Professional Documents
Culture Documents
Weaning From Mechanical Ventilation/CCM Board Review
Uploaded by
AzmachamberAzmacareOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
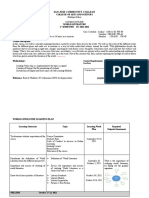
Weaning From Mechanical Ventilation/CCM Board Review
Uploaded by
AzmachamberAzmacareCopyright:
Available Formats
L|beranon from mechan|ca|
venn|anon
John F. McConville, M.D.
Associate Professor
University of Chicago
D|sc|osure
no conlcLs of lnLeresL Lo dlsclose
Objectives:
Pinpoint patient readiness for spontaneous
breathing trials (SBT)
List criteria for passing an SBT
Identify non-ventilator strategies for reducing
duration of mechanical ventilation
A. RR: 40 and Vt: 250 ml after 1 min CPAP of 5 cmH
2
O
B. MV settings of AC 20/450/12/60%
C. BP of 90/45 mmHg on norepinephrine, vasopressin,
dobutamine
D. 65 yr old male with lung cancer, pneumonia, acute
renal failure, and CHF on CXR with a RR of 30 and
Vt of 300 ml after 1 min CPAP (5 cmH2O)
Audience Response Question
Whlch of Lhe followlng condluons
suggesLs readlness for a S81?
Mechanical ventilation: Primary
prevention
! EGDT in the initial treatment of sepsis
! Use of NIV in selected patients with:
AECOPD
Acute cardiogenic pulmonary edema
Rivers. N Engl J Med. 2001; 345:13681377.
Brochard. N Engl J Med 1995;333:817-822.
Masip. JAMA. 2005;294:3124-3130.
Gray. N Engl J Med. 359;(24): 142-151.
McConville JF, Kress JP. N Engl J Med 2012;367:2233-2239
Intubation
Tx RF etiology
Extubation
liberation duration
MV International Study Group
!AMA 2002,287:343-333.
69% Acute respiratory failure
post-surgical, pneumonia, CHF, sepsis, trauma, ARDS
Intubation
Tx RF etiology
Extubation
liberation duration
Duration of time on MV
60% 40%
Esteban Chest 1994;106:1186
Esteban JAMA 2002;287:345
Esteban AJRCCM 2008;177:170
136 brain injury-MV pts. Readiness criteria daily
Extubation delay = days b/t readiness and extubation
Complications of MV
Coplin AJRCCM 2000;162:1530
0
5
10
15
20
25
30
35
40
Pneum (%) Mortality
(%)
Hosp LOS
Delay (37/136) No delay (99/136)
Intubation
Tx of RF
Extubation
Liberation duration
GOAL: minimize time on MV
1970 through early 1980s
Weaning = disconnect patients from MV
for gradually increasing periods
Predictors sought to identify earliest time
a patient could resume spontaneous
breathing
Yang and Tobin NEJM 1991;324:1445-50.
Frequency/tidal volume ratio (f/Vt)
Calculated during a 1 minute spontaneous
breathing trial (SBT)
Ratio of < 105 best determines success
If clinical equipoise about SBT success
" f/Vt of 80 # LR of 7.5 and 95% success rate
Weaning predictors
Meade Chest 2001;120:400S
Systematic review and meta-
analysis
51 weaning predictors
Take home:
No ideal predictors for liberation readiness
5 predictors minimally helpful
NIF, VE, Vt, RR and f/Vt
Intermittent mandatory ventilation (IMV)
had replaced disconnecting MV for short
periods time as the primary means of
weaning
By the mid 1980s
1990s: Mode of weaning studies
Brochard and Esteban studies
1002 medical surgical MV patients
SIMV vs. PSV vs. T-piece
Brochard AJRCCM 1994;150:896-903
Esteban NEJM 1995;332:345-350
76% passed the initial SBT
Mode of weaning studies
Duration of weaning (days)
Brochard AJRCCM 1994;150:896-903
Esteban NEJM 1995;332:345-350
300 adult patients
Intervention group received
- daily screen respiratory function
- SBT: if passed # M.D. notified
Control pts were screened daily
Ely NEJM 1996;335:1864-1869
When can they breathe?
To pass screen test:
PaO
2
:FiO
2
ratio >200
PEEP ! 5
adequate cough
no vasopressor or sedatives in use
f/Vt ratio ! 105 during 1 min CPAP 5 cmH
2
0
Ely NEJM 1996;335:1864-1869
2 hour SBT on CPAP of 5 cm H
2
0
SBT terminated if:
RR > 35 for more than 5 minutes
O
2
% < 90%
HR > 140/min
sustained " in HR by 20%
SBP > 180 mmHg or < 90 mmHg
increased anxiety or diaphoresis
Ely NEJM 1996;335:1864-1869
P
t
s
o
n
M
V
(
%
)
Days after passed screen
Intervention group was sicker ( higher APACHE and LIS)
Median duration of MV until successful screen
test# 3 vs. 2 days (intervention and control)
Ely NEJM 1996;335:1864-1869
Decreased in intervention group:
Duration of MV
Reintubation rate
Cost of ICU stay
Ely NEJM 1996;335:1864-1869
roLocols: noL Always 8euer
Lecuve
MlCu/SlCu: kollef CCM '97, Marellch ChesL '00
L1AC: vlLacca A!8CCM '01, Schelnhorn ChesL '01
noL Superlor
nuSu: namen A!8CCM '01
eds: 8andolph !AMA '03
Academlc, well-sLaed MlCu: krlshnan A!8CCM '04
Take home points
Most patients can be liberated
quickly
Systematic approaches are needed
Physicians are bad at recognizing
when the weaning period begins
Assess readiness early
Whlch of Lhe followlng sLaLemenLs
abouL a S81 ls false?
A. Successful 30 mln S81 suggesLs adequaLe sLrengLh for
llberauon
8. valldaLed for 1-plece, Sv, or CA
C. A pauenL wlLh 88 of 30 and vL of 300ml aer a 60
mlnuLe S81 should noL be llberaLed
u. 8esL lf performed wlLh an alerL pauenL o sedauon
L. PosplLal morLallLy ls lncreased ln pLs falllng 3 S81s
Audience Response Question
What mode for SBT
T-piece = PSV 7 cm H
2
O
T-piece: 78% liberated and 38 reintubated
PSV: 86% liberated and 36 reintubated
Esteban AJRCCM 1997;156:459
Esteban AJRCCM 1999;159:512
30 min SBT = 120 min SBT
88% and 85% passed
13.5% and 13.4% reintubated
Duration of SBT
Patients are ready to breathe earlier
than we think
Systematic approach is much more
important than SBT mode and
duration
SBT summary
Why do patients fail SBTs?
Worsening respiratory mechanics
increased respiratory resistance
decreased lung compliance
gas trapping
Cardiac etiology
Tobin AJRCCM 1997;155:906-15
McConville JF, Kress JP. N Engl J Med 2012;367:2233-2239
Load > Strength
Why do patients fail SBTs?
8reaLhlng Challenges Lhe Clrculauon
- 19 hemodynamlcally sLable,
venulaLed sub[ecLs
- S81 (1-plece) for 60 mlnuLes
- lallures lncreased C
2
exLracuon whlle successes
lncrease C
1
Jubran AJRCCM 1998; 158:1763
Why do patients fail SBTs?
S
v
O
2
(
%
)
Weaning classification
Boles ERJ 2007;29:1033-1056
Simple: 1
st
SBT & liberation successful
Difficult: requires up to 3 SBTs
< 7 days 1
st
SBT to liberation
Prolonged: fail at least 3 SBTs or
> 7 days weaning after 1
st
SBT
Weaning classification
Funk ERJ 2010;35:88-94
257 patients prospective study
Simple: 59% # 13% hospital mortality
Difficult: 26% # 9% hospital mortality
Prolonged: 14% # 32% hospital
mortality
Other factors effecting liberation
Sedation strategies
- medications
- interruption
Timing of awakening and SBT
Physical therapy
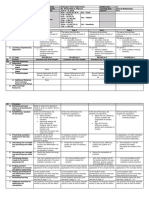
k|chmond Ag|tanon Sedanon Score (kASS)
+4 Combanve Combanve, v|o|ent, danger to sta
+3 Very Ag|tated u||s or removes tubes, aggress|ve
+2 Ag|tated Ireq non-purposefu| movement,
hghts venn|ator
+1 kest|ess Anx|ous, but movements not aggress|ve or v|gorous
0 A|ert and Ca|m
-1 Drowsy Not fu||y a|ert, susta|ned awaken|ng vo|ce (eye
open|ng]contact >10 sec)
-2 L|ght Sedanon 8r|ey awakens to vo|ce
(eye open|ng and contact<10sec)
-3 Mod Sedanon Movement or eye open to vo|ce
-4 Deep Sedanon No response to vo|ce, but movement or eye
open|ng to phys|ca| snmu|anon
-S Unarousab|e No response to vo|ce of phys|ca| snm.
Wake Up! Daily Sedation Interruption
Kress NEJM 2000;342:1471
Intervention
(wake-up)
Control P
value
N 68 60
MV duration, d 4.9 (2.5-8.6) 7.3 (3.4-16.1) 0.004
ICU LOS, d 6.4 (3.9-12.0) 9.9 (4.7-17.9) 0.02
Hosp LOS, d 13.3 (7.3-20.0) 16.9 (8.5-26.6) 0.19
Clrard LanceL 2008, 371:126-134
Wake up! And breathe.
SBT only SAT +SBT p value
n = 168 167
Vent free
days
11.7 14.8 0.01
Duration of
MV (days)
6.0 4.8 0.02
ICU LOS 12.8 9.1 0.02
Hosp LOS 19 14.8 0.04
Self
Extubation
6 16 0.03
SchwelckerL LanceL 2009, 373:1874-1882
Wake up! And move?
Intervention Patients
Daily passive ROM and PT/OT
Control Patients
PT and OT per primary team
Both groups received protocol-directed
SBT
Daily sedation interruption
Nutrition
Glycemic control
Outcome
Intervention
(n = 49)
Control
(n = 55) P value
Ventilator-free days 23.5 [7.4,25.6] 21.1 [0.0,23.8] 0.05
MV duration, days 3.4 [2.3,7.3] 6.1 [4.0,9.6] 0.02
ICU LOS, days 5.9 [4.5,13.2] 7.9 [6.1,12.9] 0.08
Hospital LOS, days 13.5 [8.0,23.1] 12.9 [8.9,19.8] 0.93
Hospital mortality, % 18 26 0.53
Wake up! And move?
SchwelckerL LanceL 2009, 373:1874-1882
Take home points
Stop sedation every day
SBT early! (awake if possible)
Awakening and Breathing Coordination,
Delirium monitoring, Early mobilization
and Exercise # ABCDE approach
How to reduce duration of MV
Daily interruption of sedative infusions
Paired interruption of sedatives and SBT
Early physical and occupational therapy
No sedative use in MV patients
ARDS
$ Vt of 6ml/kg (ideal body weight)
$ Conservative fluid strategy
$ Prone positioning
$ Early paralysis
Strategies to reduce VAP
N Engl J Med 2000, 342:1301-1308.
Strm. Lancet. 2010; 375: 475-480.
N Engl J Med. 2006; 354: 1-12.
N Engl J Med 2010, 363:1107-1116.
N Engl J Med. 2013; 368: 2159-2168.
Dezfulian. A. J. Med. 2005;118,11-18
Whlch sLaLemenL ls false?
Audience Response Question
A. 8e-lnLubauon ls assoclaLed wlLh lncreased morLallLy
8. neumonla pauenLs requlrlng Mv are aL an lncreased
rlsk of llberauon fallure desplLe passlng an S81
C. Medlcal lCu pauenLs are more llkely Lo fall llberauon
auempLs Lhan surglcal lCu pauenLs
u. A Lrlal of nlv ls recommended for pauenLs
developlng resplraLory dlsLress 18 hours posL-llberauon
Mode of weaning studies: part II
Computer driven weaning
automated reduction in PSV based on
continuous evaluation of:
RR, Vt and end-tidal CO
2
Computer driven weaning
Closed-loop, automated system (Drger Smartcare)
- 144 Subjects: SBT when minimal PSV achieved
- Reduced weaning time (median 5.0 v 3.0d),
days ventilated, ICU LOS
Lellouche et.al: Am J Respir Crit Care Med 174: 894, 2006
1he same auLomaLed, closed-loop sysLem
- 102 pauenLs
- no dlerence ln wean durauon, hrs venulaLed
Rose L: Intensive Care Med 34:1788; 2008
Extubation failure
0
2
4
6
8
10
12
14
16
18
MICU
Mixed
Peds
SICU
CTS
Trauma
Neuro
%
p
a
t
i
e
n
t
s
e
x
t
u
b
a
t
e
d
N~ 35,000 (60 studies)
LpsLeln Sk. !"#$%& ()&"* 2009,34(2):198 -208.
Extubation failure = increased mortality
0
10
20
30
40
50
60
70
Death ICU LOS Home
Failure Success
LpsLeln ChesL 1997,112,186
Liberation readiness vs. SBT success
auenLs passed a 30-60 mln S81
eak cough ow < 60L/mln: 88 4.8
Secreuons > 2.3 mL/h: 88 3.0
Can'L compleLe 4 slmple commands: 88 4.3
All 3: 88 23 (100 fallure)
none: 3 fallure
Salam: Intensive Care Med 30:1334; 2004
37 ICUs in 8 countries
Liberation failure in 121 of 900 pts (13.4%)
Logistic regression identified:
f/Vt (OR 1.009 per unit)
+ fluid balance in 24 hr prior (OR 1.70)
MV for pneumonia (OR 1.77)
Frutos-Vivar Chest 2006;130:1664
Liberation readiness vs. SBT success
Frutos-Vivar Chest 2006;130:1664
R
e
i
n
t
u
b
a
t
i
o
n
r
a
t
e
(
%
)
f/Vt ratio
Liberation readiness vs. SBT success
Frutos-Vivar Chest 2006;130:1664
R
e
i
n
t
u
b
a
t
i
o
n
r
a
t
e
(
%
)
Fluid balance
Liberation readiness vs. SBT success
NIPPV in liberation failure
Post liberation respiratory distress
- Keenan, JAMA 2002 # NO
- Esteban, NEJM 2004 # NO
Preventive for high risk patients
- Nava, CCM 2005 # YES
- Ferrer, AJRCCM 2006 # YES
Failure of more than one consecutive SBT
Chronic heart failure
P
a
CO
2
> 45 mmHg after extubation
More than one co-morbidity other than heart
failure
Weak cough
Upper airway stridor at extubation
Age > 65
APACHE II score > 12 on the day of extubation
Medical, pediatric or multispecialty ICU patient
Pneumonia as etiology of respiratory failure
Risk factors for liberation failure
Time to reintubation likely matters
Time to reintubation (hrs) Deaths (%)
0-12 24
13-24 39
25-48 50
49-72 69
Epstein. AJRCCM. 1998; 158:489493.
Assess kead|ness
SLable 8
/l >200 on LL < 3 cmP20
Lxtubate
Iu|| Venn|atory Support
Airway
Cough
Secretions
Mentation
Define
mechanism
of failure
and treat
Not SIMV
Progressive withdrawal vs. SBT
RT-RN
Driven
Protocol
30-120 m|n S81
S < 7, CA = 3, or 1-plece
Sllde adapLed from Creg SchmldL, M.u.
Summary of key o|nts
Assess readlness" every day
MosL pauenLs can be llberaLed qulckly
hyslclans are bad aL recognlzlng when
Lhe weanlng perlod" beglns
S81 success = llberauon readlness /
kecommended kead|ng and Add|nona|
kesources
Yang and Tobin. NEJM 1991;324:1445
Meade. Chest 2001;120:400S
Ely. NEJM 1996;335:1864-1869
MacIntyre. Chest. 2001 120: 375S-396S.
Girard. Lancet 2008, 371:126-134
Salam. Intensive Care Med 2004, 30:1334-1339
Esteban. NEJM 2004,350:2452-2460
Nava. CCM 2006,33:2465-2479
Cuesuons?
You might also like
- SEEK/Pulmonary Board ReviewDocument102 pagesSEEK/Pulmonary Board ReviewAzmachamberAzmacare100% (2)
- Mechanical Ventilation/CCM Board ReviewDocument45 pagesMechanical Ventilation/CCM Board ReviewAzmachamberAzmacareNo ratings yet
- Infective Endocarditis: A Multidisciplinary ApproachFrom EverandInfective Endocarditis: A Multidisciplinary ApproachArman KilicNo ratings yet
- Internation Classification ICSD III BetaDocument8 pagesInternation Classification ICSD III BetaRikizu HobbiesNo ratings yet
- Liberation From Mechanical VentilationDocument21 pagesLiberation From Mechanical VentilationRins Chacko50% (2)
- Miller's Anesthesia, 8th Edition: Anesthesiology April 2016Document3 pagesMiller's Anesthesia, 8th Edition: Anesthesiology April 2016Sabbir AhammedNo ratings yet
- SEEK/Pulmonary Board ReviewDocument34 pagesSEEK/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Teaching Debate To ESL Students - A Six-Class Unit (TESL - TEFL)Document9 pagesTeaching Debate To ESL Students - A Six-Class Unit (TESL - TEFL)Kristen FieldsNo ratings yet
- SteelDocument23 pagesSteelMelinda GordonNo ratings yet
- Guideline, Research WritingDocument70 pagesGuideline, Research WritingBilal Kemal89% (18)
- Coma-Delirium in ICU/CCM Board ReviewDocument61 pagesComa-Delirium in ICU/CCM Board ReviewAzmachamberAzmacareNo ratings yet
- Exercise Testing/Pulmonary Board ReviewDocument42 pagesExercise Testing/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Waveform Questions /critical Care Board ReviewDocument14 pagesWaveform Questions /critical Care Board ReviewAzmachamberAzmacareNo ratings yet
- Shock/CCM Board ReviewDocument60 pagesShock/CCM Board ReviewAzmachamberAzmacareNo ratings yet
- Principles and Practice of Pharmacology for AnaesthetistsFrom EverandPrinciples and Practice of Pharmacology for AnaesthetistsRating: 5 out of 5 stars5/5 (1)
- Perioperative Medicine: Medical Consultation and Co-managementFrom EverandPerioperative Medicine: Medical Consultation and Co-managementAmir K. JafferNo ratings yet
- Evidence-Base ICU Care/CCM Board ReviewDocument61 pagesEvidence-Base ICU Care/CCM Board ReviewAzmachamberAzmacareNo ratings yet
- Ethics/Pulmonary Board ReviewDocument43 pagesEthics/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- ICU Imaging/CCM Board ReviewDocument46 pagesICU Imaging/CCM Board ReviewAzmachamberAzmacareNo ratings yet
- Anesthesia for Congenital Heart DiseaseFrom EverandAnesthesia for Congenital Heart DiseaseStephen A. StayerNo ratings yet
- Asthma and Lung MassDocument4 pagesAsthma and Lung MassAzmachamberAzmacareNo ratings yet
- Hypersensitivity Pneumonia in BakerDocument3 pagesHypersensitivity Pneumonia in BakerAzmachamberAzmacareNo ratings yet
- Pulsus Paradoxus - Wikip PDFDocument4 pagesPulsus Paradoxus - Wikip PDFAniket MittalNo ratings yet
- ACCPCritical Care Medicine Board ReviewDocument491 pagesACCPCritical Care Medicine Board ReviewdianaMDNo ratings yet
- Environmental Occupational /part 1/pulmonary Board ReviewDocument55 pagesEnvironmental Occupational /part 1/pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Regional Nerve Blocks And Infiltration Therapy: Textbook and Color AtlasFrom EverandRegional Nerve Blocks And Infiltration Therapy: Textbook and Color AtlasDanilo JankovicNo ratings yet
- Acquired Platelet Dysfunction in a Child with Chronic Renal FailureDocument100 pagesAcquired Platelet Dysfunction in a Child with Chronic Renal FailureEli EidNo ratings yet
- Evidence-Based Obstetric AnesthesiaFrom EverandEvidence-Based Obstetric AnesthesiaStephen H. HalpernNo ratings yet
- Rational fluid and volume therapy in anaesthesia and intensive care medicineFrom EverandRational fluid and volume therapy in anaesthesia and intensive care medicineNo ratings yet
- Perioperative Neuroscience: Translational ResearchFrom EverandPerioperative Neuroscience: Translational ResearchHemanshu PrabhakarNo ratings yet
- Fungal Diseases/Pulmonary Board ReviewDocument54 pagesFungal Diseases/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Pulmonary EmbolismDocument2 pagesPulmonary EmbolismArijit ChakravortyNo ratings yet
- Anesthesia Considerations for Microlaryngoscopy and Direct LaryngoscopyDocument6 pagesAnesthesia Considerations for Microlaryngoscopy and Direct LaryngoscopyRubén Darío HerediaNo ratings yet
- AnaesthesiaDocument8 pagesAnaesthesiarakeeb qadriNo ratings yet
- Infectious Disease Questions/Critical Care Board ReviewDocument5 pagesInfectious Disease Questions/Critical Care Board ReviewAzmachamberAzmacareNo ratings yet
- Ventilatory crisis/CCM Board ReviewDocument48 pagesVentilatory crisis/CCM Board ReviewAzmachamberAzmacareNo ratings yet
- 1996 Ite ExamDocument72 pages1996 Ite Exampiano543No ratings yet
- Rapid Sequence Intubation and Cricoid PressureDocument16 pagesRapid Sequence Intubation and Cricoid PressureErlin IrawatiNo ratings yet
- Pulmo ThromboembolismDocument34 pagesPulmo ThromboembolismAlexander Santiago ParelNo ratings yet
- Resp Physio SAQsDocument25 pagesResp Physio SAQsanaeshkl100% (1)
- Essay 3 Final DraftDocument6 pagesEssay 3 Final Draftapi-360460383No ratings yet
- Perioperative Medication Management - UpToDateDocument46 pagesPerioperative Medication Management - UpToDateEvy Alvionita YurnaNo ratings yet
- Exam ANS Report Final2022 1 PRVDocument18 pagesExam ANS Report Final2022 1 PRVtestingNo ratings yet
- Should We Use Driving Pressure To Set Tidal Volume? PDFDocument7 pagesShould We Use Driving Pressure To Set Tidal Volume? PDFYaxkin NikNo ratings yet
- Arterial Blood Gas Case Questions AnalyzedDocument4 pagesArterial Blood Gas Case Questions AnalyzedAnandNo ratings yet
- Captopril Renography - Detect Renal Artery StenosisDocument3 pagesCaptopril Renography - Detect Renal Artery StenosisSri HariNo ratings yet
- Copy-Question PapersDocument87 pagesCopy-Question Paperspooja patilNo ratings yet
- Surgical Cricothyrotomy (Assist)Document5 pagesSurgical Cricothyrotomy (Assist)ydtrgnNo ratings yet
- Cabg Vs OpcabDocument17 pagesCabg Vs OpcabVijay AnandNo ratings yet
- Capnography Guidance for CPR EffectivenessDocument25 pagesCapnography Guidance for CPR EffectivenessDaniel CrookNo ratings yet
- Interventional Pulmonology in 2015: A Survey of Practice Patterns and Future Directions of This Emerging FieldDocument4 pagesInterventional Pulmonology in 2015: A Survey of Practice Patterns and Future Directions of This Emerging FieldPeertechz Publications Inc.No ratings yet
- OSA and Periop Complications 2012Document9 pagesOSA and Periop Complications 2012cjbae22No ratings yet
- Poisonings and overdose/CCM Board ReviewDocument61 pagesPoisonings and overdose/CCM Board ReviewAzmachamberAzmacareNo ratings yet
- Telegram Cloud Document 4 5893461163299045618 PDFDocument232 pagesTelegram Cloud Document 4 5893461163299045618 PDFAndreea FlorinaNo ratings yet
- Summer 2016 MCQDocument16 pagesSummer 2016 MCQDaniel CoyleNo ratings yet
- Recruitment Maneuvers and PEEP TitrationDocument17 pagesRecruitment Maneuvers and PEEP TitrationDiego Cruces OrdoñezNo ratings yet
- The RUSH Exam - Rapid Ultrasound in SHock in The Evaluation of The Critically LLLDocument28 pagesThe RUSH Exam - Rapid Ultrasound in SHock in The Evaluation of The Critically LLLCARLOSNo ratings yet
- Prehospital Anesthesia HandbookDocument46 pagesPrehospital Anesthesia HandbookoscarNo ratings yet
- The Hong Kong College of Anaesthesiologists Final Fellowship Examination July/September 2007 Examiners ReportDocument16 pagesThe Hong Kong College of Anaesthesiologists Final Fellowship Examination July/September 2007 Examiners ReportJane KoNo ratings yet
- AHA Statement-Cardiopulmonary Impact of E-Cigarettes and Vaping-2023Document26 pagesAHA Statement-Cardiopulmonary Impact of E-Cigarettes and Vaping-2023Walter ReyesNo ratings yet
- Anaesthesia For Carotid EndarterectomyDocument19 pagesAnaesthesia For Carotid EndarterectomyFahran HakeemNo ratings yet
- 1) Vasoplegia During Cardiac Surgery Current Concepts and Management 2010Document5 pages1) Vasoplegia During Cardiac Surgery Current Concepts and Management 2010Carolina QuirogaNo ratings yet
- Quality Safety Complications/Pulmonary Board ReviewDocument135 pagesQuality Safety Complications/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Acid Base Disorders/Pulmonary Board ReviewDocument75 pagesAcid Base Disorders/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Mycobacterium/Pulmonary Board ReviewDocument59 pagesMycobacterium/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Thromboembolic Disease/Pulmonary Board ReviewDocument60 pagesThromboembolic Disease/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Unusual Lung Infect Bronch & CF/Pulmonary Board ReviewDocument87 pagesUnusual Lung Infect Bronch & CF/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Asthma/Pulmonary Board ReviewDocument66 pagesAsthma/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- CAP/Pulmonary Board ReviewDocument64 pagesCAP/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Bronch IP/Pulmonary Board ReviewDocument73 pagesBronch IP/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- SEEK/Pulmonary Board ReviewDocument101 pagesSEEK/Pulmonary Board ReviewAzmachamberAzmacare100% (1)
- HAP/Pulmonary Board ReviewDocument80 pagesHAP/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Pulmonary Hypertension/Pulmonary Board ReviewDocument66 pagesPulmonary Hypertension/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Vasculitis & Alveolar Hemorrhage/Pulmonary Board ReviewDocument62 pagesVasculitis & Alveolar Hemorrhage/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- COPD - I/Pulmonary Board ReviewDocument68 pagesCOPD - I/Pulmonary Board ReviewAzmachamberAzmacare100% (1)
- Cellular Biology and Immunology/Pulmonary Board ReviewDocument68 pagesCellular Biology and Immunology/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Diffues Lung Disease I/Pulmonary DBoard ReviewDocument184 pagesDiffues Lung Disease I/Pulmonary DBoard ReviewAzmachamberAzmacare100% (1)
- Copd /pulmonary Board ReviewDocument68 pagesCopd /pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Diffuse Lung Disease II/Pulmonary Board ReviewDocument181 pagesDiffuse Lung Disease II/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Unusual and Uncommon Pulmonary Disorder/pulmonary Board ReviewDocument68 pagesUnusual and Uncommon Pulmonary Disorder/pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Mediastinal & Other Neoplasms/Pulmonary Board ReviewDocument86 pagesMediastinal & Other Neoplasms/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Sleep Science Polysomnography/Pulmonary Board ReviewDocument154 pagesSleep Science Polysomnography/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Sleep Disorders - I/Pulmonary Board ReviewDocument87 pagesSleep Disorders - I/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Ethics/Pulmonary Board ReviewDocument43 pagesEthics/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Sleep Disorders II/Pulmonary Board ReviewDocument106 pagesSleep Disorders II/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- PFT Excercise Testing Case Studies/pulmonary Board ReviewDocument64 pagesPFT Excercise Testing Case Studies/pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Pleural Diseases I & II/Pulmonary Board ReviewDocument181 pagesPleural Diseases I & II/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Women's Issues in Pulmonary Medicine/Pulmonary Board ReviewDocument67 pagesWomen's Issues in Pulmonary Medicine/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- Eosinophilic Lung Disease/Pulmonary Board ReviewDocument51 pagesEosinophilic Lung Disease/Pulmonary Board ReviewAzmachamberAzmacareNo ratings yet
- 2nd Sem Result MbaDocument2 pages2nd Sem Result MbaPrem KumarnNo ratings yet
- Veena Kumawat CVDocument1 pageVeena Kumawat CVVeena KumavatNo ratings yet
- (ACV-S06) Week 06 - Pre-Task - Quiz - Weekly Quiz (PA) - INGLES IV (36824)Document5 pages(ACV-S06) Week 06 - Pre-Task - Quiz - Weekly Quiz (PA) - INGLES IV (36824)Gianfranco Riega galarzaNo ratings yet
- Software Engg. Question Paper - 40 CharacterDocument14 pagesSoftware Engg. Question Paper - 40 Characteranon_572289632No ratings yet
- Differianted Math Lesson Plan Triangular Prisms - Diego MenjivarDocument4 pagesDifferianted Math Lesson Plan Triangular Prisms - Diego Menjivarapi-491433072No ratings yet
- San Jose Community College: College of Arts and SciencesDocument5 pagesSan Jose Community College: College of Arts and SciencesSH ENNo ratings yet
- Jipmer MbbsDocument3 pagesJipmer MbbsHari SreenivasanNo ratings yet
- Conceptual Framework: Dr. Fariza KhalidDocument23 pagesConceptual Framework: Dr. Fariza KhalidrameshNo ratings yet
- Nishan Singh's Education and Career ProfileDocument2 pagesNishan Singh's Education and Career Profileshahid aliNo ratings yet
- Lamm, J. Schleiermacher's PlatoDocument278 pagesLamm, J. Schleiermacher's PlatonicodeloNo ratings yet
- Core OM - Term 1 - 2019Document5 pagesCore OM - Term 1 - 2019chandel08No ratings yet
- Weekly Report, Literature Meeting 2Document2 pagesWeekly Report, Literature Meeting 2Suzy NadiaNo ratings yet
- Reflection On Idealism and Realism in EducationDocument2 pagesReflection On Idealism and Realism in EducationDiana Llera Marcelo100% (1)
- Learn Culture, Society & Politics (Part 1: CultureDocument2 pagesLearn Culture, Society & Politics (Part 1: Cultureramil quilasNo ratings yet
- Chapter 1-5 Teacher-Attributes (Full Research)Document26 pagesChapter 1-5 Teacher-Attributes (Full Research)Honeyvel Marasigan BalmesNo ratings yet
- Grade 11 Math Lesson Log on FunctionsDocument4 pagesGrade 11 Math Lesson Log on FunctionsMardy Nelle Sanchez Villacura-Galve100% (2)
- CPDProgram Nurse 111919 PDFDocument982 pagesCPDProgram Nurse 111919 PDFbrikgimNo ratings yet
- Paket MK Rejoin 2022 (Last Udpate)Document23 pagesPaket MK Rejoin 2022 (Last Udpate)Eric PrayogaNo ratings yet
- Unit Summary: Superheroes Making A DifferenceDocument2 pagesUnit Summary: Superheroes Making A DifferenceIvan ICNo ratings yet
- Boost Teacher Effectiveness with School Learning Action Cell (SLAC) PlanDocument5 pagesBoost Teacher Effectiveness with School Learning Action Cell (SLAC) PlanKashmier Taylor Celis100% (1)
- Budget Proposal TVL SampleDocument4 pagesBudget Proposal TVL SampleScarlette Beauty EnriquezNo ratings yet
- Simulations A Tool For Testing Virtual Reality in The Language ClassroomDocument10 pagesSimulations A Tool For Testing Virtual Reality in The Language ClassroomSyed Qaiser HussainNo ratings yet
- Pre-Coaching Questionnaire For ExecutivesDocument2 pagesPre-Coaching Questionnaire For ExecutivesNatalie BrownNo ratings yet
- Group CohesivenessDocument26 pagesGroup CohesivenessRaviWadhawanNo ratings yet
- Smart Lesson Plan WwiiDocument3 pagesSmart Lesson Plan Wwiiapi-302625543No ratings yet
- Shaurya Brochure PDFDocument12 pagesShaurya Brochure PDFAbhinav ShresthNo ratings yet
- Hang Out 5 - Unit Test 8Document2 pagesHang Out 5 - Unit Test 8Neila MolinaNo ratings yet