Professional Documents
Culture Documents
Neurobiology of Stress
Uploaded by
Diana ArleneCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neurobiology of Stress
Uploaded by
Diana ArleneCopyright:
Available Formats
The neurobiology of stress and its relevance to psychotherapy
Philip W. Gold
*
Clinical Neuroendocrinology Branch, DIRP, NIMH, Building 10, RM. 2D46, 10 Denter Drive, Bethesda, MD 10892-1284, USA
Abstract
Stress precipitates depression and signicantly inuences its course and severity. The neurobiology and clinical manifestation of the stress
response and depression are similar, but in depression, the features persist and override the usual counter-regulating forces. Both the stress
response and depression are characterized by hyperarousal, anxiety, increased expectation of harm, xation of mood, and a bias towards well-
rehearsed, relatively automatic cognitive programs. Furthermore, each is associated with preferential access to negatively charged emotional
memories that emerge unconsciously, usually without identiable cognitive content. The same stress-responsive CNS mediators that produce
emotional, cognitive, and behavioral manifestations also lead to inhibition of endocrine programs for growth and reproduction to preserve
energy, a catabolic state toprovide glucose to the brain, and increased heart rate and blood pressure. While these phenomena are transient during
stress, they may become chronic in depression, overriding their usual counter-regulatory inuences. These biological phenomena constitute the
basis for the now well-documented fact that depression is associated with a doubling of mortality at any age, independent of smoking, other
physical risk factors, and suicide. Thus, depression is not only a state of anguish, but also the tip of the iceberg of a systemic disorder that leads to
illness and signicantly shortens life. Psychotherapy plays an enormously critical role in the treatment of any depression. The intersection of
stressful, disturbing life experiences encoded in emotional memory, as well as genetic vulnerability provide the context for understanding how
psychotherapeutic intervention can inuence a disorder with biological vulnerability that is responsive to somatic treatments. Indeed, current
well-controlled data indicate that pharmacological intervention is signicantly more effective when combined with psychotherapy. Otherwise,
unfortunate circumstances during childhood or later, persistent maladaptive behavioral patterns that increase the likelihood of stressful events,
and a massive, untouched burden of aversively charged memories cam overwhelm skillful psychopharmacologic intervention.
q2005 Published by Elsevier B.V. on behalf of Association for Research in Nervous and Mental Disease.
Keywords: Major depression; Melancholic depression; Atypical depression; Stress; Psychotherapy
1. Introduction
Major depression is a heritable disorder that affects
approximately 8% of men and 15% of women in the course
of their lifetime [36,61,18]. For over 75% of patients,
major depression is a recurrent illness, characterized by
repeated remissions and exacerbations [18]. Over 50% of
patients who recover from a rst depressive episode will
have a second within 6 months unless they are given
maintenance antidepressant treatment [17]. For those who
never receive treatment, as many as 15% will succumb to
suicide [29].
Depression not only causes great mental anguish but also
intrudes upon fundamental biological processes that
regulate sleep, appetite, metabolic activity, autonomic
function, and neuroendocrine regulation (reviewed in
Refs. [25,27,22]). These disturbances are likely to contrib-
ute to the premature coronary artery disease, premature
osteoporosis and the doubling of mortality in patients with
major depression at any age independent of suicide,
smoking, or signicant physical illness [2,6,56,51,52]. In
taking into account the natural history, mental suffering, and
medical morbidity associated with major depression, the
World Health Organization ranked this disorder as the
fourth leading cause of disability worldwide [13].
Major depression and the stress response share many
mediators, circuitries, and phenomenologies. Stress precipi-
tates major depression [37] and inuences its, severity,
duration, and natural history [32,35]. Depressive illness, like
stress system activation share a relatively unshifting affect,
a shift from complex modes of thought to those that are
relatively well-rehearsed or reexive, and a dysregulation of
Clinical Neuroscience Research 4 (2005) 315324
www.elsevier.com/locate/clires
1566-2772/$ - see front matter q 2005 Published by Elsevier B.V. on behalf of Association for Research in Nervous and Mental Disease.
doi:10.1016/j.cnr.2005.03.006
* Corresponding author. Tel.: C1 301 496 1945; fax: C1 301 402 1561.
E-mail address: philipgold@mail.nih.gov.
fundamental biological processes that regulate sleep,
appetite, growth, reproduction, and autonomic function
[38,39,18].
2. Depression as a complex disorder of adaptation
Two-thousand and ve hundred years ago, Hippocrates
advanced the principle that we are continually beset by
disturbing forces that threaten to upset the interior balance
upon which our lives depend. Fortunately, he noted, there
are counteracting forces that oppose the disturbing forces
and work to maintain or restore homeostasis. Galen called
these Vis Medicatrix Naturae, the healing forces of nature.
For the purpose of this overview, we shall call the disturbing
forces stressors, the balance, homeostasis, and the counter-
acting forces, adaptive responses. According to this schema,
we can dene stress as an ongoing or perceived state of
threatened homeostasis.
We have subsequently learned that the adaptive forces
themselves can become disturbing forces or stressors that
threaten homeostasis. Autoimmune disorders are perhaps
the most thoroughly elucidated. We need our immune
system to survive a myriad of disturbing forces, and it is
among our most critical of our adaptive responses.
However, the survival value of the immune response can
be circumvented by a dysregulalation of the immune
adaptive response that becomes either hyperactive or
inappropriately directed at the self. Major depression is
also a disorder of adaptation, and can be conceived, in part,
as a dysregulation of the stress response. For humans, this
dysregulation involves a perception of the world that
provokes fear and dread of the future, and a perception of
self that is full of anxiety and dissatisfaction. Thus,
depression can also be considered a disorder of the self.
Disorders of the immune system occur in the context of
multiple predisposing genes and a predisposing environ-
ment. For autoimmune disease, the predisposing environ-
ment is one that contains a specic inciting antigen or
repertoire of antigens that either provokes an excessive or
self-directed immune response. For depression, the predis-
posing factors include the burdens of internal and external
conicts, and the sum and intensity of stored aversively
charged emotional memories of abandonment, unkind
treatment, or abuse.
It is well documented that disturbing events at critical
periods early in life are particularly well encoded in
emotional memory, and alter the physiology and phenom-
enology of the stress response and of self-perception for the
rest of the individuals life. Indeed, in experimental animals,
early stress such as relatively short maternal separation turns
up the intensity of the stress response for the remainder of
the organisms life. Conversely, early gentle handling and
lack of interference with the maternal-offspring bond are
associated with a relatively restrained stress response
throughout life [45,60].
The intersection of stressful, disturbing life experiences
encoded in emotional memory, as well as genetic vulner-
ability [34] provide the context for understanding how
psychotherapeutic intervention can inuence a disorder with
biological vulnerability that is responsive to somatic
treatments.
2.1. Two depressive phenotypes
While there are many forms of depression, this report
will focus on two major subtypes that are delineated by the
DSM-IV, melancholic and atypical depression [1,16].
Melancholic depression belies the term depression in that
is a state of pathological hyper-arousal and anxiety, most
notably, about the self. Melancholic depression cruelly
prevents the taking of pleasure in what one has achieved or
become, pleasures in everyday life, and hopes for the future.
Melancholic depression can, thus, be seen as a state of
organized anxiety and anguish that has inltrated the entire
cycle of life, past, present, and future (reviewed in Refs.
[24,25]). It seems, at times, that patients with melancholic
depression are dominated by a preferential access to
negatively charged emotional memories without recall of
explicit content.
Patients with melancholic depression also manifest
evidence of physiological hyperarousal such as hypercorti-
solism, suppression of the growth hormone and reproduc-
tive axes, insomnia (most often early morning awakening),
loss of appetite, and loss of interest in sexual activity.
Another consistent feature of melancholia is a diurnal
variation in the severity of depressed mood, which is
greatest early in the morning 1994.
Although both atypical and melancholic depression are
associated with dysphoria and anhedonia, atypical
depression is in many ways the antithesis of melancholia.
Atypical depression is associated with a disturbing sense of
disconnectedness and emptiness, punctuated by brief
emotional reactions to external circumstances [16]. In
contrast to melancholics, who seem to have ready access
to negatively charged memories, patients with atypical
depression often seem walled off from themselves. They
may complain of a cognitive and mental weariness and
avoid others, often with the sense that contact would be too
demanding, tiring, and poorly received. Neurovegetative
symptoms in atypical depression are the reverse of those in
melancholia and consist of lethargy, fatigue, excessive
sleepiness, increased food intake, weight gain, and depress-
ive symptoms that worsen as the day progresses.
Only 2530% of patients with major depression present
with pure melancholic features while another 1530%
present with pure atypical features [41]. Those with
melancholic or atypical features show a much more severe
course of illness than those with mixed neurovegetative
features. Recent data from identical twin and family studies
indicate that melancholic and atypical features are each
heritable entities [33]. However, only a few studies of
P.W. Gold / Clinical Neuroscience Research 4 (2005) 315324 316
depression have stratied patients on the basis of clinical
subtype.
2.1.1. Melancholic depression versus grief
Although grief can be confused with melancholic
depression, grief is generally a much more complex and
nuanced state. In the midst of grieving we can contemplate
what we valued most in the one we lost, and celebrate what
we brought to them when they were alive. We also have the
exibility to recall happy as well as sad memories and to
reect on conicts without devaluing the other or ourselves.
The options are far more limited in melancholic depression.
When negatively charged memories emerge, they are
accompanied by the conviction that an unsatisfactory
event or outcome was of our own doing. If anger emerges,
it is almost always at the self. The past is robbed of its many
textures, and the future looks only like an indenite
extension of what has gone before.
In the following sections, I will rst briey describe some
of the circuitry sand mediators of the stress system and then
provide a stress system-related formulation of the action of
psychotropic agents.
3. The stress response
The stress response consists of a series of coordinated
behavioral and physiological manifestations that promote
survival. Anxiety is a foremost component. The brain has
evolved an abundant circuitry for generating anxiety and for
the conscious experience of fear [38]. Anxiety and fear-
related phenomena have been carefully selected to promote
survival during life threatening situations, and these remain
well remembered in the amygdala and emerge reexively
during threatening situations (including social stress) [40].
There is also an intense focus on the dangerous threat at the
expense of attending to other elements of the environment.
Cognitive programs shift from those that are complex,
sequence dependent, and integrative to those that are well-
rehearsed, acquired during previous bouts with danger, and
encoded to readily emerge in subsequent life-threatening
situations [20,38,39].
At the same time, a variety of physiological adaptations
simultaneously occur, many driven by the same neuro-
transmitters and circuits that are involved in the cognitive
and affective changes that characterize the response to
threatening situations. There is activation of the sympathetic
nervous system with an attendant increase in blood pressure,
pulse rate, and cardiac output. An inhibition of vegetative
functions such as food intake and sleep occurs because these
would be very maladaptive during a life-threatening
situation. Moreover, metabolic changes occur to provide
fuel for the brain. These consist of hypothalamicpituitary
adrenal activation and glucocorticoid-mediated breakdown
of fat, muscle, and bone and their ultimate transformation
into glucose, as well as insulin resistance for the
mobilization of glucose. We now know that there is a
priming of the immune system in case of an ensuing injury,
promoting a mild proinammatory state, and a priming of
the coagulation system as a defense against hemorrhage.
When these occur in an accentuated and prolonged stress
response characteristic of major depression, various somatic
manifestations and early mortality are the result [22].
In short: if you are a rat being chased by a cat, you will be
very anxious, have fear-related behaviors, and a strict focus
on the dangerous threat. Your cognitive functions will bias
towards well-rehearsed, simple, virtually reexive ones
rather than complex, sequence dependent ones requiring
concentration. Your mood will be clamped rather than
exible to facilitate absolute focus on the life-threatening
stimulus.
You will also reexively recall previous emotional
memories that were acquired during your last encounter
with danger, to prepare you for the current crisis. You will
unconsciously set aside the propensity for complex
behavioral and cognitive programs that may require
concentration.
As a corollary, you will not stop to eat, will not stop for
sexual activity, will not rest or sleep, and, as before, will
encode information that might be relevant to a subsequent
encounter with danger that will emerge unconsciously in the
next life-threatening situation.
If you have melancholic depression, you are anxious,
especially about yourself, experienced a loss of self-esteem,
self-contempt, and guilt, have relatively stereotyped think-
ing, inexible affect, insomnia, decreased food intake,
disinterest in sexual activity, and will feel worst in the
morning. If you have an atypical depression, your stress
system may be shut off, and you overeat, oversleep, feel
lethargic, and complain of fatigue. While these are great
oversimplications, they provide a link between a dysregu-
lated stress system and the clinical and biochemical
manifestations of major depression.
3.1. Anatomy and neuromediators of the stress response
3.1.1. The prefrontal cortex
The prefrontal cortex accounts for approximately one-
third of human brain volume. In many respects the
prefrontal cortex exerts cognitive, behavioral, affective,
and physiological responses that are the virtual antithesis of
those set into motion during stress. At the same time, the
prefrontal cortex and the stress system inhibit each others
activity.
In many ways, areas of the prefrontal cortex act as a
restraint upon the stress system and transduce many key
cognitive and emotional processes that transpire only in the
context of relative freedom from an acutely threatening
situation.
The prefrontal cortex is the area of the brain that
determines whether the individual is likely to experience
punishment or reward, and the extent to which a realistic
P.W. Gold / Clinical Neuroscience Research 4 (2005) 315324 317
assessment has been rendered about an accomplishment or
relationship [20].
The prefrontal cortex is also actively involved in
restraining the amygdala fear system [47], and, among
other tasks, promotes the extinction of aversively charged
emotional memories [43]. Medial prefrontal cortex-restraint
of the amygdala fear system and its opposition to the process
of conditioned fear are two of the functions of the prefrontal
cortex that are important in opposition to depressive illness.
[47,43,4].
The prefrontal cortex arbitrates the bias towards two
cognitive domains, and as noted, determines the extent to
which complex, newly synthesized, novel programs pre-
dominate versus the extent to which these are suspended in
favor of relatively reexive responses that generically offer
protection against threatening stimuli. An activated pre-
frontal cortex promotes complex cognitive programs and
inhibits those that are more reexive [19]. The prefrontal
cortex is also essential for the shift of one affective state to
another [20,53]. This is adaptive during a dangerous
situation, in which affect should be clamped in a fearful
mode rather than have the capacity to range broadly to
stimuli that may be distracting.
One area of the prefrontal cortex, the subgenual
prefrontal cortex, subserves or inuences many of the
processes noted above. In addition, the subgenual prefrontal
cortex provides cortical restraint upon the hypothalamic
pituitaryadrenal axis and the sympathetic nervous system.
[47,15]. The prefrontal cortex is the only cortical brain
structure that sends direct connections to the hypothalamus
and to brainstem norepinephrine neurons.
3.2. The amygdala fear system
Because fear is essential for surviving serious threats, the
stress system must be capable of producing the experience
of being afraid. The amygdala is a key structure that
transforms experiences into feeling [39]. To accomplish this
task, the amygdala provides working memory with further
information about whether something is good or bad and
activates disparate arousal centers to maintain focus upon
the current danger. The amygdala evolved relatively early
compared to higher cortical centers.
The amygdala is responsible for acquiring and storing
classic fear conditioned responses that can be immediately
mobilized even though they remain outside of conscious
awareness Because the amygdala cannot store complex,
explicit aversively charged emotional memories, it relays
them to areas such as the hippocampus and striatum for
retrieval during subsequent emergencies
The amygdala is a key structure for receiving and either
encoding or transmitting neural information regarding
aversively charged emotional memories [44,10]. Emotional
memories are very well remembered. They are stored in
sites distinct from those that store and transmit knowledge
regarding everyday functioning in a material world such as
spatial memory [50]; Cahill, 1998 #13; [11], and other
forms of non-emotionally laden memories [63].
The distinct loci for explicit and emotional memory [63]
are demonstrated by the phenomenon in which individuals
with damage to explicit, fact-laden memories but intact sites
for emotional memories respond to someone who had
frightened them by crying out, without recognizing the
person or the context in which they were frightened. They
say, instead, that they have no idea why they became
frightened, but only that they are frightened without
apparent cause. This emergence of an unconscious
emotional memory without apparent content occurs fre-
quently in everyday life and in patients under treatment for
depression. Thus, in response to a situation resembling that
explicit event or place in which the upsetting experience
occurred, an emotional response can occur in the absence of
a conscious awareness of the context in which it was
acquired [20,38,39,11]. As noted later, the imprinting of
emotional memory is greatly strengthened by the classic
hormones secreted during stress. This make sense because it
is adaptive to increase the strength of an emotional
memorys encoding so that it can emerge unconsciously
to signal an individual that danger is imminent, including
not only physical danger, but the danger of abandonment,
loss, or humiliation.
The corticotropin releasing hormone and locus ceruleus-
norepinephrine systems; physiological components of the
stress response that also activate the amygdala and inhibit
the prefrontal cortex.
Two principal physiological components of the stress
system are the CRH-HPA axis and Locus-Ceruleus
Norepinephrine Systems. In addition to exerting important
physiologic effects and inuencing the repertoire of
vegetative functions, they also exert behavioral effects on
their own and inuence the amygdala fear system and the
activity of the prefrontal cortex.
3.3. The corticotropin releasing hormone (CRH) and
hypothalamicpituitaryadrenal (HPA) axis
CRH was rst isolated and identied as the principal
hypothalamic hormone that releases corticotropin (ACTH),
which in turn activates adrenocorticosteroid secretion [57]
Over the years, a series of painstaking studies in rodents has
established roles for CRH in the stress response other that of
HPA axis regulation. These include activation of the
amygdala fear system, and thus anxiety and fear related
behavior. CRH also activates the HPA axis, the locus
ceruleus [58], the sympathetic nervous system [9], and the
adrenal medulla. Finally, CRH participates in the inhibition
of a variety of neurovegetative functions such as food
intake, sexual activity, and the endocrine programs for
growth and reproduction. Taken together, CRH in the rat
participates in virtually the entire cascade of the physiologic
and behavioral alterations occurring in response to stressors.
P.W. Gold / Clinical Neuroscience Research 4 (2005) 315324 318
CRH not only transduces these effects in rodents, but also in
primates [30].
We have recently shown in rhesus macaques that the oral
administration of a non-peptide CRH type 1 receptor
antagonist (antalarmin) that penetrates the blood brain
barrier signicantly inhibited stress-induced anxiety-like
responses while promoting exploration [30]. We also found
that antalarmin signicantly inhibited increases in plasma
ACTH, NE, epinephrine and cortisol [30]. Thus, these data
indicate that CRH plays a tonic role in the comprehensive
modulation of the stress response not only in rodents, but in
primates as well.
3.3.1. Cortisol
The hypothalamicpituitaryadrenal axis, along with
norepinephrine, is among the most frequently studied
mediators in all of psychiatric research. For many years,
investigators have known that cortisol is elevated in some
depressed patients. Efforts to utilize cortisol secretion as a
marker for certain forms of major depression have been
unsuccessful. However, cortisol hypersecretion is an
extremely important phenomenon in major depression and
is involved in many of the long-term medical consequences
of major depression, covered later in this review.
Cortisol is secreted by the adrenal cortex during stress,
and, as noted, contributes to the mobilization of glucose for
the brain during stress by its catabolic actions of breaking
down muscle, bone, and other tissues. Cortisol is also
essential for effective cardiovascular adaptation during
stress. The secretion of cortisol by the adrenal glands is
regulated by the brain. During stress, CRH [57] is released
from the hypothalamus and travels to the pituitary to
stimulate ACTH release into the bloodstream. ACTH, in
turn, stimulates the adrenal glands to produce cortisol.
For the most part, the adaptive advantages conferred by
cortisol secretion during stress are limited to its acute rather
than chronic release. Acute cortisol release coordinates
processes that occur during stress, especially mobilization
of fuel and increased cardiac contractility. Chronic cortisol
excess is almost always deleterious and includes excessive
fear, insulin resistance/visceral fat deposition and their
many pro-atherogenic sequella, pathologic loss of bone and
muscle, inhibition of cellular immunity, and suppression of
the brain center that plays an important role in mediating
reward and pleasure (reviewed in Ref. [22]).
Glucocorticoid receptors are widely distributed in brain.
Acutely, activation of glucocorticoid receptors located in
the prefrontal cortex, hippocampus, amygdala, and the
hypothalamus, inhibit the HPA axis. McEwen, Sapolsky,
and their colleagues found that chronic activation of
glucocorticoid receptors located in the hippocampus could
damage hippocampal neurons containing glucocorticoid
receptors, potentially leading to more severe hypercortiso-
lism [55]. Not all glucocorticoid receptors transduce
inhibitory effects. We found that activation of glucocorti-
coid receptors located in the central nucleus of the amygdala
and the bed nucleus of the stria terminalis increase rather
than decrease compounds that cause amygdala mediated
anxiety and fear related behaviors [42]. Another roles of
cortisol secretion during stress is to strengthen the encoding
of aversively charged emotional memory and to enhance its
unconscious retrieval [54]. Thus, cortisol secretion actually
directly enhances amygdala activity.
Depression is by no means the only illness that is
characterized by hypercortisolism. Hypercortisolism is the
primary manifestation of patients with Cushings disease. In
fact, severe hypercortisolism in major depression is virtually
impossible to distinguish from the very high cortisol levels
characteristic of Cushings Disease. We developed a test
that is used in clinical medicine as the standard means of
distinguishing this differential diagnosis [28]. We also
showed that the hypercortisolism of anorexia nervosa is
caused by the hypersecretion of CRH. In this case the stress
is not strictly psychological stress, but because of the stress
of not eating and being severely underweight to the point of
cachexia [26].
3.4. The locus ceruleus-norepinephrine system
The LC-NE system resides in brain stem and contains the
highest concentration of noradrenergic cell bodies in the
brain. A single LC neuron can have as many as 100,000
nerve terminals and can innervate cells in several different
portions of the brain. In addition, activation of the LC
contributes to sympathetic nervous system and HPA axis
stimulation. At the same time, LC activation inhibits the
parasympathetic nervous system as well as neurovegetative
functions such as feeding and sleep (reviewed in Ref. [5]).
During stress, the LC enhances the role of the amygdala
and other structures involved in the encoding of aversively
charged memories. Thus, the LC not only promotes survival
during an acute crisis, but helps in preparing for subsequent
dangers as well. Arnsten et al. have recently found another
important role of the LC-NE during stress, namely
inhibition of the prefrontal cortex [3], thereby favoring
rapid instinctual responses over more complex ones in the
service of surviving acute life-threatening situations Taken
together, the LC, like the CRH system, plays a role in
promoting arousal, inhibiting several vegetative functions,
and biasing towards a loss of affective and cognitive
exibility.
4. Studies of the role of stress system dysregulation
in patients with major depression
4.1. Neuroimaging: prefrontal cortex and amygdala
Many studies have revealed abnormalities in multiple
CNS sites in patients with depression. The most notable
revealed a signicant loss of volume in the left subgenual
prefrontal cortex. This area participates in the assessment of
P.W. Gold / Clinical Neuroscience Research 4 (2005) 315324 319
whether to expect punishment or reward, and assessment of
whether a task has gone well or not [20,39]. The subgenual
prefrontal cortex is closely connected to the amygdala and
participates in the extinction of conditioned fear responses
[47]. The subgenual prefrontal cortex is also the primary site
for cortical projections to the hypothalamus and noradren-
ergic brain stem nuclei. These projections represent the
principal means for cortical restraint of the hypothalamic
pituitaryadrenal axis and the sympathetic nervous system.
One of the most important ndings in recent times is that
of Drevets et al. who showed that the size and metabolic
activity of the subgenual prefrontal cortex was signicantly
reduced in depression [15]. This would have the following
effects: increased anticipation of harm; decreased regard for
oneself and what one has accomplished; disinhibiton of the
amygdala and increased anxiety and fear; disinhibiton of
the CRH and the LC-NE systems; reinforcing all of the
processes noted above, reminiscent of the clinical picture of
melancholia; and participating in the setting into motion of
somatic consequences of major depression such as inhi-
bition of growth and reproduction, a catabolic state, and
increased heart rate and blood pressure.
It is, therefore, not unexpected that patients with major
depression also had signicant increases in the metabolic
activity of the amygdala. This nding is entirely compatible
with the nding of loss of volume of the subgenual
prefrontal cortex. In addition, because the amygdala
activates the HPA axis and the sympathetic nervous system,
this nding compounds the loss of inhibition of these
systems that is secondary to the loss of prefrontal cortex-
inhibition.
4.1.1. CRH system
The hypercortisolism of depression is one of the most
frequent ndings in biological psychiatry, though many
papers cited normal cortisol levels as well. Utilizing the
CRH stimulation test, we rst advanced evidence that
hypothalamic CRH was elevated in depression [23]. Shortly
thereafter, Nemeroff found that CSF CRH levels in
depressed patients were elevated [49] and later showed
that CSF CRH levels in patients fell signicantly after
treatment. Nemeroff et al. also found that CRH receptor
numbers were reduced in frontal cortex in post mortem
samples taken from patients who had suicided [48]. These
data suggest down-regulation of CRH receptor numbers
because of chronic hyperstimulation by CRH. Character-
istically, hypersecretion of a compound results in the down-
regulation, or decease in number of receptors. Later,
Holsboer replicated the work of Gold et al. using the same
methodology [31]. DeBellis found that Prozac signicantly
lowered CSF CRH levels when depressions remitted. In
addition, we found that the chronic administration of
imipramine to healthy volunteers produced effects compa-
tible with a central down-regulation of the HPA axis and
CRH secretion (Michelson, 1997 #1957). CSF CRH.
Finally, in experimental animals, we showed that the
chronic, but not acute, administration of imipramine, Prozac,
and an MAO inhibitor signicantly reduced CRH levels [7].
4.1.2. The locus ceruleus-norepinephrine system
The original catecholamine hypothesis of major
depression stated that depression resulted from a deciency
of NE at critical synapses in the CNS. This hypothesis was
based on the assumptions that pharmacologic depletion of
NE by reserpine apparently induced major depression, while
apparent pharmacologic augmentation of noradrenergic
activity by MAO inhibitors and NE uptake inhibitors
(tricyclic antidepressants) exerted antidepressant effects.
By positing that depression could be caused by a deciency
of NE, the catecholamine hypothesis served as a major
impetus for the emergence of modern biological psychiatry.
However, as research became more sophisticated, it became
clear that early life stress profoundly increases the activity
of all stress components throughout the life of the individual
(vide infra). It is now unequivocal that environmental
factors are critical to the development of noradrenergic
abnormalities in depression
Although many forms of depression are clearly charac-
terized by a deciency of NE in the CNS, melancholic
depression is likely to be associated with increased
noradrenergic function in the CNS. Decreased exibility
of mood and cognition, hyperarousal, increased anxiety,
decreased feeding, and insomnia could all be driven by
norepinephrine excess. This is compatible with the effects of
NE in the CNS to inhibit the medial prefrontal cortex,
activate the amygdala, and activate the CRH-cortisol
system. We have shown that the secretion of cerebrospinal
uid NE is elevated around the clock in patients with
melancholic depression [62]. The levels rise throughout the
night, during sleep, and peak in the morning, the time when
patients with melancholic depression experience the most
intense depression. This is also the time of maximal
vulnerability to myocardial infarction, and may contribute
to the increased mortality and premature heart disease in
patients with major depression, to be covered below. Thus,
the CNS mediators that contribute to depression also
contribute to its long-term medical consequences, establish-
ing major depression as a serious systemic disease.
Recent data further support the presence of an activated
locus ceruleus-norepinephrine system in major depression.
SSRIs. tricyclic antidepressants, and MAO inhibitors all
decrease the ring rate of the locus ceruleus in freely
moving rats. We found that imipramine [8], Prozac [7], and
an MAO inhibitor [7] down-regulated the expression of the
rate-limiting enzyme in catecholamine synthesis in the locus
ceruleus.
4.2. Long-term medical consequences of melancholic
depression
Patients with major depression show a doubling of the
mortality rate at any age, independent of suicide and other
P.W. Gold / Clinical Neuroscience Research 4 (2005) 315324 320
risk factors for poor health [6]. Premature ischemic heart
disease is likely to play an important role, and the relative
risk for clinically signicant coronary artery disease in
patients with major depression is 2.0 or more in studies that
independently controlled for risk factors such as smoking
and hypertension [2,56,21]. Increased sympathetic outows
add to cardiac risk in several other ways. Norepinephrine is
well known to promote insulin resistance, left ventricular
hypertrophy and increases in myocyte growth, arteriolar and
ventricular remodeling, and increased blood volume and
viscosity. In addition, NE also activates platelets, releases
cytokines and is arrythmogenic.
We have also shown that as many as 25% of
premenopausal women (average age 41) with severe
affective disorder have pathologic loss of bone mineral
density, including frank osteoporosis [46]. Indeed, in this
sample of women with relatively severe depression, almost
15% had frank osteoporosis. It should be noted that these
patients were not at very high risk for fracture. Osteoporosis
is dened by the number of standard deviations below bone
mineral density of young, healthy women. Young women
have other factors that would protect them, including greater
and stronger muscle mass. However, there is no reason to
believe that these women will not continue to lose bone
mineral density at a faster rate than controls.
Many factors could contribute to this loss of bone
mineral density in women with past or current depression.
Hypercortisolism is an obvious potential cause. In patients
given glucocorticoids, maximal bone loss occurs at 34
months after treatment. Since depressed, hypercortisolemic
patients have glucocorticoid concentrations that are often
equivalent to a patient receiving 12 mg of prednisone for 4
months or longer, the loss of bone in hypercortisolemic
depressed patients can be quite severe. These data make a
clear plea for the early and effective treatment of
melancholic depression. In addition to hypercortisolism,
other factors could also contribute to bone mineral density
loss in women with depression, including suppression of the
growth hormone and gonadal axes. The hypersecretion of
NE in patients with melancholia could also contribute to
bone loss via activation of the secretion of IL-6, an
inammatory mediator that is a potent inducer of bone
loss. IL-6 hypersecretion in the face of falling estrogen
levels is primarily responsible for post-menopausal
osteoporosis.
4.2.1. Atypical depression
Rene Spitz and others made seminal observations
regarding developmental abnormalities that befell infants
placed in understaffed orphanages with a dearth of human
contact shortly after birth. For the rst 5 or 6 months, most
of the infants cried bitterly for hours until attended.
Subsequently, they withdrew and ceased crying altogether,
even if they were left alone or had gone without eating for
many hours. In addition, they lost apparent interest in the
environment around them. It was as if the trauma of their
early deprivation had led to a virtual shutdown of their
affective existence to protect them from unendurable pain.
Subsequent studies in non-human primates who were
abandoned or abused by their mothers reveal a similar
behavioral withdrawal in association with hypoactivity of
the HPA axis.
We rst hypothesized that the lethargy, fatigue, and
hypersomnia of atypical depression was associated with a
pathological reduction of stress system mediators [24,12,25].
This possibility was supported by the previously cited data in
experimental animals showing that lesions in a specic part of
the rat prefrontal cortexresultedinpathological suppressionof
CRH and LC-NE systems. Our data based on studies of
different components of the HPA axis in fatigue states such as
chronic fatigue syndrome and seasonal affective disorder
raises the possibility that the HPA axis is hypoactive in states
that resemble atypical depression, but by no means proves an
inactivation of stress system activity in patients with this
disorder [14,59].
5. Conclusion
An axiom regarding stress system activity: multiple
positive feedback loops sustain and augment stress system
activity, a process further augmented by signicant stressors
experienced early in life.
The schema provided here for the organization of the
stress response has embedded in it many positive, reciprocal
feedback loops. For example, the medial frontal cortex
restrains the amygdala. When its activity is diminished, the
amygdala is activated. An activated amygdala further
restrains the activity of the medical prefrontal cortex. The
medial prefrontal cortex restrains the sympathetic nervous
system and the HPA axis. When medial prefrontal cortex
activity is reduced, norepinephrine and cortisol secretion
increase. Norepinephrine and cortisol further reduce medial
prefrontal cortex activity, leading to further increases in the
secretion of norepinephrine and cortisol. Moreover, both
norepinephrine and cortisol activate the amygdala, which in
turn activates norepinephrine and cortisol secretion. Finally,
both norepinephrine and cortisol accentuate the strength
and persistence of aversively charged emotional memories
(Fig. 1).
As noted, the stress response is augmented throughout
life in individuals or experimental animals who experi-
ence excessive stress, trauma, and loss early in life. This
applies not only to the experience of excessive psycho-
logical stress early in life, but also to excessive physical
stress, such as prematurity. Premature infants experience
an excess of stress related metabolic and autonomic
activity for the rest of their lives. The purpose of this
critical period for setting the tone for the lifetime of
responses to stressful stimuli is unknown. Perhaps being
born into a stressful environment triggers the brain to
prepare for an excess of stressful situations throughout
P.W. Gold / Clinical Neuroscience Research 4 (2005) 315324 321
life. Parenthetically, preliminary data suggest that a
sequella of frequent and intense stress responses through-
out life causes a progressive increase in the magnitude of
the stress response to a given stimulus.
There are many analogies between this schema regarding
the organization of the stress system and clinical psychiatric
practice and theory. Certainly, early stress or trauma can
provoke a lifetime of augmented anxiety, a diathesis to
depression, and alterations in the capacity to trust, form
relationships, deal with loss, and stabilize self-esteem. Life
can become organized around defending against vulner-
abilities conferred by early loss and stress and reinforced
throughout life. Individuals with difculties in trusting
others, manifested by anxiety and dysphoria, often organize
an avoidant lifestyle that signicantly impoverishes their
lives. The impoverishment leads to further liabilities in
interpersonal relationships, withdrawal from many of the
gratifying experiences in life, and dysphoria or depression.
Dysphoria or depression further compromises the ability
to trust, bear loss, and experience pleasure. A series of
positively re-enforcing feedback loops is an emergent
phenomena on the basis of early life stress and repeated
stress responses and maladaptive defenses developed over
the lifespan. This vicious cycle is virtually impossible to
reverse in isolation. It requires highly skillful psychother-
apy, combined, when necessary, with effective psychophar-
macological treatment.
A maladaptive or unrealistic view of the world also
promotes a signicant diathesis towards a style of living and
relating that causes substantial stress responses throughout
life. Years ago, Roy Schaefer wrote a beautiful monograph
entitled the Psychoanalytic Vision of Reality. He wrote
about the liabilities of comic or romantic visions of life.
Comic visions expect everything to turn out all right, and
failure is therefore catastrophic. The romantic version is
predicated n the premise that a lifetime of heroic events is
not only possible, but necessary for solidifying ones
identity. Ironic and tragic views that promoted the capacity
Fig. 1. Schematic diagram of the interrelation of stress system mediators and circuitries in melancholic and atypical depression. (Middle) Normal. In the
absence of stressful stimuli, the stress system is not quiescent, but rather resides in a dynamic state of bidirectional interactions among stress mediators. Such a
homeostatic equilibrium can react exibly to a range of different stimuli that may preferentially affect one component over another. Available data in primates
suggest that under ordinary circumstances: (1) the prefrontal cortex inhibits the amygdala, HPA axis, and LC-NE system; (2) an activated amygdala inhibits the
prefrontal cortex and stimulates both the HPA axis and the LC-NE. In the reverse direction: (3) the LC-NE activates the amygdala and HPA axis and inhibits
the prefrontal cortex; (4) the HPA axis activates the amygdala and HPA axis and inhibits the prefrontal cortex; (4) the HPA axis activates the LC-NE and the
amygdala. Dotted lines inhibitory, solid lines excitatory. Schematically, in the normal state, the relative strength of each component is similar, denoted by
circles of identical diameter. (Left) Melancholic depression can be conceptualized as a prolonged and intensied stress response that does not yield to its
ordinary counter-regulatory restraints. The net effect is a pronounced shift in equilibrium with the following results: (1) diminished activity of the prefrontal
cortex; (2) activation of the amygdala; (3) activation of the core stress system. The primary defect could arise from any of the structures pictured in the
schematic diagram or circuits in which they participate. Note reciprocal relation between prefrontal cortex and subcortial stress components. Also note that the
amygdala, LC, and CRH system are all excitatory to one anther so that an increase in the activation of one component could set off a reverberate sequence of
further activations unless overtaken by inhibitory stimuli. Similarly, the prefrontal cortex and the components of the stress system exhibit bi-directional
inhibition on one another. (Right) Atypical depression can be conceptualized as a state of stress system hypoactivity that has yielded too readily to its counter-
regulatory restraints. The net effect is a pronounced shift in equilibrium with hypoactivity of each of the components of the stress system. Theoretically, the
prefrontal cortex could be disinhibited or primarily hyperactive. Abbreviations: PFC, prefrontal cortex; AMYG, amygdala.
P.W. Gold / Clinical Neuroscience Research 4 (2005) 315324 322
to interpret reality with greater acuity and to deal with
intense sadness or loss without a catastrophic loss of self-
esteem were essential. For example, individuals with these
views understood that in every loss there may be growth,
and that in every success something is lost. The shift to such
a view of the world that can occur implicitly in a skillful
psychotherapeutic setting can signicantly reduce the stress
and strain of everyday living. As a consequence, vicious
positive feedback loops in the physiologic organization of
the stress response can be minimized. The result is a better
control of fear and anxiety, especially less anxiety about the
self, experienced as self-deprecation, increases in cognitive
and affective stability in the face of loss, and, enhanced
capacity to trust and relate.
In summary, the physiology of the stress response
shares many features that skillful therapists observe in the
lives of their patients as they organize their lives around
avoiding scenarios, which they nd almost unendurably
painful. Both the physiology and the behavior, without
intervention, tend to spiral downward. Activation of the
physiological stress response interferes with growth and
development by imposing an ever-increasing burden of
anxiety, fear, and preferential access to negatively charged
emotional memory. Stabilizing the stress system, a
process that is facilitated by psychotherapeutic and
psychopharmacologic intervention, can signicantly alter
the course of self-defeating behaviors and thus have a
salutary impact on physiology. A life thrown about by
internal and external conicts that often place the
individual in an escalating state of anxiety and dysphoria
further pushes on the physiology of the stress system, and
the augmentation of each potentate the other. It is a
common phenomenon that depressed individuals caught in
a maladaptive lifestyle do not respond well to pharmaco-
logic agents; the effect of the pharmacologic agent on in
regulating a dyregulated stress response is overridden by
the stress of a chaotic or chronically ungratifying
existence. It is clear that therapeutic success often depends
on a combination of psychotherapy and psychopharma-
cology for optimal results.
We now know that dysregulations of the physiologic
stress system, and of the capacity for a satisfactory
everyday life and attenuate its length. In this regard, the
great biologist Seymour Benzer exposed fruit ies to a
compound, which profoundly promotes genetic mutations,
and isolated those ies whose mutations led to a
substantially extended lifespan. Those with highly
extended lifespans, when explored by molecular tech-
niques, had an up-regulated system that counter-regulates
or reduces the strength and frequency of stress responses.
Thus, the union of psychotherapy and psychopharma-
cology in the treatment of affective and anxiety disorders,
in countering the long-term activation of the stress system,
is a matter of life and death that goes beyond self-
destructive behavior and suicide.
References
[1] American Psychiatric Association. Task force on DSM-IV. Diag-
nostic and statistical manual of mental disorders: DSM-IV. Washing-
ton, DC: American Psychiatric Association; 1994.
[2] Anda R, Williamson D, et al. Depressed affect, hopelessness, and the
risk of ischemic heart disease in a cohort of US adults. Epidemiology
1993;4(4):28594 [see comments].
[3] Arnsten A, Mathew R, et al. Alpha-1 noradrenergic receptor
stimulation impairs prefrontal cortical cognitive function. Biol
Psychiatry 1999;45:2631.
[4] Arnsten AF. The biology of being frazzled. Science 1998;280(5370):
17112.
[5] Ashton-Jones G, Rajkowski J, et al. Role of the locus coeruleus in
emotional activation. Prog Brain Res 1996;107:379402.
[6] Barefoot JC, Schroll M. Symptoms of depression, acute myocardial
infarction, and total mortality in a community sample. Circulation
1996;93(11):197680 [see comments].
[7] Brady LS, Gold PW, et al. The antidepressants uoxetine, idazoxan
and phenelzine alter corticotropin-releasing hormone and tyrosine
hydroxylase mRNA levels in rat brain: therapeutic implications. Brain
Res 1992;572(12):11725.
[8] Brady LS, Whiteld HJ, et al. Long-term antidepressant adminis-
tration alters corticotropin-releasing hormone, tyrosine hydroxylase,
and mineralocorticoid receptor gene expression in rat brain.
Therapeutic implications. J Clin Invest 1991;87(3):8317.
[9] Brown M, Fisher L, et al. Corticotropin-releasing-factor: actions on
the sympathetic nervous system and metabolism. Endocrinology
1982;111:92831.
[10] Cahill L, Haier RJ, et al. Amygdala activity at encoding correlated
with long-term, free recall of emotional information. Proc Natl Acad
Sci USA 1996;93(15):801621.
[11] Cahill L, McGaugh JL. Mechanisms of emotional arousal and lasting
declarative memory. Trends Neurosci 1998;21(7):2949.
[12] Chrousos G, Gold P. The concepts of stress and stress system
disorders. J Am Med Assoc 1992;267:124452.
[13] CJL Murray AL. Evidence based health policy-lessons from the
global burden of disease. Science 1996;274:740.
[14] Demitrack MA, Dale JK, et al. Evidence for impaired activation of the
hypothalamicpituitaryadrenal axis in patients with chronic fatigue
syndrome. J Clin Endocrinol Metab 1991;73(6):122434.
[15] Drevets WC, Price JL, et al. Subgenual prefrontal cortex abnormal-
ities in mood disorders. Nature 1997;386(6627):8247 [see
comments].
[16] DSM-IV, A.P.A.T.F. o. Diagnostic and statistical manual of mental
disorders: DSM-IV. Washington, DC: American Psychiatric
Association;1994.
[17] Frank E, Kupfer DJ, Perel JM, et al. Three year outcomes for
maintenance in therapies in recurrent depression. Arch Gen Psychiat
1990;47:10939.
[18] Frank EaTM. Natural history and preventive treatment of recurrent
mood disorders. Annu Rev Med 1999;50:45368.
[19] Fuster JM. The prefrontal cortex. New York: Raven; 1989.
[20] Fuster JM. The prefrontal cortex and its relation to behavior. Prog
Brain Res 1991;87:20111.
[21] Glassman AH, Shapiro PA. Depression and the course of coronary
artery disease. Am J Psychiatry 1998;155(1):411.
[22] Gold P, Chrousos G. Organization of the stress system andits
dysregulation inmelancholic and atypical depression. Mol Pschiat
2002;7:25475.
[23] Gold PW, Chrousos G, et al. Psychiatric implications of basic and
clinical studies with corticotropin-releasing factor. Am J Psychiatry
1984;141(5):61927.
[24] Gold PW, Goodwin FK, et al. Clinical and biochemical manifestations
of depression: relation to the neurobiology of stress (Part 1 of 2 parts).
N Engl J Med 1988;319:34853.
P.W. Gold / Clinical Neuroscience Research 4 (2005) 315324 323
[25] Gold PW, Goodwin FK, et al. Clinical and biochemical manifestations
of depression: relation to the neurobiology of stress (Part 2 of 2 parts).
N Engl J Med 1988;319:41320.
[26] Gold PW, Gwirtsman H, et al. Abnormal hypothalamicpituitary
adrenal function in anorexia nervosa. Pathophysiologic mechanisms
in underweight and weight-corrected patients. N Engl J Med 1986;
314(21):133542.
[27] Gold PW, Kling MA, et al. The clinical implications of corticotropin-
releasing hormone. Adv Exp Med Biol 1988;245(507):50719.
[28] Gold PW, Loriaux DL, et al. Responses to corticotropin-releasing
hormone in the hypercortisolism of depression and Cushings disease.
Pathophysiologic and diagnostic implications. N Engl J Med 1986;
314(21):132935.
[29] Guze S, Robins E. Suicide among primary affective disorders.
Br J Psychiat 1970;117:4338.
[30] Habib K, Weld K, et al. Oral administration of a corticotropin-
releasing hormone antagonist signicantly attenuates behavioral,
neuroendocrine, and autonomic responses in rimates. Proc Natl Acad
Sci 2000;97:607984.
[31] Holsboer F, Girken A, et al. Blunted corticotropin and normal cortisol
response to human corticotropin-releasing factor in depression.
1984;311:1127.
[32] Kendler K, Neale M, et al. Childhood parental loss and adult
psychopathology in women: a twin study perspective. Arch General
Psychiatry 1992;49:10916.
[33] Kendler KS, Eaves LJ, et al. The identication and validation of
distinct depressive syndromes in a population-based sample of female
twins. Arch Gen Psychiatry 1996;53(5):3919.
[34] Kendler KS, Eaves LJ. Models for the joint effect of genotype and
environment on liability to psychiatric illness. Am J Psychiatry 1986;
143:27989.
[35] Kendler KS, Kessler RC, et al. Stressful life events, genetic liability,
and onset of an episode of major depression in women. Am
J Psychiatry 1995;152(6):83342.
[36] Kendler KS, Neale MC, et al. The lifetime history of major depression
in women. Reliability of diagnosis and heritability. Arch Gen
Psychiatry 1993;50(11):86370.
[37] Kessler RC, McGonagle KA, et al. Lifetime and 12-month prevalence
of DSM-III-R psychiatric disorders in the United States. Results from
the National Comorbidity Survey. Arch Gen Psychiatry 1994;51(1):
819.
[38] LeDoux JE. Emotion and the amygdala. In: Aggleton JP, editor. The
amygdala: neurobiological aspects of emotion, memory, and mental
dysfuction. New York: Wiley; 1992. p. 33951.
[39] LeDoux JE. Emotion: clues from the brain. Annu Rev Psychol 1995;
46:20935.
[40] LeDoux JE, Romanski LM, Xagoraris AE. Indelibility of subcortical
emotional memories. J Cognitive Neurosci 1989;1:23843.
[41] Levitan R, Lesage A, et al. Reversed neurovegetative symptoms of
depression: a community study. Am J Psychiatry 1997;154:93440.
[42] Makino S, Gold PW, et al. Corticosterone effects on corticotropin-
releasing hormone mRNA in the central nucleus of the amygdala and
the parvocellular region of the paraventricular nucleus of the
hypothalamus. Brain Res 1995;640:10512.
[43] McGaugh JL, Cahill L, et al. Involvement of the amygdala in memory
storage: interaction with other brain systems. Proc Natl Acad Sci USA
1996;93(24):1350814.
[44] McGaugh JL, Introini-Collison IB, Cahill LF, Castellano C,
Dalmaz C, Parent MB, Williams CL. Neuromodulatory systems and
memory storage: role of the amgydala. Behav Brain Res 1993;58:
8190.
[45] Meaney MJ, Mitchell JB, Bhatnagar S, Iny LJ, Bodnoff SR, Viau V,
Sarrieau A. The effects of neonatal handling on the development of
the adrenocortical stress response: implications for neuropathology
and cognitive decits in later life. Psychoneuroendocrinology 1991;
16:87105.
[46] Michelson D, Stratakis C, et al. Bone mineral density in women with
depression. N Engl J Med 1996;335(16):117681.
[47] Morgan M, Romanski L, et al. Extinction of emotional learning:
contribution of medial prefrontal cortex. Neurosci Lett 1993;163:
10913.
[48] Nemeroff CB, Owens MJ, et al. Reduced corticotropin releasing factor
binding sites in the frontal cortex of suicide victims. Arch Gen
Psychiatry 1988;45:5779.
[49] Nemeroff CB, Wilderlov E, et al. Elevated concentrations of CSF
corticotropin-releasing-factor-like immunoreactivity in depressed
patients. Science 1984;226:13424.
[50] Packard MG, Cahill L, et al. Amygdala modulation of hippocampal-
dependent and caudate nucleus-dependent memory processes. Proc
Natl Acad Sci USA 1994;91(18):847781.
[51] Penninx B, Guralnik J, et al. Cardiovascular events and mortality in
newly and chronically depressed persons O70 years of age. Am
J Cardiol 1998;81:98894.
[52] Penninx BW, Geerlings SW, et al. Minor and major depression and
the risk of death in older persons. Arch Gen Psychiatry 1999;56(10):
88995.
[53] Rolls E. A theory of emotion and consciousness, and its application
to understanding the neural basis of emotion. In: Gazzaniga M,
editor. The cognitive neurosciences. Cambridge, MA: MIT Press;
1995. p. 1091106.
[54] Roozendaal B, Williams CL, et al. Glucocorticoid receptor activation
in the rat nucleus of the solitary tract facilitates memory consolida-
tion: involvement of the basolateral amygdala. Eur J Neurosci 1999;
11(4):131723 [in process citation].
[55] Sapolsky RM, Krey LC, et al. Prolonged glucocorticoid exposure
reduces hippocampal neuron number: implications for aging.
J Neurosci 1985;5(5):12227.
[56] Shapiro PA, Lidagoster L, et al. Depression and heart disease.
Psychiatric Annals 1997;27(5):34752.
[57] Vale W, Spiess J, et al. Characterization of a 41-residue ovine
hypothalamic peptide that stimulates secretion of corticotropin and
beta-endorphin. Science 1981;213(4514):13947.
[58] Valentino RJ, Foote SL, et al. Corticotropin-releasing hormone
activates noradrenergic nuerons of the locus coeruleus. Brain Res
1983;270:3637.
[59] Vanderpool J, Rosenthal NE, et al. Abnormal pituitaryadrenal
responses to corticotropin-releasing hormone in patients with seasonal
affective disorder: clinical and pathophysiological implications. J Clin
Endocrinol Metab 1991;72(6):13827.
[60] Viau V, Sharma S, et al. Increased plasma ACTH responses to stress
in nonhandled compared with handled rats require basal levels of
corticosterone and are associated with increased levels of ACTH
secretagogues in the median eminence. J Neurosci 1993;13:1097105.
[61] Wittchen HU, Knauper B, et al. Lifetime risk of depression. Br
J Psychiatry 1994;(Suppl.).
[62] Wong M-L, Kling MA, Munson PJ, Listwak S, Licinio J, Prolo P,
et al. Pronounced and sustained central hypernoradrenergic function
in major depression with melancholic features: relation to hypercorti-
solism and corticotropin-releasing hormone. Proc Natl Acad Sci 2000;
97:32530.
[63] Zola-Morgan S, Squire LR, Alvarez-Royo P, Clower RP. Indepen-
dence of memory functions and emotional behavior: separate
contributions fo the hippocampal formation and the amygdala.
Hippocampus 1991;1:20720.
P.W. Gold / Clinical Neuroscience Research 4 (2005) 315324 324
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Directed Energy Attacks & Mind Assault - Www-raven1-NetDocument12 pagesDirected Energy Attacks & Mind Assault - Www-raven1-Netstop-organized-crime100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Manual Del Conductor 2013-2014 COSTA RICADocument62 pagesManual Del Conductor 2013-2014 COSTA RICADiana Arlene88% (8)
- A Complete Neurological Nursing Assessment GuideDocument57 pagesA Complete Neurological Nursing Assessment GuideSarithaRajeshNo ratings yet
- CRPS and Compartment SyndromeDocument19 pagesCRPS and Compartment Syndromegbc1989No ratings yet
- Genetics Searching For AnswersDocument3 pagesGenetics Searching For AnswersDiana ArleneNo ratings yet
- AdhdDocument17 pagesAdhdDiana Arlene50% (2)
- Brain Structural and Functional Abnormalities in Mood Disorders PDFDocument27 pagesBrain Structural and Functional Abnormalities in Mood Disorders PDFDiana ArleneNo ratings yet
- Neurochemical Brain Imaging Studies inDocument9 pagesNeurochemical Brain Imaging Studies inDiana ArleneNo ratings yet
- Neurobiology of SorrowDocument9 pagesNeurobiology of SorrowDiana ArleneNo ratings yet
- Illustrated Poetry and Epic Images Persian Painting of The 1330s and 1340s PDFDocument149 pagesIllustrated Poetry and Epic Images Persian Painting of The 1330s and 1340s PDFChristine TongNo ratings yet
- Picturesque Ideas On The Flight Into EgyptDocument68 pagesPicturesque Ideas On The Flight Into EgyptDiana ArleneNo ratings yet
- Socially Explosive MindsDocument29 pagesSocially Explosive MindsDiana ArleneNo ratings yet
- Evolución EmocionesDocument23 pagesEvolución EmocionesDiana ArleneNo ratings yet
- EvilDocument8 pagesEvilDiana ArleneNo ratings yet
- 6 Tecar Vs Tens in Phantom Limb PainDocument8 pages6 Tecar Vs Tens in Phantom Limb PainSilvia PluisNo ratings yet
- Neural Control N Coordination-NotesDocument5 pagesNeural Control N Coordination-Notessudeep27krNo ratings yet
- Hannah Cheng, "Take Two Notes and Call Me in The Morning: The Science of Music Therapy"Document40 pagesHannah Cheng, "Take Two Notes and Call Me in The Morning: The Science of Music Therapy"MIT Comparative Media Studies/WritingNo ratings yet
- Endo & Exogenous Pacemakersin Biological RhythmsDocument2 pagesEndo & Exogenous Pacemakersin Biological RhythmsMiss_M90No ratings yet
- Ana Phisio Lab Report.Document4 pagesAna Phisio Lab Report.Diana Amor100% (1)
- Febrile SeizureDocument32 pagesFebrile SeizureShiva Valeska ArdhaniswariNo ratings yet
- Autonomic Nervous System - HandoutsDocument5 pagesAutonomic Nervous System - HandoutsKelly Trainor100% (1)
- The Neural Basis of Motor-Skill Learning: Current Directions in Psychological Science December 1999Document6 pagesThe Neural Basis of Motor-Skill Learning: Current Directions in Psychological Science December 1999Charitini PetridouNo ratings yet
- Chapter 15 - Neural Integration I: Sensory Pathways and Somatic Nervous SystemDocument4 pagesChapter 15 - Neural Integration I: Sensory Pathways and Somatic Nervous Systemtomorrow.today.yesterday .yesterdayNo ratings yet
- Brain-Based Models of Developmental Language DisordersDocument19 pagesBrain-Based Models of Developmental Language DisordersЈован Д. РадовановићNo ratings yet
- BIONICS: A Proposal for a Transatlantic Research Program in Bio-Inspired Information TechnologiesDocument62 pagesBIONICS: A Proposal for a Transatlantic Research Program in Bio-Inspired Information Technologiesliang102009No ratings yet
- Revalida Review NotesDocument14 pagesRevalida Review NotesBryan Lloyd RayatNo ratings yet
- Reflection PaperDocument2 pagesReflection PaperVia RoderosNo ratings yet
- Case Report: Supevisor: Dr. Irma Tarida Listiawati, SP - KK By: Alif Ramadhan, S.KedDocument22 pagesCase Report: Supevisor: Dr. Irma Tarida Listiawati, SP - KK By: Alif Ramadhan, S.Kedpang_paangNo ratings yet
- Pain Physiology Pathways Mechanisms ClassificationDocument71 pagesPain Physiology Pathways Mechanisms Classificationkeerthi_keshapagaNo ratings yet
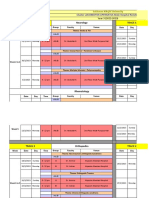
- Sulaiman AlRajhi University Neurology & Orthopedics Hospital Rotation ScheduleDocument10 pagesSulaiman AlRajhi University Neurology & Orthopedics Hospital Rotation ScheduleAbdullah MelhimNo ratings yet
- Neurotransmitter TepiDocument32 pagesNeurotransmitter TepiAmallia Nuggetsiana SetyawatiNo ratings yet
- Performance Task in Personal Development (Depression) : Submitted By: Submitted ToDocument6 pagesPerformance Task in Personal Development (Depression) : Submitted By: Submitted ToJanea Arinya100% (1)
- Primary Brain TumorDocument33 pagesPrimary Brain Tumoriura echin100% (2)
- Topographic Anatomy of Basal NucleiDocument44 pagesTopographic Anatomy of Basal NucleiRafique AhmedNo ratings yet
- Quiz Sensation 103Document11 pagesQuiz Sensation 103amandeep251702No ratings yet
- Children and Teens With Asperger Syndrome: Instant Help ForDocument4 pagesChildren and Teens With Asperger Syndrome: Instant Help Foraleksandra_radevicNo ratings yet
- Psikologi UmumDocument28 pagesPsikologi UmumKristina DominikaNo ratings yet
- Chapter 7 - NERVOUS SYSTEM PDFDocument58 pagesChapter 7 - NERVOUS SYSTEM PDFMary LimlinganNo ratings yet
- Åyurvedic Check-List: Chaukhambha OrientaliaDocument114 pagesÅyurvedic Check-List: Chaukhambha OrientaliaNirav TrivediNo ratings yet
- CSF (Cerebrospinal Fluid)Document4 pagesCSF (Cerebrospinal Fluid)few10No ratings yet
- SMK MAMBAU SCIENCE CURRICULUM SPECIFICATIONSDocument26 pagesSMK MAMBAU SCIENCE CURRICULUM SPECIFICATIONSNurul AzniNo ratings yet