Professional Documents
Culture Documents
The Role of Honey in The Management of Wounds: Discussion
Uploaded by
Ni Wayan Ana PsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Role of Honey in The Management of Wounds: Discussion
Uploaded by
Ni Wayan Ana PsCopyright:
Available Formats
DISCUSSION
The role of honey in the
management of wounds
A review of the evidence on the advantages of using honey as a topical wound
treatment together with practical recommendations for its clinical use
he widespread development of
antibiotic -resistant bacteria l
has generated an increasing
interest in the use of alternate therapies
for the treatment of infected wounds. In
1989, an editorial in the Journal of the
Royal Society of Medicine, referring to
reports o n the successful use o f
ho ney in wounds, stated: 'The
therapeutic potential of uncontaminated,
pure honey is grossly underutilized.' This
paper examines how the chemical and
physical properties of honey may facilitate
wound healing and offers guidance on
practical issues related to clinical use.
Antibacterial action
A number of laboratory studies have
demonstrated the significant antibacterial
activity of honey. Using concentrations of
honey ranging from 1.8% to 11% (v/v),
researchers have achieved complete inhibition of the major wound-infecting
species of bacteria.3 Other reports include:
complete inhibition of a collection of
strains of MRSA (1%-4% v/v honey);4
complete inhibition of 58 strains of coagulase-positive Staphylococcus aureus isolated from infected wounds (2%-4% v/v
honey);5 complete inhibition of 20 strains
of Pseudomonas isolated from infected
wounds (5.5%-8.7% v/v honey).6
The antibacterial activity of honey has
also been shown in vivo, with reports of
infected wounds dressed with honey
becoming sterile in 3-6 days,7,8 7 days9-11
and 7-10 days.12
Solutions of high osmolarity, such as
honey, sugar and sugar pastes, inhibit
microbial growth13 because the sugar
molecules 'tie up' water molecules so that
bacteria have insufficient water to support
their growth. When used as dressings,
dilution of these solutions by wound
exudate reduces osmolarity to a
P.C.Molan, BSc, PhD, Director, Honey Research
Unit, University of Waikato, Hamilton, New Zealand
Abscesses; Burns; Honey; Moist wound
healing;-Necrotising-fasclitis;
Ulcers; Wound infection
level that ceases to control infection,
especially if wounds are infected with
Staphylococcus aureus (a common osmotolerant wound pathogen). 14, 15 Even
when diluted by exudate to a point where
its osmolarity no longer inhibits bacterial
growth, honey's additional antibacterial
components still ensure sterility.
Honey's antibacterial activity is
thought to be due primarily to the
presence of hydrogen peroxide, generated
by the action of an enzyme that the
bees add to nectar.16 Some floral
sources provide additional antibacterial
components by way of plant-derived
chemicals in the nectar, such as
flavonoids and aromatic acids.17 This
partly explains the very large variation
that is seen in the antibacterial potency of
honeys from different floral sources.18
However, the variation results mainly
from differences in the amount of
hydrogen peroxide formed in the honeys,
because nectar from some floral sources
contains components that break down
hydrogen peroxide or destabilise the
enzyme that produces it. Exposure of
honey to heat and light also deactivates
the enzyme that produces hydrogen
per-oxide.18
Differences
in
the
antibacterial potency are reflected in the
varying sensitivity results reported for
wound-infecting species of bacteria.18
The use of hydrogen peroxide as an
antiseptic agent in the treatment of
wounds is generally considered to give
outcomes that are less than successful.
However, when honey is used, the
hydrogen peroxide is delivered in a very
J O U R N A L O F W O U N D C A R E S E P T E M B E R , VOL 8 , NO 8, 1999
different way. Hydrogen peroxide is an
effective antimicrobial agent if present at a
sufficiently high concentration,19 but at
'higher concentrations-it-causes-cellular
and protein damage in tissues by giving
rise to oxygen radicals 20,21 This limits the
concentration of hydrogen peroxide that
can be used as an antiseptic.
Honey effectively provides a slow-release
delivery of hydrogen peroxide; the enzyme
producing it becomes active only when
honey is diluted16 and continues to
produce it at a steady rate for at least 24
hours (unpublished work). In honey
diluted with an equal volume of pH7
buffer, the concentration of hydrogen
peroxide accumulating in one hour is typically about 1000 times less than that in
the solution of hydrogen peroxide (3%)
that is commonly used as an antiseptic.
Honey also has high levels of
antioxi-dants,22 which would protect
wound tissues from oxygen radicals that
may be produced by the hydrogen
peroxide.
Deodorising action
The deodorisation of offensive odour
from wounds is an expected conse quence of honey's antibacterial action.
The malodour is due to ammonia,
amines and sulphur compounds, which
are produced when infecting bacteria
metabolise amino acids from proteins in
the serum and necrotic tissue in a
wound. The rapidity of honey's deodorising action is probably due to the provision of a rich source of glucose, which
would be used by the infecting bacteria
in preference to amino acids,23 resulting
in the production of lactic acid instead of
malodorous compounds.
Debriding action
The debriding action of honey has not
yet been explained. It may be simply a
415
DISCUSSION
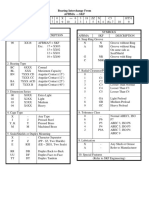
Table I. Advantages of using honey
Wound care advantages
It provides a protective barrier to
prevent cross-infection10,34,31,40,41,54,61
It creates an antibacterial moist healing
environment
It rapidly dears infecting bacteria7-12
including antibiotic-resistant strains37
It has a debriding effect and its osmotic
action causes an outflow of lymph, lifting
debris from the wound bed8-10,31,33,34,38,49,50,61
It rapidly removes malodour9-11,33,34,61
It hastens healing through stimulation of
tissue regeneration7-10,12, 26-30,33,37-41
It prevents scarring and
hypertrophicaton9,30,33,48
It minimises the need for skin
grafting8,9,30,61
It is non-adherent and therefore minimises
trauma and pain during dressing
changes30,34,37,39,48,49,55
Its and-inflammatory action reduces
oedemas.9,10,31-33
It has no adverse effect on wound
tissues10,11,31,37,40,49
Economic advantages
Reduced costs of dressing materials and
antibacterial agents12,37,52,59
More rapid healing8,11,12,26,30,37,41,53
The obviation of surgical
debridement8-10,31
The obviation of skin grafting8,9,30,33
Ease of use allows patients to manage
their own wound care at home, thus
reducing nursing costs
result of the moist healing environment
that is created by the honey dressing.
Another possibility is that it is an enzymatic debridement process. There have
been no reports of honey having any
proteolytic activity, but the debridement
action may be due to activation of
pro-teases in wound tissues by hydrogen
peroxide generated by the honey
dressing. It has been reported that
metalloproteases can be activated by
oxidation,24 and the inhibitors of serine
proteases can be deactivated by
oxidation.25
Anti-inflammatory action
Histological studies using experimental
wounds in animals have shown that
416
honey has an anti-inflammatory influence even when there is no infection present, this being seen as a reduction in the
number of inflammatory cells infiltrating
the wound tissue. 26-29 This confirms
clinical observations of reduction in
inflammation,26,30 oedema,9,10,31-33 and
exudation,9,10,26 and a soothing effect26,34,35
when honey is applied to wounds. This
anti-inflammatory influence may be associated with the antioxidant content of
honey, which has been found to be of a
significant level when assayed as the
capacity of honey to scavenge free radicals?, Oxygen radicals are involved in various aspects of inflammation,25 and the
application of antioxidants to burns has
been shown to reduce inflammation.36
Stimulation of tissue growth
Honey promotes the formation of clean
healthy granulation tissue7-10,12,30,32,37-39
and
epithelialisation,9,10,30,33,40
as
demonstrated histologically in animal
studies 26-29,41 This may be due to the
generation of hydrogen peroxide, low
levels of which stimulate angiogenesis42
and the growth of fibroblasts43 Increased
angiogenesis would provide more oxygen,
which is a limiting factor for tissue
regeneration.
Acidification of the wound may also be
responsible: honey typically has a pH from
3 to 4, and topical acidification has been
shown to promote healing44 by causing
more oxygen to be released from haemoglobin.45 Also it has been suggested that the
decreased turgor resulting from the
application of honey may increase tissue
oxygenation;10
the
reduction
in
hydrostatic pressure in the interstitial
fluid resulting from anti-inflammatory
action would allow improved circulation
in the tissues.
Another theory is that the nutrient content of honey may stimulate growth it
has a wide range of amino acids, vitamins
and trace elements, in addition to large
quantities of readily assimilable sugars.
Studies in animals46 and humans47 have
shown an association between topical
application of nutrients to wounds and
increased growth of granulation tissue.
In addition, the high osmolarity of
honey will draw fluid out from a wound
bed. This outflow of lymph with its dissolved nutrients would also provide
nutrition for regenerating tissue.
Clinical experience
Honey has been used to treat a number
of different wound types, including surgical wounds8,11,12,41,48-51 most notably
v u l v e c to m y
wo u nd s , 8 , 1 1 , 1 2 , 4 1 , 4 8 - 5 1
w o u n d s related to trauma,10,50,52-54
wounds associated with necrotising
fasciitis,9,33 pressure tlICerS10.38.53'55.58 and
venous and diabetic leg ulcers.52,59,60
However, it is in the management of
burn wounds that the role of honey has
probably received most attention.
Investigations have shown honey to
be
more
effective
than
other
products29.30.34,61 in the management of
partial-thickness burns. A retrospective
study also has shown that honey is as
effective as silver sulphadiazine in the
management of burns.62
In prospective randomised controlled
trials comparing honey with silver sulphadiazine-impregnated gauze in the treatment of fresh partial-thickness burns,
honey was shown to produce an early subsidence of acute inflammatory changes
and quicker wound healing, better control
of infection, better relief of pain, less irritation of the wound, less exudation, and a
lower incidence of hypertrophic scar and
post-burn contracture.30,61 The advantages
of using honey in the management of
wounds are listed in Table 1.
Guidelines for practice
Honey varies in consistency, from liquid
to solid, with the glucose content crystallised. Solid honeys may be liquified by
warming and semi-solid honeys can often
be liquified by stirring. Heating above
37C should be avoided, as this may bum
the patient and will destroy the enzyme
that produces hydrogen peroxide.
The honey should be spread evenly on
the dressing pad rather than directly to the
wound. The amount of honey required on
a wound depends on the amount of
exudation; the beneficial effects of honey
on wound tissues will be reduced or lost
if small quantities of honey become
diluted by large amounts of exudate.
Wounds with deep infection require
greater amounts of honey to obtain an
effective level of antibacterial activity by
diffusion into the wound tissues.
Dressing technique
Typically, 30mL of honey is used on a
10cm x 10cm dressing. Dressing pads
impregnated with honey (such as those
produced by REG International, New
Zealand) (Figs 1 & 2) are the most convenient way of applying honey to surface
wounds. Occlusive or absorbent secondary
dressings are needed to prevent honey
oozing out from the wound dressing (Fig
3). The frequency of dressing changes will
also depend on how rapidly the honey is
diluted by exudate. Daily dressing changes
are usual, but up to three times daily may
JOURNAL OF WOUND CARE SEPTEMBER, VOL 8, NO 8, 1999
uniquely high level of a herbal antibacterial
63
component that is particularly effective
against
some
of
the
important
3
wound-infecting bacteria. However, ail
honeys vary very much in their potency.
There is a high chance of the activity being
little better than that of sugar if a honey is
63
taken at random. There is a large variance in
the level of antibacterial activity even within
honeys from the same floral source.
be necessary.
Exudation should be
reduced by the anti-inflammatory action of
honey, so the frequency of dressing
changes should decline as treatment
progresses. Deep wounds (Figs 4-6) or
abscesses are most easily filled by using
honey packed in 'squeeze-out' tubes, now
available commercially (Actimel) (Fig 7).
Honey quality
Although ancient physicians were aware that
honeys from particular sources had the
best therapeutic properties, little regard is
given to this in current clinical practice. Any
honey to be used for infected wounds
should therefore have its antibacterial
activity assayed. A 'UMF' rating (equivalent to
the concentration of phenol which has the
same activity against Staphylococcus aureus)
is being used by producers of manuka
honey to show the potency of its
plant-derived component.
Potential risk
There is no report of any type of infection
Honeys from Leptospermum species (for
resulting from the application of honey to
example,
manuka
honey)CARE
can SEPTEMBER,
have a VOL 8, NOwounds
JOURNAL
OF WOUND
8, 1999 although there is no reference in
reports of the clinical application of honey on
open wounds being sterilised before use.
Honey sometimes contains spores of
clostridia, which poses a small risk of infection,
such as wound botulism. Any risk can be
overcome by the use of honey that has been
treated by gamma-irradiation, which kills
clostridial spores without loss of any of the
honey's antibacterial activity."
Conclusion
This paper has described the chemical and
physical properties of honey and has
shown how these may have a positive
influence on wound healing. Honey is an ideal
substance to use as a wound dressing
material. Its fluidity, especially when
warmed, allows it to be spread and makes
honey dressings easy to apply and
37,39,55
remove.
The osmotic action resulting
from honey's high sugar content draws out
wound fluid and thus dilutes the honey that is
in contact with the wound bed, minimising
adhesion or damage to the granulating surface
30-44,49
of the wounc1
when the dressing is
34
removed. The high solubility of honey in
water allows residual
417
DISCUSSION
'
honey to be washed away by bathing54
Although the clinical experiences
detailed in this paper show positive results,
more quality randomised controlled trials
are needed to provide evidence to
encourage the use of honey in wound care.
REFERENCES
I. Greenwood, D. Sixty years on: antimicrobial drug
resistance comes of age. Lancet 1995; 346: (Suppl I), s I,
2. Zumla, A., Lulat, A. Honey; a remedy rediscovered. J R
Soc Med 1989; 82: 384-385,
3. Willix, D.J., Molan, P.C., Harfoot, C.J. A comparison of
the sensitivity of wound-infecting species of bacteria to the
antibacterial activity of manuka honey and other honey.]
Appl Bacteriol 1992: 73: 388-394.
4. Molan, P.. Brett. M. Honey has potential as a dressing
for wounds infected with MRSA. The Second Australian
Wound Management Association Conference: 1998
March 18-21; Brisbane, Australia.
5. Cooper, R.A., Molan, P.C., Harding, K.G. The
effectiveness of the antibacterial activity of honey against
strains of Staphylococcus aureus isolated from infected
wounds.) R Soc Med 1999; 1999; 92: 283-285.
6. Cooper, RA, Molan, P.C. The use of honey as an
antiseptic in managing Pseudomonas infection.) Wound
Care 1999; 8: 4, 161-164.
7. Branikl, F.J. Surgery in Western Kenya. Ann R Con Surg
Eng! 1981; 63: 348-352.
8. Cavanagh, D., Beazley, J., Ostapowica F. Radical
operation for carcinoma of the vulva: a new approach to
wound healing.) Obstet Gynaecol Commonw 1970; 77:
I 1, 1037.1140.
9, Efem, S.E.E. Recent advances in the management of
Fournier's gangrene; preliminary observations. Surgery
1993; 113: 2. 200-204,
10. Efem S.E,E, Clinical observations on the wound healing
properties of honey. Sr) Surg 1988; 75: 679.681.
11. Phuapradit, W., Saropala, N. Topical application of
honey In treatment of abdominal wound disruption. Austr
NZ J Obstet Gynaecol 1992; 32: 4, 381-384.
12. Armors, P.J. The use of honey in the treatment of
infected wounds. Trop Doct 1980; 10: 91.
13. Chirife, J., Scarmato, G., Herszage, L. Scientific basis for
use of granulated sugar in treatment of Infected wounds.
Lancet 1982; I: (March 6), 560-561.
14. Chirife, J., Herszage, L. Joseph, A. et at In vitro study of
bacterial growth inhibition in concentrated sugar solutions:
microbiological basis for the use of sugar in treating
infected wounds. Antimicrobial Agents & Chemother 1983;
23: 5, 766-773.
I 5. Herszage, L, Montenegro, J.R., Joseph, A.L
Tratamiento de las heridas supur-adas con azcecar
granulado comercial. Bol Trab Soc Argent Or 1980; 41:
21-22, 315-330.
16. White, J.W., Subers, M.H., Schepartz, A.I. The
identification of inhibine, the antibacterial factor in honey,
as hydrogen peroxide and Its origin In a honey
glucose-oxidase system. Blochim alophys Acta 1963; 73:
57-70.
17. Molan P.C. The antibacterial activity of honey, I: The
nature of the antibacterial activity. Bee World 1992; 73: 1,
5-28.
18. Molan, P.C. The antibacterial activity of honey. 2:
Variation in the potency of the antibacterial activity. Bee
World 1992; 73: 2, 59-76.
19. Roth, L.A., Kwan, S., Sporns, P. Use of a disc-assay
system to detect oxytetracycline residues in honey.
J Food Prot 1986; 49: 6, 436-441.
20. Cochrane, C.G. Cellular injury by oxidants. Am J Med
1991; 91: (Suppl 3c), 235.305.
21. Simon, R.H., Scoggin, C.H.. Patterson, D. Hydrogen
peroxide causes the fatal injury to human fibroblasts
exposed to oxygen radicals. J Biol Chem 1981; 256: 14,
7181-7186.
22. Frankel, 5., Robinson, G.E., Berenbaum, M.R.
Antioxidant capacity and correlated characteristics of 14
unifioral honeys. J Apic Res 1998; 37: I, 27-31.
23. Nychas, G.J., Dillon, V.M., Board, R.G. Glucose, the key
substrate in the microbiological changes in meat and certain
meat products. Brotechnol App/ Biochem 1988; 10: 203-231.
24. Van Wart, H.E.. Birkedal-Hansen, H. The cystein
418
int J Crude Drug Res 1988; 26: 3, 161-168.
KEY ISSUES FOR PRACTICE
The use of honey dressings may have a
beneficial effect in wound management
and can be cost-effective
Solid honeys may be liquified by stirring or
warming but honey should not be heated
above 37C
The honey should be spread evenly and
applied to the dressing pad rather than
directly the wound
Deep wounds can be filled with honey from
a 'squeeze-out' tube
The amount of honey required depends on
the amount of exudate; wounds with deep
infection require greater amounts of
honey
Dressing pads pre-impregnated with honey
are the most convenient method of applying
honey to wounds
Frequency of dressing change depends on
quantity of exudate
switch: a principle of regulation of metalloproteinase
activity with potential applicability to the entire matrix
metalloproteinase gene family. Proc Nat Acad Sri USA
1990;87: 14.5578-5582,
25.
Floh, L. Beckmann, R., Giertz, H. et al.
Oxygen-centred free radicals as mediators of
inflammation. In: Sies, H. (ed). Oxidative Stress. London,
Orlando: Academic Press, 1985.
26.
Burlando, F. Sull'azione terapeutica del miele
nelle ustioni. Minerva Dermatol 1978; 113: 699-706.
27.
Gupta, S.K., Singh, H., Varshney, A.G. et
al. Therapeutic efficacy of honey in infected wounds in
buffaloes. Indian J Anim Sri 1992; 62: 6, 521-523. 28,
Kumar, A., Sharma, V.K., Singh, H.P. et al. Efficacy of some
indigenous drugs in tissue repair in buffaloes. Indian Vet)
1993; 70: I, 42-44.
29. Postures, T.J., Bosch, M.M.C., Dutrieux, R. et al.
Speeding up the healing of burns with honey. An
experimental study with histological assessment of
wound biopsies. In: Mizrahl, A., tensity, Y. (eds). Bee
Products: Properties, applications and apitherapy. New York,
NY: Plenum Press, 1997.
30. Subrahmanyam, M. A prospective randomised clinical
and histological study of superficial burn wound healing
with honey and silver sulfadiazine. Bums 1998; 24: 2,
157-161.
31. Subrahmanyam, M. Honey dressing versus boiled
potato peel in the treatment of burns: a prospective
randomized study. Bums 1996; 22: 6, 491-493.
32. Dumrongiert, E. A follow-up study of chronic wound
healing dressing with pure natural honey. ) Nat Res Counc
Than 1983; 15: 2, 39-66.
33. Hejase,11.J., Simonin,
BIhrle, R., Coogan. C.L
Genital Fournier's gangrene: experience with 38 patients.
Urology 1996; 47: 5. 734-739.
34. Subrahmanyam, M. Honey impregnated gauze versus
polyurethane film (OpSite) in the treatment of burns: a
prospective randomised study. Br) Piast Surg 1993; 46: 4,
322.323.
35. Keast-Butler J. Honey for necrotic malignant breast
ulcers. Lancet 1980;
(October II ), 809.
36. Tanaka, H., Hanumadass, M., Matsuda. H. et al.
Hemodynamic effects of delayed initiation of antioxidant
therapy (beginning two hours after burn) in extensive
third-degree burns.] Burn Care Rehabil 1995; 16: 6,
610-615.
37. Farouk, A., Hassan, T., Kashif, H. et at Studies on
Sudanese bee honey: laboratory and clinical evaluation.
38. Hutton. D.J. Treatment of pressure sores. Nurs Times
1966; 62: 46, 1533-1534.
Wadi. M., Al-Amin, H., Farouq, A. et al. Sudanese bee
honey in ;he treatment of suppurating wounds. Arab
Medico 1987; 3: 16-18.
39. Subrahmanyam, M. Honey-impregnated gauze versus
amniotic membrane in the treatment of burns. Bums
1994; 20:4, 331-333.
40. Bergman, A., Yana!, J., Weiss, J. et al. Acceleration of
wound healing by topical application of honey: an animal
model. Am J Surg 1983; 145: 374-376.
41. Tur, E., Bolton, L, Constantine, B.E. Topical
hydrogen peroxide treatment of ischemic ulcers in the
guinea pig: blood recruitment in multiple skin sites. J Am
Acad Dermatoi 1995; 33:2 (Part I), 217-221.
42. Schmidt, R.J., Chung, LY., Andrews, A.M. et al.
Hydrogen peroxide is a murine (L929) fibroblast cell
proliferant at micro- to nanomolar concentrations. In:
Harding, K.G., Cherry. G., Dealey, C.. Turner, T.D.
(eds). Proceedings of the 2nd European Conference on
Advances in Wound Management. London: Macmillan
Magazines, 1993.
43. Kaufman, T., Eichenlaub, E.H., Angel, M.F. et al.
Topical acidification promotes healing of experimental
deep partial thickness skin burns; a randomised
double-blind preliminary study. Bums 1985; 12:
84-90.
44. Leveen, N.H., Falk, G., Borek, B. et al. Chemical
acidification of wounds: an adjuvant to healing and the
unfavourable action of alkalinity and ammonia, Ann Surg
1973; 178: 6, 745-753.
45. Kaufman, T., Levin, M., Hurwitz, D.J. The effect of
topical hyperalimentadon on wound healing rate and
granulation tissue formation of experimental deep
second-degree burns in guinea-pigs. Bums 1984; 10: 4,
252-256.
46. Viljanto, J., Raekallio, J. Local hyperallmentation of
open wounds. Br) Surg 1976; 63: 3, 427-430.
47. McInerney, R.J.F. Honey: a remedy rediscovered.
J R Soc Med 1990; 83: 127.
48. Bulman, M.W. Honey as a surgical dressing. Middlesex
Hosp./ 1955; 55: 188-189.
49. Ndaylsaba, G., Bazira, L, Habonimana, E. et at
Clinical and bacteriological results in wounds treated
with honey. J Orthop Surg 1993; 7: 2, 202-204.
50. Dany-Mazeau, M., Pautard, G. L'utilisadon du miel
dans le processus de cicatrisation: de la ruche a PhOpital.
Krankenpfl Soins Infirm 1991; 84: 3, 63-69.
52: Wood, B., Rademaker, M., Molan, P.C. Manuka
honey, a low cost leg ulcer dressing. N Z Med J 1997;
110: 107.
53. Hamdy, M.H., El-Banby, MA, Khakifa ICI. et al. The
antimicrobial effect of honey in the management of
septic wounds. In: Proceedings of the Fourth International
Conference on Apiculture in Tropical Climates. London:
International Bee Research Association, 1989.
54. Green, AE Wound healing properties of honey. Br J
Surg 1988; 75: 12, 1278.
55. Blomfleld, R. Honey for decubitus ulcers. J Am Med
Assoc 1973; 224: 6, 905.
56. Dany-Mazeau, M.P.G. Honig auf die Wunde.
Krankenpflege 1992; 46: 1, 6-10.
57. SomeHield, S.D. Honey and healing.) R Soc Med
1991; 84: 3, 179.
58. Weheida, S.M.. Nagubib, H.H. El-Banna, H.M. et at
Comparing the effects of two dressing techniques on
healing of low grade pressure ulcers. J Med Res Inst
Alexandria Univ 1991; 12: 2.259-278.
59. Harris, S. Honey for the treatment of superficial
wounds: a case report and review. Primary intention 1994;
2:4, 18-23.
60. Tovey, F.I. Honey and healing. j R Sot Med 1991: 84:
7, 447.
61. Subrahmanyam, M. Topical application of honey in
treatment of burns. Br .1 Surg 1991; 78: 4, 497-498.
62. Adesunkanmi, K., Oyelami, 0.A. The pattern and
outcome of burn injuries at Wesley Guild Hospital,
Ilesha, Nigeria: a review of 156 cases.) Trop Med Hyg
1994; 97: 2, 108-112.
63. Allen, K.L, Molan, P.C., Reid, G.M. A survey of the
antibacterial activity of some New Zealand honeys. J
Phorm Pharmacol 1991; 43: 12, 817-822.
64. Molan, P.C., Allen, K.L The effect of
gamma-irradiation on the antibacterial activity of honey.
J Phorm Pharmacol 1996; 48: 1206-1209.
JOURNAL OF WOUND CARE SEPTEMBER, VOL 8, NO 8, 1999
You might also like
- Honey: A Biologic Wound DressingDocument22 pagesHoney: A Biologic Wound DressingTeuku FennyNo ratings yet
- Antimicrobial Properties of Natural Honey: A Review of LiteratureDocument7 pagesAntimicrobial Properties of Natural Honey: A Review of LiteratureDanielle PecsonNo ratings yet
- Research Article: International Research Journal of PharmacyDocument5 pagesResearch Article: International Research Journal of PharmacyGrassellaNo ratings yet
- Honey Paper - Rose CooperDocument3 pagesHoney Paper - Rose CooperMax Jordan DooleyNo ratings yet
- Manisha Deb Mandal Shyamapada Mandal: Honey: Its Medicinal Property and Antibacterial ActivityDocument9 pagesManisha Deb Mandal Shyamapada Mandal: Honey: Its Medicinal Property and Antibacterial Activityriyaldi_dwipaNo ratings yet
- 276) 2010 Cerio - Mechanism Action Clinical Benefits Colloidal Oatmeal Dermatologic PracticeDocument5 pages276) 2010 Cerio - Mechanism Action Clinical Benefits Colloidal Oatmeal Dermatologic Practicezebulon78No ratings yet
- Throughout History Man Has Had To Contend With Dermal WoundsDocument9 pagesThroughout History Man Has Had To Contend With Dermal Woundswisnutato22No ratings yet
- 9 Honey Medicine ReviewDocument20 pages9 Honey Medicine ReviewjivasumanaNo ratings yet
- Application of Essential Oils As Natural Cosmetic PreservativesDocument15 pagesApplication of Essential Oils As Natural Cosmetic PreservativesjosareforNo ratings yet
- Elhage 2021Document8 pagesElhage 2021Trần Duy TânNo ratings yet
- JURNAL INTERNASIONAL SENSITIVITAS (Study Antibacterial Activity of Honey Against Some Common Species Of)Document9 pagesJURNAL INTERNASIONAL SENSITIVITAS (Study Antibacterial Activity of Honey Against Some Common Species Of)windaNo ratings yet
- Molecules 20 16068Document17 pagesMolecules 20 16068RezanovianingrumNo ratings yet
- Invitro Evaluation of Antibacterial Activity of Honey Against Wound PathogenDocument5 pagesInvitro Evaluation of Antibacterial Activity of Honey Against Wound PathogenEditor IJTSRDNo ratings yet
- Evaluation of Effectiveness of Honey-Based Alginate Hydrogel On Wound Healing in Rat ModelDocument5 pagesEvaluation of Effectiveness of Honey-Based Alginate Hydrogel On Wound Healing in Rat ModelAlief AkbarNo ratings yet
- 7762075-Dreger and WielgusDocument15 pages7762075-Dreger and WielgusAlma KunicNo ratings yet
- Actividad EnzimaticDocument11 pagesActividad EnzimaticherfuentesNo ratings yet
- Effect of Natural Honey (Produced by African Sculata in Guyana)Document5 pagesEffect of Natural Honey (Produced by African Sculata in Guyana)Melivea Paez HerediaNo ratings yet
- Impact of Honey Dressing On Chronic UlcerDocument6 pagesImpact of Honey Dressing On Chronic UlcerIJAR JOURNALNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument6 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- !! 1-S2.0-S2666154322001934-MainDocument9 pages!! 1-S2.0-S2666154322001934-Mainancuta.lupaescuNo ratings yet
- Hydroalcoholic Extract Based-Ointment From Punica Granatum L. Peels With Enhanced in Vivo Healing Potential On Dermal WoundsDocument9 pagesHydroalcoholic Extract Based-Ointment From Punica Granatum L. Peels With Enhanced in Vivo Healing Potential On Dermal WoundsLa Ode Muhammad FitrawanNo ratings yet
- Krim Mentimum11Document15 pagesKrim Mentimum11Takeshi MondaNo ratings yet
- Hipochlorous Acid Anjing Kucing 2-5 Mikro L LDocument10 pagesHipochlorous Acid Anjing Kucing 2-5 Mikro L LyulianaNo ratings yet
- Determination of Antioxidant and Antimicrobial Properties of Agaricus Bisporus From Romanian MarketsDocument7 pagesDetermination of Antioxidant and Antimicrobial Properties of Agaricus Bisporus From Romanian MarketsKhairul WaldiNo ratings yet
- Scientific Brochure: Science For Healthy SkinDocument25 pagesScientific Brochure: Science For Healthy SkinHunt ApplegateNo ratings yet
- Al Waili2003Document6 pagesAl Waili2003wizuraihakimroyNo ratings yet
- Research Life ScienceDocument8 pagesResearch Life ScienceDan Jenniel CedeñoNo ratings yet
- Ijbms 16 731Document12 pagesIjbms 16 731TututWidyaNurAnggrainiNo ratings yet
- Antibacterial Profile of Honey On Staphylococcus Aureus Isolated From Surgical Wound in Awomamma General HospitalDocument5 pagesAntibacterial Profile of Honey On Staphylococcus Aureus Isolated From Surgical Wound in Awomamma General HospitalasclepiuspdfsNo ratings yet
- Body Malodours and Their Topical Treatment AgentsDocument14 pagesBody Malodours and Their Topical Treatment AgentsChiper Zaharia DanielaNo ratings yet
- 58 Arshad AJBIODocument12 pages58 Arshad AJBIOvidiNo ratings yet
- Antibacterial Activity of Phyto Essential Oils On Flaccherie Causing Bacteria in The Mulberry Silk Worm, B.Mori. LDocument5 pagesAntibacterial Activity of Phyto Essential Oils On Flaccherie Causing Bacteria in The Mulberry Silk Worm, B.Mori. LIOSRjournalNo ratings yet
- Mod Med La v6n1p22 enDocument7 pagesMod Med La v6n1p22 enta22122001No ratings yet
- Antimicrobial Activity of HoneyDocument20 pagesAntimicrobial Activity of HoneyYadiNo ratings yet
- Antibiotic, Pestisida HoneyDocument9 pagesAntibiotic, Pestisida HoneyDian Laras SuminarNo ratings yet
- SavlonDocument4 pagesSavlonArif MuhammadNo ratings yet
- Sabinsa Developing All Natural Personal Care Products 2009 v3Document12 pagesSabinsa Developing All Natural Personal Care Products 2009 v3JeanNo ratings yet
- Gelee RoyaleDocument5 pagesGelee Royalerabahhalim183No ratings yet
- Apiteraphy HandbookDocument69 pagesApiteraphy HandbookladygagajustinNo ratings yet
- Title Defense Life Group 10Document8 pagesTitle Defense Life Group 10Dan Jenniel CedeñoNo ratings yet
- Antimicrobial Effect of Honey Produced by On Some Common Human PathogensDocument6 pagesAntimicrobial Effect of Honey Produced by On Some Common Human Pathogensreal_septiady_madrid3532No ratings yet
- Artikel JurnalDocument5 pagesArtikel Jurnalsalman fardNo ratings yet
- Allantoin Anti Inflamatory ActivityDocument17 pagesAllantoin Anti Inflamatory ActivityValentina CarreroNo ratings yet
- Antimicrobial Activity of Plant Extracts ThesisDocument4 pagesAntimicrobial Activity of Plant Extracts Thesiskimberlybundypittsburgh100% (1)
- Antimicrobial Property of Over-the-Counter Essential Oils and Ayurvedic Powders Against Aeromonas Hydrophila Isolated From Labeo RohitoDocument4 pagesAntimicrobial Property of Over-the-Counter Essential Oils and Ayurvedic Powders Against Aeromonas Hydrophila Isolated From Labeo RohitoInternational Journal of Innovative Science and Research Technology100% (1)
- Antibiotic, Pesticide, and Microbial Contaminants of Honey Human HealthDocument10 pagesAntibiotic, Pesticide, and Microbial Contaminants of Honey Human HealthJuan Alejandro JiménezNo ratings yet
- An Invitro Study of Determination of Anti-Bacterial, Antioxidant, Anti-Inflammatory Potential of Piper Betel Essential OilDocument8 pagesAn Invitro Study of Determination of Anti-Bacterial, Antioxidant, Anti-Inflammatory Potential of Piper Betel Essential OilSaiful AbdulNo ratings yet
- Exploring Cucumber Extract For Skin RejuvenationDocument12 pagesExploring Cucumber Extract For Skin Rejuvenationemiliana.wirawanNo ratings yet
- Preliminary PagesDocument43 pagesPreliminary PagesShem AngelesNo ratings yet
- Surface Culturing of Chromobacterium Violaceum MTCC 2656 For Violacein Production and Prospecting Its Bio ActivitiesDocument12 pagesSurface Culturing of Chromobacterium Violaceum MTCC 2656 For Violacein Production and Prospecting Its Bio Activitieskrishna YurekaNo ratings yet
- The Antibacterial Effect of Roselle Hibiscus SabdaDocument4 pagesThe Antibacterial Effect of Roselle Hibiscus SabdaIid Fitria TNo ratings yet
- Assyifa Jurnal, Minawati Said SuatDocument11 pagesAssyifa Jurnal, Minawati Said SuatNur WahidaNo ratings yet
- Colloidal Oatmeal Formulations and The Treatment of Atopic Dermatitis - JDDonline - Journal of Drugs in DermatologyDocument1 pageColloidal Oatmeal Formulations and The Treatment of Atopic Dermatitis - JDDonline - Journal of Drugs in DermatologyMelvy RozaNo ratings yet
- IJCRT2402204Document11 pagesIJCRT2402204VickyNo ratings yet
- Biological Properties and Therapeutic Activities of Honey in Wound Healing: A Narrative Review and Meta-AnalysisDocument21 pagesBiological Properties and Therapeutic Activities of Honey in Wound Healing: A Narrative Review and Meta-AnalysisJuan Enrique EspinozaNo ratings yet
- Pylori: Susceptibility The Antibacterial Activity HoneyDocument4 pagesPylori: Susceptibility The Antibacterial Activity HoneyLoredanaNo ratings yet
- Handbook ApitherapyDocument60 pagesHandbook ApitherapyengrezgarNo ratings yet
- Example Review of Related StudiesDocument5 pagesExample Review of Related StudiesMarianne MontefalcoNo ratings yet
- 27 Vol9Document6 pages27 Vol9Amine BenineNo ratings yet
- Ibnt 06 I 3 P 377Document2 pagesIbnt 06 I 3 P 377Ni Wayan Ana PsNo ratings yet
- Pi Is 0002937814008084Document8 pagesPi Is 0002937814008084snrarasatiNo ratings yet
- Content ServerDocument5 pagesContent ServerNi Wayan Ana PsNo ratings yet
- Content ServerDocument4 pagesContent ServerNi Wayan Ana PsNo ratings yet
- ObsosDocument6 pagesObsosNi Wayan Ana PsNo ratings yet
- Quinn Et A Predictores de Composicion de Leche 2012Document8 pagesQuinn Et A Predictores de Composicion de Leche 2012Adriana CavazosNo ratings yet
- Content ServerDocument3 pagesContent ServerNi Wayan Ana PsNo ratings yet
- Content ServerDocument4 pagesContent ServerNi Wayan Ana PsNo ratings yet
- Cervical Stitch (Cerclage) For Preventing Pregnancy Loss: Individual Patient Data Meta-AnalysisDocument17 pagesCervical Stitch (Cerclage) For Preventing Pregnancy Loss: Individual Patient Data Meta-AnalysisNi Wayan Ana PsNo ratings yet
- The Causes of CancerDocument11 pagesThe Causes of CancerShailNo ratings yet
- Cerebrovascular Accident in B-Thalassemia Major (B-TM) and B-Thalassemia Intermedia (b-TI)Document3 pagesCerebrovascular Accident in B-Thalassemia Major (B-TM) and B-Thalassemia Intermedia (b-TI)Ni Wayan Ana PsNo ratings yet
- 2Document10 pages2Ni Wayan Ana PsNo ratings yet
- The Hypercoagulable State in Thalassemia: Hemostasis, Thrombosis, and Vascular Biology Clinical Trials and ObservationsDocument9 pagesThe Hypercoagulable State in Thalassemia: Hemostasis, Thrombosis, and Vascular Biology Clinical Trials and ObservationsNi Wayan Ana PsNo ratings yet
- 1391283400Document7 pages1391283400Ni Wayan Ana PsNo ratings yet
- 07 DJMCJ v7 I1 151 Nazia Akhter Obstructed LabourDocument4 pages07 DJMCJ v7 I1 151 Nazia Akhter Obstructed LabourDewi Rahmawati SyamNo ratings yet
- P ('t':'3', 'I':'668636885') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document10 pagesP ('t':'3', 'I':'668636885') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ni Wayan Ana PsNo ratings yet
- Clinical Characteristics of Clear Cell Carcinoma of The OvaryDocument6 pagesClinical Characteristics of Clear Cell Carcinoma of The OvaryNi Wayan Ana PsNo ratings yet
- Title of The Presentation: Your SubtitleDocument2 pagesTitle of The Presentation: Your SubtitleNi Wayan Ana PsNo ratings yet
- Chemotherapy For Recurrent and Metastatic Cervical CancerDocument5 pagesChemotherapy For Recurrent and Metastatic Cervical CancerNi Wayan Ana PsNo ratings yet
- Do Clear Cell Ovarian Carcinomas Have Poorer Prognosis Compared To Other Epithelial Cell Types? A Study of 1411 Clear Cell Ovarian CancersDocument7 pagesDo Clear Cell Ovarian Carcinomas Have Poorer Prognosis Compared To Other Epithelial Cell Types? A Study of 1411 Clear Cell Ovarian CancersNi Wayan Ana PsNo ratings yet
- Using Antimicrobial Surgihoney To Prevent Caesarean Wound InfectionDocument5 pagesUsing Antimicrobial Surgihoney To Prevent Caesarean Wound InfectionNi Wayan Ana PsNo ratings yet
- Distosia Ncbi (Ana)Document8 pagesDistosia Ncbi (Ana)Ni Wayan Ana PsNo ratings yet
- 416 1391 1 PBDocument5 pages416 1391 1 PBNi Wayan Ana PsNo ratings yet
- Passage and Passanger Image Collection (Ana)Document16 pagesPassage and Passanger Image Collection (Ana)Ni Wayan Ana PsNo ratings yet
- Skrining CMVDocument10 pagesSkrining CMVNi Wayan Ana PsNo ratings yet
- Jurnal GastroenterohepatologiDocument18 pagesJurnal GastroenterohepatologiRarasRachmandiarNo ratings yet
- Cytokeratin 7 and Cytokeratin 19 Expressions in Oval Cells and Mature Cholangiocytes As Diagnostic and Prognostic Factors of CholestasisDocument6 pagesCytokeratin 7 and Cytokeratin 19 Expressions in Oval Cells and Mature Cholangiocytes As Diagnostic and Prognostic Factors of CholestasisNi Wayan Ana PsNo ratings yet
- Liver Disease Pediatric PatientDocument14 pagesLiver Disease Pediatric PatientNi Wayan Ana PsNo ratings yet
- CMV Primer Non PrimerDocument3 pagesCMV Primer Non PrimerNi Wayan Ana PsNo ratings yet
- EXAMPLE 8.6 Veneer Grades and RepairsDocument2 pagesEXAMPLE 8.6 Veneer Grades and RepairsnickNo ratings yet
- Multi Organ Dysfunction SyndromeDocument40 pagesMulti Organ Dysfunction SyndromeDr. Jayesh PatidarNo ratings yet
- FBC MNCS Service-, Error-, Infocodes ENDocument23 pagesFBC MNCS Service-, Error-, Infocodes ENDragos Stoian100% (1)
- MSDS DowthermDocument4 pagesMSDS DowthermfebriantabbyNo ratings yet
- Tips For A Healthy PregnancyDocument2 pagesTips For A Healthy PregnancyLizaNo ratings yet
- CCNA Training New CCNA - RSTPDocument7 pagesCCNA Training New CCNA - RSTPokotete evidenceNo ratings yet
- Wildlife Emergency and Critical CareDocument14 pagesWildlife Emergency and Critical CareRayssa PereiraNo ratings yet
- 1.1.3.12 Lab - Diagram A Real-World ProcessDocument3 pages1.1.3.12 Lab - Diagram A Real-World ProcessHalima AqraaNo ratings yet
- Precision CatalogDocument256 pagesPrecision CatalogImad AghilaNo ratings yet
- Practice For Mounting Buses & Joints-374561Document11 pagesPractice For Mounting Buses & Joints-374561a_sengar1No ratings yet
- The Working of KarmaDocument74 pagesThe Working of KarmaSuhas KulhalliNo ratings yet
- Ecological Quality RatioDocument24 pagesEcological Quality RatiofoocheehungNo ratings yet
- Statics: Vector Mechanics For EngineersDocument39 pagesStatics: Vector Mechanics For EngineersVijay KumarNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaMel DaNo ratings yet
- Adaptive Reuse Architecture Documentation and Analysis 2168 9717 1000172Document9 pagesAdaptive Reuse Architecture Documentation and Analysis 2168 9717 1000172Komal HundiaNo ratings yet
- Flusser-The FactoryDocument2 pagesFlusser-The FactoryAlberto SerranoNo ratings yet
- Asco Series 238 ASCO Pilot Operated Solenoid Valves (Floating Diaphragm)Document2 pagesAsco Series 238 ASCO Pilot Operated Solenoid Valves (Floating Diaphragm)Khyle Laurenz DuroNo ratings yet
- Joby Aviation - Analyst Day PresentationDocument100 pagesJoby Aviation - Analyst Day PresentationIan TanNo ratings yet
- Rectifier 5G High Density Embedded Power (3U Power Rack, Three Phase Four Wire) E...Document4 pagesRectifier 5G High Density Embedded Power (3U Power Rack, Three Phase Four Wire) E...Lintas LtiNo ratings yet
- GSD Puppy Training Essentials PDFDocument2 pagesGSD Puppy Training Essentials PDFseja saulNo ratings yet
- Rachel Joyce - A Snow Garden and Other Stories PDFDocument118 pagesRachel Joyce - A Snow Garden and Other Stories PDFИгорь ЯковлевNo ratings yet
- Kimi No Na Wa LibropdfDocument150 pagesKimi No Na Wa LibropdfSarangapani BorahNo ratings yet
- Nomenclatura SKFDocument1 pageNomenclatura SKFJuan José MeroNo ratings yet
- Adriano Costa Sampaio: Electrical EngineerDocument3 pagesAdriano Costa Sampaio: Electrical EngineeradrianorexNo ratings yet
- GBJ0232 - en GLX 3101 T2Document43 pagesGBJ0232 - en GLX 3101 T2mnbvqwert100% (2)
- Arts Class: Lesson 01Document24 pagesArts Class: Lesson 01Lianne BryNo ratings yet
- Medical GeneticsDocument4 pagesMedical GeneticsCpopNo ratings yet
- Gujral FCMDocument102 pagesGujral FCMcandiddreamsNo ratings yet
- Isulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atDocument1 pageIsulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atMysterious StudentNo ratings yet
- LinkageDocument9 pagesLinkageHarshu JunghareNo ratings yet