Professional Documents
Culture Documents
10 Principle in Medical Documentation
Uploaded by
KKCDIALCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 Principle in Medical Documentation
Uploaded by
KKCDIALCopyright:
Available Formats
10 Principles of Documentation for Medical
Records
From the Centers for Medicare and Medicaid Services and TrailBlazer Health Enterprises,
LLC
1. The medical record should be complete and legible.
2. The documentation of each patient encounter should include:
the date;
the reason for the encounter;
appropriate history and physical exam in relationship to the patients chief complaint;
review of lab, x-ray data and other ancillary services, where appropriate;
assessment; and
a plan for care (including discharge plan, if appropriate)
3. Past and present diagnoses should be accessible to the treating and/or consulting physician.
4. The reasons for and results of x-rays, lab tests and other ancillary services should be
documented or included in the medical record.
5. Relevant health risk factors should be identified
6. The patients progress, including response to treatment, change in treatment, change in
diagnosis, and patient non-compliance, should be documented.
7. The written plan for care should include, when appropriate:
treatments and medications, specifying frequency and dosage;
any referrals and consultations;
patient/family education; and
specific instructions for follow-up.
8. The documentation should support the intensity of the patient evaluation and/or the treatment,
including through processes and the complexity of medical decision-making s it relates to the
patients chief complaint for the encounter.
9. All entries to the medical record should be dated and authenticated.
10. The CPT/ICD-9-CM codes reported on the CMS-1500 claim form should reflect the
documentation in the medical record.
Medical record
From Wikipedia, the free encyclopedia
This article is about the documentation of a patient's medical history. For digital records, see
electronic medical record and electronic health record. For the New York journal published by
the Washington Institute of Medicine, see Medical Record (journal). For the BBC Radio 4
medical programme, see Case Notes (radio show).
The terms medical record, health record, and medical chart are used somewhat
interchangeably to describe the systematic documentation of a single patient's medical history
and care across time within one particular health care provider's jurisdiction.
[1]
The medical
record includes a variety of types of "notes" entered over time by health care professionals,
recording observations and administration of drugs and therapies, orders for the administration of
drugs and therapies, test results, x-rays, reports, etc. The maintenance of complete and accurate
medical records is a requirement of health care providers and is generally enforced as a licensing
or certification prerequisite.
The terms are used for both the physical folder that exists for each individual patient and for the
body of information found therein.
Medical records have traditionally been compiled and maintained by health care providers, but
advances in online data storage have led to the development of personal health records (PHR)
that are maintained by patients themselves, often on third-party websites.
[2]
This concept is
supported by US national health administration entities
[3]
and by AHIMA, the American Health
Information Management Association.
[4]
importance
A medical record folder being pulled from the records
Because many consider the information in medical records to be sensitive personal information
covered by expectations of privacy, many ethical and legal issues are implicated in their
maintenance, such as third-party access and appropriate storage and disposal.
[5]
Although the
storage equipment for medical records generally is the property of the health care provider, the
actual record is considered in most jurisdictions to be the property of the patient, who may obtain
copies upon request.
Importance of Documentation
Medical record documentation is required to record pertinent facts, findings, and observations
about an individuals health history including the past and present illnesses, examinations, tests,
treatments, and outcome. The medical record chronologically documents the care of the patient
and is an important element contributing to high quality care. The medical record should be
complete and legible. Proper documentation facilitates:
The ability of the physician and other health care professionals to evaluate and plan the
patients immediate treatment, and to monitor his/her health care over time.
Communication and continuity of care among the physicians and other health care professionals
involved in the patient care.
Accurate and timely claims review and payment.
Appropriate utilization review and quality of care evaluations.
Collection of data that may be used for research and education.
Basic Principles of Documentation:
Documentation of each patient encounter should include or provide reference to:
Chief complaint and/or reason for the encounter.
Relevant history, examination findings and prior diagnostic test results.
Assessment, clinical impression or diagnosis and plan of care.
Date and legible identity of health care professional.
The CPT and ICD-9-CM codes reported on the health insurance claim form or billing statement
must be supported by the documentation in the medical record.
The confidentiality of the medical record should be fully maintained consistent with the
requirements of medical ethics and of law.
purpose
Primary Purpose of a Medical Record
Are we losing sight of the primary purpose of a patient medical record, which is to support
patient care?
Narrative notes serve several purposes by helping physicians and other caregivers:
1. Decide upon the appropriate course of care and provide rationale
2. Create context for a patients story, and make one patient memorable from the next
3. Provide continuity of care over time and among clinicians
4. Communicate with referring and consulting colleagues
The most important part of the medical record is the physicians narrative note, which documents
the thought process for why a course of treatment is decided upon after each patient encounter.
Narrative notes also provide a useful summary of the other information contained in a medical
record, such as the results of labs, imaging and other diagnostic tests.
Over time, the medical record has been commandeered for other purposes, most notably as a
legal record of care provided and as the basis for insurance billing and payment.
Although clinical documentation plays a central role in EHRs and occupies a substantial
proportion of physicians time, documentation practices have largely been dictated by billing
and legal requirements. Yet the primary role of documentation should be to clearly describe
and communicate what is going on with the patient.
Gordon Schiff, MD & David Bates, MD -- NEJ M 25 Mar 2010
You might also like
- Ahima Data Quality Management ModelDocument11 pagesAhima Data Quality Management Modelselinasimpson2301No ratings yet
- Textbook of Urgent Care Management: Chapter 42, Evaluation and Management of Coding and DocumentationFrom EverandTextbook of Urgent Care Management: Chapter 42, Evaluation and Management of Coding and DocumentationNo ratings yet
- Clinical Audit ToolkitDocument41 pagesClinical Audit ToolkitDewi Ratna Sari100% (1)
- DocumentationDocument13 pagesDocumentationNathaniel Karl Enin Pulido100% (1)
- Cracking the Code: A quick reference guide to interpreting patient medical notesFrom EverandCracking the Code: A quick reference guide to interpreting patient medical notesNo ratings yet
- Clinical Documentation and RA CodingDocument24 pagesClinical Documentation and RA CodingVANESSANo ratings yet
- Healthcare Environmental Services A Complete Guide - 2020 EditionFrom EverandHealthcare Environmental Services A Complete Guide - 2020 EditionNo ratings yet
- Assessment TelephoneDocument5 pagesAssessment TelephoneWidfdsafdsaNo ratings yet
- Patient Safety Organization A Complete Guide - 2020 EditionFrom EverandPatient Safety Organization A Complete Guide - 2020 EditionNo ratings yet
- @@assessment of Medical Documentation As Per Joint Commission InternationDocument6 pages@@assessment of Medical Documentation As Per Joint Commission InternationNahari ArifinNo ratings yet
- Clinical ValidationDocument39 pagesClinical ValidationMohammed HammedNo ratings yet
- Cdip - 4Document58 pagesCdip - 4SURESHNo ratings yet
- Provider Contracting Credentialing Checklist GUIDE 02-2015 PDFDocument3 pagesProvider Contracting Credentialing Checklist GUIDE 02-2015 PDFboned100% (1)
- Medical Records in PracticeDocument429 pagesMedical Records in PracticeChokri HamoudaNo ratings yet
- Medical Office Management PDFDocument9 pagesMedical Office Management PDFAyessa Joy Tajale100% (1)
- Medical CodingDocument7 pagesMedical CodingRaj DhotreNo ratings yet
- Specification of Use Cases For Information Management Practices in Healthcare: Patient Registration Use CaseDocument24 pagesSpecification of Use Cases For Information Management Practices in Healthcare: Patient Registration Use Casecooking with shab'sNo ratings yet
- CPT 2024 Anticipated Code ChangesDocument5 pagesCPT 2024 Anticipated Code ChangesArnold Ashish GomesNo ratings yet
- Clinical Documentation Improvement (CDI) TrainingDocument6 pagesClinical Documentation Improvement (CDI) Trainingmaricel bismani0% (1)
- Medical DocumentationDocument42 pagesMedical Documentationtummalapalli venkateswara raoNo ratings yet
- CPHQ Content Outline - Effective 01-2018Document3 pagesCPHQ Content Outline - Effective 01-2018empire707No ratings yet
- Medical RecordDocument12 pagesMedical RecordMoin Medicans100% (3)
- Behavioral Health Medical RecordsDocument4 pagesBehavioral Health Medical RecordsRam KumarNo ratings yet
- Assg Codingcasestudies 20171109 Ah102 KPDocument1 pageAssg Codingcasestudies 20171109 Ah102 KPapi-427618755No ratings yet
- Analytics Landscape in Healthcare-1Document24 pagesAnalytics Landscape in Healthcare-1positiveworker88No ratings yet
- The Model For ImprovementDocument17 pagesThe Model For Improvementapi-487551161100% (1)
- KPI-Surgical Cancellation RateDocument1 pageKPI-Surgical Cancellation Rateangeli punoNo ratings yet
- Principles of Healthcare Reimbursement: Sixth EditionDocument28 pagesPrinciples of Healthcare Reimbursement: Sixth EditionDestiny Hayes100% (2)
- Importance of Effective Clinical Documentation by Medical Doctors To Patient Care Management in Federal Teaching Hospital, Ido Ekiti, Ekiti State, NigeriaDocument9 pagesImportance of Effective Clinical Documentation by Medical Doctors To Patient Care Management in Federal Teaching Hospital, Ido Ekiti, Ekiti State, NigeriaInternational Journal of Innovative Science and Research Technology100% (1)
- Credentialing and PrivilegingDocument113 pagesCredentialing and PrivilegingRobert Montuya100% (1)
- Appeal That ClaimDocument65 pagesAppeal That ClaimParag Shinde100% (2)
- CDI Guide To ICD10Document31 pagesCDI Guide To ICD10Banin Abadi100% (1)
- Guidelines For Updating Medical Staff Bylaws: Credentialing and Privileging Physician AssistantsDocument12 pagesGuidelines For Updating Medical Staff Bylaws: Credentialing and Privileging Physician AssistantsYukiMaedaNo ratings yet
- Legal Implications Document A Schneider PDFDocument52 pagesLegal Implications Document A Schneider PDFAmrod Inglorion100% (2)
- Economics of An Urgent Care Center in A Market of Emergency DepartmentsDocument6 pagesEconomics of An Urgent Care Center in A Market of Emergency Departmentsdaron_vchulekNo ratings yet
- Essential Soap Pearce2016Document8 pagesEssential Soap Pearce2016Jou Álvarez100% (1)
- Medical Staff EssentialsDocument20 pagesMedical Staff EssentialsAnonymous SUlZ7VK100% (1)
- Guide To APRN RoleDocument4 pagesGuide To APRN RoleLaceyNo ratings yet
- Assignment 1Document4 pagesAssignment 1mp1757100% (1)
- Clinical Concepts For Family PracticeDocument31 pagesClinical Concepts For Family PracticeabdulqayyumNo ratings yet
- HEDIS Documentation Coding Guide-Adult 2020 - 900-3807A-0819 Approved 9.6rev10.21Document10 pagesHEDIS Documentation Coding Guide-Adult 2020 - 900-3807A-0819 Approved 9.6rev10.21Stephany GrandersonNo ratings yet
- Care ManualDocument70 pagesCare ManualQMx2014No ratings yet
- Revenue CycleDocument240 pagesRevenue CyclePercentage International School100% (2)
- JCAHO Medication Management Standards 2004Document10 pagesJCAHO Medication Management Standards 2004Afdhal MawardinNo ratings yet
- Value Based Care, Reimbursement ModelsDocument3 pagesValue Based Care, Reimbursement ModelsAlexandria NovaNo ratings yet
- CDIP Recommended Resources 060518 PDFDocument1 pageCDIP Recommended Resources 060518 PDFsunnyNo ratings yet
- ModifiersDocument8 pagesModifiersKarna Palanivelu100% (6)
- Medical Transcription Industry: Prepared byDocument27 pagesMedical Transcription Industry: Prepared byrohitpatel203100% (1)
- Virtual Medical ScribesDocument4 pagesVirtual Medical ScribesphysiciansangelsNo ratings yet
- White Paper TelemedicineDocument8 pagesWhite Paper TelemedicineKamau GabrielNo ratings yet
- DRG Overview of All Patient Refined Diagostic Related GroupsDocument42 pagesDRG Overview of All Patient Refined Diagostic Related Groupsjaypee pengNo ratings yet
- Medical MalpracticeDocument18 pagesMedical MalpracticeGlo Allen Cruz0% (1)
- Nurse PractitionersDocument6 pagesNurse PractitionersJakeGilNo ratings yet
- Joint Commission Tracers 2011: What Hospitals Need To KnowDocument223 pagesJoint Commission Tracers 2011: What Hospitals Need To KnowAndreasAndokoNo ratings yet
- Certification/Recertification Examination Content Outline: Cma (Aama)Document4 pagesCertification/Recertification Examination Content Outline: Cma (Aama)pen2trinity3200No ratings yet
- Initial Sheet Medical Case Sheet AuditDocument2 pagesInitial Sheet Medical Case Sheet AuditSrinivas Polikepati0% (1)
- Managing Healthcare OrganisationsDocument16 pagesManaging Healthcare OrganisationsSamuel Josafat Olam100% (1)
- Presentor-: Ruma Sen: MN (Previous) RakconDocument40 pagesPresentor-: Ruma Sen: MN (Previous) Rakconcy100% (1)
- Natcher Vs CADocument4 pagesNatcher Vs CAKKCDIALNo ratings yet
- Tan vs. Sycip PDFDocument20 pagesTan vs. Sycip PDFKKCDIALNo ratings yet
- Sy Bang Vs Sy PDFDocument18 pagesSy Bang Vs Sy PDFKKCDIALNo ratings yet
- RCBC Vs Hitri Dev Corp PDFDocument8 pagesRCBC Vs Hitri Dev Corp PDFKKCDIALNo ratings yet
- Valle Verde Vs Africa PDFDocument12 pagesValle Verde Vs Africa PDFKKCDIALNo ratings yet
- Bernas vs. Cinco PDFDocument23 pagesBernas vs. Cinco PDFKKCDIALNo ratings yet
- Vivares Vs St. Theresa's College PDFDocument12 pagesVivares Vs St. Theresa's College PDFKKCDIALNo ratings yet
- Thornton Vs Thornton PDFDocument5 pagesThornton Vs Thornton PDFKKCDIALNo ratings yet
- Republic v. City of Davao PDFDocument14 pagesRepublic v. City of Davao PDFKKCDIALNo ratings yet
- Collector of Internal Revenue vs. Club Filipino, Inc. de CebuDocument5 pagesCollector of Internal Revenue vs. Club Filipino, Inc. de CebuKKCDIALNo ratings yet
- Republic vs. City of Parañaque PDFDocument24 pagesRepublic vs. City of Parañaque PDFKKCDIALNo ratings yet
- Lanuza vs. Court of Appeals PDFDocument18 pagesLanuza vs. Court of Appeals PDFKKCDIALNo ratings yet
- Saniwares Manufacturing Corp. Vs Aurbach G.R. No. 75875Document14 pagesSaniwares Manufacturing Corp. Vs Aurbach G.R. No. 75875crizaldedNo ratings yet
- 7.litonjua, Jr. vs. Litonjua, Sr.Document24 pages7.litonjua, Jr. vs. Litonjua, Sr.KKCDIALNo ratings yet
- 1.acebedo Optical Vs CA PDFDocument7 pages1.acebedo Optical Vs CA PDFKKCDIALNo ratings yet
- 4.obillos, Jr. vs. Commissioner of Internal RevenueDocument8 pages4.obillos, Jr. vs. Commissioner of Internal RevenueKKCDIALNo ratings yet
- 3.oña vs. Commissioner of Internal RevenueDocument16 pages3.oña vs. Commissioner of Internal RevenueKKCDIALNo ratings yet
- 5.lim Tong Lim vs. Philippine Fishing Gear Industries, Inc.Document23 pages5.lim Tong Lim vs. Philippine Fishing Gear Industries, Inc.KKCDIAL100% (1)
- 4.obillos, Jr. vs. Commissioner of Internal RevenueDocument8 pages4.obillos, Jr. vs. Commissioner of Internal RevenueKKCDIALNo ratings yet
- 2.gatchalian vs. Collector of Internal Revenue PDFDocument11 pages2.gatchalian vs. Collector of Internal Revenue PDFKKCDIALNo ratings yet
- Republic v. City of Davao PDFDocument14 pagesRepublic v. City of Davao PDFKKCDIALNo ratings yet
- 3.oña vs. Commissioner of Internal RevenueDocument16 pages3.oña vs. Commissioner of Internal RevenueKKCDIALNo ratings yet
- 2.gatchalian vs. Collector of Internal Revenue PDFDocument11 pages2.gatchalian vs. Collector of Internal Revenue PDFKKCDIALNo ratings yet
- UERM Memorial Medical Center vs. NLRCDocument7 pagesUERM Memorial Medical Center vs. NLRCKKCDIALNo ratings yet
- Pioneer Texturizing Corp Vs NLRCDocument23 pagesPioneer Texturizing Corp Vs NLRCKKCDIALNo ratings yet
- 1.acebedo Optical Vs CA PDFDocument7 pages1.acebedo Optical Vs CA PDFKKCDIALNo ratings yet
- Samahang Manggagawa Sa Top Form ManufacturingDocument21 pagesSamahang Manggagawa Sa Top Form ManufacturingKKCDIALNo ratings yet
- San Miguel Corporation Employees Union Phil. TransportDocument33 pagesSan Miguel Corporation Employees Union Phil. TransportKKCDIALNo ratings yet
- Pier 8 Arrastre & Stevedoring Services, Inc. vs. RoldanConfesorDocument17 pagesPier 8 Arrastre & Stevedoring Services, Inc. vs. RoldanConfesorKKCDIALNo ratings yet
- Philippine Airlines, Inc. vs. NLRCDocument11 pagesPhilippine Airlines, Inc. vs. NLRCKKCDIALNo ratings yet
- MiesDocument40 pagesMiessanthiyasandyNo ratings yet
- "Nisi Dominus Frustra" College of Nursing & Allied Health Sciences Maasin City, Southern LeyteDocument2 pages"Nisi Dominus Frustra" College of Nursing & Allied Health Sciences Maasin City, Southern Leytecoosa liquorsNo ratings yet
- Cell Damage and DeathDocument1 pageCell Damage and DeathfgdhgfrhNo ratings yet
- Employee Benefits India PDFDocument2 pagesEmployee Benefits India PDFshahidki31100% (1)
- A Review On Water Used in Pharma Industry: European Journal of Pharmaceutical and Medical ResearchDocument11 pagesA Review On Water Used in Pharma Industry: European Journal of Pharmaceutical and Medical ResearchDinesh babuNo ratings yet
- Cen Cenelec Wp2016 enDocument80 pagesCen Cenelec Wp2016 enVamsi Pavan PavuluriNo ratings yet
- Pathologist Job SpecificationDocument16 pagesPathologist Job SpecificationLalaluluNo ratings yet
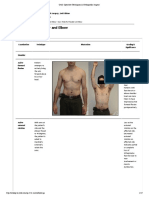
- Exam Table For Shoulder and ElbowDocument17 pagesExam Table For Shoulder and ElbowLouie OkayNo ratings yet
- FDP Form 7 - 20% Component of The IRA Utilization 20% Component of The Ira Utilization For The First Quarter, Cy 2017Document32 pagesFDP Form 7 - 20% Component of The IRA Utilization 20% Component of The Ira Utilization For The First Quarter, Cy 2017Juna Majistad CrismundoNo ratings yet
- Capnography Application in Acute and Critical Care: Tom Ahrens, DNS, RN, CCRN, CS Carrie Sona, MSN, RN, CCRN, CSDocument10 pagesCapnography Application in Acute and Critical Care: Tom Ahrens, DNS, RN, CCRN, CS Carrie Sona, MSN, RN, CCRN, CSJavier Enrique Barrera PachecoNo ratings yet
- Adverse Events Associated With Melatonin For The Treatment of Primary or Secondary Sleep Disorders: A Systematic ReviewDocument20 pagesAdverse Events Associated With Melatonin For The Treatment of Primary or Secondary Sleep Disorders: A Systematic ReviewZach Segmuel MiñanoNo ratings yet
- Nutrition For Liver Gallbladder and Pancreas DiseasesDocument39 pagesNutrition For Liver Gallbladder and Pancreas DiseasesMaricar Car CartallaNo ratings yet
- Foss L.-The End of Modern Medicine. Biomedical Science Under A Microscope-State Univ. of NY (2002) PDFDocument352 pagesFoss L.-The End of Modern Medicine. Biomedical Science Under A Microscope-State Univ. of NY (2002) PDFSusi RutmalemNo ratings yet
- Medical Supplies - English VocabularyDocument4 pagesMedical Supplies - English Vocabularyfatimageraldinep2564No ratings yet
- Shalkya TantraDocument3 pagesShalkya Tantratejpat2k7No ratings yet
- Hazmat Transportation Training RequirementsDocument12 pagesHazmat Transportation Training RequirementsSafety IezzproNo ratings yet
- Prof Nik Marzuki Data PDFDocument3 pagesProf Nik Marzuki Data PDFsue labanNo ratings yet
- Development of Road Header Roof Bolting ModuleDocument7 pagesDevelopment of Road Header Roof Bolting ModuleCraig ThomasNo ratings yet
- Air PollutionDocument3 pagesAir PollutionGaurav Singh JantwalNo ratings yet
- How To Build Your Creative Confidence PDFDocument2 pagesHow To Build Your Creative Confidence PDFSteph GonzagaNo ratings yet
- 2017 ESC Guidelines For The Management of Acute Myocardial Infarction in Patients Presenting With ST Segment ElevationDocument66 pages2017 ESC Guidelines For The Management of Acute Myocardial Infarction in Patients Presenting With ST Segment ElevationMoises Torres AlvarezNo ratings yet
- Aqucar IG 50 PDFDocument4 pagesAqucar IG 50 PDFSteven Reuben PurnomoNo ratings yet
- Casos de Dat Positivos - AabbDocument101 pagesCasos de Dat Positivos - AabbVictor Vargas100% (1)
- One Compartment Open ModelDocument81 pagesOne Compartment Open Modelanon_937994778No ratings yet
- Peavey XR 1220 Manual (ENG) PDFDocument120 pagesPeavey XR 1220 Manual (ENG) PDFRuben David Hurtado RoblesNo ratings yet
- Diary Card Sample 04Document3 pagesDiary Card Sample 04MaryNo ratings yet
- VACCP Template Checklist - SafetyCultureDocument7 pagesVACCP Template Checklist - SafetyCulturepattysaborio520No ratings yet
- FLOWSERVE 350-LNN 71569074-EDocument56 pagesFLOWSERVE 350-LNN 71569074-Eroyert80100% (1)
- Genflex Roofing Systems, LLC Material Safety Data SheetDocument4 pagesGenflex Roofing Systems, LLC Material Safety Data SheetgjroddyNo ratings yet
- Save The ChildrenDocument12 pagesSave The ChildrenBen PalmerNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No ratings yet
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (27)