Professional Documents
Culture Documents
Themed Week 7 - LIVER
Uploaded by
AinahMahaniCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Themed Week 7 - LIVER
Uploaded by
AinahMahaniCopyright:
Available Formats
THEMED WEEK 7: LIVER
Hepatitis inflammation of the liver
1.
2.
3.
Acute
<6 months, usually <3months
Ranges from mild self-limiting illness to fulminant liver failure
Chronic
Ongoing hepatitis > 6 months
Chronic hepatitis can cause fibrosis leading to cirrhosis
Liver enzymes in hepatitis
a. Usually ^ ALT/AST the transaminases indicate liver cell (hepatocellular) damage
Blood tests
1.
2.
3.
4.
Hepatitis serology:
Hep A IgM- acute infection, IgG past infection
One in red should be
Hep B sAg, eAg, sAb, cAb IgM and IgG, eAb, HBV DNA
done as initial tests in
HCV antibodies and RNA PCR
a patient with acute
Delta Ab and Delta RNA (only on a background of HBV)
hepatitis!!
HEV IgM and IgG, HEV RNA
Autoantibodies
Antinuclear antibody (ANA) and anti-smooth muscle antibody (ASMA) in autoimmune
hepatitis (AIH)
Anti-mitochondrial antibody (AMA) in Primary Biliary Cirrhosis (PBC)
Immunoglobulins
IgG autoimmune hepatitis
IgM PBC
IgA alcoholic liver disease
Iron and copper studies
Hemochromatosis: ferritin and transferrin saturation
Wilsons disease: LOW caeruloplasmin and urinary copper
THEMED WEEK 7: LIVER
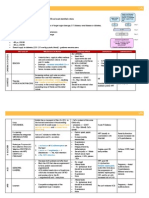
Virus
Hepatitis A
Hepatitis B
Hepatitis C
Hepatitis D
Type of virus
ssRNA
partially
dsDNA
ssRNA
Viral family
Hepatovirus;
related to
picornavirus
Hepadnavirus
Flaviridae
Route of
transmission
Fecal-oral
(contaminated
food or water)
Parenteral,
sexual
contact,
perinatal
Parenteral;
intranasal cocaine
use is a risk factor
Parenteral
Fecal-oral
incubation
period
24 weeks
14 months
78 weeks
Same as HBV
45 weeks
Never
PCR for HEV
RNA; detection
of serum IgM
and IgG
antibodies
Circular defective
ssRNA
Subviral particle
in Deltaviridae
family
Frequency of
chronic liver
disease
Never
10%
80%
5% (coinfection);
70% for
superinfection
Diagnosis
Detection of
serum IgM
antibodies
Detection of
HBsAg or
antibody to
HBcAg
PCR for HCV
RNA; 3rdgeneration ELISA
for antibody
detection
Detection of IgM
and IgG
antibodies; HDV
RNA serum;
HDAg in liver
Hepatitis E
ssRNA
Calicivirus
Case of HAV
40 year old University lecturer invited to give talk at International meeting in Bangladesh
Attended travel clinic a few months prior to trip; found to be HAV IgG negative so vaccination
recommended
5 weeks after returning felt unwell with:
anorexia, nausea, abdominal discomfort,
then she noticed:
dark urine, pale stools
jaundice
o/e: pyrexial, tender slightly enlarged liver
Investigations:
Bilirubin 80 iu/l (ULN=19),
Alkaline phosphatase, ALP (bile stasis) 200 iu/l (ULN=120)
Alanine transaminase, ALT (liver cell inf, inj, death) 2,430 iu/l (ULN=45)
International normalised ratio (INR) 1.8
HBsAg negative, HCV Ab negative, HAV IgM negative [but IgG positive following vaccination]
HEV IgM requested
Treatment:
No specific therapy is available. Avoid alcohol
Importance of good personal hygiene emphasised
Progress:
Repeat LFTs in 5 days:
Bil 55, ALT 1420, INR 1.3
Felt better in herself over next week and confirmed HEV IgM positive (can also request HEV
RNA)
Repeat LFTs in 6 weeks: Bil normal, ALT 90, INR 1.0
Summary:
Self-limiting infection, followed by recovery, but overall population mortality rates of 0.5%- 4%
rd
NB: mortality rate of 20% among pregnant women in 3 trimester
THEMED WEEK 7: LIVER
Hepatitis E
1.
2.
3.
4.
5.
6.
7.
8.
9.
HEV : 4 major genotypes genotypes 1 & 2 are restricted to humans and transmitted by
contaminated water in developing countries
Genotypes 3 & 4 infect humans, pigs and other mammalian species;
G3 is largely responsible for indigenous cases of HEV in Europe, N America & Australia
Acute hepatitis E increasingly seen in developed countries
Genotype 3, HEV is now the most common acute viral hepatitis in the UK
Zoonoses found in pigs - 85% of pigs affected
Undercooked meat implicated, can be transmitted by transfusion also
High mortality in patients with chronic liver disease
Please test for HEV in patients with acute hepatitis or decompensated cirrhosis
Hepatitis B
1.
Risk factors
a. Sexual - sex workers and homosexuals are particular at risk.
b. Parenteral - IVDA, Health Workers are at increased risk.
c. Perinatal - Mothers who are HBeAg positive are much more likely to transmit to their
offspring than those who are not. Perinatal transmission is the main means of transmission in
high prevalence populations.
Marker*
HBsAg
Anti-HBs antibody
HBeAg
Anti-HBe antibody
Interpretation
Exposure to Hepatitis B virus. Present in acute or chronic infection
Immunity acquired via natural infection or immunisation
Marker of infectivity. It correlates with high level of viral replication
It correlates with low level of viral replication
Anti-HBc IgM antibody
Infection in previous 6 months
Anti-HBc IgG antibody
Distant HBV infection or chronic HBV infection. Past or chronic HBV
Hep B DNA >105 copies /mL
2.
3.
4.
5.
6.
Rapid viral replication. Indicates active replication of virus, more accurate
than HBeAg especially in cases of escape mutants. Used mainly for
monitoring response to therapy.
Safe and effective vaccines against HBV have been available since 1982 over 1 billion doses have
been used world wide
HB vaccine is 95% effective in preventing chronic infections from developing
HB vaccine is the first vaccine against a major human cancer
Individuals with chronic HBV are at high risk of death from cirrhosis and liver cancer.
Surveillance for hepatocellular cancer is recommended in cirrhotics using 6 monthly ultrasound and
-fetoprotein
THEMED WEEK 7: LIVER
CASE OF HEB 1
28 year old attends GU clinic
Offered screening for sexually transmitted diseases
Found to be HBsAg postive
Subsequent tests show:
HBeAg positive, HBV DNA positive
LFTs normal except ALT of 96 iu/l
Abdo ultrasound scan - normal
Liver biopsy - moderate chronic hepatitis
CASE OF HEB 2
57 year old man presents with fatigue, RUQ discomfort and weight loss
Social history born in Hong Kong, came to UK 30 years ago, owns
Chinese restaurant
o/e; Palmar erythema, Firm palpable liver edge, Spleen palpable
Investigations:
Bil 19 iu/l, Alkaline phosphatase 115 iu/l,
ALT 72 iu/l, AST 80 iu/l, Albumin 32 iu/l (LOW).
Prothrombin time 2 seconds prolonged
HBsAg positive, HBeAb positive, HBV DNA positive
U/S scan liver has irregular margin and spleen is enlarged
consistent with portal hypertension
Management:
Undertake surveillance for
complications of cirrhosis
such as oesophageal varices
and hepatocellular cancer
Specific anti-viral therapy Lower viral load with agents
such as Lamivudine +
Tenofovir
Hepatitis C
1.
2.
3.
4.
5.
6.
Virology
12
a. Daily virion production >10 virions/day
b. RNA-dependent RNA polymerase
c. Frequent mutations and no proof reading
d. Results in HCV variants (quasispecies)
Six major types
Causes chronic liver disease and HCC
Transmission
a. Unsafe injection practice/contaminated needles
b. Blood or blood products (not since 1991 when screening was introduced)
c. Rarely by sexual exposure
d. Very rarely during medical care.
Indications for screening for HCV
a. Any hx of injecting or intranasal drug use
b. Blood transfusion or solid organ transplant before 1992(UK)
c. Blood product for clotting problem produced before 1987
d. Long term dialysis
e. Any elevation of ALT
f. HIV infection
Current treatment
Genotype 2-6
Pegylated interferon Alpha 2a (PEGASYS) + Ribavirin
Pegylated interferon Alpha 2b (Pegintron) 1.5 mcg/kg + Ribavirin
Genotype 1
Pegylated interferon Alpha 2a or 2b + ribavirin
THEMED WEEK 7: LIVER
7.
+/- protease inhibitor Telaprevir or Boceprevir
Progression
CASE OF HCV
28 year single man in drug rehab on
maintenance methadone 90mls/day.
First use of illegal drugs age 16 yrs, moved on to
injecting drug use aged 18 yrs
Offered screening for blood borne viruses in
prison when on remand for drug-related crime
Investigations:
HBsAg negative, HBcAb and HBsAb negative
HIV negative
HCV Ab positive
Management:
HB vaccine accelerated course
Advice on harm reduction measures
Check:
HCV RNA - positive,
HCV genotype 3
LFTs ALT 103
Refer for further assessment and treatment
Liver ultrasound scan - mild fatty/fibrotic
change
Declined liver biopsy keen to proceed to
treatment
Discussed all the side-effects of pegylated
interferon alpha and ribavirin
Completed 24 weeks combination therapy
despite developing depression (needed antidepressant), weight loss and anaemia (needed
dose reduction of Ribavirin)
HCV RNA 6 months later = negative (Sustained
Virological Response)
THEMED WEEK 7: LIVER
Introduction to autoimmune liver disease
1.
2.
3.
4.
It is a chronic inflammatory liver diseases
RARE (approx 5% of liver disease)
It is important because;
a. Involved YOUNG patients
b. Treatable
c. Symptoms
Mild liver disease -> CIRRHOSIS
Figure 1 Characteristic histological and radiological features of autoimmune liver diseases
THEMED WEEK 7: LIVER
Diagnosis and management of
Primary Biliary Cirrhosis (PBC) = AMA + ALP
1.
2.
3.
4.
Predominantly FEMALE 10:1
Middle aged women
Damage to small intrahepatic bile ducts
Genetic susceptibility + trigger (infectious, environmental toxins, hormones)
Symptoms
1.
2.
3.
4.
5.
6.
Asymptomatic (Incidental finding 7080%)
Fatigue
Itch
Dry eyes and dry mouth
Poor memory
Symptoms of advanced liver disease
Diagnostic criteria
1.
Abnormal LFTs (cholestatic - bile cannot
flow from the liver to the duodenum)
2. Positive Anti-mitochondrial Antibody
(AMA)
3. Compatible histology
4. 2 of above = probable PBC
5. 3 of above = definite PBC
6. Liver biopsy, usually not required unless:
a. Uncertain diagnosis
b. Possibility of overlap syndrome
Disease aetiology
Genetic associations allele association studies have shown IL12 regulation
and pathway, various other cytokines and the HLA region to be important
Association with Novosphingobium aromaticivorans first reported in 2003
and confirmed by others including in a mouse model
Associated with coeliac disease possibly via alteration of gut permeability
or immune regulation of exposure to gut luminal allergens
Treatment aim
Disease Progression
Ursodeoxycholic Acid (UDCA)
Hydrophilic bile acid
SE: weight gain, hair thinning and diarrhoea
Transplantation guided by Mayo score
Definitive treatment, only one that improves prognosis
10% of all transplants done for PBC up to 70 years old
Very good outcome normal survival in the 90% who survive the first year
Symptoms relieved
Itch Cholestyramine (Rifampicin Naltrexone, Sertraline)
Fatigue - No treatment with strong evidence some suggest modafinil but many side effects
Review contributing factors
Anaemia
Thyroid disease
Autonomic dysfunction
Obstructive sleep apnoea
THEMED WEEK 7: LIVER
Complications
Varices screen and treat primary prophylaxis with propanolol (s.e.=tiredness)
Osteoporosis oral high dose Vit D and calcium. Monitor Vit D (not absorbed in severe cholestasis)
so may need parenteral
Monitor for evidence of cirrhosis US and bloods
HCC annual USS and AFP
Case presentation
54 year old lady
Presents to GP with tiredness for many
years
Sleeps through the day
Always worn out
After a busy day it takes her several days to
recover
Itching which keeps her awake at night
Examination and Ix
PMHx
High cholesterol
Depression (diagnosed when originally
presented with tiredness)
Medication
Citalopram
Social history
Non smoker
Alcohol 5 units / week
Works as a teacher
Examination xanthelasma and scratch
marks on arms and legs
Bloods
U&Es normal
FBC normal
LFTs
Bilirubin
12
(0 - 21)
ALP
364
(30 - 130)
ALT
46
(0 40)
Albumin
42
(35 50)
TFTs normal
Autoantibodies
Anti-Nuclear Antibody Negative
Anti-Mitochondrial Ab Positive 1:640
Anti-smooth Muscle Antibody Negative
Immunoglobulins
IgA
1.4
(0.64 2.97)
IgG
12.5
(5.8 15.4)
IgM
5.42
(0.24 1.9)
Liver screen
Viral hepatitis Negative HBV sAG, HCV
antibodies
Ferritin Normal
Alpha-feto protein 3
Coeliac antibodies
NB we dont always check caeruloplasmin
and alpha-1 anti-trypsin
Abdo US - Normal
Autoimmune Hepatitis (AIH) - ANA / ASMA + raised IgG
1.
2.
3.
4.
5.
Immune attack on hepatocytes
Any age
Female : Male 3:1
Can be precipitated by drugs; imatinib
Genetic susceptibility (HLA associations) + trigger drug or infection - Brucella, tetracyclines, herpes 6
viruses, HCV, parvovirus, post-partum
THEMED WEEK 7: LIVER
Type 1
Type 2
75% cases
All ages
F:M 3:1
ANA / ASMA
<10% cases
Young adults
F: M 10:1
Commoner in Southern Europe
Anti-liver kidney microsomal-1 (LKM-1) antibodies or anti-liver
cytosolic antibodies (LC-1)
Presentation
Often asymptomatic (incidental finding)
Symptomatic
Fatigue, anorexia, nausea, joint pains
Acute hepatitis
Complications of cirrhosis
Investigations
Exclude drug, viral and metabolic causes
(full liver screen)
Combination of hepatitic LFTs,
autoantibodies and immunoglobulins
Usually need liver biopsy
Confirm diagnosis & stage
Treatment
Immunosuppression
Steroids
Azathioprine
MMF, Tacrolimus
Transplantation rarely unless cirrhotic at
presentation
Aim for normalisation of ALT and IgG or
BIOPSY
Duration of therapy uncertain. c.50% of
cases do not relapse when treatment
stopped at 2 years.
Case presentation
Examination
28 year old female
Presented to GP with several month history of:
Joint aches and pains
Anorexia and nausea
No medications
No risk factors for viral hepatitis
Strong FHx of A/I disease (coeliac disease, RA
and thyroid disease)
Not jaundice
Not encephalopathic
No stigmata of CLD
Bloods
Autoantibodies
FBC Normal
U&Es Normal
LFTS
Bilirubin 32 (0 30)
ALT
864 (0 40)
ALP
124 (30 130)
Albumin 40 (35 50)
Coagulation screen Normal
ANA
AMA
ASMA
1:320
Negative
1:160
Immunoglobulins
IgA 1.8
IgG
IgM 1.2
(0.64 2.97)
22.4
(5.8 15.4)
(0.24 1.9)
Viral hepatitis screen - Negative
Ferritin, caeruloplasmin and 1AT Negative
US - Normal
THEMED WEEK 7: LIVER
Primary Sclerosing Cholangitis (PSC) ANCA + ALP
Inflammation and fibrosis of intra and extra-hepatic bile ducts
Multifocal bile duct strictures
Small duct PSC clinical, biochemical and histological features of PSC but normal cholangiogram
60-80% patients with PSC have IBD
Presentation
Often asymptomatic
o Incidental finding of abnormal LFTs
Symptomatic
o Fatigue, itch, RUQ pain, weight loss
o Cholangitis (often not at presentation)
o Jaundice and complications of cirrhosis
Investigations
Bloods - Cholestasis
US often normal
CT often not helpful in diagnosis
Magnetic resonance cholangiopancreatography (MRCP) gold standard
o multi-focal, short, annular strictures alternating with normal or dilated segments beading
Liver biopsy
o Early stages often non-specific
o onion skin fibrosis (periductal concentric)
ERCP not usually used for diagnosis only if there is diagnostic doubt
Management
1.
2.
3.
4.
5.
6.
Look for IBD
Strictures
a. If dominant and causing symptoms (cholangitis, jaundice, pruritis, worsening LFTs) TREAT
i. ERCP (sphincterotomy, balloon dilatation, stent)
ii. Surgical (bypass of biliary stricture)
Itch (manage as for PBC)
Bone disease
Screen for malignancy
a. cholangiocarcinoma
b. colorectal
Transplantation
THEMED WEEK 7: LIVER
Case presentation
46 year old man
Incidental finding of abnormal LFTs
10 year history of Ulcerative Colitis
DHx - Mesalazine
Social Hx - No alcohol, Non smoker
Investigations
FBC Normal
U&Es Normal
LFTs
Bilirubin
ALP
ALT
Albumin
28
420
42
40
Autoantibodies
ANA, AMA, ASMA Negative
ANCA 1:360
Immunoglobulins - Normal
US Normal
MRCP
Multifocal strictures and segmental
dilatations
Involvement of intra and extra hepatic ducts
Beading
No mass lesion
(0 30)
(30 130)
(0 40)
(35 50)
Summary
PBC
Middle aged women
ALP + AMA + IgM
Symptoms of fatigue, itch,
dry eyes and dry mouth
Treat with UDCA
AIH
ALT + ANA + ASMA
Any age, any sex
Often asymptomatic
Treat with
immunosuppression
PSC
ALP + ANCA
Men
Associated with IBD
Screen for cholangiocarcinoma and
bowel cancer
AMA
ANA/ASMA
ANCA
PRIMARY BILIARY CIRRHOSIS
AUTOIMMUNE HEPATITIS
PSC
IGA
IGM
IGG
ALCOHOL, NAFLD
PRIMARY BILIARY CIRRHOSIS
AUTOIMMUNE HEPATITIS
THEMED WEEK 7: LIVER
Classification
1.
2.
Primary liver cancer
a. Cancers that originate in the liver
i. Hepatocellular carcinomas
ii. Cholangiocarcinomas
Secondary
a. Cancers that spread to the liver from an extra-hepatic primary site
b. Metastatic
Primary liver cancer
Epidemiology
More common in developing
country: higher incidence of
Hep B and C
1.
2.
3.
4.
th
5 most common malignancy worldwide
rd
3 most frequent cause of cancer mortality
Prevalent in areas of Asia and Africa
4x more common in men vs. women
Aetiology
90% of patients with hepatocellular carcinoma are (+) for HBV
HCC development is related to integration of viral HBV to the genome of the host
THEMED WEEK 7: LIVER
Risk factors
chronic, low grade liver cell damage and mitosis ->increased risk of HCC
alcoholic liver disease,
tyrosinemia,
alpha 1-anti trypsin deficiency,
primary biliary cirrhosis,
hemochromatosis,
cirrhosis
associated NASH
Clinical presentation
1.
2.
3.
4.
5.
6.
asymptomatic underlying cirrhosis
abdominal pain with a RUQ mass
a friction rub/bruit
Blood tinged ascites (20%)
jaundice
Small percentage may have a paraneoplastic syndrome
a. Erythrocytosis
b. Hypercalcemia
c. Diarrhea
Investigations
1.
FBC
a. Anemia, thrombocytopenia
2. Bleeding parameters
a. Prolonged PT/INR
3. Liver function test
a. Elevated liver enzymes
b. Increased bilirubin levels
4. Serum electrolytes
a. Hyponatremia (LOW Na+)
5. High AFP levels (>500 ug/L) seen in 70-80%
6. High AFP + adult with liver disease + no obvious GIT
tumor strongly suggest HCC
7. Correlation between history, PE, diagnostic
examinations
8. Tissue diagnosis is not required percutaneous liver biopsy of the tumour is discouraged 2 to
concern for seeding the biopsy track.
9. CT scan and MRI are preferred modalities for diagnosis of HCC
10. Ultrasound initial test if HCC is suspected
11. Hepatic artery angiography
THEMED WEEK 7: LIVER
THEMED WEEK 7: LIVER
Management
1.
2.
3.
4.
Surgical resection gold standard
a. generally offered to patients with liver-localized disease & adequate hepatic reserve for
recovery
b. Important to determine hepatic reserve
c. Cause of death after resection liver failure
Liver transplantation
a. offered to cirrhotic patients with no major cardiopulmonary comorbid conditions
b. local disease is limited
Thermal ablation
a. Killing small tumors via RF ablation
b. Can be used for:
i. Poor candidates for surgical resection
ii. Inaccessible tumors
iii. Large tumor burden
iv. Decreased hepatic reserve
Embolization
a. Targets the tumor by cutting of the blood supply
b. Ex: transarterial chemoembolization (TACE), transarterial embolization (TAE), and
radioembolization
c. Can be used to down stage a tumor or as a bridge for patients awaiting transplant
THEMED WEEK 7: LIVER
Secondary liver cancer
1.
2.
3.
4.
Most common tumor of the liver
20x more common than primary liver cancer
Most common primary tumors include the GIT, lung, breast
& melanomas.
Less common: thyroid, prostate, and skin
Pathogenesis
Vulnerable to invasion by tumor because of
Its size
high rate of blood flow
double perfusion by the hepatic artery and portal
vein
Next most common site of metastases after the lymph
nodes
Clinical presentation
Most patients with metastases present with symptoms referable to the primary tumor
Nonspecific symptoms of weakness, weight loss, fever, sweating, and loss of appetite
Investigation
Blood exams
increase in serum alkaline phosphatase is the most
common and frequently the only abnormality
Hypoalbuminemia, anemia, and mild elevation of
aminotransferase
Substantially elevated serum levels of CEA
Imaging
Ultrasound
CT scan
MRI
Treatment
For colonic carcinomas:
Out of 15% of patients with metastases limited to the liver, 20% are potentially resectable for
cure
Management is mostly palliative
Most respond poorly to all forms of treatment
Systemic chemotherapy may slow tumor growth and reduce symptoms, but it does not alter the
prognosis
Chemoembolization, intrahepatic chemotherapy, and alcohol or radiofrequency ablation may provide
palliation
THEMED WEEK 7: LIVER
ACUTE LIVER FAILURE
Liver failure occurring within 26 weeks of
onset of symptoms
Fulminant within 8 weeks
Hyperacute within 1 week
Prognosis: age (worse in very young and
very old), cause (worse in drugs and nonABCDE), acuteness (more acute the
better)
Potential mechanisms of interaction
and toxicity
Inadequate supply of the conjugate
Induction of one (toxic) pathway over a
safer route
Inhibition of the safer metabolic route
Competition at the enzyme with an
alternative substrate
What the liver does
Immune organ
Liver is central to immune function
function in clearing bacteraemia from gut,
opsonisation, kuppfer cells etc
Ergo, in acute (and chronic) liver failure
bacterial (80%) and fungal (30%)
infections are common and frequently
contribute to death
Role in refulation of vascular system
Mechanism not completely clear but
mainly mediated through nitrous oxide
Vasodilation (Systemic Iinflammatory
Response Syndrome)
Cerebral autoregulation
Hepatorenal syndrome
Control of metabolic status
In severe ALF, lactic acidosis occurs
(circulatory failure)
Before this metabolic alkalosis may occur
Abnormal water retention hyponatraemia, hypokalaemia, etc etc
Summary
Patients develop:
cerebral dysfunction then cerebral oedema
Coagulopathy
severe refractory hypoglycaemia
sepsis
renal failure and circulatory failure
electrolyte abnormalities
THEMED WEEK 7: LIVER
CASE 1
Presentation
Management
A 30 year old farmer is brought to A
and E by his family
They report that he has been acting
oddly for 3 months. He has stopped
eating and has been drinking alcohol
daily.
In the last 3 days they suspect he took
some tablets and he has become
confused and drowsy
BLOODS/PHYSIOLOGY
ALT 25,000 (0-40), Bilirubin 200 (0-21)
Prothrombin time 40 secs (n<14)
Creatinine 250
BP 85/50, pulse 120, warm peripheries
Bleeds when cannula inserted
Fulfils definition of hyperacute liver
failure coagulaopathy, cerebral
dysfunction with hepatic dysfunction
within 7 days of illness
ABC! fluids and lots
Airway management would be intubated in UK if
drowsy
Check blood glucose and prophylatically give 20%
glucose
Sepsis cultures, low threshold for broad spectrum
antibiotics
Replace glutathione with N-acetylcysteine (NAC)
Treatment
Supportive plus glutathione replacement NAC given
until PT improves.
Resus and support organ failure
Liver transplant if any of the following:
Persisting acidosis after fluids (pH<7.3)
PT>100 and creatinine >300
Grade 3 or 4 encephalopathy
Plus suitable EARLY TRANSFER
70-80% die if transplant criteria are fulfilled
With transplant, >50% survival
c.100-20 deaths a year in UK, 20 transplants
Many saved with NAC and supportive therapy
If they recover without transplant, liver returns to
normal
Death usually occurs on day 4 or 5 if it is going to
happen so transplant is very urgent.
Paracetamol metabolism
Therapeutic Dose
It is mostly converted to nontoxic metabolites
The sulfate and glucuronide pathways become
saturated, and more paracetamol is shunted to
sulfate and glucuronide, with a small portion
the CYP450 system to produce NAPQI.
As a result, hepatocellular supplies of
Cytochromes P450 2E1 and 3A4 convert
glutathione become depleted, as the demand
approximately 5% of paracetamol to a highly
for glutathione is higher than its regeneration.
reactive intermediary metabolite, N-acetyl-p
via Phase II metabolism by conjugation with
being oxidized via the CYP450 enzyme system.
Overdose
NAPQI therefore remains in its toxic form in the
benzoquinoneimine (NAPQI)
liver and reacts with cellular membrane
Under normal conditions, NAPQI is detoxified by
molecules, resulting in widespread hepatocyte
conjugation with glutathione to form cysteine
damage and death, leading to acute hepatic
and mercapturic acid conjugates.
necrosis especially in zone 3 of the liver
So, anything that increases the conjugation pathway via CYP450 induction is more likely to lead
to toxicity, especially if the possibility of detoxification by glutathione is reduced
So, (1) starvation/nutritional status, being (2) underweight and taking (3) enzyme inducers (alcohol
and phenytoin), make toxicity more likely.
ALF can occur at therapeutic doses in high risk individuals
THEMED WEEK 7: LIVER
CASE 2
55 year old woman presents to primary care
Unwell for 3 weeks with non-specific N and V,
lethargy, dark urine
GP notes abnormal LFTs ALT 800, bilirubin 30,
albumin 25, PT 16 secs.
Cause unclear checks a liver screen, watchful
waiting
2 weeks later, husband brings her to A and E
because she is confused
Drug and risk history only medication is
traditional medicine. Nothing else for >3/12
No risks for parenteral transmission
No FH. Does not drink, no PMH.
HBV/HCV/HAV and auto-antibodies negative
PT now 25, bilirubin 150
Does she have ALF? If so, is it severe?
ALF - yes cerebral disturbance with
coagulopathy within 8 weeks of onset
Severity criteria for transplant:
Prothrombin time > 100 seconds
OR
Three of the following:
Age < 10 yr or > 40 years
Cause: Hep C or E (or non-ABCDE)
Drug reaction
Jaundice > 7 days before onset of
encephelopathy
PT>50
Bilirubin >300
Currently transplant criteria not met
Supportive care
Likely induced by traditional medicine (many
examples)
Need close monitoring as may well continue to
deteriorate
THEMED WEEK 7: LIVER
CIRRHOSIS
Cirrhosis, as the end stage of chronic liver disease, is defined by
morphologic characteristics:
three main
a. Bridging fibrous septa
b. Diffuse disruption of the architecture of the entire liver.
c. Regenerative parenchymal nodules
Pathogenesis
1.
2.
3.
4.
5.
The central pathogenic processes in cirrhosis are
a. Death of hepatocytes,
b. Extracellular matrix (ECM) deposition, and
c. Vascular reorganization.
Excess of Types I and III collagen are deposited in the space of Disse, creating fibrotic septal tracts.
The vascular architecture of the liver is disrupted by the parenchymal damage and scarring, with the
formation of new vascular channels in the fibrotic septa.
Activated hepatic stellate cells, portal fibroblasts, and myofibroblasts of bone marrow origin have
been identified as major collagen-producing cells in the injured liver.
These cells are activated by fibrogenic cytokines such as TGF-1, angiotensin II, and leptin.
Clinical features
40% - cirrhosis are asymptomatic until late in the course of the disease.
THEMED WEEK 7: LIVER
Symptomatic - nonspecific C/F : anorexia, weight loss, weakness
Diagnosis
Clinical examination spider naevi, leuconychia, palmer erythema, gynaecomastia, Splenomegaly,
Testicular atrophy. Palmar contractures
Abnormal LFTs low albumin.
Ultrasound heterogeneous liver, enlarged spleen
Low white cells and platelets.
Signs of decompensation
Increasing jaundice
Increasing ascites
Abdominal pain
Abdominal distension
Breathlessness
Peripheral Oedema
Confusion flap
Internal bleeding
Complications of cirrhosis
1. Liver cell failure
a. Jaundice: Bilirubin 223 (<17)
b. Albumin 23g/l (>40)
c. Prothrombin time 23 secs (11-13)
2. Ascites
a.
b.
c.
d.
e.
Portal Hypertension
Abdominal distension with shifting dullness
Transudate albumin 9g/l
Ascitic WBC 140/l (<500); 98% mononuclear cells.
Prognosis 50% die within 2 years of onset
PARACENTESIS
14 litre paracentesis protein replacement with 7x 100ml 20% albumin
Spironolactone and furosemide prophylaxis
Speeds recovery
Shortens hospital admission
Total volume paracentesis safe with colloid replacement
Lowers variceal pressure gradient
Decreases variceal size
Refractory ascites: (prognosis)
o 50% die <6 months
o 75% die <1 year
THEMED WEEK 7: LIVER
3. Hepatorenal syndrome
a. May be precipitated by: (1) Over diuresis, (2) Infections
b. The syndrome is heralded by a drop in urine output and rising blood urea nitrogen and creatinine
values
c. If unresponsive to diuretic withdrawal and colloid infusion:
i. Almost universally fatal.
ii. Dialysis resistant but may respond to vasoconstriction with Terlipressin (counteract
splanchnic vasodilation)
4. Variceal bleeding
a.
b.
c.
d.
e.
Normal portal venous pressure <7mmHg.
Varices develop when portal pressure rises >10mmHg.
In portal hypertension collaterals develop Portal-Systemic Shunting
Many patients with Cirrhosis present with:
i. Haematemesis
ii. Malaena
iii. Anaemia
Gastroscopy shows
i. Oesophageal Varices
ii. Portal Gastropathy
Prediction of first variceal bleed
1.
2.
3.
Endoscopic findings:
a. Size of varices
b. Red wall markings (predict bleeding time)
Severity of liver disease
Intra variceal (portal) pressure
Haemodynamic Factors in Pathophysiology of Portal Hypertension
1.
2.
Increase in splanchnic (and systemic) blood flow
- splanchnic arteriolar vasodilatation
- Increased cardiac output
- Decrease splanchnic and systemic vascular resistance
- Treatment: Vasoconstrictor drugs eg. Vasopressin analogues, Beta-2-adrenoreceptors
Increase in intra hepatic resistance
- structural alteration
- active contraction of sinusoidal myofibroblasts
- Treatment: Vasodilatory drugs eg. nitrates, alpha blockers, Calcium channel blockers.
Emergency
1.
2.
3.
4.
Baloon tamponade
Vasoconstrictors: Vasopressin and Terlipressin
Somatostatin: decreases portal pressure and azygos blood flow
Emergency Sclerotherapy / Rubber Band Ligation
5. Encephalopathy
a. A spectrum of neuropsychiatric abnormalities observed in patients with hepatic dysfunction.
b. Vienna Classification 2002
i. Type A - Acute liver failure associated
THEMED WEEK 7: LIVER
ii. Type B - HE in patients with porto-systemic Bypass and no liver disease
iii. Type C - HE in chronic liver disease/ Cirrhosis
Treatment
1.
2.
3.
4.
5.
Treat precipitant infection, overdiuresis, bleeding
Maintain dietary protein intake / nutrition
Non absorbable disaccharide's
a. lactulose
b. lactitol
Non absorbable Antibiotics
a. Neomycin
b. Metronidazole
Hepatocellular of cirrhosis
6. Hepatocellular Carcinoma
a.
Most commonly seen in:
a. Hepatitis C after 30 years
b. Hepatitis B
c. Alcoholic Cirrhosis
d. Haemachromatosis
b. Screen for with ultrasound and alpha fetoprotein
THEMED WEEK 7: LIVER
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- A Diagnostic Approach To PruritusDocument8 pagesA Diagnostic Approach To PruritusSpica AdharaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Helicobacter Pylori InfectionDocument18 pagesHelicobacter Pylori InfectionPMNo ratings yet
- Gastroenterology - Internal Medicine, Dr. A. Mowafy (2020-2021)Document199 pagesGastroenterology - Internal Medicine, Dr. A. Mowafy (2020-2021)Mohammed Risq100% (1)
- Care of Patient With Liver Cirrhosis For Nursing Process Related Nursing CareDocument89 pagesCare of Patient With Liver Cirrhosis For Nursing Process Related Nursing CareMohamed Anwer Naleef100% (3)
- Liver PathologyDocument21 pagesLiver Pathologyzeroun24100% (6)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Liver - Dr. Allam 2021 PDFDocument70 pagesLiver - Dr. Allam 2021 PDFMohammedNo ratings yet
- Liver CirrhosisDocument83 pagesLiver CirrhosisRusiana NasilahNo ratings yet
- Git MRCGP 2015Document170 pagesGit MRCGP 2015AlexandraOsmanNo ratings yet
- Biopsy Interpretation of The Liver First Edition Michael TorbensonDocument540 pagesBiopsy Interpretation of The Liver First Edition Michael TorbensonByron Gonzalez UsmaNo ratings yet
- (Hepatology Research and Clinical Developments) Miranda L. Michelli-Liver Cirrhosis - Causes - Diagnosis and Treatment (Hepatology Research and Clinical Developments) - Nova Science Pub Inc (2011) PDFDocument303 pages(Hepatology Research and Clinical Developments) Miranda L. Michelli-Liver Cirrhosis - Causes - Diagnosis and Treatment (Hepatology Research and Clinical Developments) - Nova Science Pub Inc (2011) PDFnoname19191100% (2)
- Primary Biliary Cirrhosis Primary Sclerosing CholangitisDocument44 pagesPrimary Biliary Cirrhosis Primary Sclerosing CholangitisTK RowlingNo ratings yet
- Penilaian Bahan MUAYYIDDocument3 pagesPenilaian Bahan MUAYYIDAinahMahaniNo ratings yet
- Penilaian Bahan TamhidiDocument3 pagesPenilaian Bahan TamhidiAinahMahaniNo ratings yet
- All Clinical CasesDocument118 pagesAll Clinical CasesMichael AbioyeNo ratings yet
- Csim2.26 - Pituitary F (X)Document1 pageCsim2.26 - Pituitary F (X)AinahMahaniNo ratings yet
- CSIM2.90 - Occupational AsthmaDocument1 pageCSIM2.90 - Occupational AsthmaAinahMahaniNo ratings yet
- Urinary IncontinenceDocument1 pageUrinary IncontinenceAinahMahaniNo ratings yet
- CSIM2.26 - Pituitary FunctionDocument3 pagesCSIM2.26 - Pituitary FunctionAinahMahaniNo ratings yet
- Csim2.71 - The Patient With Proteinuria and HaematuriaDocument11 pagesCsim2.71 - The Patient With Proteinuria and HaematuriaAinahMahaniNo ratings yet
- Csim2.25 - Electrolyte ImbalanceDocument4 pagesCsim2.25 - Electrolyte ImbalanceAinahMahaniNo ratings yet
- Csim2.26 - Pituitary F (X) Unusual DiabetesDocument2 pagesCsim2.26 - Pituitary F (X) Unusual DiabetesAinahMahaniNo ratings yet
- Csim2.25 - Iron Metabolism & StorageDocument4 pagesCsim2.25 - Iron Metabolism & StorageAinahMahaniNo ratings yet
- Csim2.94 - Interstitial Lung DiseaseDocument3 pagesCsim2.94 - Interstitial Lung DiseaseAinahMahaniNo ratings yet
- Csim2.25 - Electrolyte Imbalance Calcium and BoneDocument7 pagesCsim2.25 - Electrolyte Imbalance Calcium and BoneAinahMahaniNo ratings yet
- CPTP - Pud + Altered Bowel HabitDocument3 pagesCPTP - Pud + Altered Bowel HabitAinahMahaniNo ratings yet
- Csim2.25 - Electrolyte Imbalance Iron Metabolism & StorageDocument1 pageCsim2.25 - Electrolyte Imbalance Iron Metabolism & StorageAinahMahaniNo ratings yet
- CSIM2.24 - Signal TransductionDocument6 pagesCSIM2.24 - Signal TransductionAinahMahaniNo ratings yet
- Csim2.92 - HypoventilationDocument1 pageCsim2.92 - HypoventilationAinahMahaniNo ratings yet
- CSIM2.91 - COPD and Pulmonary HypertensionDocument2 pagesCSIM2.91 - COPD and Pulmonary HypertensionAinahMahaniNo ratings yet
- CPTP - PainDocument3 pagesCPTP - PainAinahMahaniNo ratings yet
- CPTP - Pregnancy & LactatingDocument1 pageCPTP - Pregnancy & LactatingAinahMahaniNo ratings yet
- CPTP - Parkinson & MVMT DisordersDocument2 pagesCPTP - Parkinson & MVMT DisordersAinahMahaniNo ratings yet
- CPTP - Infection and Antibiotics 2Document3 pagesCPTP - Infection and Antibiotics 2AinahMahaniNo ratings yet
- CPTP - Poisonig MH Misuse of DrugsDocument5 pagesCPTP - Poisonig MH Misuse of DrugsAinahMahaniNo ratings yet
- Infection and AntibioticsDocument4 pagesInfection and AntibioticsAinahMahaniNo ratings yet
- CPTP - HPT & HFDocument4 pagesCPTP - HPT & HFAinahMahaniNo ratings yet
- CPTP - EpilepsyDocument4 pagesCPTP - EpilepsyAinahMahaniNo ratings yet
- CPTP - Diabetes and Lipid Lowering DrugsDocument4 pagesCPTP - Diabetes and Lipid Lowering DrugsAinahMahaniNo ratings yet
- CPTP - Asthma & CopdDocument5 pagesCPTP - Asthma & CopdAinahMahaniNo ratings yet
- Infection and AntibioticsDocument4 pagesInfection and AntibioticsAinahMahaniNo ratings yet
- CPTP - Af & Anti CoagulationDocument4 pagesCPTP - Af & Anti CoagulationAinahMahaniNo ratings yet
- Chung 2014Document6 pagesChung 2014Retno ManggalihNo ratings yet
- Atlas of Liver Pathology - Chapter 8 Biliary Tree DiseaseDocument45 pagesAtlas of Liver Pathology - Chapter 8 Biliary Tree DiseaseShabir HussainNo ratings yet
- Biliary AtresiaDocument25 pagesBiliary Atresiajulius billiNo ratings yet
- Pathology of LiverDocument15 pagesPathology of Liverערין גבאריןNo ratings yet
- Medical and Nutritional Management of Cholestasis in Infants and ChildrenDocument29 pagesMedical and Nutritional Management of Cholestasis in Infants and ChildrenYi Teng SohNo ratings yet
- LiverCirr 2011Document303 pagesLiverCirr 2011EnderNo ratings yet
- Autoimmune HepatitisDocument13 pagesAutoimmune HepatitisVita Delfi YantiNo ratings yet
- SopDocument13 pagesSopAnita OctaviaNo ratings yet
- Chronic Liver DiseaseDocument75 pagesChronic Liver DiseasebitspurNo ratings yet
- Moore Et Al-2018-Clinical Liver DiseaseDocument4 pagesMoore Et Al-2018-Clinical Liver DiseaseCarlos Francisco Enciso MartinezNo ratings yet
- Diseases of The Biliary Tract: Hepatic, Biliary Tract, and Pancreatic Dysfunction: Nursing ManagementDocument57 pagesDiseases of The Biliary Tract: Hepatic, Biliary Tract, and Pancreatic Dysfunction: Nursing ManagementMichael Baylon DueñasNo ratings yet
- Grading and Staging Systems for Liver DiseaseDocument10 pagesGrading and Staging Systems for Liver DiseasePD18No ratings yet
- Gastroentrology بالشرحDocument103 pagesGastroentrology بالشرحMahmoud AbouelsoudNo ratings yet
- Cholestatic Liver Disease & Jaundice: Dr. David Minter, D.ODocument79 pagesCholestatic Liver Disease & Jaundice: Dr. David Minter, D.ONabeel ShahzadNo ratings yet
- The Almost-Normal Liver Biopsy: Presentation, Clinical Associations, and OutcomeDocument7 pagesThe Almost-Normal Liver Biopsy: Presentation, Clinical Associations, and OutcomeAntonio RolonNo ratings yet
- Pathology Solved Papers 2015Document35 pagesPathology Solved Papers 2015Lakshmi Venkataraman100% (3)