Professional Documents
Culture Documents
Chapter 51
Uploaded by
Londera BainOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 51
Uploaded by
Londera BainCopyright:
Available Formats
Kee: Pharmacology, 8th Edition
Chapter 51: Endocrine Drugs: Pituitary, Thyroid, Parathyroid, and Adrenal Disorders
Downloadable Key Points
Chapter 51 discusses drugs used for hormonal replacement and for inhibition of hormonal
secretion from the pituitary, adrenal, thyroid, and parathyroid glands.
The anterior pituitary gland secretes the following hormones that target glands and
tissues: (a) growth hormone (GH), (b) thyroid-stimulating hormone (TSH), (c)
adrenocorticotropic hormone (ACTH), and (d) gonadotropins (follicle-stimulating
hormone [FSH] and luteinizing hormone [LH]).
Growth hormone does not have a specific target gland. It affects body tissues and bone;
GH replacement stimulates linear growth when there is a GH deficiency. Growth
hormone drugs cannot be given orally, because they are inactivated by gastrointestinal
enzymes.
Because GH acts on newly forming bone, it must be administered before the epiphyses
are fused.
Prolonged GH therapy can antagonize insulin secretion and eventually cause diabetes
mellitus.
Somatrem and somatropin are two growth hormones used to treat growth failure in
children because of pituitary GH deficiency.
Somatropin is contraindicated in pediatric patients who have growth deficiency due to
Prader-Willi syndrome and are severely obese or who have severe respiratory
impairment, because fatalities associated with these risk factors have been reported.
Gigantism and acromegaly can occur with GH hypersecretion and are frequently caused
by a pituitary tumor. The prolactin-release inhibitor bromocriptine can inhibit the release
of GH from the pituitary gland.
Octreotide is a potent synthetic somatostatin used to suppress GH release. GI side effects
are common.
Excess TSH secretion can cause hyperthyroidism, and a TSH deficit can cause
hypothyroidism.
ACTH secretion stimulates the release of glucocorticoids, mineralocorticoids, and
androgen from the adrenal cortex.
The ACTH drug corticotropin is used to diagnose adrenal gland disorders, to treat adrenal
gland insufficiency, and as an antiinflammatory drug in the treatment of allergic response.
Copyright 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc.
Downloadable Key Points
51-2
Corticotropin has numerous drug interactions. Persons with diabetes may need increased
insulin and oral antidiabetic drugs.
ADH promotes water reabsorption from the renal tubules to maintain water balance in the
body fluids.
When there is a deficiency of ADH, large amounts of water are excreted by the kidneys.
This condition, called diabetes insipidus (DI), can lead to severe fluid volume deficit and
electrolyte imbalances.
Fluid and electrolyte balance must be closely monitored in patients with DI, and ADH
replacement may be needed with the ADH preparations vasopressin and desmopressin
acetate.
SIADH can be treated by fluid restriction, demeclocycline, conivaptan, and tolvaptan.
Serum sodium levels must be monitored closely.
Thyroxine (T4) and triiodothyronine (T3) are secreted by the thyroid gland. The functions
of T4 and T3 are to regulate protein synthesis and enzyme activity and to stimulate
mitochondrial oxidation. Feedback mechanisms regulate T4 and T3 secretion from the
thyroid gland.
Decreased T4 and elevated TSH levels indicate primary hypothyroidism. Myxedema is
severe hypothyroidism in the adult; in children, hypothyroidism can have a congenital
(cretinism) or prepubertal (juvenile hypothyroidism) onset.
Levothyroxine sodium is the drug of choice for replacement therapy for the treatment of
hypothyroidism. It increases the levels of T3 and T4.
Liothyronine is a synthetic T3 that has a short half-life and duration of action; it is not
recommended for maintenance therapy.
Many drug interactions are associated with T4 and T3 drugs.
Hyperthyroidism is an increase in circulating T4 and T3 levels. Hyperthyroidism may be
mild with few symptoms or severe, as in thyroid storm in which death may occur from
vascular collapse. Graves disease, or thyrotoxicosis, is the most common type of
hyperthyroidism.
The purpose of antithyroid drugs is to reduce the excessive secretion of thyroid hormones
(T4 and T3) by inhibiting thyroid secretion.
Thiourea derivatives are the drugs of choice used to decrease thyroid hormone
production. This drug group interferes with synthesis of thyroid hormone.
Propylthiouracil and methimazole are effective thioamide antithyroid drugs. They are
useful for treating thyrotoxic crisis and in preparation for subtotal thyroidectomy.
Prolonged use of thioamides may cause a goiter.
Antithyroid drugs interact with many other drugs.
Copyright 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc.
Downloadable Key Points
51-3
The parathyroid glands secrete parathyroid hormone (PTH), which regulates calcium
levels in the blood. The action of PTH is to promote calcium absorption from the GI
tract, promote reabsorption of calcium from the renal tubules, and activate vitamin D.
Calcitriol is a vitamin D analogue that promotes calcium absorption from the GI tract and
secretion of calcium from bone to the bloodstream.
Corticosteroids promote sodium retention and potassium excretion. Because of their
influence on electrolytes and carbohydrate, protein, and fat metabolism, a deficiency of
corticosteroids can result in serious illness or death.
A decrease in corticosteroid secretion is called adrenal hyposecretion (adrenal
insufficiency, or Addisons disease), and an increase in corticosteroid secretion is called
adrenal hypersecretion (Cushings syndrome).
Glucocorticoids are used to treat many diseases and health problems, including
inflammatory, allergic, and debilitating conditions.
The side effects and adverse reactions of glucocorticoids that result from high doses or
prolonged use include increased blood sugar, abnormal fat deposits in the face and trunk,
decreased extremity size, muscle wasting, edema, sodium and water retention,
hypertension, euphoria or psychosis, thinned skin with purpura, increased intraocular
pressure, peptic ulcers, and growth retardation.
When drug therapy is discontinued, the dose should be tapered to allow the adrenal
cortex to produce cortisol and other corticosteroids. Abrupt withdrawal of the drug can
result in severe adrenocortical insufficiency.
The antineoplastic hormone antagonists mitotane and aminoglutethimide inhibit
glucocorticoid synthesis. Aminoglutethimide is frequently prescribed for temporary
treatment of selected patients with Cushings syndrome.
Mineralocorticoids secrete aldosterone. Aldosterone is controlled by the reninangiotensin system. These hormones maintain fluid balance.
Fludrocortisone is an oral mineralocorticoid. It can cause a negative nitrogen balance;
therefore, a high-protein diet is usually indicated. Serum potassium levels should be
monitored.
Copyright 2015, 2012, 2009, 2006, 2003, 2000, 1997, 1993 by Saunders, an imprint of Elsevier Inc.
You might also like
- The Complete List of NANDA Nursing Diagnosis For 2012Document4 pagesThe Complete List of NANDA Nursing Diagnosis For 2012annNo ratings yet
- Kee: Pharmacology, 8th Edition: Chapter 43: Diuretics Downloadable Key PointsDocument3 pagesKee: Pharmacology, 8th Edition: Chapter 43: Diuretics Downloadable Key PointsLondera BainNo ratings yet
- Respiratory TermsDocument1 pageRespiratory TermsLondera BainNo ratings yet
- Kee: Pharmacology, 8th Edition: Chapter 59: Adult and Pediatric Emergency Drugs Downloadable Key PointsDocument8 pagesKee: Pharmacology, 8th Edition: Chapter 59: Adult and Pediatric Emergency Drugs Downloadable Key PointsLondera BainNo ratings yet
- History of ChildrenDocument4 pagesHistory of ChildrenLondera BainNo ratings yet
- Chapter 51Document3 pagesChapter 51Londera BainNo ratings yet
- AML Employment ApplicationDocument6 pagesAML Employment ApplicationLondera BainNo ratings yet
- Chapter 02Document3 pagesChapter 02Londera BainNo ratings yet
- Fundamental Keypoint Chapter 4Document1 pageFundamental Keypoint Chapter 4nkuligowskiNo ratings yet
- Physical AssessmentDocument6 pagesPhysical AssessmentLondera BainNo ratings yet
- Chapter 002Document3 pagesChapter 002Londera BainNo ratings yet
- Unit 1 Dimensions of MCHDocument5 pagesUnit 1 Dimensions of MCHLondera BainNo ratings yet
- Chapter 03Document3 pagesChapter 03Londera BainNo ratings yet
- Respiratory TermsDocument1 pageRespiratory TermsLondera BainNo ratings yet
- Physical DevelopmentDocument3 pagesPhysical DevelopmentLondera BainNo ratings yet
- Fundamental Keypoint Chapter 4Document1 pageFundamental Keypoint Chapter 4nkuligowskiNo ratings yet
- Kee: Pharmacology, 8th Edition: Chapter 7: Pediatric Pharmacology Downloadable Key PointsDocument2 pagesKee: Pharmacology, 8th Edition: Chapter 7: Pediatric Pharmacology Downloadable Key PointsLondera BainNo ratings yet
- Chapter 01Document4 pagesChapter 01Londera BainNo ratings yet
- Chapter 002Document3 pagesChapter 002Londera BainNo ratings yet
- Chapter 02Document3 pagesChapter 02Londera BainNo ratings yet
- Fact SheetDocument6 pagesFact SheetLondera BainNo ratings yet
- WHO - Essential Drugs PDFDocument376 pagesWHO - Essential Drugs PDFnrhmhealthNo ratings yet
- Kee: Pharmacology, 8th Edition: Chapter 59: Adult and Pediatric Emergency Drugs Downloadable Key PointsDocument8 pagesKee: Pharmacology, 8th Edition: Chapter 59: Adult and Pediatric Emergency Drugs Downloadable Key PointsLondera BainNo ratings yet
- Chapter 03Document3 pagesChapter 03Londera BainNo ratings yet
- Potter: Fundamentals of Nursing, 8 Edition: Chapter 01: Nursing Today Answer Key - Review Questions and RationalesDocument2 pagesPotter: Fundamentals of Nursing, 8 Edition: Chapter 01: Nursing Today Answer Key - Review Questions and RationalesLondera BainNo ratings yet
- BlommesteinDocument1 pageBlommesteinLondera BainNo ratings yet
- Chapter 40-Upper RespiratoryDocument2 pagesChapter 40-Upper RespiratoryLondera BainNo ratings yet
- An Historical and Contemporary Overview of Gendered Caribbean RelationsDocument10 pagesAn Historical and Contemporary Overview of Gendered Caribbean RelationsdjlogonNo ratings yet
- Vital Statistics Section Department of StatisticsDocument1 pageVital Statistics Section Department of StatisticsLondera BainNo ratings yet
- The FamilyDocument4 pagesThe FamilyLondera BainNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Drugs Acting On The Endocrine System Compiled WRDocument74 pagesDrugs Acting On The Endocrine System Compiled WREyz PabloNo ratings yet
- Sun 800 RoidRage Innovative Trends Treatment Male HypogonadismDocument19 pagesSun 800 RoidRage Innovative Trends Treatment Male HypogonadismM. Sz.No ratings yet
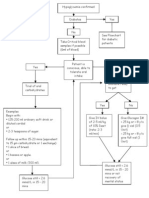
- Hypoglycaemia FlowchartDocument1 pageHypoglycaemia FlowchartMohammad SultanNo ratings yet
- Insulin Initiation GuidanceDocument4 pagesInsulin Initiation GuidanceRahma WatiNo ratings yet
- Oxytocin, ADH Lecture For 2nd Year MBBS by DR Waeem KausarDocument28 pagesOxytocin, ADH Lecture For 2nd Year MBBS by DR Waeem KausarIMDCBiochemNo ratings yet
- Chapter 13Document27 pagesChapter 13Itzel XD HerreraNo ratings yet
- Immulite Assay Menu PDFDocument2 pagesImmulite Assay Menu PDFОлександрNo ratings yet
- Diseases of Adrenal Gland: DR Samir ChakrabortyDocument14 pagesDiseases of Adrenal Gland: DR Samir ChakrabortyJaymalyaNo ratings yet
- Case Study Analysis (1,2,3,4) ENDOCRINOLOGYDocument3 pagesCase Study Analysis (1,2,3,4) ENDOCRINOLOGYDayledaniel Sorveto100% (1)
- Snakes AnatomyDocument26 pagesSnakes AnatomyRoxana Nae PuccaNo ratings yet
- Acromegaly: Excess Growth Hormone SecretionDocument4 pagesAcromegaly: Excess Growth Hormone SecretionKavita PathakNo ratings yet
- Ramadan Guide For DiabetesDocument9 pagesRamadan Guide For DiabetesUjwal TickooNo ratings yet
- Biology: Topic - Endocrine System Class-VIII Board - ICSEDocument3 pagesBiology: Topic - Endocrine System Class-VIII Board - ICSEItu DeyNo ratings yet
- Thyroid Disease and OsteoporosisDocument60 pagesThyroid Disease and Osteoporosisplay_wright2084No ratings yet
- Diabetes InsipidusDocument4 pagesDiabetes Insipidusshelly_shellyNo ratings yet
- Jurnal HipertiroidDocument6 pagesJurnal HipertiroidUmmulAklaNo ratings yet
- Thyroid Function and Obesity: Translational Thyroidology / ReviewDocument9 pagesThyroid Function and Obesity: Translational Thyroidology / ReviewXochitemiqui YoacihualtNo ratings yet
- PD22 Hap1 L03Document33 pagesPD22 Hap1 L03Ka Yan LAUNo ratings yet
- Geriatric EndocrinologyDocument65 pagesGeriatric EndocrinologyZaidanNo ratings yet
- Pituitary Gland DisordersDocument80 pagesPituitary Gland DisordersNang KhamNo ratings yet
- Hyperprolactinemia: A Systematic Review of Diagnosis and ManagementDocument12 pagesHyperprolactinemia: A Systematic Review of Diagnosis and ManagementJaveria RphNo ratings yet
- Hypothyroidism Pregnancy BrochureDocument2 pagesHypothyroidism Pregnancy BrochureNungky KusumaNo ratings yet
- RFI Strip Chart 333 To 379Document90 pagesRFI Strip Chart 333 To 379mad21_No ratings yet
- South-East Asia Trend P-A M-1 L-12: Number of People Suffering From DM in SEA Region Is Also IncreasingDocument1 pageSouth-East Asia Trend P-A M-1 L-12: Number of People Suffering From DM in SEA Region Is Also IncreasingtanzirNo ratings yet
- What Steroid Supplementation Is Required For A Patient With Primary Adrenal Insufficiency Undergoing A Dental Procedure?Document6 pagesWhat Steroid Supplementation Is Required For A Patient With Primary Adrenal Insufficiency Undergoing A Dental Procedure?AnthonyNo ratings yet
- Dulutalias - Chapter18-THE ENDOCRINE SYSTEMDocument10 pagesDulutalias - Chapter18-THE ENDOCRINE SYSTEMGwen Valerie DulutaliasNo ratings yet
- Estimation of Blood GlucoseDocument16 pagesEstimation of Blood GlucoseAhmed MohamadNo ratings yet
- Adrenal Glands 2018 - 2019Document32 pagesAdrenal Glands 2018 - 2019Bianca BiaNo ratings yet
- Biology Endocrine System Notes Compiled by Srikrshna p1 PDFDocument8 pagesBiology Endocrine System Notes Compiled by Srikrshna p1 PDFKazi AslamNo ratings yet
- Therapeutics: Thyroid DisordersDocument24 pagesTherapeutics: Thyroid DisordersSharas FarhadNo ratings yet