (LWW) PDFDocument766 pagesManual of Obstetrics, 8e (Jun 25, 2014) - (1451186770) - (LWW) PDFPrem100% (9)
- Davao Doctors College Nursing Program Drug Study: General Malvar St.,DavaocityDocument3 pagesDavao Doctors College Nursing Program Drug Study: General Malvar St.,DavaocityJerremy LuqueNo ratings yet
- SHC Antimicrobial Prophylaxis in Surgery RecommendationsDocument3 pagesSHC Antimicrobial Prophylaxis in Surgery RecommendationsCatherine MorrisNo ratings yet
- Phcist Letter Sept 2006Document52 pagesPhcist Letter Sept 2006MichelNo ratings yet
- Hirschprung Associated EnterocolitisDocument9 pagesHirschprung Associated Enterocolitiskeyla_shineeeNo ratings yet
- Drug Study - MetronidazoleDocument1 pageDrug Study - MetronidazoleDeeRicachoMembela76% (17)
- Antiamebic DrugsDocument17 pagesAntiamebic DrugsAhmed AmgedNo ratings yet
- Bacterial VaginosisDocument12 pagesBacterial VaginosisAudioBhaskara TitalessyNo ratings yet