Professional Documents
Culture Documents
Copd Notes
Uploaded by
family_jvc0 ratings0% found this document useful (0 votes)
71 views27 pagesCOPD
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCOPD
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
71 views27 pagesCopd Notes
Uploaded by
family_jvcCOPD
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 27
COPD
Monday, July 09, 2012
10:05 AM
Page 1
Obstructive Lung Disease: COPD
Anthony J. Busti, PharmD, FNLA, FAHA
Editor-in-Chief
Pharmacology Weekly Inc.
Background of COPD
COPD is also a major contributor to other co-
morbidities:
- Pneumonia
- Stroke
- lung cancer
- Heart Disease
Right sided heart failure (indicates severe COPD)
Pulmonary hypertension
Cor pulmonale
Arch Intern Med 2003,163 797802
Ctrculat.on 2003;107 1514-1519
Arln Intern Med 1987,106 512-518
COil 1 Oi>mb .. tlonV. trod tt
C1010 .... !,lnc.. Allllif;ha RtwrW!d
Page 2
Background of COPD
A chronic disease characterized as:
- An irreversible obstruction of airflow typically
from inflammation and emphysematous changes
in lung tissue.
- Airway hyperresponsiveness also occurs in about
60- 80% of patients.
- Broken down into chronic bronchitis and
emphysema (centriacinar and panacinar)
Am J Resp11Cnt Care Med 2001.163 1256-1276
ArnRev Resplf Ots 1992.145301310
ec;. ,....,& Oillr
Cl2010
Types of Emphysema
Centriacinar (Centrilobular):
- Most common type in smokers
- Destruction of the distal terminal and respiratory bronchioles
in mainly UPPER airway
Panacinar:
- Most common type in patients with alpha-1 antitrypsin (AAT)
deficiency; patients with MM phenotype make normal
amounts vs. ZZ phenotype release very little from liver
Smokmg 1nh1b1ts AAT abtlity to breakdown elastase released from the
neutrophtls thereby causmg proteolytiC degradation of elastm m lung
- Presents early in life if genetic type
- Destruction of the distal respiratory unit ( respiratory
bronchioles) in mainly LOWER airway
Oi\mht iOf'l W otkOUlApprOif.jlll\ Proltlh uod
Cl2010 Inc. All JUo!!.u
Page 3
Types of Emphysema
Paraseptal Emphysema:
- Localized disease in a subpleural location
- Primarily targets the alveolar ducts and alveoli
- Does not produce obstructive airway disease
- Increased spontaneous pneumothorax due to
rupture of subpleural blebs
Irregular Emphysema:
- Localized disease associated with scar tissue
-Also does not produce obstructive airway disease
ec;.,....,& Oillr
02010 6
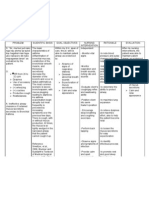
Comparison of Obstructive Lung Diseases
Asthma:
- Eosinophiles
- Airway hyperreactivity
- Bronchodilator response
- Inhaled corticosteroid
response
COPD:
- Neutrophils
- No airway hyperreactivity
- limited bronchodilator
response
- limited inhaled
corticosteroid response
Oi\trohtiOf'IWotkOUlApprOif.jli!tProlllh uod
02010 Inc. All JUo!!.u
Page 4
Obstructive Airway Diseases
ec;. ,....,& Oillr
02010 8
Risk Factors
Tobacco smoking is leading ri sk factor
Smoking
- 80-90% of all risk factors
- Only 12-15% of smokers have COPD
- Smoking cessation is the most important therapy for
improving health outcomes
Occupational effects (chronic exposure to vapors,
etc.)
Childhood illnesses especially associated with
low-birth weight, respiratory infections, &
symptomatic childhood asthma
JAN.A 1994 27214971505
Oi\trohtiOf'IWotkOUlApprOif.jli!tProlllh uod
02010 Inc. All JUo!!.u
Page 5
COPD: Pathophysiology
Chronic Bronchitis:
- Airway inflammation and hypersecretion of
mucous
Peri bronchiolar fibrosis results in narrowing of
peripheral airways, loss of elastic recoil
Intraluminal mucous may contribut e to airflow
obstruction
Reflected by a Reid index >0.4 (ratio of the thickness
of mucous gland layer to t hickness of the wall
between epithelium & cartilage)
Co,>, r>a&
02010 AIIJioialou R....-.'<'d
COPD: Pathophysiology
Emphysema:
- Influx of neutrophils that release IL-8, LTB4, elastase, cathepsin
and proteinase-3-A creating an imbalance towards destruction
- Macrophages are activated by cigarette smoking and release of
TNFo, LTB4, ll-8, ROA, & proteinases
- T-lymphocytes infiltrate small airways, lung parenchyma and
adventitial layer of pulmonary arteries & shift balance of
CD4+/CD8+ T cell ratio towards CDS+ which correlates to the
degree of airflow obstruction
- Loss of elastic recoil (patency in the smaller airways depends on
elastic recoil and as intraluminal pressure is reduced the airways
collapse)
- Presence of parenchymal destruction & airflow obstruction
- Airway obstruction
Is progressive
May be partially due to hyperreactivity
May be partially reversible
U>py.n 3 & Oimobuuon Wothouu\ppr.,..l" Po oil bl@d
02010 Ph IN<OiocYWffk t Inc. All Re1HW<I
Page 6
Cl inical Presentation
Chronic Bronchitis:
- Chronic, productive cough >
3 months in 2
consecutive years
- Moderate dyspnea
- Recurrent respiratory
infections
-Obese
- Greater risk of cor
pulmonale due to hypoxia
- " Blue Bloater" because of
mucous plugs in terminal
bronchioles
Emphysema:
- Little to no cough
- Diminished breath
sounds due to
hyperinflation
- Severe dyspnea
- Thin extremities
- Barrel-chested
- Pursed lipped breathing
- "Pink Puffer"
(OF, "'6 Olwobuuon WothoUI ProhlbitP<I
C2010 PtwtNCIOiopWff'iy Inc. All Jliillll
Pertinent History
Smoking history
- Pack per day
- Cessation history
- Willingness to quit: use clinical markers as an incentive to
quit.
Ext ent and severity of symptoms
Occupational and environmental exposure
Use of oxygen
Cot> r It OIHibutlon ll/11hoU1 Prohol>otP<I
Page 7
Differential Diagnosis
Bronchial asthma
Bronchiectasis
Cystic fibrosis
Bronchiolitis (obliterative, follicular, diffuse)
Alpha-1 antitrypsin deficiency
Coal workers pneumoconiosis
Upper airway obstruction: vocal cord paralysis
or dysfunction, tracheal tumors, tracheal
stenosis, traf:heomalacia
Cop 1 & Di<1 nbuuon 1<Prohlb t..d
C2010 R.....-.....t 1
Diagnosis of COPD
Patient history and clinical presentation
Presence of nonreversible airway restriction
Confirmed by spirometry
- FEV
1
< 80% of predicted value
- FEV dFVC < 70%
Cop & Di\ltlbuttonW.tho .. bot!!d
C2010 Ph.,NcoiosvWco..O,'vlnc. All Jliiflu R<!M'fW'd
Page 8
Normal Lung Volumes
IRV
I(
vc
Volume TV
TLC
2.2 L
ERV
1.2 L 1----+-
FRC
RV
RV
Ol
Figure 1. Normal lung volumes during various respiratory cycles.
()2010 Pharmacology Weekly Inc.
(op'( n o;.,nbwuon Prohlh<c..t
.... -..1 16
Lung Volumes: Restricted vs. Obstructive
VOIUITK'
6.0
IRV
l.]l
Ul
1V
RV
uL
RV
Ol
rfp9 ..,.,...., ........ voeum., d"'nc v-. ,.,.,.,.,...,.
O >OH) PNnnKolosy WHI.Iy Inc..
nc
RV
<op., Oi<HobwuonWrchoUIAppr.,.,l" Prohlh<c..t
ClJOIOPhtNcoiosr'h'H tlnc. AIIJI.ihuR.-...,-..1 11
Page 9
Normal Flow Volume Loop
Expiration
Inspiration
8L/s
4L/S
Volume (L)
4L/S
Peak Inspiratory flow Rate
8L/S
rigure 1. Nonnallung flow volume loop.
01010 Pharmacology Weekly Inc.
Obstructive Lung Disease
Expiration
Inspiration
8L/s
4L/S
4L/S
8L/s
Normal: = > 0.70
Obstruction: FEV1/FVC = < 0.70
Figure 1. Obstructive lung disease flow volume loop.
Pharmacology Weekly Inc.
13
19
Page 10
Classification of COPD
Guidelines for Obstructive Lung Disease (GOLD)
Stage Severity FEV
1
FEV
1
/FVC Symptoms
I Mild 2!80% <70% With/without
II Moderate 50%-80% <70% With/without
Ill Severe 30%-50% <70/o With/without
Respiratory
IV
Very
<30%
<70% failure/right
Severe
<50%
heart failure
Arterial Blood Gases
Low to normal cq.mpensated pH (normal 7.35-
7.45)
High pC02 (chronic respiratory aci dosis; normal
is 35-45)
Low Pa02 (chronic hypoxemia; normal 80-100
mmHg)
eop., ng Oi<Hobuuon Prohlh<ud
02010 PhuNcoiO(yW..., tlnc. All Jl.iht< 11
Page 11
Chest X-Ray Findings
Hyperlucency
Increased anterior-post erior diamet er
Vert ically oriEfcnted heart
Depressed or "fl attened" di aphragms due to
hyperinflati on
()1010 I'Nnnacolol'WnUr Inc. AlllliGhll 1!..--d 22
Progression of COPD
Nonsmokers: ! FEVl 25-30 ml/yr (after age 35)
..
Smokers: !>60 ml/yr
5 year mortality is about SO% in patients with an FEVl < 1
Liter
Only way to stop decline in FEVl is smoking cessation.
Prognosis: BODE Index
- j!ody mass index (BMI)
- Obstruction or Degree of airflow limitation (0)
- Dyspnea
- capacity (6 minutes walk test)
Value: 0-10; the higher the worse the prognosis/mortalit y
cern BR elal NEJM 2004.350(10) 1005-12
Protalb tood
()1010 Inc. Alll!l;;!>u Rew<Wid 23
Page 12
Goals of Treatment
Stop smoking
Improve symptoms and quality of life
- Attempt to reduce health care utilization
Prevent and treat complications
Reduce decline in lung function
Increase survival
Cop,
() 2010 'ly Inc. AIIRopu
Monitoring
Disease of
- Expect condition to worsen over time
Monitor for changes in symptoms
- Patient diary
- Spouse and family
Spirometry if significant change in symptoms
Adverse Effects
Cop r It 11/lthoi.il Prohol> t..d
Page 13
General Considerations to Current Therapy
No cure
- symptom control
- Prevent1on of exacerbations
- None of the short-acting bronchodilators decrease the rate of decline in
lung function or survival.
Regimen not decreased
Patient specific
Increase therapy based on patient progression
Pulmonary rehabilitation should be considered as part
of the treatment plan especially in moderate to severe
patients
Consider ::!: home 0
2
JAMA.1994 272 1497-1505
Am J Respw Cnt Cere Med 2002,166 333-339
Eur Resptt J 2002.19 393-404
Cotr{.n ProhlbitfOd
01010 AII!Uptt
Current Therapy
Smoking cessation: tt
- Consider incentives as a motivation:
The FEV
1
1n smokers dechnes at a rate of 60 ml/yr vs. 30 ml/yr in ex-
smokers
Reductions in all-cause mortahty of about 27'"/o
Reductions in cardiOvascular related mortalit y- relat1ve nsk of 0.54
compared to contmued
- Approach to treatment:
Counseling, education, mcotme replacement and buprop1on can
resul t in abstinence rates of about 25%
JAJ.'.A.1994 2721497-1505
JAA'.A 1982 2481465-1477
Prev M_, 2002.35 314-319
Color "
01010 lolc. "-'YYd
Page 14
Current Pharmacotherapeutic Options
Bronchodilators:
-
agonists (short & long acting)
- Anticholinergics (short & long acting)
- Methylxanthines
- Mucolytic:s (no longer recommended by GOLD)
'(
Corticosteroids:
-Oral vs.IV
-Inhaled
Cotr{.n ProhlbitfOd
01010 AII!Uptt
Inhaled Anticholinergics
Color" 29
01010 lolc.
Page 15
Anticholinergic Agents
Short-Acti ng Agents:
- lpratropium bromide (Atrovent): MDI, Neb
- lpratropium/albuterol (Combivent, OuoNeb) : MDI, Neb
Long-Acti ng Agents:
- Tiotropium Bromide (Spiriva): DPI
Cotr{.n ProhlbitfOd
01010 AII!Uptt
MOA: Anticholinergic Agents
Blocking of the muscarinic receptor
results in j cGMP levels
l
! Intracellular c a
1
Smooth muscle relaxation
CoJ>,.,
01010 lolc. "-'YYd
Page 16
Anticholinergic Agents
Tiotropium bromide (Spiriva)
1 capsule per inhaler QD
Side Effects: minimat but can experience
dry eyes, increase risk of worsening narrow
angle glaucoma, and dry mouth.
Notes:
-May offer improvement compared to
ipratropium due to compliance
Cotr{.n ProhlbitfOd
01010 AII!Uptt
Anticholinergic Agents
Tiotropium bromide:
- A recent meta-analysis of 5 clinical trials including 3,574
patients witt+moderate - severe COPD followed up for 6
months showed a 26% (RR, 0.74; 95%CI, 0.62- 0.89)
reduction in exacerbation rates when compared to
placebo.
- When compared to ipratropium there was still a reduction
in exacerbations (RR, 0.78; 95% Cl, 0.63- 0.95).
JAJ,'IA 2003 290 23012312
CoJ>,.,
01010 lolc. "-'YYd
Page 17
Anticholinergic Agents
Tiotropium bromide:
-It is FDA approved to reduce exacerbation rates
when compared to long-acting P
2
-agonists. Can
delay time to first exacerbation by about 4
months.
-In addition, the effect of tiotropium on trough
FEV
1
is good:
an average of 121 ml per year compared to placebo or
ipratropium monotherapy.
An additional 37 ml compared to long-acting
agonists over 6 months
JAMA2003 290 2301-2312
Cotr{.n ProhlbitfOd
01010 AII!Uptt
Corticosteroids
Inhaled corticosteroids:
- A recent meta-ar:}alysis of 6 placebo-controlled clinical
trials including 1,741 patients w1th follow up for 2 6
months showed a 24% (95%CI, 20- 28%) reduction in
exacerbation rates.
- The majority of this benefit was seen in patients with
mean FEV
1
< 2l; pooled RR, 0.75 (95% Cl, 0.71-0.80)
compared toRR of 0.96 (95% Cl, 0.77-1.20) in patients
whose mean FEV
1
was > 2l.
JAMA 2003 290 2301-2312
CoJ>,.,
01010 lolc. "-'YYd
Page 18
Lung Health Study and EUROSCOP
Bone Mineral Data
972 patients with 3 to 4 years of follow up
A net reduction in BMD of 1.57% (95% Cl , 2.40%-
0.74%) in the femoral neck and 1.07/o (95/o Cl,
1.86%-0.28/o) in the lumbar spine.
No excess fractures seen (RR, 0.70; 95% Cl , 0.36-
1.37)
The lifetime risk remains unknown
N Engl J Med 2000 3.4319021909
EurRespvJ 2002.191058-1063
Cotrf.n ProhlbitfOd
01010 AII!Uptt
Mucolytic Agents
L
Ambroxol, erdosteine, carbocysteine
May be of very small benefit in pts with viscous
sputum
Not enough evidence to support wide spread
use per GOLD guidelines
CoJ>,.,
01010 lolc. "-'YYd
Page 19
Vaccinations
It
Pneumococcal (Pneumovax-23)
Influenza
Though their use has not been specifically
evaluated in COPD, in the elderly population
they have been shown to reduce all -cause
pneumonia and cardiac hospitalization and
deaths by 30- 40%.
JAMA 1994 272 16611665
N Engl J Med 2003.348 13221332
Cop,
() 2010 'ly Inc. AIIRopu
Home Oxygen Therapy
Supplemental home 0
2
is effective a
prolonging survival whose resting Pa02 is <
60 mm Hg.
2 trials totaling 290 patients, revealed a RR,
0.61 (95% Cl, 0.46-0.82)
Only has small benefit on mean pulmonary
arterial pressure and CRQ scores.
Eur Respr J 2002 20 306-312
Ann Intern Med 1985,102 2936
Cop r It 11/lthoUI Prohol>ot..d
Page 20
Home Oxygen Therapy
Indications for long-term oxygen therapy:
- Pa02 s; 55 fl\mHg or Sa02 < 88%
- Pa02 56-59 mmHg with:
EKG evidence of pulmonary HTN or cor pulmonale
Secondary erythrocytosis (Hct > 55%)
Clinical evidence of right sided heart failure and/or pedal
edema
- Oxygen delivery options:
Concentrator (converts room air to higher concentrations)
0-cylinder (carry on the patients back)
E-cylinder (type that you pull canister around with)
()1010 I'Nnnacolol'WnUr Inc. AlllliGhll 1!..--d .&0
Page 21
Drugs to use with Caution in COPD
P-Biockers: (especial ily
- Recent data suggests carvedilol may be better tolerated
than selective B-Biocker
Respiratory Depressants:
- Opioids
- Benzodiazepines
- Only a concern initially & at specific doses
- Antitussives {regular use)
(opy>n& & rlb.,llon WithoiM ProhobMd
All llo;;hto Rt .. ro'f'd
Smoking Cessation
Pack per day
Cessation history
Willingness to quit
Method:
- Use of US Pu'blic Healt h Service 5-step program
- Use of bupropion (Wellbutrin; Zyban) or nortriptyline
- Nicotine patches, gum
- Counseling
(opy>na & Ol1 rlb.,llon WithoiM Prohob.tl'd
Cl2010 All Ro;;ht> Re->er.'f'd
Page 22
Global lnitiative for Chronic
Obstructive Lung Disease
(GOLD)
2008 Guidelines
(opy>n& & rlb.,llon WithoiM ProhobMd
All llo;;hto Rt .. ro'f'd
Significant Changes
Stage 0: At Risk
- no longer included as a stage of COPD
- insufficient evidence that patients with chronic cough and
sputum production and normal spirometry necessarily
progress to Stage 1: Mild COPD
Varenicline (Chantix)
- mentioned as being safe and efficacious for smoking
cessation
- no recommendation regarding its specific role
Page 23
Bronchodilators
Central to symptomatic management
No effect on disease progression Qr prognosis
Give PRN for relief of persist ent or worsening symptoms or
regularly to prevent or reduce symptoms
Regular use of LABA or anticholinergic improves health status
Inhaled route preferred
Long-acting agents
- more effective and convenient than short-acting agents
(opy>n& & rlb.,llon WithoiM ProhobMd
All llo;;hto Rt .. ro'f'd
Bronchodilators
Nebulizers not recommended
- more expensive, require maintenance
- not appropriate for stable patients unless shown to be better
than conventional therapy
- nebulized anticholinergics reported to precipitate glaucoma
Increasing dosage of bronchodi lator
- beneficial in acute episodes, but not in stable disease
- higher doses increase side effects
Combination bronchodilator therapy
- increased bronchodilation
(opy>na & Ol1 rlb.,llon WithoiM Prohob.tl'd
Cl2010 All Ro;;ht> Re->er.'f'd
Page 24
Corticosteroids
Effect s less dramatic in COPD t han in asthma
- Role limited to specific indications
Oral not r ec:ornrnended for routine
use
Inhaled corti cost eroids
- no effect on long-term decline of FEVl
- do reduce frequency of exacerbations and improve health
status
- appropriate for patients with Stage Ill (Severe) and Stage IV
(Very Severe) COPD and repeated exacerbations
- combination of inhaled glucocorticosteroid + LABA more
effective than individual components
(opy>n& & rlb.,llon WithoiM ProhobMd
All llo;;hto Rt .. ro'f'd
Stepwise Approach to Therapy
Stage 1: Mild COPO (few or intermittent symptoms)
- Short-acting i nhaled bronchodilator PRN
Stage II: Moderate to Stage IV: Very Severe COPD with dyspnea
during daily activities not c-ontrolled with PRN short-acting
bronchodilator
- Add long-acting bronchodilator (LABA or tiotropium)
- addition of theophylline may provide additional benefits
Stage Ill or IV with repeated exacerbations
- Add regular treatment with ICS to long-acti ng inhaled bronchodilator
Page 25
Exacerbations - Home Management
Increase dose and/or frequency of existing short-acting
bronchodilator therapy
- If not already used, anticholinergic can be added until symptoms
improve
- No difference in clinical response between MOl with a spacer
and nebulizer
Systemic glucocorticosteroids beneficial
- 30-40 mg/day for 7-10 days
Exacerbations - Home Management
Increase dose and/or frequency of existing short-acting
bronchodilator therapy
- If not already used, anticholinergic can be added until symptoms
improve
- No difference in clinical response between MOl with a spacer
and nebulizer
Systemic glucocorticosteroids beneficial
- Prednisolone 30-40 mg/day for 7-10 days
Q
Page 26
Therapy at Each Stage of COPD
I: Mild II: Moderate
FEVdFVC < 70%
FEVtfFVC < 70%
III: Severe
FEV P.-./C < 7 ~ o
30% < FEV < soo'O
pred1cted
Conclusion
Differences in t reatment
IV: Very Severe
FEV FVC < 70o'o
FEV < 300.o pred>cted
o FEY < 50% prea cted
pas chron c ew;atory
fa ue
long term oxygen
if chronic respiratory
failure.
surgiCal treatments
Importance of t reatment vs. maintenance t herapy
Importance of education and inhaler technique
GINA and GOLD Guidelines
Page 27
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Immune Complexes Deposit in The JointsDocument1 pageImmune Complexes Deposit in The Jointsfamily_jvcNo ratings yet
- BB Unit7RhSpring2011Document20 pagesBB Unit7RhSpring2011family_jvcNo ratings yet
- Chapter 35 - Clinical Chemistry and The PediatricDocument3 pagesChapter 35 - Clinical Chemistry and The Pediatricfamily_jvcNo ratings yet
- Review ChemDocument2 pagesReview Chemfamily_jvcNo ratings yet
- BB unit7RhSpring2011Document56 pagesBB unit7RhSpring2011Jayniel Erys MollenoNo ratings yet
- Tutorial For Unit 1 (Acanthamoeba and N Fowleri Included)Document60 pagesTutorial For Unit 1 (Acanthamoeba and N Fowleri Included)family_jvcNo ratings yet
- Mls Imls Reading ListDocument3 pagesMls Imls Reading ListDeanne LambanNo ratings yet
- Carbon Dioxide (Liquid) Reagent Set: AnalyzeDocument2 pagesCarbon Dioxide (Liquid) Reagent Set: Analyzefamily_jvcNo ratings yet
- Diagnosis EntamoebaDocument2 pagesDiagnosis EntamoebaElsya ApriliaNo ratings yet
- Case Study For Unit 1Document95 pagesCase Study For Unit 1family_jvcNo ratings yet
- Dilution HelpDocument4 pagesDilution Helpfamily_jvcNo ratings yet
- PretransfusionTesting EditedDocument70 pagesPretransfusionTesting Editedfamily_jvcNo ratings yet
- Mls Imls Reading ListDocument3 pagesMls Imls Reading ListDeanne LambanNo ratings yet
- Dilution HelpDocument4 pagesDilution Helpfamily_jvcNo ratings yet
- Secondary Hemostasis: Coagulation Factors and PathwaysDocument4 pagesSecondary Hemostasis: Coagulation Factors and Pathwaysfamily_jvcNo ratings yet
- Case Study For Unit 1Document95 pagesCase Study For Unit 1family_jvcNo ratings yet
- Endocrine or Hormonal FunctionDocument1 pageEndocrine or Hormonal Functionfamily_jvcNo ratings yet
- ImmunoassayDocument20 pagesImmunoassayfamily_jvc100% (1)
- Exercise 7Document4 pagesExercise 7family_jvcNo ratings yet
- CrystalDocument8 pagesCrystalfamily_jvcNo ratings yet
- Exam 1 Review Questions - PresentationDocument43 pagesExam 1 Review Questions - Presentationfamily_jvcNo ratings yet
- BB unit7RhSpring2011Document56 pagesBB unit7RhSpring2011Jayniel Erys MollenoNo ratings yet
- 3 Complement and CytokinesDocument31 pages3 Complement and Cytokinesfamily_jvcNo ratings yet
- C Elegan ProjectDocument11 pagesC Elegan Projectfamily_jvcNo ratings yet
- Solute Activity Coefficients From DissociationDocument1 pageSolute Activity Coefficients From Dissociationfamily_jvcNo ratings yet
- The Experiment Was Conducted To Test Out The Hypothesis That With The Use of Drosophila Melanogaster Fruit FliesDocument1 pageThe Experiment Was Conducted To Test Out The Hypothesis That With The Use of Drosophila Melanogaster Fruit Fliesfamily_jvcNo ratings yet
- TyeryDocument51 pagesTyeryfamily_jvcNo ratings yet
- BuiDocument1 pageBuifamily_jvcNo ratings yet
- BuiDocument1 pageBuifamily_jvcNo ratings yet
- BuiDocument1 pageBuifamily_jvcNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Ineffective Airway ClearanceDocument1 pageIneffective Airway ClearancejomerdalonaNo ratings yet
- Tecme Neumovent Technical Manual 94Document94 pagesTecme Neumovent Technical Manual 94Marina Garza GaliciaNo ratings yet
- Chest Physiotherapy ChecklistDocument1 pageChest Physiotherapy ChecklistRhea Mae BeeNo ratings yet
- Pengaruh Variasi Tekanan Negatif Suction Endotracheal Tube (Ett) Terhadap Nilai Saturasi Oksigen (Spo)Document4 pagesPengaruh Variasi Tekanan Negatif Suction Endotracheal Tube (Ett) Terhadap Nilai Saturasi Oksigen (Spo)Amin KutbiNo ratings yet
- KTP 1 RespiratoryDocument5 pagesKTP 1 RespiratoryMarisa TullochNo ratings yet
- Finals Act 5Document2 pagesFinals Act 5zoro100 88No ratings yet
- Mechanical Ventilation Weaning Protocol GuideDocument48 pagesMechanical Ventilation Weaning Protocol GuideJR VendeventerNo ratings yet
- LCP Asthma Club Seminar Teaches Patients to Manage AsthmaDocument2 pagesLCP Asthma Club Seminar Teaches Patients to Manage AsthmaEliseo RamirezNo ratings yet
- Chest TraumaDocument25 pagesChest Traumadrpravalk100% (1)
- Upper Respiratory Tract Infection (Uri)Document4 pagesUpper Respiratory Tract Infection (Uri)Anna Zhifa AbNo ratings yet
- ANNEX F (Page 1of 3)Document12 pagesANNEX F (Page 1of 3)elmersgluethebombNo ratings yet
- Enfermedad Pulmonar IntersticialDocument39 pagesEnfermedad Pulmonar IntersticialDanhi V. EchevarriaNo ratings yet
- Bronchiolitis PDFDocument5 pagesBronchiolitis PDFjuniorebindaNo ratings yet
- Approach of TraumaDocument45 pagesApproach of TraumaAqila MumtazNo ratings yet
- Acute BronchitisDocument4 pagesAcute BronchitisLenjunNo ratings yet
- Besmed Indonesia - Google SearchDocument1 pageBesmed Indonesia - Google SearchPelayanan ResusitasiNo ratings yet
- Kronik. Fakultas Kedokteran Universitas Lampung. J Majority: Vol 4 No 5Document2 pagesKronik. Fakultas Kedokteran Universitas Lampung. J Majority: Vol 4 No 5ayu praptiNo ratings yet
- A Male Adult Patient Hospitalized For Treatment of A Pulmonary Embolism Develops Respiratory AlkalosisDocument4 pagesA Male Adult Patient Hospitalized For Treatment of A Pulmonary Embolism Develops Respiratory AlkalosisCezanne CruzNo ratings yet
- Breathing Circuits For SLE6000 - EnglishDocument4 pagesBreathing Circuits For SLE6000 - EnglishIndah P SariNo ratings yet
- Nursing Assessment and Care Plan for Asthma ExacerbationDocument3 pagesNursing Assessment and Care Plan for Asthma ExacerbationElla Neiza AngelesNo ratings yet
- Pharmacotherapy For COPD: Prepared ByDocument35 pagesPharmacotherapy For COPD: Prepared ByYogi RavalNo ratings yet
- Bronchiolitis in ChildrenDocument16 pagesBronchiolitis in ChildrenNym Angga Santosa100% (1)
- Diagnosis, Treatment, and Prevention of 2019 Novel Coronavirus Infection in Children: Experts' Consensus StatementDocument10 pagesDiagnosis, Treatment, and Prevention of 2019 Novel Coronavirus Infection in Children: Experts' Consensus StatementBaiq DysaNo ratings yet
- Trauma ThoraksDocument54 pagesTrauma ThoraksLisana ShidqiNo ratings yet
- Ventilation Handbook WordDocument55 pagesVentilation Handbook WordHndr100% (2)
- 3rd Edition Self-Assessment in Respiratory MedicineDocument267 pages3rd Edition Self-Assessment in Respiratory MedicineamjadsabahNo ratings yet
- Chronic Obstructive Pulmonary Disease: Prof. Ma. Nancy T. MartinezDocument24 pagesChronic Obstructive Pulmonary Disease: Prof. Ma. Nancy T. MartinezKrizzia Charmaine Rallonza BaggayanNo ratings yet
- eVolution 3e HP Ventilator Features and SpecificationsDocument5 pageseVolution 3e HP Ventilator Features and SpecificationsPamela OsunzaNo ratings yet
- Modes of Mechanical Ventilation For The Operating Room BestPracResAnest 2015 PDFDocument15 pagesModes of Mechanical Ventilation For The Operating Room BestPracResAnest 2015 PDFRicardoNo ratings yet
- Bronchial+asthma+questionnaire ApplicantDocument2 pagesBronchial+asthma+questionnaire ApplicantClaudine Limasa TabudlongNo ratings yet