Professional Documents
Culture Documents
Gynzmedicalzhistoryzquestionnaire PDF
Uploaded by
api-2674300630 ratings0% found this document useful (0 votes)
27 views2 pagesOBSTETRIC HISTORY Number of Pregnancies: Vaginal Deliveries: Cesarean Deliveries: Largest Baby Weight: Forceps or Vacuum Yes No Episiotomy Yes No Laceration / Tear Yes No Degree / Details Other Complications or Prolonged Labor. MEDICAL CONDITIONS AND MEDICATIONS Please list all your medical conditions, the medication(s) you are taking for them (If any), how long you have been on
Original Description:
Original Title
GYNZMEDICALZHISTORYZQUESTIONNAIRE.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentOBSTETRIC HISTORY Number of Pregnancies: Vaginal Deliveries: Cesarean Deliveries: Largest Baby Weight: Forceps or Vacuum Yes No Episiotomy Yes No Laceration / Tear Yes No Degree / Details Other Complications or Prolonged Labor. MEDICAL CONDITIONS AND MEDICATIONS Please list all your medical conditions, the medication(s) you are taking for them (If any), how long you have been on
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
27 views2 pagesGynzmedicalzhistoryzquestionnaire PDF
Uploaded by
api-267430063OBSTETRIC HISTORY Number of Pregnancies: Vaginal Deliveries: Cesarean Deliveries: Largest Baby Weight: Forceps or Vacuum Yes No Episiotomy Yes No Laceration / Tear Yes No Degree / Details Other Complications or Prolonged Labor. MEDICAL CONDITIONS AND MEDICATIONS Please list all your medical conditions, the medication(s) you are taking for them (If any), how long you have been on
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
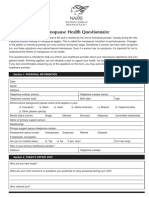
Practice Forms: GYN Medical History Questionnaire Revised: August 2013
MEDICAL HISTORY QUESTIONNAIRE
Name Date of Birth Age Drug Allergies: Reactions:
Please describe the reason for your visit (chief complaint)
OBSTETRIC HISTORY
Number of Pregnancies: Vaginal Deliveries: Cesarean Deliveries: Largest Baby Weight:
Forceps or Vacuum Yes No
Episiotomy Yes No Laceration/Tear Yes No
Degree/Details Other Complications or Prolonged
Labor
GYNECOLOGIC HISTORY
Gynecologist Name: Do you experience any of the following? (check ones you have)
Gynecologist Phone Number:
Bleeding between periods
Date of last menstrual period:
Heavy menstrual periods
Date of last PAP smear: Normal?
Pain with periods
Date of last mammogram: Normal?
Bleeding after intercourse
Have you ever had a sexually transmitted disease?
Pain with intercourse
If Yes, when?
Falling of pelvic organs or prolapse
Are you sexually active at the present time?
Are you presently taking, or have you taken in the past,
hormone replacement therapy? If yes, medication and dose
Are you using contraception? If yes, what type? schedule, vaginal/oral:
MEDICAL CONDITIONS AND MEDICATIONS
Please list ALL your medical conditions, the medication(s) you are taking for them (If any), how long you have been on the medication.
Medical Condition Name of Medication
Dosage
How often you take it
How long have you been on
the medication?
Example Hypertension Tenormin 50mg 1 daily 2 years
Reviewed with Patient____________ _____/_____/______
Drs Initials & Date
Practice Forms: GYN Medical History Questionnaire Revised: August 2013
Name DOB Date
PAST SURGICAL AND HOSPITAL HISTORY: None Yes, if yes
Please describe your past experience with, operations, serious injuries, all and any
hospitalizations and related treatments. Please include dates (month/year) of any surgeries.
FAMILY HISTORY
Are there medical events in your familys history, including diseases that may be hereditary or place you at risk?
Please circle Y or N for each condition (no blanks please )
Yes No Condition Yes No Condition Yes No Condition
Y N Asthma Y N Diabetes Y N Stroke
Y N Bleeding problems Y N Heart Disease Y N Thyroid Disease
Y N Breast Disease Y N High Blood Pressure Y N Other
Y N Breast CA Y N Kidney Disease
Y N Cancer (indicate type)
Y N Adopted
SOCIAL HISTORY
Marital Status
Single Married
Widowed Separated Divorced
Drug/Alcohol Use: Yes No
Drinks/week
Current Smoker: Yes
Former Smoker: Yes
# of Cigarettes/day
Never Smoked:
Highest Level of Education Employment (please include job title)
Race: Caucasian African American Hispanic
Asian American Other
Ethnicity: Latino / Hispanic Other Refused
REVIEW OF SYSTEMS
Do you have or have you had any serious or chronic medical conditions?
Please Circle Y or N for any condition(s) you have had or that you have currently. (no blanks please )
Yes No Yes No Yes No
Constitutional: Weight change Y N Fatigue Y N
Eyes: Vision changes Y N Cataracts Y N Glaucoma Y N
Ears/Nose/Mouth/Throat: Ulcers Y N URI (upper respiratory infection) Y N
Cardiovascular: Chest pain Y N Orthopnea (difficulty breathing
when lying down)
Y N DOE (difficulty breathing
on exertion)
Y N
Respiratory: SOB (short of breath) Y N Wheezing Y N
Gastrointestinal: Nausea/Vomiting Y N Diarrhea Y N Bloody Stool Y N
Musculoskeletal: Weakness Y N
Integumentary/Skin: Rash Y N
Neurological: Seizure Y N Syncope (fainting) Y N Neuropathy Y N
Psychiatric: Depression Y N Anxiety Y N
Endocrine: Hot Flashes Y N Diabetes Y N Thyroid Y N
Hematologic/Lymphatic: Easy bruising Y N Bleeding Y N Adenopathy (Swollen Y N
Allergic/Immunologic: : Seasonal Y N Animal Dander / Foods Y N Glands
Other:
Patient Signature Date
Reviewed with Patient____________ _____/_____/______
Drs Initials & Date
You might also like
- Primary Care Intake PaperworkDocument7 pagesPrimary Care Intake Paperworkasalizwa ludlalaNo ratings yet
- OB-GYN Intake Form New Patient InformationDocument6 pagesOB-GYN Intake Form New Patient InformationaltenereNo ratings yet
- UKOAA - Medical QuestionnaireDocument6 pagesUKOAA - Medical Questionnairemashangh50% (2)
- Medical HXDocument1 pageMedical HXapi-180434871No ratings yet
- 302 RUA - Interview WorksheetDocument4 pages302 RUA - Interview WorksheetChristy RobinettNo ratings yet
- Health History QuestionnaireDocument3 pagesHealth History QuestionnaireDaryl Adrian RecaidoNo ratings yet
- 2 CA - Health Profile - 2014-12-19 PDFDocument9 pages2 CA - Health Profile - 2014-12-19 PDFLiamNo ratings yet
- History Taking FormDocument9 pagesHistory Taking FormEren ErkılınçNo ratings yet
- Key Points of Obstetrics and Gynaecological HistoryDocument44 pagesKey Points of Obstetrics and Gynaecological HistoryRoisah Yunan NegariNo ratings yet
- Fit To Work Certificate DocxDocument3 pagesFit To Work Certificate DocxBlood ViernesNo ratings yet
- Base Line Health Assessment For PrintedDocument3 pagesBase Line Health Assessment For Printedferry7765No ratings yet
- Prenatal Questionnaire: General InformationDocument6 pagesPrenatal Questionnaire: General InformationChristine HernandezNo ratings yet
- Health Assessment FormDocument8 pagesHealth Assessment FormIrina Chpitalnik100% (1)
- Medical HistoryDocument1 pageMedical HistoryEmily KirbyNo ratings yet
- PTPT Patient Health InformationDocument1 pagePTPT Patient Health InformationRachael DavisNo ratings yet
- Colon and Rectal Surgery New PatientsDocument4 pagesColon and Rectal Surgery New PatientsTalha WaheedNo ratings yet
- 1.annual Physical Therapy Visit For Aging Adult-Intake FormDocument5 pages1.annual Physical Therapy Visit For Aging Adult-Intake FormReza ANo ratings yet
- Student Health Form: General InformationDocument1 pageStudent Health Form: General Informationreza329329No ratings yet
- Client Health HistoryDocument22 pagesClient Health HistoryAudrygodwynNo ratings yet
- Pat FundamentalsDocument14 pagesPat Fundamentalsapi-281676750No ratings yet
- History Obstetrics 3Document15 pagesHistory Obstetrics 3VICTOR OLUWAKEYENo ratings yet
- New PT PacketDocument11 pagesNew PT PacketKrishnaSomayajulaNo ratings yet
- Antenatal Case SheetDocument4 pagesAntenatal Case SheetRia SinghNo ratings yet
- Adult Med HXDocument2 pagesAdult Med HXapi-3868874No ratings yet
- FINAL Cervical CADocument14 pagesFINAL Cervical CAroselo alagaseNo ratings yet
- BokSmart - General Medical AssessmentDocument12 pagesBokSmart - General Medical AssessmentDirko SmutsNo ratings yet
- Patient Profile AdultDocument2 pagesPatient Profile AdultBrandon HubbardNo ratings yet
- Approved - CE Preop Questionnaire-1Document0 pagesApproved - CE Preop Questionnaire-1Cristina TarcatuNo ratings yet
- Case Record FormDocument30 pagesCase Record FormVirag Patil100% (1)
- Gastrointestinal History - VomitingDocument2 pagesGastrointestinal History - VomitingAmjad_2020No ratings yet
- Ob History Form PDFDocument2 pagesOb History Form PDFRoan Marie JumaquioNo ratings yet
- Examination of Peripheral Vascular DiseaseDocument6 pagesExamination of Peripheral Vascular DiseaseManas RanjanNo ratings yet
- Adult Communication Case HistoryDocument2 pagesAdult Communication Case HistoryHarshit AmbeshNo ratings yet
- Patient History Form: Last First M. IDocument4 pagesPatient History Form: Last First M. IMukundan SubramanianNo ratings yet
- Clinical Nutrition IntakeDocument6 pagesClinical Nutrition IntakeAudrygodwynNo ratings yet
- 32-Week OB CheckDocument4 pages32-Week OB CheckG. Crusor-PriceNo ratings yet
- Pat Revised 2013 1Document18 pagesPat Revised 2013 1api-324886317No ratings yet
- Medical History FormDocument2 pagesMedical History Formapi-279870303No ratings yet
- Hijama Consultation FormDocument2 pagesHijama Consultation Formdentistsaif100% (1)
- FNP 1 InfertilityDocument32 pagesFNP 1 Infertilityapi-555392359No ratings yet
- Portfolio Pat 3Document19 pagesPortfolio Pat 3api-300861055No ratings yet
- PPGMedical History FormDocument2 pagesPPGMedical History Formmb344617No ratings yet
- NutritionalTherapy QuestionnaireDocument13 pagesNutritionalTherapy Questionnairehalima mainaNo ratings yet
- Brightstone Transitions Medical HistoryDocument5 pagesBrightstone Transitions Medical HistoryRidhwan Hakim ZainurinNo ratings yet
- Self Declaration Medical Fitness FormDocument1 pageSelf Declaration Medical Fitness FormGorav BhallaNo ratings yet
- Menopause Health QuestionnaireDocument8 pagesMenopause Health QuestionnaireFatma Risda HidayantiNo ratings yet
- Final Nursing Care PlanDocument12 pagesFinal Nursing Care PlanBerina SelimovicNo ratings yet
- New Patient History FormDocument6 pagesNew Patient History Formعبدالله الكافNo ratings yet
- Obstetric and Clinical Medicine - Gynaecological History and ExaminationDocument7 pagesObstetric and Clinical Medicine - Gynaecological History and ExaminationShahin Kazemzadeh100% (1)
- $egrpl QDO SDL Q: &RQVL Ghudw L RQVDocument4 pages$egrpl QDO SDL Q: &RQVL Ghudw L RQVjegan555No ratings yet
- Medical Certificate (To Be Filled by Registered Doctor Only)Document2 pagesMedical Certificate (To Be Filled by Registered Doctor Only)nikhilviruNo ratings yet
- Antenatal Assessment ToolDocument16 pagesAntenatal Assessment Toolpandem soniyaNo ratings yet
- Sem 4 OBGYNPresentationDocument16 pagesSem 4 OBGYNPresentationAdamNo ratings yet
- Newpatient FormsDocument2 pagesNewpatient Formsapi-239262305No ratings yet
- Holistic Approach to Health CareDocument13 pagesHolistic Approach to Health CareRebecca KnightNo ratings yet
- Physician'S School Entrance Examination: ImmunizationsDocument2 pagesPhysician'S School Entrance Examination: ImmunizationsBianca ChanNo ratings yet
- Health HistoryDocument8 pagesHealth HistoryQurrat Ul Ain FaizanNo ratings yet
- Personal Trainer Consultation FormDocument3 pagesPersonal Trainer Consultation Formsamssgrr1100% (4)
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicFrom EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicRating: 5 out of 5 stars5/5 (1)
- Urmium Eng - 1 - CTYDocument50 pagesUrmium Eng - 1 - CTYnguyenthequang03No ratings yet
- CHAPTER 8 - Abnormal Uterine BleedingDocument42 pagesCHAPTER 8 - Abnormal Uterine BleedingJesselyn ReginaNo ratings yet
- Close Relations An Introduction To The Sociology of Families 6th Edition Mcdaniel Test BankDocument36 pagesClose Relations An Introduction To The Sociology of Families 6th Edition Mcdaniel Test Bankbedwarfratitemmg4100% (27)
- Jurnal The Heart and Cardiovascular System in The Qur'An and HadeethDocument19 pagesJurnal The Heart and Cardiovascular System in The Qur'An and HadeethWidya Derattano Pikal LimNo ratings yet
- Lec. 3 - Abnormal Uterine BleedingDocument14 pagesLec. 3 - Abnormal Uterine BleedingDr-Saja O. DmourNo ratings yet
- Endometrial Cytology OriginalDocument37 pagesEndometrial Cytology Originalreuben kwotaNo ratings yet
- Your Health - 6 August 2019Document8 pagesYour Health - 6 August 2019Times MediaNo ratings yet
- Mid-Semester Test English in Nursing - Dysfunctional of Menstrual Cycle (Menorrhagia, Metrorrhagia, Meno-Metrorrhagia) - 190411Document5 pagesMid-Semester Test English in Nursing - Dysfunctional of Menstrual Cycle (Menorrhagia, Metrorrhagia, Meno-Metrorrhagia) - 190411Chalida HayulaniNo ratings yet
- Antenatal AssessmentDocument24 pagesAntenatal AssessmentIshrat PatelNo ratings yet
- Sarcodes from body parts and glandsDocument6 pagesSarcodes from body parts and glandsnitkolNo ratings yet
- Meditation and yoga relieve dysmenorrhea and absenteeismDocument6 pagesMeditation and yoga relieve dysmenorrhea and absenteeismrifdaNo ratings yet
- Case Scenario For Group 2Document8 pagesCase Scenario For Group 2nikki sabsNo ratings yet
- Anaemia in PregnancyDocument81 pagesAnaemia in PregnancyEmmanuel Kings100% (3)
- Pushyanuga ChurnaDocument3 pagesPushyanuga Churnaarjun_chip_cNo ratings yet
- Ginekologi UKDI MANTAP Batch NovemberDocument156 pagesGinekologi UKDI MANTAP Batch NovemberIsmail Eko SaputraNo ratings yet
- Fetal Growth and Development During PregnancyDocument13 pagesFetal Growth and Development During PregnancyJamica Anne Rias CostinianoNo ratings yet
- Health Education on DysmenorrheaDocument18 pagesHealth Education on DysmenorrheaSheyma HaraniNo ratings yet
- Last Hour Review 2020 by Mci Gurukul DR Bhuoendra Armaan Chourasiya PDFDocument49 pagesLast Hour Review 2020 by Mci Gurukul DR Bhuoendra Armaan Chourasiya PDFadiNo ratings yet
- ICD-10 Common Codes: Diagnostic ServicesDocument6 pagesICD-10 Common Codes: Diagnostic ServicesAnasNo ratings yet
- Block W POP Case ProtocolDocument7 pagesBlock W POP Case ProtocoltabatchNo ratings yet
- TCM Patent-Study Guide - FinalDocument9 pagesTCM Patent-Study Guide - FinalpranajiNo ratings yet
- Answers On Issues of Menstruation (Shafi'i)Document9 pagesAnswers On Issues of Menstruation (Shafi'i)talibabdiNo ratings yet
- Manual Planejamento Familiar PDFDocument388 pagesManual Planejamento Familiar PDFTiago De Braga SoaresNo ratings yet
- Menstrual Disorder PDFDocument23 pagesMenstrual Disorder PDFAndalisNo ratings yet
- Nursing Interview Guide - HADocument6 pagesNursing Interview Guide - HAJohn CenaNo ratings yet
- ONE POINT ACUPRESSURE TREATMENT - TCM Part 1 PDFDocument75 pagesONE POINT ACUPRESSURE TREATMENT - TCM Part 1 PDFshamim hijama83% (6)
- Studies in The Psychology of Sex, Volume 1Document196 pagesStudies in The Psychology of Sex, Volume 1Ana28No ratings yet
- Opening the Third Eye - Understanding the Power of the Pineal and Pituitary GlandsDocument7 pagesOpening the Third Eye - Understanding the Power of the Pineal and Pituitary GlandsJay-King Tut Guy100% (2)
- Your Health HistoryDocument19 pagesYour Health Historyjasoneinstein100% (1)
- Al-Murshid Al-Mu'in - Translation & Commentary On Selected SectionsDocument52 pagesAl-Murshid Al-Mu'in - Translation & Commentary On Selected SectionsSaíd Allan Bak100% (1)