Professional Documents
Culture Documents
Screening For Abnormal Placentation and Adverse Pregnancy Outcomes With Maternal Serum Biomarkers in The Second Trimester
Uploaded by
Diapositivas08Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Screening For Abnormal Placentation and Adverse Pregnancy Outcomes With Maternal Serum Biomarkers in The Second Trimester
Uploaded by
Diapositivas08Copyright:
Available Formats
DOI: 10.1002/pd.
4370
REVIEW
Screening for abnormal placentation and adverse pregnancy
outcomes with maternal serum biomarkers in the second trimester
Katherine R. Goetzinger and Anthony O. Odibo*
Department of Obstetrics and Gynecology, Washington University, St. Louis, MO, USA
*Correspondence to: Anthony O. Odibo. E-mail: odiboa@wudosis.wustl.edu
ABSTRACT
Second trimester biomarkers were initially introduced with the intent of screening for neural tube defects and then
subsequently for Down syndrome. It was soon realized that these markers can be indirect evidence of abnormal
placentation and, therefore, can be used for screening for adverse pregnancy outcomes. Several new biomarkers have
subsequently been described with conicting ndings regarding their efciency for screening for adverse pregnancy
outcomes. Although a biologically feasible mechanism has been proposed for the role of these biomarkers, they still
fall short of an ideal screening test to be clinically useful. 2014 John Wiley & Sons, Ltd.
Funding sources: None
Conicts of interest: None declared
INTRODUCTION
Second trimester maternal serum biomarker screening was rst
introduced into the eld of obstetrics in the 1970s with the
discovery of elevated levels of alpha-fetoprotein (AFP) in the
maternal serum of pregnancies affected by fetal open neural
tube defects (NTDs). Approximately one decade later, low
maternal serum levels of AFP were identied in pregnancies with
fetal trisomy 21. Since that time, AFP has been combined with
other maternal serum biomarkers, including human chorionic
gonadotrophin (hCG), unconjugated estriol, and inhibin A, in
order to improve the detection rate of fetal aneuploidy in the
second trimester of pregnancy.
These biomarkers are secreted by the placenta and enter the
maternal bloodstream in small amounts throughout gestation.
The detection of abnormal biomarker levels in fetal trisomies
suggest that aneuploid fetuses demonstrate a degree of fetal
placental immaturity that results in both unregulated
hypersecretion and undersecretion of both fetal and placental
products.1 This suggests that abnormal levels of this biomarker
may be representative of abnormal placentation and, thus,
associated with adverse pregnancy outcomes such as
preeclampsia, fetal growth restriction (FGR), preterm delivery,
and fetal loss. Abnormal maternal serum markers obtained during
the rst trimester of pregnancy are also risk factors for subsequent
adverse pregnancy outcomes; however, these rst trimester
markers will not be addressed in this review. The objective of this
review is to critically evaluate the current literature regarding
abnormal levels of maternal serum biomarker in the second
trimester of pregnancy and their association with and screening
efciency for adverse pregnancy outcomes.
Prenatal Diagnosis 2014, 34, 635641
Routine second trimester serum biomarkers
Alpha-fetoprotein
Alpha-fetoprotein was the rst maternal serum biomarker
identied as a screening tool for fetal structural malformations
and chromosomal anomalies. Subsequently, it is the most
studied biomarker to be associated with adverse pregnancy
outcome. AFP is an oncofetal protein that is synthesized by
the yolk sac early in gestation and later by the fetal liver. The
placenta transports small amounts of AFP into the maternal
circulation during early gestation, where it reaches peak
concentrations between 28 and 32 weeks.2 Elevated levels of
maternal serum AFP >2.5 multiples of the median (MoMs)
between 16 and 18 weeks gestation are associated with an
~80% detection rate for open NTDs.3 In the absence of an
NTD, the differential diagnosis for elevated levels of AFP in
maternal serum in the second trimester of pregnancy includes
false positive test reading, inaccurate pregnancy dating,
multiple gestations, intrauterine fetal demise, maternalfetal
hemorrhage, aneuploidy, congenital infection such as
Parvovirus, and other fetal structural malformations, most
commonly abdominal wall defects. However, approximately
1% of women persistently will have an abnormally elevated
serum level of AFP that cannot be accounted for by these
diagnoses.4 It has been demonstrated that these women
remain at increased risk for adverse pregnancy outcomes, with
an incidence as high as 20% to 38% in some studies.5 In 1988,
Barbara Burton demonstrated that patients with an
unexplained elevated maternal serum AFP level 2.5 MoMs
were at a signicantly increased risk for fetal loss beyond
20 weeks gestation, low birth weight, and neonatal death as
2014 John Wiley & Sons, Ltd.
K. R. Goetzinger et al.
636
compared with controls with a normal maternal serum AFP
level.6 Milunsky and colleagues further quantied these risks
demonstrating that patients with unexplained elevated
maternal serum AFP levels 2.0 MoMs were at a twofold
increased risk for preeclampsia, a threefold increased risk for
placental abruption, a fourfold increased risk for low birth
weight, and an eightfold increased risk for fetal death.7 In
1991, Waller and colleagues published a case-control study of
612 women whose pregnancies ended in fetal death and
compared them with 2501 live births. After controlling for
confounders, this study demonstrated a 10.4-fold increased risk
for fetal death in women with a serum AFP level greater than
3.0 MoMs and a 2.4-fold increased risk for fetal death in women
with a serum AFP level between 2.0 and 2.9 MoMs. Most
interestingly, this study also demonstrated that the increased risk
for fetal death persisted throughout gestation, months after the
second trimester AFP level was obtained.8 Most recently, Smith
and colleagues published data suggesting an increased risk for
sudden infant death syndrome [odds ratio (OR) 2.8, 95%
condence interval (CI) 1.45.4] in children born to women with
a maternal serum AFP level in the highest quintile as compared
with those in the lowest quintile; however, this nding may be
partially mediated by FGR and preterm birth.9
The mechanism for these associations remains unclear.
Elevated AFP levels have been found in women who have
experienced early vaginal bleeding that may occur in the setting
of recent or impending fetal death. However, the fact that the risk
for fetal death persists far into the third trimester of pregnancy
suggests an alternative mechanism. It has been hypothesized that
a disruption in the maternalfetal interface allows increased
transfer of AFP into the maternal circulation.10 Others suggest that
elevated AFP levels are a surrogate marker for abnormal
implantation and placental malfunction that are the underlying
pathologic mechanisms for many adverse obstetric outcomes.11,12
This is further substantiated by research demonstrating a large
range of both sonographic and pathologic abnormalities in both
the placenta and umbilical cord in patients with an elevated
maternal serum AFP level.13 Salaa and colleagues identied
distinct placental lesions including chronic villitis, thrombosis,
and infarction in women with elevated maternal serum AFP
levels.14 Furthermore, an increased risk for abnormal placental
adherence (i.e. placenta accreta/increta/percreta) also has been
demonstrated in women with an elevated maternal serum AFP
level, especially in the presence of a placenta previa.15,16
Risk stratication has been evaluated to identify those
women at highest risk for adverse pregnancy outcome
among those with an elevated AFP level. Using maternal
characteristics and medical comorbidities, Chandra and
colleagues assigned women into high-risk and low-risk groups
based on their a priori risk of having an obstetric complication.
They found that women with an unexplained elevated
maternal serum AFP level were at increased risk for obstetric
complications regardless of their prepregnancy risk status.12
Biophysical measurements such as uterine artery Doppler also
have been combined with serum levels of AFP in order to
improve screening efciency. Multiple small studies have
reported an increased risk for adverse pregnancy outcomes in
patients with abnormal second trimester uterine artery
Prenatal Diagnosis 2014, 34, 635641
Doppler studies in the setting of an unexplained elevated
maternal serum AFP level.1721 Bromley and colleagues
demonstrated that severe grade II uterine artery notching was
associated with a greater than threefold increased risk for a
composite perinatal morbidity including preterm delivery <37
weeks, birth weight <10th percentile for gestational age, and
fetal/neonatal death.19 Similarly, Konchak and colleagues
demonstrated an increased risk for preeclampsia, preterm
birth, and low birth weight in patients with uterine artery
notching and an elevated maternal serum AFP level.20 Despite
these associations, the positive predictive value (PPV) of these
combined tests remains relatively low. In one of the largest
published series, the combination of an elevated serum level
of AFP and bilateral uterine artery notching demonstrated a
PPV of 21% and 43% for preeclampsia and FGR, respectively.21
Obstetric surveillance and pregnancy management in these
patients remains controversial. Although many practitioners will
opt to follow these patients with increased frequency of antenatal
visits, uterine artery Doppler studies, serial ultrasounds for fetal
growth, and antenatal surveillance, there is no existing evidence
to support any specic obstetric surveillance protocol.22 In 2001,
Huerta-Enochian and colleagues published a retrospective cohort
study of 136 pregnancies with maternal serum AFP levels >2.0
MoMs. This study demonstrated that intensive antenatal
surveillance consisting of twice-weekly nonstress tests and
amniotic uid index determinations did not achieve earlier or
improved detection of adverse pregnancy outcome. In fact, all
adverse outcomes were either detected with routine pregnancy
care or remained undetected despite intensive antenatal
surveillance.23 Given the retrospective design of this study, timing
of initiation of antenatal surveillance was left to the discretion of
the provider. It remains unclear whether increased obstetric
surveillance can improve outcomes in patients with an
unexplained elevated maternal serum AFP level.
Far less data exists on the association between unexplained
low levels of maternal serum AFP and adverse pregnancy
outcomes. There are a few small cohort studies suggesting a
paradoxically increased risk for low birth weight and fetal
demise in patients with maternal serum AFP levels <0.25
MoMs. Regrettably, chromosomal analysis in many of these
demise cases was not obtained; therefore, fetal trisomy, a
well-established cause of low AFP levels, cannot be denitely
ruled out in all cases of demise.6,8,24,25 This limitation could
introduce signicant ascertainment bias to the results of such
studies, thereby, decreasing the robustness of their ndings.
Other studies have suggested an increased incidence of high
birth weight infants and associated delivery trauma in women
with low maternal serum AFP levels.26 Finally, still other
studies suggest a much more favorable pregnancy outcome
in the setting of low maternal serum AFP levels, reecting an
intact maternalfetalplacental unit.12,27,28
Human chorionic gonadotrophin
Soon after the discovery that low levels of maternal serum AFP
were associated with an increased risk for trisomy 21, it also
was discovered that high levels of maternal serum hCG
(typically 2.5 MoMs) also could be found in aneuploid
pregnancies.29 hCG is a glycoprotein produced by the placental
2014 John Wiley & Sons, Ltd.
Second trimester biomarkers screening
syncytiotrophoblast. It has been hypothesized that decreased
placental perfusion, with resultant hypoxic injury, may lead to
increased hCG production.30 Placental pathologic evaluation from
pregnancies with unexplained elevated maternal serum hCG
levels shows an increased incidence of retroplacental hematomas,
large for gestational age placentas, increased decidual plasma
cell inltrates, and low mean fetoplacental weight ratios.
Morphometric placental analysis also demonstrates an increased
volume of hCG-positive trophoblast per unit surface area.31
Together, these ndings suggest that elevated levels of hCG may
be reective of placental dysfunction and, therefore, also may
have an association with adverse pregnancy outcomes.
In a cohort study of over 25 000 pregnancies, Benn and
colleagues demonstrated a signicantly increased risk for
fetal/neonatal death, preterm birth, low birth weight, and
preeclampsia in patients with a maternal serum hCG >3.0
MoMs.32 Subsequent studies have produced similar
results.12,3335 In fact, Chandra and colleagues demonstrated
that the risk for adverse outcome was increased even when
maternal hCG levels exceeded 2.0 MoMs, with the most
pronounced risk being for intrauterine fetal demise [relative
risk (RR) 4.91, 95% CI 2.688.98].12 Although Lepage and
colleagues were underpowered to study intrauterine fetal
demise, they did demonstrate an association between elevated
maternal serum hCG levels and spontaneous miscarriage,
small for gestational age, pregnancy-associated hypertensive
disorders, and preterm delivery. Interestingly, they also were
able to demonstrate a doseresponse relationship, as 87%
(13/15) of pregnancies with extremely elevated maternal serum
hCG levels (10 MoMs) in their cohort experienced at least one
adverse pregnancy outcome.33 Alternatively, a large casecontrol study by Spencer demonstrated that an isolated
elevated maternal serum hCG level (>2.0 MoMs) was not
associated with any adverse pregnancy outcome.36
Furthermore, Walton and colleagues showed only a slight
association between maternal serum hCG levels >2.0 MoMs
and the adverse outcomes of pregnancy-induced hypertension
and preterm delivery and no association with premature
rupture of membranes nor FGR. However, that study did show
that higher levels of hCG were associated with stillbirth with an
OR of 1.4 (95% CI 1.11.9) for every increase of one MoM.37
In rare case of elevated levels of both maternal serum AFP
and hCG, it is more apparent that the risk for adverse
pregnancy outcome is signicant.12,36,38 Spencer and
colleagues observed a sixfold increased risk for preterm
delivery and a sevenfold increased risk for stillbirth when both
AFP and free hCG were >2.0 MoMs.36 Chandra and colleagues
demonstrated a risk increase for FGR from a RR of 1.28 in the
setting of an isolated maternal hCG level to a RR of 4.11 in
the setting of elevated levels of both AFP and hCG. Similarly,
the risk of intrauterine fetal demise was reported to increase
to 13.8 when both AFP and hCG levels are elevated.12
Unconjugated estriol and inhibin A
Unconjugated estriol and Inhibin A are the other two serum
analytes that comprise the quadruple second trimester
aneuploidy screen. Unconjugated estriol levels are typically
<0.7 MoMs in pregnancies affected by trisomy 21, whereas
Prenatal Diagnosis 2014, 34, 635641
637
Inhibin A levels are typically elevated >1.6 to 1.8 MoMs in
trisomy 21.3941 Low unconjugated estriol levels have been
associated with a number of adverse pregnancy outcomes.4246
Yaron and colleagues observed that unconjugated estriol
levels <0.5 MoM were associated with pregnancy-induced
hypertension, miscarriage, FGR, and fetal death.42 Dugoff and
colleagues later demonstrated that low unconjugated estriol
levels 0.5 MoMs were associated with an increased risk for birth
weight less than the fth percentile and less than the tenth
percentile for gestational age and fetal loss 24 weeks. In that
study, there was no association found between low estriol levels
and preterm birth, preeclampsia, or fetal demise >24 weeks.43 In
another study restricted only to cases of FGR, patients with a low
estriol level <0.5 MoMs were at a greater than vefold increase
for composite adverse perinatal outcome, with a sensitivity of
36% and a specicity of 87%. This study suggested that serum
biomarker screening in the second trimester may be able to
differentiate a subset of growth-restricted fetuses at highest
risk for adverse outcome.44 The pathophysiologic mechanism
behind these associations with low estriol level remains
unclear. In the 1970s, serial urine estriol measurements were
routinely obtained during the third trimester of pregnancy in
order to evaluate for fetal well-being, with normal levels
being highly predictive a healthy fetus.45 Successful biosynthesis
of unconjugated estriol requires contributions both from the
fetus and placenta; therefore, abnormally low estriol levels
may be representative of a dysfunctional maternalfetal
placental unit. This is further illustrated by the association of
extremely low estriol levels in both fetal genetic and metabolic
placental disorders such as placental sulfatase deciency and
SmithLemliOpitz syndrome.47,48
Inhibin A is a member of the transforming growth factor
superfamily. Outside of pregnancy, the ovary is primarily
responsible for its production; however, during pregnancy,
there is a shift towards increased placental production of this
glycoprotein.49,50 Inhibin A is primarily localized to the surface
layer of the syncytiotrophoblast. Abnormal trophoblastic
invasion into the myometrium with subsequent hypoxic
placental injury, as can be seen in preeclampsia, causes
damage to the syncytiotrophoblast and leakage of inhibin A
into the maternal circulation. Additionally, hypoxic placental
injury can also result in proliferation of the cytotrophoblast
layer, resulting in increased production of inhibin A.51,52 Either
or both of these mechanisms could explain the biologic
plausibility of these ndings.
Elevated inhibin A levels in chromosomally normal fetuses
have been most extensively studied for their association with
preeclampsia.43,51,5355 Aquilina and colleagues demonstrated
that women with inhibin A levels >2.0 MoMs are at an
increased risk for all preeclampsia (OR 9.4, 95% CI 4.619.3)
and preeclampsia necessitating delivery <37 weeks (OR 18.2,
95% CI 6.054.8).51 These ndings were conrmed in a follow
up study that demonstrated a sensitivity of 48.6% and
specicity of 90% for the prediction of preeclampsia.54 Other
studies have demonstrated an even higher screening efciency
for elevated inhibin A levels and preeclampsia, with a
sensitivity of 71.4% and specicity of 96.3%.55 Other studies
have demonstrated an association between elevated inhibin
2014 John Wiley & Sons, Ltd.
K. R. Goetzinger et al.
638
A levels and FGR; however, these associations appear to be less
robust.43,51 The addition of uterine artery Doppler studies to
enhance the screening efciency of inhibin A has been
proposed; however, studies have produced conicting
results.5558 Ultimately, it appears that while abnormal uterine
artery Doppler studies in the setting of elevated inhibin A levels
may increase the detection rate of adverse pregnancy
outcomes, the nding of normal uterine artery Doppler
studies does not negate the increased risk for adverse
pregnancy outcome in the setting of abnormal second
trimester serum screening.57
The quadruple screen: combinations of serum markers
Although it is clear that individual second trimester maternal
serum biomarkers can be predictive of multiple adverse
pregnancy outcomes, these biomarkers are rarely measured
individually. Instead, they are interpreted as part of the second
trimester quad screen for fetal aneuploidy. Currently, there
are no published studies that prospectively evaluate the use
of the quad screen for the primary intent of quantifying the risk
of adverse pregnancy outcomes; however, multiple studies
have evaluated these outcomes in patients pursuing second
trimester serum screening for the purpose of aneuploidy
detection. In a secondary analysis of the FASTER trial, Dugoff
and colleagues evaluated both the individual components of
the quad screen and their various combinations to determine
their screening efciency for adverse pregnancy outcome. That
study found that combinations of at least two abnormal
biomarkers were more strongly predictive for any adverse
pregnancy outcome compared with only one abnormal
marker. That association became stronger with increasing
numbers of abnormal biomarkers. For example, the adjusted
OR for fetal loss 24 weeks increased from 3.63 (95% CI 1.81
7.27) in the setting of elevated AFP levels 2.0 MoMs to 8.81
(95% CI 5.213.12) in the setting of two abnormal biomarkers.
This risk association increased even further to 23.15 (95% CI
12.6142.49) in the setting of three or more abnormal
biomarkers.43 Huang and colleagues observed similar results
when evaluating combinations of AFP, hCG, and unconjugated
estriol in addition to pregnancy-associated plasma protein A
(PAPP-A) levels obtained in the rst trimester of pregnancy.46
Despite the strong associations observed with multiple
abnormal serum markers, the sensitivity and PPV for adverse
pregnancy outcomes remain relatively low, and the false
positive rates can be high. As the rst trimester aneuploidy
screening and cell-free fetal DNA gain more and more
popularity, the frequency at which second trimester
aneuploidy screening will continue to be obtained remains
questionable. Given the modest predictive efciency of these
second trimester serum biomarkers and the lack of
management strategies that are proven to improve pregnancy
outcome, it is unlikely that second trimester serum biomarker
testing can be recommended as a population-based screening
tool for adverse pregnancy outcome; however, when screening
is performed for the clinical indication of aneuploidy
detection, abnormal serum screening results may be used to
identify high-risk patients and to guide clinical management
at the discretion of the physician.22
Prenatal Diagnosis 2014, 34, 635641
Beyond the quadruple screen
Pregnancy-associated plasma protein A
Pregnancy-associated plasma protein A is an insulin-like
growth factor binding protein (IGFBP) protease with specicity
for IGFBP 2 and 4.58 Reduced levels of PAPP-A may result in
increased amounts of IGF being bound to its carrier proteins
and, hence, not available at the cell receptor level to stimulate
fetal growth and trophoblast invasion of the decidua.59
Many studies have reported reduced maternal serum PAPP-A
concentration at 11 to 14 weeks and increased risk for
subsequent development of preeclampsia, small for gestational
age, and preterm delivery; however,58,6063 only few studies have
evaluated the association between PAPP-A and adverse
outcomes in the second trimester. For example, in a case-control
study, DAnna et al. compared PAPP-A levels drawn between 14
and 17 weeks in 40 women who developed preeclampsia with
562 that had uncomplicated pregnancies.64 The area under the
receiver operating characteristic curve for prediction of
preeclampsia was 0.88 with a 95% CI of 0.80 to 0.96. For a xed
false positive rate of 5%, the detection rate for preeclampsia
was 66.7%. The ndings from this study are yet to be validated
by other studies. In fact, another case-control study found no
difference in early second trimester PAPP-A levels between
77 cases with preeclampsia and 224 unaffected pregnancies.65
A disintegrin and metalloprotease
A disintegrin and metalloprotease 12 (ADAM12) is a placentaderived multidomain glycoprotein involved in controlling fetal
and placental growth and development. Human ADAM12
exists in two forms: ADAM12-L (long) and ADAM12-S (short).
ADAM12-S is the secreted form of ADAM12 and is also an
IGFBP protease but with specicity for IGFBP 3 and 5.66,67
ADAM12 can also bind to adhesion receptors and mediate
shedding of oxytocinase, which may be associated with
progressive growth of placenta.68,69
Reduced ADAM12 has been shown to be a potential marker of
a preeclampsia and intrauterine growth restriction (IUGR) in the
rst trimester.7072 Similar to PAPP-A, there are only a handful of
studies estimating the value of ADAM12 as a biomarker for
preeclampsia in the second trimester. DAnna et al., using the
same population mentioned earlier, evaluated ADAM12 in
40 cases with preeclampsia compared with 562 unaffected
pregnancies.64 The area under the curve for predicting
preeclampsia was 0.95, with a 95% CI of 0.91 to 0.98. For a xed
false positive rate of 6%, the detection rate for preeclampsia
using ADAM12 was 77.8%. These ndings were not conrmed
in an early second trimester study by Bestwick et al.65
Angiogenic factors
Circulating angiogenic factors include vascular endothelial
growth factor and placental growth factor. They are thought
to contribute to normal trophoblastic proliferation and
implantation.73 Soluble fms-like tyrosine kinase-1 (sFlt-1) is
able to block the effects of vascular endothelial growth factor
and PIGF by inhibiting interaction with their receptors.
Ischemic trophoblasts have been shown to synthesize
antiangiogenic factors, notably sFlt-1.74 This deprives the
maternal vascular endothelium of these essential angiogenic
2014 John Wiley & Sons, Ltd.
Second trimester biomarkers screening
factors and causes systemic endothelial dysfunction that may
culminate in the preeclamptic syndrome.75,76
Numerous studies have documented that placental growth
factor concentration in the second trimester is reduced in
women who go on to develop preeclampsia/IUGR73,7779 and
inversely correlates with the severity of the diseases.73,75,8082
On the other hand, sFlt-1 levels in the second trimester are
increased in women destined to develop preeclampsia/
IUGR.75 In the prospective multicenter cohort study Screening
for Pregnancy Endpoints, clinical risk factors, serum PIGF, sFlt1, and soluble endoglin were measured at 14 to 16 weeks in
3529 nulliparous women, including 47 that later developed
preterm preeclampsia needing early delivery. The combination
of clinical risk factors and PIGF resulted in the best area under
the curve of 0.84 (95% CI of 0.770.91). With a xed false
positive rate of 5%, the sensitivity for predicting preeclampsia
was only 45% .83 The addition of sFlt-1 or soluble endoglin
did not improve the prediction model any further. Repeating
the analysis with samples drawn between 19 and 21 weeks
and adding uterine artery Doppler did not signicantly
improve the screening efciency for preeclampsia. The authors
concluded that while these angiogenic markers can identify
nulliparous women at risk for developing preeclampsia, their
performance was not sufciently efcient to be introduced
into routine clinical practice.83
CONCLUSION
In recent years, much interest has been shown in identifying
biomarkers of placental dysfunction in the rst and second
639
trimesters of pregnancy that can predict women at risk for
preeclampsia and fetal growth restriction. The published
literature clearly supports a positive association between
abnormal levels of these serum markers, which is
strengthened in the presence of more than one abnormal
marker. Despite these associations, the predictive accuracy
of these biomarkers, both in isolation or combined with other
clinical risk factors, still falls short of the ideal for clinically
useful screening tests. Given the clinical importance of
recognizing those patients at high risk for developing adverse
pregnancy outcomes such as preeclampsia, continued
effort at identifying markers with better discrimination
should be encouraged.
WHATS ALREADY KNOWN ABOUT THIS TOPIC?
Several studies have been published on the role of placental
biomarkers in screening for adverse outcomes.
Although it is clear that strong associations between second
trimester serum biomarkers and adverse pregnancy outcomes
do exist, the predictive accuracy of these markers remain
limited for use as a population-based screening tool in
clinical practice.
WHAT DOES THIS STUDY ADD?
This review summarizes the studies on these biomarkers in a
systematic fashion and critically evaluates the current role of second
trimester biomarkers in screening for preeclampsia and other
adverse outcomes.
REFERENCES
1. Norton ME. Genetics and prenatal diagnosis. In Ultrasonography in
Obstetrics and Gynecology (5th edn), Callen PW (ed.). Philadelphia:
Saunders Elsevier, 2008;2659.
2. Main DM, Mennuti MT. Neural tube defects: issues in prenatal
diagnosis and counseling. Obstet Gynecol 1986;67:116.
3. Wald NJ, Cuckle H, Brock JH, et al. Maternal serum-alpha-fetoprotein
measurement in antenatal screening for anencephaly and spina bida
in early pregnancy. Report of UK collaborative study on alphafetoprotein in relation to neural tube defects. Lancet 1977;1:132332.
4. Wilkins HL. Unexplained elevated maternal serum alpha-fetoprotein:
what is the appropriate follow up? Curr Opin Obstet Gynecol
1998;10:46974.
5. Katz VL, Chescheir NC, Cefalo RC. Unexplained elevations of maternal
serum alpha-fetoprotein. Obstet Gynecol Surv 1990;45:71926.
6. Burton BK. Outcome of pregnancy in patients with unexplained
elevated or low levels of maternal serum alpha-fetoprotein. Obstet
Gynecol 1988;72:70913.
7. Milunsky A, Jick SS, Bruell CL, et al. Predictive values, relative risks, and
overall benets of high and low maternal serum alpha-fetoprotein
screening in singleton pregnancies: new epidemiologic data. Am J
Obstet Gynecol 1989;161:2917.
8. Waller DK, Lustig LS, Cunningham GC, et al. Second-trimester maternal
serum alpha-fetoprotein levels and the risk of subsequent fetal death.
New Engl J Med 1991;325:610.
9. Smith GC, Wood AM, Pell JP, et al. Second-trimester maternal serum
levels of alpha-fetoprotein and the subsequent risk of sudden infant
death syndrome. New Eng J Med 2004;351:97886.
10. Berkeley AS, Killackey MA, Cedarqvist LL. Elevated maternal serum
alpha-fetoprotein levels associated with breakdown in fetalmaternal
placental barrier. Am J Obstet Gynecol 1983;146:85961.
Prenatal Diagnosis 2014, 34, 635641
11. Morssink LP, de Wolf BT, Kornman LH, et al. The relation between
serum markers in the second trimester and placental pathology: a study
on extremely small for gestational age fetuses. BJOG 1996;103:77983.
12. Chandra S, Scott H, Dodds L, et al. elevated maternal serum fetoprotein and/or human chorionic gonadotropin and the risk of
adverse outcomes. Am J Obstet Gynecol 2003;189:77581.
13. Jauniaux E, Moscoso G, Campbell S, et al. Correlation of ultrasound and
pathologic ndings of placental anomalies in pregnancies with elevated
maternal serum alpha-fetoprotein. Eur J Obstet Gynecol Reprod Biol
1990;37:21930.
14. Salaa CM, Silberman L, Herrera NE, Mahoney MJ. Placental pathology
at term associated with elevated mid-trimester maternal serum fetoprotein concentration. Am J Obstet Gynecol 1988;158:10646.
15. Zelop C, Nadel A, Frigoletto FD Jr., et al. Placenta accreta/precreta/
increta: a cause of elevated maternal serum alpha-fetoprotein. Obstet
Gynecol 1992;80:6934.
16. Kupferminc MJ, Tamura RK, Wigton TR, et al. Placenta accreta is
associated with elevated maternal serum alpha-fetoprotein. Obstet
Gynecol 1993;82:2669.
17. Aristidou A, Van den Hof MC, Campbell S, Nicolaides K. Uterine artery
Doppler in the investigation of pregnancies with raised maternal serum
alpha-fetoprotein. BJOG 1990;97:4315.
18. Karsidag AY, Buyukbayrak EE, Kars B, et al. The relationship between
unexplained elevated serum markers in triple test, uterine artery
Doppler measurements and adverse pregnancy outcome. J Pak Med
Assoc 2010;60:1816.
19. Bromley B, Frigoletto FD, Harlow BL, et al. The role of Doppler
velocimetry in the structurally normal second-trimester fetus with
elevated levels of maternal serum alpha-fetoprotein. Ultrasound Obstet
Gynecol 1994;4:37780.
2014 John Wiley & Sons, Ltd.
640
20. Konchak PS, Bernstein IM, Capeless EL. Uterine artery Doppler
velocimetry in the detection of adverse obstetric outcomes in women
with unexplained elevated maternal serum alpha-fetoprotein levels. Am
J Obstet Gynecol 1995;173:11159.
21. Audibert F, Benchimol Y, Benattar C, et al. Prediction of preeclampsia or
intrauterine growth restriction by second trimester serum screening
and uterine Doppler velocimetry. Fetal Diagn Ther 2005;20:4853.
22. Gagnon A, Wilson RD, Audibert F, et al. Obstetrical complications
associated with abnormal serum marker analytes. J Obstet Gynaecol
Can 2008;30:91849.
23. Huerta-Enochian G, Katz V, Erfurth S. The association of abnormal
alpha-fetoprotein and adverse pregnancy outcome: does increased fetal
surveillance affect pregnancy outcome? Am J Obstet Gynecol
2001;184:154953.
24. Wald NJ, Cuckle HS, Boreham J, Turnball AC. Maternal serum alphafetoprotein and birth weight. Br J Obstet Gynaecol 1980;87:8603.
25. Davenport DM, Macri JN. The clinical signicance of low maternal
serum alpha-fetoprotein. Am J Obstet Gynecol 1983;15:65761.
26. Baschat AA, Harman CR, Farid G, et al. Very low second-trimester
maternal alpha-fetoprotein: association with high birth weight. Obstet
Gynecol 2002;99:5316.
27. Simpson JL, Baum LD, Depp R, et al. Low maternal serum alpha-fetoprotein
and perinatal outcomes. Am J Obstet Gynecol 1987;156:85262.
28. Waller DK, Lustig LS, Cunningham GC, et al. The association between
maternal serum alpha-fetoprotein and preterm birth, small for
gestational age infants, pre-eclampsia, and placental complications.
Obstet Gynecol 1996;88:81622.
29. Bogart MH, Pandian MR, Jones OW. Abnormal maternal serum
chorionic gonadotropin levels in pregnancies with fetal chromosome
abnormalities. Prenat Diagn 1987;7:62330.
30. Fox H. Effect of hypoxia on trophoblast in organ culture: a morphologic
and autoradiographic study. Am J Obstet Gynecol 1970;107:105864.
31. Liu DF, Dickerman LH, Redline RW. Pathologic ndings in pregnancies
with unexplained increases in midtrimester maternal serum human
chorionic gonadotropin levels. Am J Clin Pathol 1999;111:20915.
32. Benn PA, Horne D, Briganti S, et al. Elevated second-trimester maternal
serum hCG alone or in combination with elevated alpha-fetoprotein.
Obstet Gynecol 1996;87:21722.
33. Lepage N, Chitayat D, Kingdom J, Huang T. Association between
second-trimester isolated high maternal serum human chorionic
gonadotropin levels and obstetric complications in singleton and twin
pregnancies. Am J Obstet Gynecol 2003;188:13549.
34. Vaillant P, David E, Constant I, et al. Validity of nulliparas of increased
beta-human chorionic gonadotropin at mid-term for predicting
pregnancy-induced hypertension complicated with proteinuria and
intrauterine growth retardation. Nephron 1996;72:55763.
35. Palacio M, Jauniaux E, Kingdom J, et al. Perinatal outcome in
pregnancies with a positive serum screening for Downs syndrome due
to elevated levels of free -human chorionic gonadotropin. Ultrasound
Obstet Gynecol 1999;13:5862.
36. Spencer K. Second-trimester prenatal screening for Down syndrome
and the relationship of maternal serum biochemical markers to
pregnancy complications with adverse outcome. Prenat Diagn
2000;20:6526.
37. Walton DL, Norem CT, Schoen EJ, et al. Second-trimester serum
chorionic gonadotropin concentrations and complications and
outcome of pregnancy. N Engl J Med 1999;341:20338.
38. Chitayat D, Farrell SA, Huang T, et al. Double positive maternal serum
screening results for Down syndrome and open neural tube defects: an
indicator for fetal structural or chromosomal abnormalities and adverse
obstetric outcomes. Am J Obstet Gynecol 2002;187:75863.
39. Wald NJ, Cuckle HS, Densem JW, et al. Materanl serum unconjugated
oestriol as an antenatal screening test for Downs syndrome. BJOG
1988;95:33441.
40. Wenstrom KD, Owen J, Chu DC, Boots L. Elevated second-trimester
dimeric inhibin A levels identify Down syndrome pregnancies. Am J
Obstet Gynecol 1997;177:9926.
41. Spencer K, Wallace EM, Ritoe S. Second-trimester dimeric inhibin-A in
Downs syndrome screening. Prenat Diagn 1996;16:110110.
42. Yaron Y, Cherry M, Kramer RL, et al. Second-trimester maternal serum
marker screening: maternal serum alpha-fetoprotein, beta-human
chorionic gonadotropin, estriol, and their various combinations as
predictors of pregnancy outcome. Am J Obstet Gynecol 1999;181:96874.
Prenatal Diagnosis 2014, 34, 635641
K. R. Goetzinger et al.
43. Dugoff L, Hobbins JC, Malone FD, et al. Quad screen as a predictor of
adverse pregnancy outcome. Obstet Gynecol 2005;106:2607.
44. Ilagan JG, Stamilio DM, Ural SH, et al. Abnormal multiple marker
screens are associated with adverse perinatal outcomes in cases of
intrauterine growth restriction. Am J Obstet Gynecol 2004;191:14659.
45. Kowalczyk TD, Cabaniss ML, Cusmano L. Association of low
unconjugated estriol in the second trimester and adverse pregnancy
outcome. Obstet Gynecol 1998;91:396400.
46. Huang T, Hoffman B, Meschino W, et al. Prediction of adverse
pregnancy outcomes by combinations of rst and second trimester
biochemistry markers used in the routine prenatal screening of Down
syndrome. Prenat Diagn 2010;30:4717.
47. Bradley LA, Palomaki GE, Knight GJ, et al. Levels of unconjugated estriol
and other maternal serum markers in pregnancies with SmithLemli
Opitz syndrome fetuses. Am J Med Genet 1999;82:3558.
48. Bradley LA, Canick JA, Palomaki GE. Undetectable maternal serum
unconjugated estriol levels in the second trimester: risk of perinatal
complications associated with placental sulfatase deciency. Am J
Obstet Gynecol 1997;176:5315.
49. Illingworth PJ, Reddi K, Wickings EJ, Baird DT. The source of inhibin
secretion during the human menstrual cycle. J Clin Endocrinol Metabol
1991;73:66773.
50. Qu J, Thomas K. Inhibin and activin production in the human placenta.
Endocr Rev 1995;16:485507.
51. Aquilina J, Barnett A, Thompson O, Harrington K. Second-trimester
maternal serum inhibin A concentrations as an early marker for
preeclampsia. Am J Obstet Gynecol 1999;181:1316.
52. McCluggage WG, Ashe P, McBride H, et al. Localization of the cellular
expression of inhibin in trophoblastic tissue. Histopathology
1998;32:2526.
53. Cuckle H, Sehmi I, Jones R. Maternal serum inhibin A can predict preeclampsia. BJOG 1998;105:11013.
54. Aquilina J, Maplethorpe R, Ellis P, Harrington K. Correlation between
second trimester maternal serum inhibin-A and human chorionic
gonadotropin for the prediction of pre-eclampsia. Placenta
2000;21:48792.
55. Ay E, Kavak ZN, Elter K, et al. Screening for pre-eclampsia by using
maternal serum inhibin A, activin A, human chorionic gonadotropin,
unconjugated estriol, and alpha-fetoprotein levels and uterine artery
Doppler in the second trimester of pregnancy. Aust N Z J Obstet
Gynaecol 2005;45:2838.
56. Aquilina J, Thompson O, Thilaganathan B, Harrington K. Improved
early prediction of pre-eclampsia by combining second-trimester
maternal serum inhibin-A and uterine artery Doppler. Ultrasound
Obstet Gynecol 2001;17:47784.
57. Fillippi E, Staughton J, Peregrine E, et al. Uterine artery Doppler and
adverse pregnancy outcome in women with extreme levels of
fetoplacental proteins used for Down syndrome screening. Ultrasound
Obstet Gynecol 2011;37:52052759.
58. Pihl K, Larsen T, Krebs L, Christiansen M. First trimester maternal
serum PAPP-A, beta-hCG and ADAM12 in prediction of small-forgestational-age fetuses. Prenat Diagn 2008;28(12):11315.
59. Bale LK, Conover CA. Disruption of insulin-like growth factor-II
imprinting during embryonic development rescues the dwarf
phenotype of mice null for pregnancy-associated plasma protein-A. J
Endocrinol 2005;186:32531.
60. Spencer K, Cowans NJ, Chefetz I, et al. First-trimester maternal serum
PP-13, PAPP-A and second-trimester uterine artery Doppler pulsatility
index as markers of pre-eclampsia. Ultrasound Obstet Gynecol
2007;29(2):12834.
61. Cowans NJ, Spencer K. First-trimester ADAM12 and PAPP-A as markers
for intrauterine fetal growth restriction through their roles in the
insulin-like growth factor system. Prenat Diagn 2007;27(3):26471.
62. Poon LC, Maiz N, Valencia C, et al. First-trimester maternal serum
pregnancy-associated plasma protein-A and pre-eclampsia. Ultrasound
Obstet Gynecol 2009;33(1):2333.
63. Leung TY, Sahota DS, Chan LW, et al. Prediction of birth weight by fetal
crown-rump length and maternal serum levels of pregnancy-associated
plasma protein-A in the rst trimester. Ultrasound Obstet Gynecol
2008;31(1):104.
64. DAnna R, Baviera G, Giordano D, et al. ADAM 12 and PAPP-A at
1417 weeks gestation as biomarkers of preeclampsia. Prenat Diagn
2011;31:6024
2014 John Wiley & Sons, Ltd.
Second trimester biomarkers screening
65. Bestwick JP, George LM, Wu T, et al. The value of early second-trimester PAPP-A
and ADAM12 in screening for pre-eclampsia. J Med Screen 2012;19:514.
66. Loechel F, Fox JW, Murphy G, et al. ADAM 12-S cleaves IGFBP-3 and
IGFBP-5 and is inhibited by TIMP-3. Biochem Biophys Res Commun
2000;278:5115.
67. Shi Z, Xu W, Loechel F, et al. ADAM 12, a disintegrin metalloprotease,
interacts with insulin-like growth factor-binding protein-3. J Biol Chem
2000;275:1857480.
68. Iba K, Albrechtsen R, Gilpin B, et al. The cysteine-rich domain of human
ADAM 12 supports cell adhesion through syndecans and triggers
signaling events that lead to beta1 integrin-dependent cell spreading. J
Cell Biol 2000;149:114356.
69. Ito N, Nomura S, Iwase A, et al. ADAMs, a disintegrin and
metalloproteinases, mediate shedding of oxytocinase. Biochem Biophys
Res Commun 2004;314(4):100813.
70. Laigaard J, Srensen T, Placing S, et al. Reduction of the disintegrin and
metalloprotease ADAM12 in preeclampsia. Obstet Gynecol
2005;106:1449.
71. Spencer K, Cowans NJ, Stamatopoulou A. ADAM12s in maternal serum
as a potential marker of pre-eclampsia. Prenat Diagn 2008;28:2126.
72. Cowans NJ, Spencer K. First-trimester ADAM12 and PAPP-A as markers
for intrauterine fetal growth restriction through their roles in the
insulin-like growth factor system. Prenat Diagn 2007;27:26471.
73. Taylor RN, Grimwood J, Taylor RS, et al. Longitudinal serum
concentrations of placental growth factor: evidence for abnormal
placental angiogenesis in pathologic pregnancies. Am J Obstet Gynecol
2003;188:17782.
74. Koga K, Osuga Y, Tajima T, et al. Maternal serum soluble fms-like
tyrosine kinase 1 concentrations are not increased in early pregnancy
and decrease more slowly postpartum in women who develop
preeclampsia. Am J Obstet Gynecol 2005;193:18591.
Prenatal Diagnosis 2014, 34, 635641
641
75. Maynard SE, Min JY, Merchan J, et al. Excess placental soluble fms-like
tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction,
hypertension, and proteinuria in preeclampsia. J Clin Invest
2003;111:64958.
76. Sugimoto H, Hamano Y, Charytan D, et al. Neutralization of circulating
vascular endothelial growth factor (VEGF) by anti-VEGF antibodies and
soluble VEGF receptor 1 (sFlt-1) induces proteinuria. J Biol Chem
2003;278:126058.
77. Crispi F, Llurba E, Domnguez C, et al. Predictive value of angiogenic
factors and uterine artery Doppler for early- versus late-onset preeclampsia and intrauterine growth restriction. Ultrasound Obstet
Gynecol 2008;31:3039.
78. Thadhani R, Mutter WP, Wolf M, et al. First trimester placental growth
factor and soluble fms-like tyrosine kinase 1 and risk for preeclampsia. J
Clin Endocrinol Metab 2004;89:7705.
79. Teixeira PG, Cabral AC, Andrade SP, et al. Placental growth factor (PlGF)
is a surrogate marker in preeclamptic hypertension. Hypertens
Pregnancy 2008;27:6573.
80. Lam C, Lim KH, Karumanchi SA. Circulating angiogenic factors in the
pathogenesis and prediction of preeclampsia. Hypertension 2005;46
(5):107785.
81. Moore Simas TA, Crawford SL, Solitro MJ, et al. Angiogenic factors for
the prediction of preeclampsia in high-risk women. Am J Obstet
Gynecol 2007;197(3):244. e18.
82. Akolekar R, Zaragoza E, Poon LC, et al. Maternal serum placental
growth factor at 11 + 0 to 13 + 6 weeks of gestation in the prediction of
pre-eclampsia. Ultrasound Obstet Gynecol 2008;32(6):7329.
83. Myers JE, Kenny LC, McCowan LME, et al. Angiogenic factors
combined with clinical risk factors to predict preterm pre-eclampsia
in nulliparous women: a predictive test accuracy study. BJOG
2013;120:121523.
2014 John Wiley & Sons, Ltd.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Utero-Placental Doppler Ultrasound For Improving Pregnancy Outcome (Review)Document50 pagesUtero-Placental Doppler Ultrasound For Improving Pregnancy Outcome (Review)Diapositivas08No ratings yet
- Intrauterine Growth RestrictionDocument4 pagesIntrauterine Growth RestrictionFate ZephyrNo ratings yet
- Breech PresentationDocument122 pagesBreech Presentationlieynna4996100% (1)
- Premature Rupture of MembranesDocument29 pagesPremature Rupture of MembranesIda YosopaNo ratings yet
- College of Nursing NURSING Care PlanDocument3 pagesCollege of Nursing NURSING Care PlanToyour EternityNo ratings yet
- Podocyturia As A DiagnosticMarker For Preeclampsia 2012Document6 pagesPodocyturia As A DiagnosticMarker For Preeclampsia 2012Diapositivas08No ratings yet
- Methods of Prediction and Prevention of Pre-Eclampsia (Full)Document286 pagesMethods of Prediction and Prevention of Pre-Eclampsia (Full)Diapositivas08No ratings yet
- ESHRE POR Criterios Bologna Hum. Reprod.-2011-FerrarettiDocument9 pagesESHRE POR Criterios Bologna Hum. Reprod.-2011-FerrarettiDiapositivas08No ratings yet
- Proteína S Libre en Embarazadas Normales: Comparación Entre Dos MétodosDocument6 pagesProteína S Libre en Embarazadas Normales: Comparación Entre Dos MétodosDiapositivas08No ratings yet
- Stillbirth Series OverviewDocument38 pagesStillbirth Series OverviewZaroon AhmedNo ratings yet
- Gynae Osce NotesDocument1 pageGynae Osce NotesSara QutubuddinNo ratings yet
- AbortionDocument7 pagesAbortionjamesihno100% (1)
- Model Edukasi Postnatal Melalui Pendekatan FamilyDocument19 pagesModel Edukasi Postnatal Melalui Pendekatan FamilyAgustina VivoNo ratings yet
- Soc - Sci - Med 1998 Barkre 1067 1076 PDFDocument10 pagesSoc - Sci - Med 1998 Barkre 1067 1076 PDFWaoNo ratings yet
- Maternal and Child Health Nursing 1Document20 pagesMaternal and Child Health Nursing 1Khibul Lim100% (1)
- Key Facts Menstrual CycleDocument8 pagesKey Facts Menstrual CycleMari FeNo ratings yet
- The Effect of Nursing Care Provided Based On The Philosophy of Hypnobirthing On Fear, Pain, Duration, Satisfaction and Cost of Labor: A Single - Blind Randomized Controlled StudyDocument14 pagesThe Effect of Nursing Care Provided Based On The Philosophy of Hypnobirthing On Fear, Pain, Duration, Satisfaction and Cost of Labor: A Single - Blind Randomized Controlled Studysgd bsepuluhNo ratings yet
- Jurnal Kebidanan: The Process of Uterine Involution With Postpartum Exercise of Maternal PostpartumDocument5 pagesJurnal Kebidanan: The Process of Uterine Involution With Postpartum Exercise of Maternal Postpartumakayuni mirachristinaNo ratings yet
- Misoprostol PDFDocument5 pagesMisoprostol PDFEduardNo ratings yet
- 2013 Chakraborty Outcome of Prelabor Rupture of MembranesDocument6 pages2013 Chakraborty Outcome of Prelabor Rupture of MembranesRayhan AlatasNo ratings yet
- HMS - Women's Health (MCQ & Notes)Document44 pagesHMS - Women's Health (MCQ & Notes)marouf elgoulNo ratings yet
- MCN Reviewer: Basic ConceptsDocument22 pagesMCN Reviewer: Basic ConceptsPanJan BalNo ratings yet
- Artikel Faktor-Faktor Yang Mempengaruhi Perdarahan Post Partum Di Rsia Sitti Khadijah 1 Tahun 2014-2019Document15 pagesArtikel Faktor-Faktor Yang Mempengaruhi Perdarahan Post Partum Di Rsia Sitti Khadijah 1 Tahun 2014-2019sri ayu lestari wulandariNo ratings yet
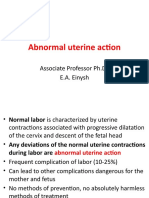
- Abnormal Uterine ActionDocument36 pagesAbnormal Uterine ActionMed PoxNo ratings yet
- Medical Management of Missed AbortionDocument4 pagesMedical Management of Missed AbortionJonathan San MartinNo ratings yet
- 1114 3914 1 PBDocument9 pages1114 3914 1 PBMaria Cresensia Akwin GuinoNo ratings yet
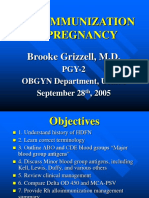
- Alloimmunization in Pregnancy: Brooke Grizzell, M.DDocument40 pagesAlloimmunization in Pregnancy: Brooke Grizzell, M.DhectorNo ratings yet
- Preterm Labor 2Document18 pagesPreterm Labor 2Олександра ЗагородняNo ratings yet
- SURROGACYDocument18 pagesSURROGACYGarima SinghNo ratings yet
- English Ii Assignment: Midwifery Management in Cephalopelvic DisproportionDocument14 pagesEnglish Ii Assignment: Midwifery Management in Cephalopelvic DisproportionBintari Ancinonyx JubatusNo ratings yet
- Surrogate MothersDocument3 pagesSurrogate MothersdyuthikNo ratings yet
- Progestogen - Only Contraceptives Bouquet of Choices: Norplant ImplanonDocument105 pagesProgestogen - Only Contraceptives Bouquet of Choices: Norplant ImplanonK.S. ReddyNo ratings yet
- Case Study #117Document4 pagesCase Study #117Cheska Paloma100% (1)
- SM A Review Full Report FINALDocument100 pagesSM A Review Full Report FINALsamylkNo ratings yet
- Statistics Related To Child Health.Document34 pagesStatistics Related To Child Health.charan pooniaNo ratings yet