Professional Documents
Culture Documents
Gastrotomia
Uploaded by
Jessica TovarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gastrotomia
Uploaded by
Jessica TovarCopyright:
Available Formats
Chapter 20
Loughin CA, Marino DJ: Delayed primary surgical treatment in a
dog with a persistent right aortic arch, J Am Anim Hosp Assoc
44:258, 2008.
MacPhail CM, Monnet E, Twedt DC: Thoracoscopic correction of
persistent right aortic arch in a dog, J Am Anim Hosp Assoc
37:577, 2001.
Monnet E: Thoracoscopic correction of persistent right aortic arch.
In Tams TR, Rawlings CA, editors: Small animal endoscopy, ed 3,
St. Louis, 2011, Elsevier, Mosby, p. 501.
Surgery of the Stomach
GENERAL PRINCIPLES AND TECHNIQUES
DEFINITIONS
Gastrotomy is an incision through the stomach wall into the
lumen. Partial gastrectomy is a resection of a portion of the
stomach, and gastrostomy is the creation of an artificial
opening into the gastric lumen. Gastropexy permanently
adheres the stomach to the body wall. Removal of the pylorus
(pylorectomy) and attachment of the stomach to the duodenum (gastroduodenostomy) is a Billroth I procedure.
Attachment of the jejunum to the stomach (gastrojejunostomy) after a partial gastrectomy (including pylorectomy) is
a Billroth II procedure. In a pyloromyotomy, an incision is
made through the serosa and muscularis layers of the pylorus
only. For a pyloroplasty, a full-thickness incision and tissue
reorientation are performed to increase the diameter of the
gastric outflow tract.
PREOPERATIVE CONCERNS
Gastric surgery is commonly performed to remove foreign
bodies (see p. 479) and to correct gastric dilatation-volvulus
(see p. 482). Gastric ulceration or erosion (see p. 490), neoplasia (see p. 494), and benign gastric outflow obstruction
(see p. 488) are less common indications. Gastric disease may
cause vomiting (intermittent or profuse and continuous) or
just anorexia. Dehydration and hypokalemia are common in
vomiting animals and should be corrected before induction
of anesthesia. Alkalosis may occur secondary to gastric
fluid loss; however, metabolic acidosis may also be seen.
Hematemesis may indicate gastric erosion or ulceration or
coagulation abnormalities. Peritonitis arising from perforation of the stomach caused by necrosis or ulceration often is
lethal if not treated promptly and aggressively (see p. 373).
Aspiration pneumonia or esophagitis may also occur in
vomiting animals. If possible, severe aspiration pneumonia
(see p. 425) should be treated before induction of anesthesia
for gastric surgery.
Mild esophagitis generally can be treated by withholding
food for 24 to 48 hours (see p. 425) and treating with
Surgery of the Digestive System
461
H2-receptor antagonists. However, severe esophagitis may
necessitate withholding oral food for 7 to 10 days. A gastrostomy tube (see p. 106) placed during surgery may be considered if continued vomiting is not expected. If continued
vomiting is likely, an enteral feeding tube is preferred (see p.
107). Treatment with H2-receptor antagonists (i.e., cimetidine, ranitidine, famotidine; see Box 20-13) or proton pump
inhibitors (i.e., omeprazole, esomeprazole, pantoprazole; see
Box 20-13) is important. Orally administered sucralfate slurries may help, but they should be given 1 hour after other
medications (see p. 425). Administration of metoclopramide
or cisapride will improve gastric emptying. Antibiotics effective against oral contaminants (e.g., ampicillin, amoxicillin,
clindamycin, cephalosporins) may be considered (see Box
20-14 on p. 425).
When possible, food should be withheld for at least 8 to
12 hours before surgery to ensure that the stomach is empty.
If gastroscopy will be performed, it is best to fast the patient
for at least 18 and preferably 24 hours before the procedure.
However, fasting for only 4 to 6 hours may help prevent
hypoglycemia in pediatric patients (see the discussion on
anesthetic and surgical management of pediatric patients,
which follows). Surgery for gastric obstruction, distention,
malpositioning, or ulceration should be performed as soon
as possible after the animals condition has been stabilized.
ANESTHETIC CONSIDERATIONS
Numerous anesthetic protocols have been used in stable
animals undergoing abdominal surgery (see Table 19-1 on
p. 358). See Table 20-4 for anesthetic recommendations for
the acute abdomen.
ANTIBIOTICS
Perioperative antibiotics may be used if the gastric lumen
will be entered; however, animals with normal immune
function undergoing simple gastrotomy (i.e., proper aseptic
technique and no spillage of gastric contents) rarely require
them. If antibiotics are used (e.g., cefazolin; 22mg/kg given
intravenously at induction; repeat once or twice at 2 to 4
hour intervals), they should be given intravenously before
induction of anesthesia and continued for up to 12 hours
postoperatively. Except for Helicobacter organisms, bacteria
are scarce in the stomach compared with other parts of the
gastrointestinal tract because of the low gastric pH.
SURGICAL ANATOMY
The stomach can be divided into the cardia, fundus, body,
pyloric antrum, pyloric canal, and pyloric ostium. The
esophagus enters the stomach at the cardiac ostium. The
fundus is dorsal to the cardiac ostium, and although relatively small in carnivores, it is easy to identify on radiographs
because it typically is filled with gas. The body of the stomach
(the middle one-third) lies against the left lobes of the liver.
The pyloric antrum is funnel-shaped and opens into the
pyloric canal. The pyloric ostium is the end of the pyloric
canal that empties into the duodenum.
Suggested reading
Holt D, Heldmann E, Michel K, et al: Esophageal obstruction
caused by a left aortic arch and an anomalous right patent ductus
arteriosus in two German shepherd littermates, Vet Surg 29:264270, 2000.
Clinical signs were alleviated in these two dogs by dissection and
division of the patent right ductus arteriosus.
Isakow K, Fowler D, Walsh P: Video-assisted thoracoscopic division
of the ligamentum arteriosum in two dogs with persistent right
aortic arch, J Am Vet Med Assoc 217:1333, 2000.
The technique is described in detail. The laparoscopic procedure
took longer than an thoracotomy, but the authors suggested that the
decreased complications made it a desirable technique.
Lee KC, Lee HC, Jeong SM, et al: Radiographic diagnosis of esophageal obstruction by persistent right aortic arch in a kitten, J Vet
Clin 20:248, 2003.
This case report describes a 3-month-old, male Persian kitten with
PRAA.
Vianna ML, Krahwinkel DJ: Double aortic arch in a dog, J Am Vet
Med Assoc 225(8):1222, 2004.
This is a case report of a dog that did well after surgery; however,
most dogs die or are euthanatized.
White RN, Burton CA, Hale JSH: Vascular ring anomaly with coarctation of the aorta in a cat, J Small Animl Pract 44:330, 2003.
This 1-month-old, male domestic short-hair cat had PRAA with a
coexisting aberrant left subclavian artery, which was the primary
cause of esophageal constriction. Following surgery the cat was
clinically normal.
Chapter 20
Surgery of the Digestive System 461.e1
TABLE 20-4
Anesthetic Considerations for the Patient with an Acute Abdomen
Preoperative Considerations
Associated conditions Dehydration
Electrolyte abnormalities
Hypotension
Anemia
Arrhythmias
Blood work
HCT
Electrolytes
BUN
Cr
TP
Lactate
Urinalysis
Blood gas if available
Physical exam
Often a younger patient that was previously healthy
May be dehydrated, tachycardic or bradycardic, hypotensive, retching, vomiting, or hypothermic
Painful or distended abdomen may be present
Other diagnostics
Blood pressure
ECG
X-ray (abdominal)
Premedications
Rehydrate over 4-6 hours if possible; if emergent, may have to give more rapid boluses to
expedite time to surgery.
Correct electrolyte and metabolic abnormalities if time permits
Avoid sedatives in depressed or cardiovascularly compromised patients.
Avoid alpha 2 agonists and acepromazine.
If patient is stable and anxious, give:
Midazolam (0.2mg/kg IV, IM) or
Diazepam (0.2mg/kg IV)
If patient is not depressed, then give:
Hydromorphone* (0.1-0.2mg/kg IV, IM in dogs; 0.05-0.1mg/kg IV, IM in cats), or
Morphine (0.1-0.2mg/kg IV or 0.2-0.4mg/kg IM), or
Buprenorphine (0.005-0.02mg/kg IV, IM)
Intraoperative Considerations
Induction
Maintenance
Fluid needs
Monitoring
Blocks
If dehydrated or unstable, give the following:
Etomidate (0.5-1.5mg/kg IV), or
Ketamine (5.5mg/kg IV) and diazepam (0.28mg/kg IV)
If hydrated and stable, give the following:
Propofol (2-6mg/kg IV)
Isoflurane or sevoflurane, plus
Fentanyl (2-10g/kg IV PRN in dogs; 1-4g/kg IV PRN in cats) for short-term pain relief, plus
Fentanyl CRI (1-5g/kg IV loading dose, then 2-30g/kg/hr IV), or
Hydromorphone* (0.1-0.2mg/kg IV PRN in dogs; 0.05-0.1mg/kg IV PRN in cats), or
Buprenorphine (0.005-0.02mg/kg IV PRN), plus
Ketamine (low dose) (0.5-1mg/kg IV)
For hypotension (to keep MAP 60-80mmHg) give phenylephrine, ephedrine, norepinephrine,
or dopamine as needed
Two large IV cephalic or jugular catheters
10-20ml/kg/hr if open abdomen with higher evaporative losses, plus 3x EBL; higher rates of
fluids are necessary if dehydration not corrected preoperatively and animal is hypotensive
Consider colloids if persistent hypotension
Blood pressure
ECG
Respiratory rate
SpO2
EtCO2
Temperature
U/O
Epidural:
Morphine (0.1mg/kg preservative free) or
Buprenorphine (0.003-0.005mg/kg diluted in saline)
Avoid local anesthetics for spinal or epidural
Incisional:
Lidocaine (<5mg/kg in dogs; 2-4mg/kg in cats), or
Bupivicaine (<2mg/kg)
Chapter 20
Surgery of the Digestive System
463
TABLE 20-4
Anesthetic Considerations for the Patient with an Acute Abdomencontd
Postoperative Considerations
Analgesia
Fentanyl CRI (1-10g/kg IV loading dose, then 2-20g/kg/hr IV), or
Morphine (0.1-1mg/kg IV or 0.1-2mg/kg IM q1-4hr in dogs; 0.05-0.2mg/kg IV or
0.1-0.5mg/kg IM q1-4hr in cats) if no hypotension, or
Hydromorphone* (0.1-0.2mg/kg IV, IM q3-4hr in dogs; 0.05-0.1mg/kg IV, IM q3-4hr in
cats), or
Hydromorphone CRI (0.025-0.1mg/kg/hr IV in dogs), or
Buprenorphine (0.005-0.02mg/kg IV, IM q4-8hr or 0.01-0.02mg/kg OTM q6-12hr in cats),
plus
Monitoring
Blood work
Estimated pain score
+/ Ketamine CRI (2g/kg/min IV. If no previous loading dose, give 0.5mg/kg IV prior to CRI)
Avoid NSAIDs in patients with hypotension
SpO2
Blood pressure
HR
Respiratory rate
Temperature
U/O
ECG
HCT if significant blood loss
Repeat abnormal preoperative blood work
Serial blood glucose checks if necessary
Blood gas if available
Moderate to moderately severe
HCT, Hematocrit; TP, total protein; CR, creatinine; HR, heart rate; EBL, estimated blood loss; MAP, mean arterial pressure, U/O, urine output;
SpO2, oxygen saturation via a pulse oximeter; EtCO2, end tidal CO2; PRN, as needed; OTM, oral transmucosal.
*Monitor for hyperthermia in cats.
Buprenorphine is a better analgesic than morphine in cats.
NOTE The gastric mucosa accounts for half of
the stomachs weight. You can easily separate the
mucosa from the submucosa and serosa when raising
flaps or making partial thickness incisions during a
gastropexy or pyloromyotomy.
The gastric (lesser curvature) and gastroepiploic (greater
curvature) arteries supply the stomach and are derived from
the celiac artery. The short gastric arteries arise from the
splenic artery and supply the greater curvature. The portion
of the lesser omentum that passes from the stomach to
the liver is the hepatogastric ligament. The stomach of the
Beagle holds more than 500ml of fluid when distended (a
mature cats stomach may hold 300 to 350ml). When the
stomach is highly distended, it can be palpated beyond the
costal arch.
NOTE The short gastric vessels often are avulsed
in animals with gastric dilatation-volvulus, which typically accounts for the intra-abdominal hemorrhage
seen in these cases (see also the discussion of gastric
dilatation-volvulus on p. 482).
SURGICAL TECHNIQUES
Gastric surgery often is performed in small animals. Generally, performing a gastrotomy is safer than performing an
esophagotomy or enterotomy. Peritonitis is uncommon after
gastrotomy if proper techniques are used. Stricture or
obstruction is also rare. Billroth procedures are more difficult and may be associated with severe complications.
Gastroscopy
Endoscopic removal of foreign bodies is preferred over surgical removal but requires appropriate endoscopic snares.
Likewise, endoscopy is more sensitive than gastrotomy when
looking for erosions, ulcers, Physaloptera, and other small
lesions. However, it is imperative that the entire gastric
mucosa be systematically examined, including the fundus
and lower esophageal mucosa. Similarly, endoscopy is the
preferred method for gastric mucosal biopsy because it
allows one to obtain more tissue samples than surgery, which
is important because gastric mucosal lesions can be very
spotty. Scirrhous carcinomas, pythiosis, and submucosal
lesions are the most important gastric lesions that cannot be
reliably diagnosed with endoscopic biopsy. Rarely, intraoperative gastroscopy can be performed to help the surgeon
find a mucosal lesion (e.g., ulcer) that is not obvious
464
PART TWO
Soft Tissue Surgery
Gastrotomy
The most common indication for gastrotomy in dogs and
cats is removal of a foreign body (see p. 479). Make a ventral
incorporates the serosal and muscularis layers (Fig. 20-67,
D). As an alternative, close the mucosa in a simple continuous suture pattern as a separate layer to reduce postoperative bleeding. Before closing the abdominal incision, substitute
sterile instruments and gloves for those contaminated by
gastric contents. Whenever you remove a gastric foreign
body, be sure to check the entire intestinal tract for additional
material that could cause an intestinal obstruction.
midline abdominal incision from the xiphoid to the pubis.
Use Balfour retractors to retract the abdominal wall and
provide adequate exposure of the gastrointestinal tract.
Inspect the entire abdominal contents before incising the
stomach. To reduce contamination, isolate the stomach from
remaining abdominal contents with moistened laparotomy
sponges. Place stay sutures to assist in manipulation of the
stomach and help prevent spillage of gastric contents. Make
the gastric incision in a hypovascular area of the ventral
aspect of the stomach, between the greater and lesser curvatures (Fig. 20-66). Make sure the incision is not near the
pylorus, or closure of the incision may cause excessive tissue
to be enfolded into the gastric lumen, resulting in outflow
obstruction. Make a stab incision into the gastric lumen with
a scalpel (Fig. 20-67, A) and enlarge the incision with Metzenbaum scissors (Fig. 20-67, B). Use suction to aspirate
gastric contents and reduce spillage. Close the stomach with
2-0 or 3-0 absorbable suture material (e.g., polydioxanone,
polyglyconate) in a two-layer inverting seromuscular pattern
(Fig. 20-67, C). Include serosa, muscularis, and submucosa
in the first layer, using a Cushing or simple continuous
pattern, then follow it with a Lembert or Cushing pattern that
FIG 20-66. Preferred location of gastrotomy incisions.
from the serosal surface. Endoscopic polypectomy using
electrocautery has been described in one dog and one cat
and was associated with resolution of clinical signs for 12
and 21 months (Foy and Bach, 2010).
FIG 20-67. Gastrotomy. A, Make a stab incision into the gastric lumen with a scalpel.
B, Enlarge the incision with Metzenbaum scissors. C and D, Close the stomach with a
two-layer inverting seromuscular suture pattern.
Chapter 20
Surgery of the Digestive System
465
Partial Gastrectomy and Invagination
of Gastric Tissue
Partial gastrectomy is indicated when necrosis, ulceration, or
neoplasia involves the greater curvature, or middle portion,
of the stomach. Necrosis of the greater curvature is primarily
associated with gastric dilatation-volvulus (GDV) and may
be treated by resection or invagination. Invagination does
not require opening of the gastric lumen (Fig. 20-68);
however, obstruction from excessive intraluminal tissue and
excessive bleeding is possible (Parton etal, 2006). Assess the
extent of necrosis by observing the serosal color, gastric wall
texture, vascular patency, and bleeding on incision; however,
in many cases it is difficult to determine tissue viability with
these techniques (see page 501 for a discussion of methods
for determining tissue viability). Necrotic tissue may range
in color from gray-green to black and often feels thin. A fullthickness incision can be made into the suspected necrotic
tissue to assess arterial bleeding. Intravenous fluorescein dye
has not proved to be an accurate method of determining
gastric viability in dogs with GDV. Generally, if you question
the viability of the gastric tissue, remove it or invaginate it.
Failure to remove or invaginate necrotic tissue may result in
perforation, peritonitis, and death. Melena is commonly
observed for a few days after gastric invagination.
NOTE Do not use mucosal color to predict gastric
viability; the mucosa is commonly black in dogs with
GDV because of vascular obstruction. Damage to the
mucosa may predispose these animals to gastric
ulceration.
To remove the greater curvature of the stomach, ligate
branches of the left gastroepiploic vessels or short gastric
vessels (or both) along the section of the stomach to be
removed (Fig. 20-69). Excise the necrotic tissue, leaving a
margin of normal, actively bleeding tissue to suture. Close
the stomach in a two-layer inverting pattern using 2-0 or 3-0
absorbable suture (e.g., polydioxanone, polyglyconate).
Incorporate the submucosa, muscularis, and serosal layers
in a Cushing or simple continuous pattern in the first layer.
Then use a Cushing or Lembert pattern to invert the serosa
and muscularis over the first layer. As an alternative, you
may use a thoracoabdominal (TA) stapling device to close
the incision. To invaginate necrotic tissue, use a simple continuous suture pattern followed by an inverting pattern. Place
sutures in healthy gastric tissue on both sides of the tissue
that is to be invaginated, bringing the healthy tissue over the
top of the necrotic tissue. Make sure the sutures are placed
in healthy tissues to prevent dehiscence.
Removal of neoplasia (see p. 494) or ulceration (see p.
490) of the greater or lesser curvature is similar to that
described for necrotic tissue. Most neoplasms in the gastric
body except for leiomyomas and leiomyosarcomas have
metastasized by the time they are diagnosed. If the abnormal
tissue involves the dorsal or ventral aspect of the stomach,
an elliptic incision encompassing the lesion and some
FIG 20-68. Invagination of necrotic gastric tissue.
adjacent normal tissue is used. Closure is as for a simple
gastrotomy. Occasionally the extent of the lesion requires
resection of both the dorsal and ventral walls of the stomach.
In such cases, ligate branches of the right and left gastric
artery and vein (lesser curvature) and left gastroepiploic
artery and vein (greater curvature) and remove the omental
attachments. After removal of the suspect tissues, perform a
two-layer end-to-end anastomosis of the stomach. If the
luminal circumferences are of disparate size, the larger circumference can be partly closed using a two-layer suture
pattern (see Fig. 20-70, B). Close the mucosa and submucosa of the dorsal surface of the stomach in a simple continuous pattern using 2-0 or 3-0 absorbable suture (e.g.,
polydioxanone, polyglyconate), then with the same suture
close the ventral aspect. Suture the serosa and muscularis
layers in an inverting pattern (e.g., Cushing or Lembert).
Temporary Gastrostomy
Temporary gastrostomy is used to decompress the stomach
and occasionally is indicated in dogs with GDV until more
definitive surgery can be performed but is rarely done. For
a description of the technique, see Small Animal Surgery,
second edition.
Pylorectomy with
Gastroduodenostomy (Billroth I)
Removal of the pylorus and gastroduodenostomy
is indicated for neoplasia (see p. 494), outflow obstruction
caused by pyloric muscular hypertrophy (see p. 488), or
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Automorphic Representations and L-Functions For The General Linear Group - Volume 2cDocument210 pagesAutomorphic Representations and L-Functions For The General Linear Group - Volume 2cluisufspaiandreNo ratings yet
- MechanismDocument17 pagesMechanismm_er100No ratings yet
- Synetek Controls Inc.: Ds1-S: Installation InstructionsDocument2 pagesSynetek Controls Inc.: Ds1-S: Installation Instructionsdgd_electromecNo ratings yet
- MRP Format MbaDocument6 pagesMRP Format Mbasankshep panchalNo ratings yet
- Hazop Recommendation Checked by FlowserveDocument2 pagesHazop Recommendation Checked by FlowserveKareem RasmyNo ratings yet
- Thick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHDocument13 pagesThick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHPrabhu PrasadNo ratings yet
- ATM ReportDocument16 pagesATM Reportsoftware8832100% (1)
- Aemses Sof Be LCP 2021 2022Document16 pagesAemses Sof Be LCP 2021 2022ROMEO SANTILLANNo ratings yet
- Telecomm SwitchingDocument49 pagesTelecomm SwitchingTalha KhalidNo ratings yet
- Liquid Air Energy Storage Systems A - 2021 - Renewable and Sustainable EnergyDocument12 pagesLiquid Air Energy Storage Systems A - 2021 - Renewable and Sustainable EnergyJosePPMolinaNo ratings yet
- Lecturer No 1 - Transformer BasicDocument1 pageLecturer No 1 - Transformer Basiclvb123No ratings yet
- AESCSF Framework Overview 2020-21Document30 pagesAESCSF Framework Overview 2020-21Sandeep SinghNo ratings yet
- ClarifierDocument2 pagesClarifierchagar_harshNo ratings yet
- Augustine and The Devil Two BodiesDocument12 pagesAugustine and The Devil Two BodiesAlbert LanceNo ratings yet
- Release emotions with simple questionsDocument10 pagesRelease emotions with simple questionsDubravko ThorNo ratings yet
- trac-nghiem-ngu-am-am-vi-hoc-tieng-anh-đã chuyển đổiDocument18 pagestrac-nghiem-ngu-am-am-vi-hoc-tieng-anh-đã chuyển đổiNguyễn ThiênNo ratings yet
- Srimanta Shankardev: Early LifeDocument3 pagesSrimanta Shankardev: Early LifeAnusuya BaruahNo ratings yet
- Corporate Subsidies On A Massive ScaleDocument2 pagesCorporate Subsidies On A Massive ScaleBurchell WilsonNo ratings yet
- Vedic Astrology OverviewDocument1 pageVedic Astrology Overviewhuman999100% (8)
- Vikash Kumar: 1. Aunico India May 2018Document4 pagesVikash Kumar: 1. Aunico India May 2018Rama Krishna PandaNo ratings yet
- Food 8 - Part 2Document7 pagesFood 8 - Part 2Mónica MaiaNo ratings yet
- On MCH and Maternal Health in BangladeshDocument46 pagesOn MCH and Maternal Health in BangladeshTanni ChowdhuryNo ratings yet
- Implementing a JITD system to reduce bullwhip effect and inventory costsDocument7 pagesImplementing a JITD system to reduce bullwhip effect and inventory costsRaman GuptaNo ratings yet
- Booklet English 2016Document17 pagesBooklet English 2016Noranita ZakariaNo ratings yet
- Provisional List of Institutes1652433727Document27 pagesProvisional List of Institutes1652433727qwerty qwertyNo ratings yet
- 2000 T.R. Higgins Award Paper - A Practical Look at Frame Analysis, Stability and Leaning ColumnsDocument15 pages2000 T.R. Higgins Award Paper - A Practical Look at Frame Analysis, Stability and Leaning ColumnsSamuel PintoNo ratings yet
- Specification: F.V/Tim e 3min 5min 8min 10MIN 15MIN 20MIN 30MIN 60MIN 90MIN 1.60V 1.67V 1.70V 1.75V 1.80V 1.85VDocument2 pagesSpecification: F.V/Tim e 3min 5min 8min 10MIN 15MIN 20MIN 30MIN 60MIN 90MIN 1.60V 1.67V 1.70V 1.75V 1.80V 1.85VJavierNo ratings yet
- Etoposide JurnalDocument6 pagesEtoposide JurnalShalie VhiantyNo ratings yet
- CFC KIDS FOR CHRIST 2020 FINAL EXAMDocument13 pagesCFC KIDS FOR CHRIST 2020 FINAL EXAMKaisser John Pura AcuñaNo ratings yet
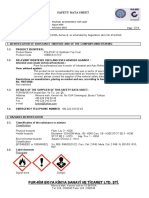
- Polifur 1K Synthetic Top Coat MSDS Rev 2 ENDocument14 pagesPolifur 1K Synthetic Top Coat MSDS Rev 2 ENvictorzy06No ratings yet