Professional Documents
Culture Documents
TB JMEDINT PDF
Uploaded by
Cintia FloresOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
TB JMEDINT PDF
Uploaded by
Cintia FloresCopyright:
Available Formats
doi: 10.1111/j.1365-2796.2011.02378.
x
Impact of a Mycobacteriumtuberculosis-specic
interferon-c release assay in bronchoalveolar lavage
uid for a rapid diagnosis of tuberculosis
C. Jafari
1,
*, P. Kessler
1,
*, G. Sotgiu
2
, M. Ernst
3
&C. Lange
1
Fromthe
1
Divisionof Clinical InfectiousDiseases, ResearchCenter Borstel, Borstel, Germany,
2
HygieneandPreventiveMedicineInstitute,
UniversitySassari, Sassari, Italy, and
3
Divisionof ImmuneCell Analytics, ResearchCenter Borstel, Borstel, Germany
Abstract. Jafari C, Kessler P, Sotgiu G, Ernst M,
Lange C(ResearchCenter Borstel, Borstel, Germany;
Hygiene and Preventive Medicine Institute, Univer-
sity Sassari, Sassari, Italy; Research Center Borstel,
Borstel, Germany). Impact of a Mycobacterium
tuberculosis-specic interferon-c release assay in
bronchoalveolar lavage uid for a rapid diagnosis of
tuberculosis. JInternMed2011; 270: 254262.
Objectives. Evaluationof different methods for aninitial
treatment decisioninindividualswithsuspectedpul-
monarytuberculosis.
Background. Recently, important advances regarding
the diagnosis of pulmonary tuberculosis have been
introduced, which inuence the decision to initiate
anti-tuberculosistreatment.
Methods. To evaluate the impact of different methods
for the presumeddiagnosis of tuberculosis, individu-
als with suspected tuberculosis were prospectively
enrolled following a specic algorithm including ini-
tial smear microscopy and Mycobacteriumtuberculo-
sis-specic nucleic acid amplication (NAAT) from
sputum. In cases of negative initial test results,
tuberculin skin testing, bronchoscopy with trans-
bronchial biopsies and interferon-c release assays
(IGRAs) in peripheral blood and bronchoalveolar
lavage(BAL) uidwereperformed.
Results. Amongst 135 individuals with suspected
tuberculosis, 42 had tuberculosis, 10 had nontuber-
culous mycobacteria pulmonary infection coloniza-
tion (one had both tuberculosis and nontuberculous
mycobacteria pulmonary infection colonization) and
84 had an alternative nal diagnosis. The sensitivity
andspecicity were41%and99%[positive likelihood
ratio (LR+) = 40] for sputum microscopy and 31%
and 98% (LR+ = 16) for BAL nucleic acid ampli-
cation, respectively. In patients with acid-fast
bacilli smear-negative tuberculosis (25 42, 59.5%),
M. tuberculosis-specic BAL uid IGRA was 92%
sensitive and87%specic (LR+ = 7) for the diagnosis
of tuberculosis.
Conclusion. None of the microbiological or immunologi-
cal methods that aim to provide a rapid diagnosis of
tuberculosis whilst waiting the conrmation of the
M. tuberculosis culture results is on its own accurate
enoughto diagnose or exclude pulmonary tuberculo-
sis. Negative sputum microscopy and M. tuberculo-
sis-specic NAAT results should prompt bronchos-
copy including BAL for M. tuberculosis-specic
IGRA in individuals with suspected pulmonary
tuberculosis.
Keywords: BAL, diagnosis, IGRA, interferon-c, tuber-
culosis.
Introduction
Tuberculosis isone of the leadingcauses of morbidity
and mortality worldwide [1]. The World Health Orga-
nization (WHO) has stated that one-third of the
worlds population is infected with Mycobacterium
tuberculosis, the bacteriumthat causes tuberculosis
[2]. However, this is anestimate as true infectionwith
M. tuberculosis canonly be diagnosed inthe minority
of individuals who develop active tuberculosis. By
contrast, latent infectionwithM. tuberculosis is diag-
nosed indirectly by a positive immune reactioninthe
in vivo tuberculinskin test or, more recently, inanex
vivointerferon-c releaseassay(IGRA) [3]. *CJandPKcontributedequallytothisarticle.
254 2011 The Association for the Publication of the Journal of Internal Medicine
Original Article
|
Detection of M. tuberculosis in liquid cultures or on
solidmediaremains the goldstandardfor the diagno-
sis of tuberculosis. In routine clinical practice, initial
treatment decisions cannot rely on this method as
culture growth of M. tuberculosis takes several weeks
before detection is possible [4]. In addition, approxi-
mately 20% of patients with tuberculosis are not
identiedbyculturegrowthof M. tuberculosis[5].
In clinical practice, the initial decision to treat a pa-
tient for tuberculosis relies on methods that mostly
yield nondenitive results. These include sputum or
bronchoalveolar lavage (BAL) uid microscopy,
M. tuberculosis-specic nucleic acid amplication
techniques (NAATs) from biological specimens or
immunodiagnosticprocedures.
To date, the value of immunological methods for the
diagnosis of tuberculosis has been limited, as the
tuberculin skin test and IGRAs performed on
peripheral blood alone cannot differentiate active
tuberculosisfromlatent infectionwithM. tuberculosis
[6]. Identication of local antigen-specic lympho-
cytes at the site of the infection, e.g. amongst cells of
the BAL uid in pulmonary tuberculosis, improves
the rapid diagnosis of tuberculosis in patients with
negative acid-fast bacilli sputum smears and can
inuence greatly the decision of whether or not to
initiatetreatment for tuberculosis[710].
We have evaluated the relative impact of different
methods for the rapid diagnosis of tuberculosis,
including sputum microscopy for the presence of
acid-fast bacilli, M. tuberculosis-specic NAATs,
tuberculinskintesting, bronchoscopy andIGRAper-
formed on cells from the peripheral blood as well as
fromBAL uidinroutine clinical practice at a clinical
tuberculosis centre inGermany, a country witha low
incidenceof tuberculosis(5.5 100,000) [11].
Methods
Patients admitted between March 2005 and May
2007 for the diagnostic evaluation of presumed
tuberculosis at the Medical Clinic of the Research
Center Borstel, Germany, were includedinthe study.
Patients withpresumedtuberculosis were referredto
the clinic if they had abnormalities on chest imaging
andsymptoms suggestive of active pulmonary tuber-
culosis. Tuberculosis was diagnosed or excluded
accordingtoarecentlysuggestedalgorithm[12]: spu-
tum samples were collected on three consecutive
days andanalysedfor the presence of acid-fast bacilli
by microscopy. If a positive microscopy result was
obtained, a M. tuberculosis-specic NAAT (BDProbe-
Tec ET assay, Becton Dickinson, Sparks, MD, USA)
was performed subsequently for the rapid identica-
tionof M. tuberculosis.
All sputum samples were cultured for up to 6 weeks
in uid media (MGIT, BD, Heidelberg), and up to
8 weeks in solid media (Loewenstein-Jensen), before
concluding that results were negative. Culture of
M. tuberculosis was considered the gold standard
method for the diagnosis of tuberculosis. Adiagnosis
of clinical tuberculosis was made after alternative
diseases had been ruled out and after patients had
received anti-tuberculosis therapy, which was pre-
scribed by the treating physician on clinical grounds
followingnoclinical responsetoantibiotictherapy.
Tuberculinskintestingwas performedonall patients
withtheexceptionof thosewithapast medical history
of tuberculosis, because of an increased risk of
ulcerative skin lesions. Tuberculin skin testing was
performed by intracutaneous injection of 0.1-mL
tuberculin RT-23 (Statens Serum Institute, Copen-
hagen, Denmark). The induration was measured
4872 hlater bytheballpoint pentechnique[13].
The M. tuberculosis-specic IGRA ELISpot (T-
SPOT.TB Test, Oxford Immunotec, Abingdon, UK)
was performed. Briey, 250 000 peripheral blood
mononuclear cells (PBMCs) were prepared by Ficoll-
Hypaque density-gradient centrifugation from
heparinized blood. PBMCs were plated overnight on
96-well plates precoated with a mouse anti-human
interferon-c antibody. The cells were (i) left unstimu-
lated (negative control), (ii) stimulated with
10 ng ml
)1
anti-CD3 monoclonal antibody (clone
X35, Beckman-Coulter, Krefeld, Germany; positive
control) or stimulated with 5 lg ml
)1
of early secre-
tory antigenic target (ESAT)-6 and culture ltrate
protein (CFP)-10 peptides (kindly provided by Oxford
Immunotec, Abingdon, UK). Culturing of the cells,
washing, counterstaining, visualizationandanalysis
of the spots were performed according to the manu-
facturers guidelines. The response of stimulated
cultures was considered positive if the test well
contained more than ve spots and had twice the
number of spots compared to the negative control
well. The response was considered negative if it did
not meet the criteria for a positive result and if the
positive control well contained at least twice the
number of spots compared to the negative control
well. Results that met neither of these denitions
were considered to be indeterminate and excluded
fromfurther analysis.
C. Jafari et al.
|
Rapid diagnosis of tuberculosis
2011 The Association for the Publication of the Journal of Internal Medicine Journal of Internal Medicine 270; 254262 255
Patients with three negative microscopy results for
the presence of acid-fast bacilli underwent bronchos-
copy, which was performed according to German
guidelines [14] and included a transbronchial biopsy
for histology and BAL with 200300 mL of normal
saline froman affected lung segment for microscopy,
M. tuberculosis-specic NAAT, M. tuberculosis cul-
tureandIGRA.
BALuidmononuclear cells(BALMCs) wereobtained
by passing the BAL through a stainless steel sieve
(WMF, Geislingen, Germany) witha meshaperture of
0.2 mm as described previously [79]. Elispot of
BALMCs was otherwise performed and analysed in
the same way as Elispot using PBMCs as described
previously [79, 15]. Positive likelihood ratios were
calculated by dividing sensitivity by (1-specicity)
whilst negative likelihood ratios were calculated by
dividing (1-sensitivity) by specicity. The study was
approvedbythe ethical committee of the Universityof
Lubeck, Germany.
Results
In total, 135 patients who were referred for further
diagnosis because of clinical suspicion of tuberculo-
siswereincludedinthestudy(Fig. 1, Table1).
Identication of acid-fast bacilli in sputum
Acid-fast bacilli were identiedinthe sputumsmears
of 18 135(13.3%) individuals, 17of whomwere diag-
nosed with tuberculosis by positive M. tuberculosis-
specic NAAT and or culture. Nontuberculous
mycobacteria (M. avium) were identied by culture in
1 18 (5.6%) individuals with a positive acid-fast
bacilli sputum smear stain. There was no statistical
difference amongst the prevalence of chronic
obstructive pulmonary disease (COPD), smoking,
alcohol abuse or diabetes mellitus in patients with
tuberculosis with or without detectable acid-fast
bacilli insputumsmears(datanot shown).
Tuberculin skin test results
Tuberculin skin test results were available in 22
tuberculosiscaseswithnegativeacid-fast bacilli spu-
tumsmears and in 61 nontuberculosis patients with
negative acid-fast bacilli sputum smears. Amongst
these 83 patients, 43 (51.8%) had a tuberculin skin
test reading of <5 mm, 10 (12.1%) had a reading be-
tween 5 and 10 mm and 30 (36.2%) had a reading
15 mm. Sensitivity and specicity were calculated
for cut-off valuesof 5and15 mm(Table2).
Blood IGRA results
Amongst 117patients withanegativeacid-fast bacilli
sputum smear result [117 135 (86.7%)], 70 (59.8%)
hadapositive bloodIGRAresult and45(38.5%) hada
negative result. One patient had an indeterminate
IGRA result and for one nontuberculosis patient, the
result was not available. Of 24 tuberculosis patients,
22 (91.7%) had a positive blood IGRA result and
76 87 (87.4%) nontuberculosis patients had a nega-
tive result. The sensitivity and specicity of the blood
IGRAwere96.0%and48.9%, respectively.
Bronchoscopy results
All 117 patients with suspected tuberculosis and
with negative sputum smears underwent bronchos-
copywithBAL.
BAL microscopy
Microscopy for the presence of acid-fast bacilli inBAL
uid was positive in1 117 (0.9%) and negative inthe
remaining116(99.2%) subjects.
BAL IGRA results
ELISpot in BALMCs was positive in 33 117 (28.2%)
cases and negative in78 117 (66.7%) cases; indeter-
minate results were obtained in six (5.1%) patients.
Twenty-twoof 24(91.7%) tuberculosis patients hada
positive BAL IGRA result, and 76 87 (87.4%) nontu-
berculosis patients had a negative BAL IGRA result.
The sensitivity and specicity of the test were 91.7%
and87.4%, respectively.
In patients with tuberculosis, median numbers of
ESAT-6- CFP-10-specic spot-forming cells (SFCs)
250 000 PBMCs and BALMCs were 11 20 and
34 45, respectively (Table 1). By contrast, in pa-
tients from the nontuberculosis group, the median
number of ESAT-6- CFP-10-SFC 250 000 PBMCs
and BALMCs were 2 5 and 1 1, respectively. Thus,
in contrast to patients with latent infection with
M. tuberculosis, ESAT-6- and CFP-10-specic SFCs
were concentrated in the BAL uid compared to the
peripheral blood in patients with active tuberculosis
(Table 1). When the production of interferon-c was
attributed only to lymphocytes amongst mononu-
clear cells in blood and BAL, the concentration
of ESAT-6- and CFP-10-specic lymphocytes at
the site of infection was of the order of magnitude of
9.1 times and 11.4 times, respectively (data not
shown).
C. Jafari et al.
|
Rapid diagnosis of tuberculosis
256 2011 The Association for the Publication of the Journal of Internal Medicine Journal of Internal Medicine 270; 254262
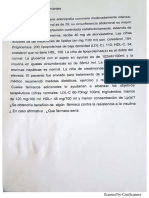
Fig. 1 Results of different diagnostic procedures for 135 individuals with suspected tuberculosis.
#
not performed in one patient
fromthe nontuberculosis group, indeterminate test results (ITR) n = 1 (1%); *not performedin34patients; **ITRn = 6 (5%);
##
one
patient with a positive culture for Mycobacteriumtuberculosis and Mycobacteriumavium. AFBdenotes acid-fast bacilli, NAAT
denotes nucleic acid amplication technique, NTMdenotes nontuberculous mycobacteria, IGRA denotes interferon-c release as-
say, TSTdenotestuberculinskintest, TBBdenotestransbronchial biopsy.
C. Jafari et al.
|
Rapid diagnosis of tuberculosis
2011 The Association for the Publication of the Journal of Internal Medicine Journal of Internal Medicine 270; 254262 257
NAAT results
The M. tuberculosis-specic NAAT using BAL speci-
mens was positive in 6 71 cases (8.5%) and negative
inthe remaining 65(91.6%). Of thesixpatients witha
positive BALNAATresult, ve hada positive M. tuber-
culosis culture. One patient had pulmonary inltra-
tion of unknown origin and developed bronchogenic
carcinoma 2 years later. Five of 16 tuberculosis pa-
tients had a positive NAAT result using BAL speci-
mens and 54 55 nontuberculosis patients had a
negative result. The sensitivity and specicity of
M. tuberculosis-specic NAAT using BAL specimens
were31.3%and98.2%, respectively.
In addition, in 44 of the 117 patients with negative
acid-fast bacilli sputum smears, NAAT was per-
formed on sputum samples. Seven of 44 (15.9%)
NAAT examinations were positive and the remaining
37(84.1%) werenegative. Amongst thesevenpatients
with a positive sputumNAAT result, four were nally
diagnosed with active tuberculosis whereas three
hadanalternativediagnosis.
Culture results
Overall, 42 135 (31.1%) patients had a nal diagno-
sis of tuberculosis. M. tuberculosis was culturedfrom
the sputum, BAL or, if available, from a biopsy in
Table 1 Demographic characteristics and Mycobacterium tuberculosis-specic immune responses in 135 individuals with sus-
pectedtuberculosisat areferral centreinGermany
Variables
TBpatients
(n = 42)
Non-TBpatients
(n = 93) P-value
Age, median(IQR) 39(25) 56(24) 0.002
Gender, n(%)
Male 26 42(61.9) 30 93(32.3) 0.001
TBconrmedbyculture 33 42(76.2)
IGRAbloodSFC 250 000ESAT-6, median(IQR) 11.0(27.5) 2.0(8.5) <0.001
IGRAbloodSFC 250 000CFP-10, median(IQR) 20.0(34.5) 5.0(11.0) <0.001
IGRABALSFC 250 000ESAT-6, median(IQR) 33.5(43.0) 1.0(3.0) <0.001
IGRABALSFC 250 000CFP-10, median(IQR) 45.0(57.0) 1.0(3.5) <0.001
TST(mm), median(IQR) 18.0(16.0) 0.0(13.0) <0.001
BAL, bronchoalveolar lavage; CFP, culture ltrate protein; ESAT, early secretory antigenic target; IGRA, interferon-c release
assay; SFC, spot-formingcells.
Table 2 Sensitivities, specicities, positiveandnegativelikelihoodratiosof different methodsfor thediagnosisof tuberculosis
Test Sensitivity Specicity
Positive
predictive
value
Negative
predictive
value
Positive
likelyhood
ratio
Negative
likelyhood
ratio
Sputummicroscopy(n = 135) 40.5 98.9 94.4 78.6 37.6 0.6
BALmicroscopy* (n = 101) 4.55 100.0 100 79 0.96
TST>5 mm(n = 83) 81 62.9 42.5 90.7 2.2 0.3
TST>15 mm(n = 83) 71.4 82.3 57.7 89.5 4.03 0.35
NAAT(BAL)* (n = 71) 31.3 98.2 83.3 83.1 17.2 0.7
NAAT(Sputum) (n = 44) 44.4 91.4 57.1 86.5 5.2 0.61
IGRAblood(n = 115) 96.0 48.9 34.3 97.8 1.9 0.08
IGRABAL* (n = 111) 91.7 87.4 66.7 97.4 7.3 0.1
BAL, bronchoalveolar lavage; TST, tuberculin skin testing; NAAT, nucleic acid amplication technique; IGRA, interferon-c
releaseassay.
*BALwasonlyperformedinpatientswithnegativeacid-fast bacillysputumsmear results.
C. Jafari et al.
|
Rapid diagnosis of tuberculosis
258 2011 The Association for the Publication of the Journal of Internal Medicine Journal of Internal Medicine 270; 254262
33 135 (24.4%) cases [in 17 17 (100%) patients with
and in 16 25 (64.0%) without the detection of acid-
fast bacilli on sputumsmear stains]. Thus, in 33 42
(78.6%) patients, the diagnosis of tuberculosis was
conrmed by M. tuberculosis culture. Of the 9 42
(21.4%) patients with a clinical diagnosis of tubercu-
losis, one had a positive NAAT result from sputum.
M. tuberculosiscultureswere positive fromsputumin
28 135 (20.7%) patients, from BAL in 14 117
(11.9%) patients, and fromhistological specimens in
6 31 (19.4%) patients. In addition, growth of both
M. tuberculosis andM. aviumwas observedinone pa-
tient with a negative acid-fast bacilli sputum smear
culture. In 10 135 (7.4%) patients, nontuberculous
mycobacteriacouldbeculturedfrombronchopulmo-
nary specimens (six M. avium, two M. fortuitum, one
M. gordonae and one M. tilburgii). Only 1 10 (10.0%)
patients with a positive culture for nontuberculous
mycobacteria had a positive acid-fast bacilli sputum
smear result.
Comparative evaluation of different tests
The positive likelihoodratio was calculated and com-
pared for all methods (Table 2). Sputum microscopy
has a high specicity (98.9%) and therefore a high
positive likelihood ratio (LR+ = 37.6) whereas the
tuberculinskintest has a somewhat lower specicity
(6382%), depending on the cut-off (>5 mm or
>15 mm), and a low positive likelihood ratio
(LR+ = 24). It is interesting that if performed using
BAL uid, the ELISpot IGRA had a higher positive
likelihood ratio than if performed on blood: LR+ = 7
for BAL ELISpot IGRA versus LR+ = 2 for blood ELI-
Spot IGRA. To estimate the diagnostic value of a
method, sensitivity also has to be taken into consid-
eration. In Table 2, sensitivity and specicity likeli-
hood ratio of the relevant methods for tuberculosis
diagnosis are shown. Microscopy showedthe highest
positive likelihood ratio but a low sensitivity (41%).
Blood ELISpot IGRA had the highest sensitivity
(96%) but because of a lowspecicity (49%), its posi-
tive likelihoodratio was only about 2.
Discussion
In this study, the clinical impact of different diag-
nostic methods for a rapid diagnosis of tuberculo-
sis, including IGRA (ELISpot) performed on cells
from the BAL uid, have been analysed under
routine clinical conditions. The key nding of the
study was that none of the evaluated methods
alone was able to reliably diagnose or exclude
tuberculosis. Microbiological methods (sputum
BAL uid smear microscopy, M. tuberculosis-spe-
cic NAAT with sputum BAL) had a superior
positive likelihood ratio for the diagnosis of tuber-
culosis compared to the immunological methods
(tuberculin skin test and IGRA). However, the low
sensitivity of the microbiological methods did not
allow the exclusion of tuberculosis in cases with
a negative test result. In this study, 25 42
(59.5%) patients with active tuberculosis would
have been missed by sputum microscopy alone.
IGRA (ELISpot) performed on cells from the BAL
uid, a procedure that is not yet widely available,
was the best method to distinguish active tuber-
culosis from latent infection with M. tuberculosis,
whereas the impact of IGRA performed on cells
from the peripheral blood was not greater than
that of the tuberculin skin test. In fact, BAL
IGRA (ELISpot) had a very high negative likeli-
hood ratio and, according to the results from this
study, to a great extend allows the exclusion of
active tuberculosis. This will help to improve cost
efciency as unnecessary patient isolation can be
avoided.
The clinical diagnosis of tuberculosis may be dif-
cult [16], especially in countries of low tuberculosis
incidence, as most individuals who are suspected of
having tuberculosis receive a different nal diagno-
sis after clinical evaluation [9]. In this study, less
than 25% of patients referred to a clinical centre for
tuberculosis in Germany had a nal diagnosis of
pulmonary tuberculosis conrmed by a positive cul-
ture of M. tuberculosis from bronchopulmonary
specimens and only 13% of suspected tuberculosis
cases had positive acid-fast bacilli sputum smears.
By contrast, the proportion of suspected cases
with positive acid-fast bacilli sputum smears is gen-
erally higher in high-incidence countries, ranging
from 17.3% and 18.6% in Malawi and Senegal to
20.2% and 32.1% in Uganda and Benin [17, 18],
respectively.
Consistent with previous ndings [19] and the report
from the WHO [20], less than 50% of patients with
active tuberculosis had acid-fast bacilli in sputum
smears. Detection of acid-fast bacilli might increase
by sputum induction, although the effect of sputum
induction may be greatest on the rates of sputum
cultureconversion[21].
In those with suspected tuberculosis and negative
acid-fast bacilli sputum smears, bronchoscopy is
usually indicated [12]. However, the identication
of additional cases of tuberculosis by BAL uid
C. Jafari et al.
|
Rapid diagnosis of tuberculosis
2011 The Association for the Publication of the Journal of Internal Medicine Journal of Internal Medicine 270; 254262 259
acid-fast bacilli stain analysis is limited. In a recent
study from Switzerland [21], 4 91 (4.4%) tuberculo-
sis patients were identiedby BALuidstaininaddi-
tion to the sputum smear examination, compared to
only1 101(1.0%) patientsinthepresent study.
Of importance, nontuberculous mycobacterial infec-
tion must be considered in patients with positive
acid-fast bacilli staining. Because of the high
sensitivity of acid-fast bacilli-positive specimens,
M. tuberculosis-specic NAAT has been used for the
rapid discrimination of M. tuberculosis from nontu-
berculous mycobacteria [22, 23]. However, the sensi-
tivity for tuberculosis of NAATinsputumor BAL uid
in acid-fast bacilli smear-negative cases is limited
[24]. A decision to treat for active tuberculosis based
ontheresult of theNAATinsputumor BALuidalone
would have missed 5669% of patients with a cul-
ture-conrmed diagnosis in this study. Of note, the
specicity of M. tuberculosis-specic NAAT was only
91% in this study and thus lower than previously
reported [22]. Two of three individuals with a positive
M. tuberculosis-specic NAAT result, who did not
have active tuberculosis, had a history of tuberculo-
sis, possiblyexplainingthisnding.
M. tuberculosis-specicIGRAincellsfromtheperiph-
eral blood had a sensitivity of 96%anda specicity of
49% for the diagnosis of active tuberculosis. The
specicity of the IGRA for the diagnosis of active
tuberculosis in this study is considerably lower than
reported in a meta-analysis by Diel et al. [25]. This
discrepancy is most probably related to the different
groups that were evaluated to determine the test
specicity. In the present study, those suspected of
tuberculosis who eventually received a different nal
diagnosiswereincludedintheevaluationfor specic-
ity. This group included migrants from countries of
hightuberculosis incidence as well as patients witha
past medical history of tuberculosis. These patients
were likely to test positive with the blood IGRA. By
contrast, individuals withalowriskof M. tuberculosis
infection are commonly included within control
groups to evaluate the test specicity of IGRAs [25].
This may lead to an incorrect diagnosis of active
tuberculosis when based on IGRAs performed on
cells from the peripheral blood. However, in active
tuberculosis, antigen-specic cells clonally expand
and are concentrated at the site of infection [7, 26
29].
In this study, patients with active tuberculosis had a
roughly 10-fold concentration of antigen-specic
lymphocytes in the BAL uid versus the peripheral
blood when compared to individuals with latent
M. tuberculosisinfection.
When compared to other immunodiagnostic meth-
ods, M. tuberculosis-specic IGRA (ELISpot) in cells
fromtheBALuidwasthebest methodfor rapiddiag-
nosis of active tuberculosis with a sensitivity of 92%
andaspecicityof 87%. Thesendingsaresupported
by the latest meta-analysis of the role of IGRAs in the
diagnosisof activetuberculosis[30].
The limitations of the study need to be addressed.
This study was performed in a single centre in a
country with a low incidence of tuberculosis and
a low prevalence of HIV infection. Results from
this study cannot be generalized to other settings,
e.g. to developing countries with an intermediate
or high incidence of tuberculosis and or with a
higher prevalence of HIV infection. Sensitivity
results of sputum smear microscopy and sputum
NAAT could have been expected to be higher when
using sputum induction methods [3133]. Culture
conrmation of tuberculosis was not possible in
9 42 patients and, although these patients
responded well to antituberculosis therapy, they
could have been misclassied. Finally, not all
individuals with negative acid-fast bacilli sputum
smear results had M. tuberculosis-specic NAAT
performed on sputum as it is not routinely recom-
mended in Germany [34]. Although M. tuberculo-
sis-specic ELISpot IGRA in cells from the BAL
uid has been evaluated in countries of high [10]
and low [79, 15, 35] tuberculosis incidence, the
procedure is not widely available yet and needs to
be evaluated by the regulatory authorities before
it can be recommended for general diagnostic
application.
In conclusion, identication of M. tuberculosis from
culture remains the goldstandardfor thediagnosis of
pulmonarytuberculosisandiscurrentlytheonlyreli-
able method for antibiotic resistance testing in the
majority of cases with negative acid-fast bacilli spu-
tumsmears. None of the microbiological or immuno-
logical methods that aimto provide a rapid diagnosis
of tuberculosis whilst awaiting the conrmation of
the culture result is on its own accurate enough to
diagnose or exclude tuberculosis. Local immunodi-
agnosis by M. tuberculosis-specic IGRA(ELISpot) in
cells fromthe BAL uid is possibly the best available
immunological methodtodistinguishactive tubercu-
losis from latent M. tuberculosis infection; however,
further studies will be needed to recommend this
methodfor routineclinical practice. Onaverage, more
C. Jafari et al.
|
Rapid diagnosis of tuberculosis
260 2011 The Association for the Publication of the Journal of Internal Medicine Journal of Internal Medicine 270; 254262
thanone inevery two patients evaluatedinthis study
has beneted from M. tuberculosis-specic ELISpot
IGRA in cells fromthe BAL uid for the rapid diagno-
sis of acid-fast bacilli smear-negative pulmonary
tuberculosis. Bronchoscopy should be indicated for
all cases of suspected active tuberculosis with nega-
tive acid-fast bacilli sputum smears, as the majority
will have a different nal diagnosis. Alternative
diagnoses to tuberculosis, such as sarcoidosis,
bronchogenic carcinoma or cryptogenic organizing
pneumonia, need to be considered and identied by
bronchoscopy. A stepwise diagnostic approach, as
suggested by the algorithm described in this study,
might yield the best results for a rapid preliminary
diagnosis of tuberculosis, justifying treatment initia-
tion whilst the results of M. tuberculosis cultures are
pending.
Conict of interest statement
Noconictsof interest todeclare.
References
1 WHO. Global Tuberculosis Control: A Short Update to the 2009
Report. Geneva: WorldHealthOrganization, 2009.
2 WHO. Tuberculosis, fact sheet 104; http://www.who.int/
mediacentre/factsheets/fs104/en/. Geneva. 2010.
3 Mack U, Migliori GB, Sester M et al. LTBI: latent tuberculosis
infection or lasting immune responses to M. tuberculosis? A
TBNETconsensusstatement. Eur Respir J2009; 33: 95673.
4 Hanna BA, EbrahimzadehA, Elliott LBet al. Multicenter evalua-
tion of the BACTECMGIT 960 systemfor recovery of mycobacte-
ria. JClinMicrobiol 1999; 37: 74852.
5 Robert-Koch-Institut. Bericht zur Epidemiologie der Tuberkulose
inDeutschlandfur 2007. Berlin: Robert-Koch-Institute, 2009.
6 Lange C, Pai M, Drobniewski F, Migliori GB. Interferon-gamma
releaseassaysfor thediagnosisof activetuberculosis: sensibleor
silly?Eur Respir J2009; 33: 12503.
7 Jafari C, Ernst M, Kalsdorf Bet al. Rapiddiagnosis of smear-neg-
ative tuberculosis by bronchoalveolar lavage enzyme-linked im-
munospot. AmJRespir Crit CareMed2006; 174: 104854.
8 Jafari C, Ernst M, Strassburg A et al. Local immunodiagnosis
of pulmonary tuberculosis by enzyme-linked immunospot.
Eur Respir J2008; 31: 2615.
9 Jafari C, Thijsen S, Sotgiu G et al. Bronchoalveolar lavage
enzyme-linkedimmunospot for arapiddiagnosisof tuberculosis:
a Tuberculosis Network European Trialsgroup study. Am J
Respir Crit CareMed2009; 180: 66673.
10 Dheda K, van Zyl-Smit RN, Meldau R et al. Quantitative lung T
cell responsesaidtherapiddiagnosisof pulmonarytuberculosis.
Thorax2009; 64: 84753.
11 Robert-Koch-Institut. Bericht zur Epidemiologie der Tuberkulose
inDeutschlandfur 2008. Berlin: Robert-Koch-Institute, 2010.
12 LangeC, Mori T. Advancesinthediagnosisof tuberculosis. Respi-
rology2010; 15: 22040.
13 Sokal JE. Editorial: measurement of delayed skin-test re-
sponses. NEngl JMed1975; 293: 5012.
14 Haussinger K, Ballin A, Becker HD et al. Recommendations for
quality standards inbronchoscopy. Pneumologie 2004; 58: 344
56.
15 StrassburgA, Jafari C, Ernst M, LotzW, LangeC. Rapiddiagnosis
of pulmonaryTBbyBALenzyme-linkedimmunospot assay inan
immunocompromisedhost. Eur Respir J2008; 31: 11325.
16 Pai M, OBrienR. Newdiagnostics for latent andactive tuberculo-
sis: state of the art and future prospects. Semin Respir Crit Care
Med2008; 29: 5608.
17 Katamba A, Laticevschi D, Rieder HL. Efciency of a third
serial sputumsmear examination in the diagnosis of tuberculo-
sis inMoldova andUganda. Int J Tuberc Lung Dis 2007; 11: 659
64.
18 Rieder HL, Arnadottir T, Tardencilla Gutierrez AA et al. Evalua-
tion of a standardized recording tool for sputum smear micros-
copy for acid-fast bacilli under routine conditions in lowincome
countries. Int JTubercLungDis1997; 1: 33945.
19 Daniel TM. The rapid diagnosis of tuberculosis: a selective
review. JLabClinMed1990; 116: 27782.
20 World Health Organization. Global tuberculosis control: a short
update to the 2009report. WorldHealthOrganizationDocument
2009; WHO HTM TB 2009.426:148.
21 SchochOD, Rieder P, Tueller Cet al. Diagnostic yield of sputum,
inducedsputum, andbronchoscopyafter radiologictuberculosis
screening. AmJRespir Crit CareMed2007; 175: 806.
22 Greco S, Girardi E, Navarra A, Saltini C. Current evidence on
diagnostic accuracy of commercially based nucleic acid ampli-
cation tests for the diagnosis of pulmonary tuberculosis. Thorax
2006; 61: 78390.
23 Greco S, Rulli M, Girardi E, Piersimoni C, Saltini C. Diagnostic
accuracy of in-house PCR for pulmonary tuberculosis in smear-
positive patients: meta-analysis and metaregression. J Clin
Microbiol 2009; 47: 56976.
24 Sarmiento OL, Weigle KA, Alexander J, Weber DJ, Miller WC.
Assessment by meta-analysis of PCR for diagnosis of smear-
negative pulmonary tuberculosis. J Clin Microbiol 2003; 41:
323340.
25 Diel R, Loddenkemper R, Nienhaus A. Evidence-based compari-
sonof commercial interferon-gammarelease assaysfor detecting
activeTB: ametaanalysis. Chest 2010; 137: 95268.
26 NemethJ, Winkler HM, ZwickRHet al. Recruitment of Mycobac-
teriumtuberculosis specic CD4 + T cells to the site of infection
for diagnosis of active tuberculosis. J Intern Med 2009; 265:
1638.
27 BiglinoA, Crivelli P, Concialdi E, BollaC, MontrucchioG. Clinical
usefulnessof ELISPOTassay onpericardial uidinacase of sus-
pectedtuberculouspericarditis. Infection2008; 36: 6014.
28 ThomasMM, Hinks TSC, RaghuramanSet al. Rapiddiagnosis of
Mycobacteriumtuberculosis meningitis by enumeration of cere-
brospinal uid antigen-specic T-cells. Int J Tuberc Lung Dis
2008; 12: 6517.
29 WilkinsonKA, WilkinsonRJ, PathanAet al. Exvivocharacteriza-
tion of early secretory antigenic target 6-specic T cells at sites of
active disease in pleural tuberculosis. Clin Infect Dis 2005; 40:
1847.
30 Sester M, SotgiuG, Lange Cet al. Interferon-{gamma} release as-
says for the diagnosis of active tuberculosis: a systematic review
andmeta-analysis. Eur Respir J 2011; 37: 10011.
31 Chang KC, Leung CC, Yew WW, Tam CM. Supervised and in-
duced sputum among patients with smear-negative pulmonary
tuberculosis. Eur Respir J2008; 31: 108590.
C. Jafari et al.
|
Rapid diagnosis of tuberculosis
2011 The Association for the Publication of the Journal of Internal Medicine Journal of Internal Medicine 270; 254262 261
32 Bell D, Leckie V, McKendrick M. The role of induced sputum in
the diagnosis of pulmonary tuberculosis. J Infection 2003; 47:
31721.
33 McWilliamsT, WellsAU, HarrisonAC, LindstromS, CameronRJ,
FoskinE. Induced sputumand bronchoscopy inthe diagnosis of
pulmonarytuberculosis. Thorax2002; 57: 10104.
34 Lange C, SchabergT, Diel R, Greinert U. Current positionregard-
ing the diagnosis of tuberculosis. Dtsch Med Wochenschr 2006;
131: 3417.
35 Horster R, Kirsten D, Gaede KI et al. Antimycobacterial immune
responses in patients with pulmonary sarcoidosis. Clin Respir
J2009; 3: 22938.
Correspondence: Christoph Lange MD PhD, Division of Clinical
Infectious Diseases, Research Center Borstel, Parkallee 35, 23845
Borstel, Germany.
(fax: +49-4537-188-313; e-mail: clange@fz-borstel.de).
C. Jafari et al.
|
Rapid diagnosis of tuberculosis
262 2011 The Association for the Publication of the Journal of Internal Medicine Journal of Internal Medicine 270; 254262
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- Cardiovascular - 2018101851516 P. M. PDFDocument142 pagesCardiovascular - 2018101851516 P. M. PDFCintia FloresNo ratings yet
- Medicine Science or Art PDFDocument5 pagesMedicine Science or Art PDFCintia FloresNo ratings yet
- NuevoDocumento 2018-10-12 11.00.34 - 1 PDFDocument1 pageNuevoDocumento 2018-10-12 11.00.34 - 1 PDFCintia FloresNo ratings yet
- Cardiovascular - 2018101851516 P. M PDFDocument142 pagesCardiovascular - 2018101851516 P. M PDFCintia FloresNo ratings yet
- NuevoDocumento 2018-10-10 20.38.29 - 1 PDFDocument1 pageNuevoDocumento 2018-10-10 20.38.29 - 1 PDFCintia FloresNo ratings yet
- Cardiovascular - 2018101851516 P. M. PDFDocument142 pagesCardiovascular - 2018101851516 P. M. PDFCintia FloresNo ratings yet
- NuevoDocumento 2018-10-10 20.38.29 - 2 PDFDocument1 pageNuevoDocumento 2018-10-10 20.38.29 - 2 PDFCintia FloresNo ratings yet
- History PDFDocument1 pageHistory PDFCintia FloresNo ratings yet
- Libro 1Document1 pageLibro 1Cintia FloresNo ratings yet
- History PDFDocument1 pageHistory PDFCintia FloresNo ratings yet
- 2018 Article 442Document9 pages2018 Article 442Cintia FloresNo ratings yet
- 1 SM PDFDocument7 pages1 SM PDFCintia FloresNo ratings yet
- Innate Immunity and Breast MilkDocument10 pagesInnate Immunity and Breast MilkCintia FloresNo ratings yet
- Diverging Trends in Reflux and H. Pylori Cardia CancerDocument13 pagesDiverging Trends in Reflux and H. Pylori Cardia CancerCintia FloresNo ratings yet
- Jvetres 62 027 PDFDocument8 pagesJvetres 62 027 PDFCintia FloresNo ratings yet
- Diferencies BetweenDocument1 pageDiferencies BetweenCintia FloresNo ratings yet
- Human Breast Milk and The Gastrointestinal Innate System. 2014 PDFDocument13 pagesHuman Breast Milk and The Gastrointestinal Innate System. 2014 PDFCintia FloresNo ratings yet
- Factual WritingDocument1 pageFactual WritingCintia FloresNo ratings yet