Professional Documents
Culture Documents
Use of Vasopressors in Sepsis Resuscitation PDF
Uploaded by
Krittin NaravejsakulOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Use of Vasopressors in Sepsis Resuscitation PDF
Uploaded by
Krittin NaravejsakulCopyright:
Available Formats
29/08/56
The Sepsis Continuum
Use of Vasopressors in
Sepsis Resuscitation
:Guideline Update 2012
.
SIRS
Sepsis
Severe
Sepsis
Septic
Shock
A clinical response
arising from a
nonspecific insult,
with 2 of the
following:
T >38oC or <36oC
HR >90 beats/min
RR >20/min
WBC >12,000/mm3
or <4,000/mm3 or
>10% bands
Sepsis with Refractory
SIRS with a
organ failure hypotension
presumed
or confirmed
infectious
process
SIRS = systemic inflammatory
response syndrome
Chest 1992;101:1644.
Severe sepsis definition = sepsis-induced
tissue hypoperfusion or organ dysfunction
Septic shock ; a complex interaction
Crit Care Med 2013; 41:580637
-pathologic vasodilation
-relative and absolute hypovolemia
-myocardial dysfunction
-altered blood flow distribution
Rational to treat absolute hypovolemia
resulting from plasma extravasation with
aggressive fluid challenge
Sepsis initiates coagulation by activating endothelium to expression of TF
coagulation cascademicrovascular thrombi & obstruction distal
ischemia & tissue hypoxia
Systemic vasodilationmay be
primarily counteracted by early initiation
of vasopressor support
-clinical consequences of the changes in coagulation caused by sepsis are
levels of markers of DIC & widespread organ dysfunction
29/08/56
Sepsis-induced cardiac dysfunction
Early aggressive, goal-directed
therapy improves the outcome of
patients who have severe sepsis &
present to ER
Early identification of patients at
high risk for cardiovascular collapse
& Early therapeutic intervention to
restore a balance between oxygen
delivery & demand
Echocardiographic studies suggest that 40% to 50% of patients
with prolonged septic shock develop myocardial depression
Crit Care Med 2007; 35:15991608
N Engl J Med 2001;345:1368-77
N Engl J Med 2001;345:1368-77
N Engl J Med 2001;345:1368-77
Surviving Sepsis Campaign (SSC)
and the Institute for Healthcare
Improvement recommend
implementation of
6-hr resuscitation bundle
N Engl J Med 2001;345:1368-77
29/08/56
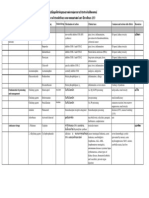
SURVIVING SEPSIS CAMPAIGN BUNDLES
Fluid Therapy
Crit Care Med 2013; 41:580637
Fluid challenge technique
Fluid Therapy of Severe Sepsis
Large amounts of fluids
Limited period of time
Close monitoring
PRO
CON
MAY BE
SHOULD BE
Patients response
Avoid pulmonary edema
Crit Care Med 2013; 41:580637
Will cardiac output increase
with fluid loading?
-
blood pressure
SvO2
heart rate
blood lactate
2mmHg
2mmHg
The change in CO. should be in the range of 300 ml/min
Current Opinion in Critical Care 2005, 11:264270
29/08/56
Vasopressors
The changes in aortic blood flow induced
by PLR are highly predictive of preload
responsiveness in ventilated patients, even
in the presence of spontaneous respiratory
efforts or arrhythmias
Crit Care Med 2006; 34:14021407
Vasopressor therapy initially to
target a mean arterial pressure
(MAP) of 65 mm Hg (grade 1C)
Norepinephrine as the first choice
vasopressor (grade 1B)
Effects of perfusion pressure on tissue
perfusion in septic shock
Crit Care Med 2000;28:27292732
Objective: To examine the effect of titrating
NE to different levels of MAP on systemic and
regional indices of perfusion
Patients: 10 pts. with the diagnosis of septic
shock who required pressor agents to maintain
a MAP 60 mm Hg after fluid resuscitation to
a PAOP 12 mm Hg
Interventions: NE was titrated to MAP of 65, 75,
and 85 mm Hg in 10 patients with septic shock
Surviving Sepsis Campaign: International guidelines for management of severe
sepsis and septic shock: 2012
Crit Care Med 2013; 41:580637
Conclusions: Increasing the MAP
from 65 mm Hg to 85 mm Hg with
NE does not significantly affect
- systemic oxygen metabolism
- skin microcirculatory blood flow
- urine output
- splanchnic perfusion
The aim of vasopressor therapy
is to improve tissue perfusion
pressure while avoiding
excessive vasoconstriction
Crit Care Med 2000;28:27292732
Adequate fluid resuscitation is
a fundamental aspect of
the hemodynamic management
of patients with septic shock
but using vasopressors early as
an emergency measure in patients
with severe shock is frequently
necessary
29/08/56
Adequate driving pressure & flow
>> sustain organ homeostasis
Norepinephrine Compared With Dopamine
in Severe Sepsis Summary of Evidence
Brain: Reversal of consciousness
Heart: Improvement of BP, PR
no signs of myocardial
ischemia
Kidney: Urine output > 0.5ml/kg/hr
Skin : warm, good skin perfusion
Reversal of lactic acidosis
Does my patient need an increase in CO. ??
Norepinephrine may be more effective at reversing hypotension
Dopamine may be particularly useful in patients with
compromised systolic function
Crit Care Med 2013; 41:580637
Safety about the administration of
low-dose dopamine ?
:Transient decrease in T-cell function
Dopamine was
associated with an
increased risk of death
(RR, 1.12; CI,1.011.20;
p =.035)
:Decreases growth-hormone
secretion negative nitrogen
balance in critical illness
:proarrhythmic effect
In the two trials that reported arrhythmias, these were more
frequent with dopamine than with norepinephrine
(RR, 2.34; CI, 1.46 3.77; p = .001)
Crit Care Med 2012; 40:725730
Crit Care Med 2006; 34:589597
Crit Care Med 2006; 34:589597
29/08/56
But no clinical study has
definitely indicated that
one catecholamine is
superior to another, so
that at present no agent
should be preferred
over the other
Epinephrine (added to and potentially
substituted for norepinephrine) when
an additional agent is needed to
maintain adequate blood pressure
(grade 2B)
Surviving Sepsis Campaign: International guidelines for management of severe
sepsis and septic shock: 2012
Crit Care Med 2013; 41:580637
to compare the efficacy and safety of
norepinephrine plus dobutamine (whenever
needed) with those of epinephrine alone in
septic shock
prospective,
double-blind
septic shock
participating
multicentre, randomised,
study was done in 330 pts with
admitted to one of 19
ICU in France
Lancet 2007; 370: 67684
Lancet 2007; 370: 67684
Lancet 2007; 370: 67684
There is no evidence for
a difference in efficacy and safety
between epinephrine alone &
norepinephrine plus dobutamine
for the management of septic shock
Should be the first alternative to norepinephrine!
Lancet 2007; 370: 67684
29/08/56
Prospective, double-blind, randomised
controlled trial
Setting: 4 Australian university-affiliated
multidisciplinary ICUs
280 patients were randomised to receive
either epinephrine or norepinephrine.
Kaplan-Meier estimates for probability of
achievement of MAP goal between epinephrine
and norepinephrine
Epinephrine was associated with the
development of significant but transient
metabolic effects that prompted the withdrawal of
18/139 (12.9%) patients from the study by
attending clinicians
Intensive Care Med (2008) 34:22262234
Vasopressin 0.03 units/minute can be added
to norepinephrine (NE) with intent of either
raising MAP or decreasing NE dosage (UG)
Low dose vasopressin is not recommended as the
single initial vasopressor for treatment of sepsisinduced hypotension and vasopressin doses higher
than 0.03-0.04 units/minute should be reserved for
salvage therapy (failure to achieve adequate MAP
with other vasopressor agents) (UG)
Intensive Care Med (2008) 34:22262234
Vasopressin is a direct vasoconstrictor
without inotropic or chronotropic effects
may result in CO and
hepatosplanchnic flow
most published reports exclude
patients from treatment with vasopressin
if the CI is < 2 or 2.5 L/min/m2, and it
should be used with caution in patients
with cardiac dysfunction
Surviving Sepsis Campaign: International guidelines for management of severe
sepsis and septic shock: 2012
Crit Care Med 2013; 41:580637
relative vasopressin deficiency in septic shock
infusion of low-dose vasopressin
(0.01 0.04 units/min yielding
plasma levels of 20100 pg/mL)
restores plasma levels to values
found during comparable
degrees of hypotension from
other origins (2030 pg/mL)
Crit Care Clin 22 (2006) 187 197
Crit Care Med 2007 Vol. 35, No. 9 (Suppl.)
29/08/56
RCT trial patients (who had septic shock and
were receiving a minimum of 5 g of NE/min) were
assigned to receive either low-dose vasopressin
(0.01- 0.03 U/min) or NE (5-15 g/min) in addition
to open-label vasopressors
The primary end point was the mortality rate 28 days after
the start of infusions
N Engl J Med 2008;358:877-87
Low-dose vasopressin did not reduce
mortality rates as compared with NE
among patients with septic shock who
were treated with catecholamine
vasopressors
N Engl J Med 2008;358:877-87
< 15 g/min NE
The effects of low-dose vasopressin
as a catecholamine-sparing drug,
not the effects in catecholamineunresponsive refractory shock
N Engl J Med 2008;358:877-87
Continuous infusion of
a relatively low dose of
TP (1.3 g/kg/h) was
effective in reversing
sepsis-induced
hypotension and in
reducing NE
requirements
45 septic shock patients with MAP < 65 mmHg were
randomized to receive continuous infusions of either
terlipressin (1.3 g/kg/h), vasopressin (0.03 U/min) or
norepinephrine (15 g/min; n = 15 per group)
In all groups, open-label norepinephrine was
added to achieve a mean arterial pressure
between 65 and 75 mmHg, if necessary
Critical Care 2009, 13:R130
Dopamine as an alternative vasopressor agent
to norepinephrine only in highly selected
patients (eg, patients with low risk of
tachyarrhythmias and absolute or relative
bradycardia) (grade 2C)
Critical Care 2009, 13:R130
Higher doses of vasopressin have been associated with cardiac,
digital, and splanchnic ischemia and should be reserved for
situations where alternative vasopressors have failed
Crit Care Med 2003; 31:13941398
Surviving Sepsis Campaign: International guidelines for management of severe
sepsis and septic shock: 2012
Crit Care Med 2013; 41:580637
29/08/56
Phenylephrine is not recommended in the treatment
of septic shock except in circumstances where
Low-dose dopaminenot be used for
renal protection(1A)
(a) Norepinephrine is associated with serious
arrhythmias
(b) Cardiac output is known to be high and blood
pressure persistently low
(c) As salvage therapy when combined
inotrope/vasopressor drugs and low dose
vasopressin have failed to achieve MAP target
(grade 1C)
All patients requiring vasopressors
have an arterial catheter placed as
soon as practical if resources are
available(UG)
Surviving Sepsis Campaign: International guidelines for management of severe
sepsis and septic shock: 2012
Crit Care Med 2013; 41:580637
Arterial catheter provides a more accurate
and reproducible measurement of arterial
pressure (also allows beat-to-beat analysis)
Surviving Sepsis Campaign: International guidelines for management of severe
sepsis and septic shock: 2012
Crit Care Med 2013; 41:580637
Inotropic Therapy
Anesthesiology 2005; 103:41928
Dobutamine infusion
administered in the presence
of myocardial dysfunction as
suggested by elevated cardiac
filling pressures and low C.O.
Dobutamine is the first-choice
inotrope for patients with measured or
suspected low CO in the presence of
adequate left ventricular filling
pressure & adequate MAP
If used in the presence of low BP,
it should be combined
with vasopressor therapy
Surviving Sepsis Campaign: International guidelines for management of severe
sepsis and septic shock: 2012
Crit Care Med 2013; 41:580637
29/08/56
Against the use of a strategy
to increase Cardiac Index to
predetermined supranormal levels
Surviving Sepsis Campaign: International guidelines for management of severe
sepsis and septic shock: 2012
Crit Care Med 2013; 41:580637
P values are for the comparison of mortality rates among the three groups
N Engl J Med 1995;333:1025-32
There are recognized limitations to
ventricular filling pressure estimates
as surrogates for fluid resuscitation
However, measurement of CVP is
currently the most readily obtainable
target for fluid resuscitation
There may be advantages to targeting
fluid resuscitation to flow and perhaps to
volumetric indices (and even to
microcirculation changes)
arterial pulse contour analysis allow stroke volume
variation (SVV) to be tracked continuously
MICROCIRCULATION
TAKE HOME
volunteer
sepsis
10
29/08/56
RECOMMENDATIONS FOR HEMODYNAMIC
SUPPORT OF SEPTIC PATIENTS
Vasopressors are indicated to
maintain MAP >65 mm Hg, both during
and following adequate fluid
resuscitation
Norepinephrine are the vasopressors
of choice in the treatment of septic
shock
Norepinephrine may be combined with
dobutamine when cardiac output is
being measured
Epinephrine, phenylephrine, &
vasopressin are not recommended as
first-line agents
Vasopressin may be considered for
salvage therapy
Low-dose dopamine is not
recommended for the purpose of renal
protection
Dobutamine is recommended as the
agent of choice to increase cardiac
output
Resuscitation
more earlymore effective
Monitor
in ICU & arterial cannulation
Clinical end points
MAP,HR, urine output, skin
perfusion, mental status, &
indexes of tissue perfusion
( blood lactate conc. & SvO2)
11
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Adam Goleman Emotionl Inteligence Non Violent ComunicationDocument655 pagesAdam Goleman Emotionl Inteligence Non Violent Comunicationtomy100% (2)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Medical Assistant Resume Sample - Notre Dame Sea GreenDocument1 pageMedical Assistant Resume Sample - Notre Dame Sea Greenmalik_saleem_akbarNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Common Ent Emergencies 24126Document64 pagesCommon Ent Emergencies 24126Krittin NaravejsakulNo ratings yet
- Dementia and NeuropsychiatryDocument133 pagesDementia and NeuropsychiatryKrittin Naravejsakul100% (1)
- 17 Principles PDFDocument1 page17 Principles PDFKing KarvoNo ratings yet
- Lipton Ice Tea Final Report1Document113 pagesLipton Ice Tea Final Report1Lochana Madushanka75% (4)
- Fundamentals of Nursing Questionnaire With Answer Key (Lippincott Manual of Nursing Practice)Document6 pagesFundamentals of Nursing Questionnaire With Answer Key (Lippincott Manual of Nursing Practice)YujenNo ratings yet
- PollutionDocument11 pagesPollutionModem BodbenNo ratings yet
- 160 - 3.HP and NSAID Negative Peptic PDFDocument12 pages160 - 3.HP and NSAID Negative Peptic PDFKrittin NaravejsakulNo ratings yet
- Definition of Terms2013Document80 pagesDefinition of Terms2013Krittin NaravejsakulNo ratings yet
- 160 2.hepatolithiasis PDFDocument19 pages160 2.hepatolithiasis PDFKrittin NaravejsakulNo ratings yet
- 160 2.hepatolithiasis PDFDocument19 pages160 2.hepatolithiasis PDFKrittin NaravejsakulNo ratings yet
- PE Spine2010Document38 pagesPE Spine2010Krittin NaravejsakulNo ratings yet
- 160 - 3.HP and NSAID Negative Peptic PDFDocument12 pages160 - 3.HP and NSAID Negative Peptic PDFKrittin NaravejsakulNo ratings yet
- 165 - 5.constipation in Patients With Spinal Cord InjuryDocument13 pages165 - 5.constipation in Patients With Spinal Cord InjuryKrittin NaravejsakulNo ratings yet
- 165 - 5.constipation in Patients With Spinal Cord InjuryDocument13 pages165 - 5.constipation in Patients With Spinal Cord InjuryKrittin NaravejsakulNo ratings yet
- 160 - 4.probiotics and Irritable Bowel PDFDocument15 pages160 - 4.probiotics and Irritable Bowel PDFKrittin NaravejsakulNo ratings yet
- 165 - 5.constipation in Patients With Spinal Cord InjuryDocument13 pages165 - 5.constipation in Patients With Spinal Cord InjuryKrittin NaravejsakulNo ratings yet
- 160 2.hepatolithiasis PDFDocument19 pages160 2.hepatolithiasis PDFKrittin NaravejsakulNo ratings yet
- Electrolytes in PediatricsDocument84 pagesElectrolytes in PediatricsKrittin NaravejsakulNo ratings yet
- 160 - 4.probiotics and Irritable Bowel PDFDocument15 pages160 - 4.probiotics and Irritable Bowel PDFKrittin NaravejsakulNo ratings yet
- 160 - 4.probiotics and Irritable Bowel PDFDocument15 pages160 - 4.probiotics and Irritable Bowel PDFKrittin NaravejsakulNo ratings yet
- 160 2.hepatolithiasis PDFDocument19 pages160 2.hepatolithiasis PDFKrittin NaravejsakulNo ratings yet
- Lecture Diarrhea and ConstipationDocument63 pagesLecture Diarrhea and ConstipationKrittin NaravejsakulNo ratings yet
- ReA SittichaiDocument22 pagesReA SittichaiKrittin NaravejsakulNo ratings yet
- °Âõπ∑Ÿ¡∫√‘‡«≥™Àõß∑Âõß °"√Æ‘‡§√"-Àåªí≠À"°Âõπ∑Ÿ¡∫√‘‡«≥™Àõß∑Âõß„Π‡¥Á° ·Π«∑"ß°"√´-°ª√-«-Μ‘·≈-Μ√«®√À"ß°"¬ ‡§√◊Ëõß¡◊Õ ◊∫§Âπ∑"ß√-ß '«‘∑¬"·≈-‡«™»" Μ√Å𑫇§≈'¬√Å Tumor Markers °"√¬◊Π¬-Π°"√«‘Π‘®©-¬¢-Èπ Ÿ¥∑Â"¬Document40 pages°Âõπ∑Ÿ¡∫√‘‡«≥™Àõß∑Âõß °"√Æ‘‡§√"-Àåªí≠À"°Âõπ∑Ÿ¡∫√‘‡«≥™Àõß∑Âõß„Π‡¥Á° ·Π«∑"ß°"√´-°ª√-«-Μ‘·≈-Μ√«®√À"ß°"¬ ‡§√◊Ëõß¡◊Õ ◊∫§Âπ∑"ß√-ß '«‘∑¬"·≈-‡«™»" Μ√Å𑫇§≈'¬√Å Tumor Markers °"√¬◊Π¬-Π°"√«‘Π‘®©-¬¢-Èπ Ÿ¥∑Â"¬priscillaNo ratings yet
- Drug List-53 STDDocument24 pagesDrug List-53 STDKrittin NaravejsakulNo ratings yet
- Pediatriccardiovascularproblemsinemergencysetting15 Feb 2011 110216224036 Phpapp02Document75 pagesPediatriccardiovascularproblemsinemergencysetting15 Feb 2011 110216224036 Phpapp02Krittin NaravejsakulNo ratings yet
- EYE EXAMSDocument42 pagesEYE EXAMSKrittin NaravejsakulNo ratings yet
- EYE EXAMSDocument42 pagesEYE EXAMSKrittin NaravejsakulNo ratings yet
- Ent Instruments 100503041754 Phpapp02Document59 pagesEnt Instruments 100503041754 Phpapp02Krittin NaravejsakulNo ratings yet
- 191-Pitfalls in Management of Bleeding Disorders-20111117163513Document81 pages191-Pitfalls in Management of Bleeding Disorders-20111117163513Krittin NaravejsakulNo ratings yet
- Anticoagulants in AcsDocument66 pagesAnticoagulants in AcsKrittin NaravejsakulNo ratings yet
- Immune Reconstitution Inflammatory Syndrome (IRIS) : V. LuviraDocument32 pagesImmune Reconstitution Inflammatory Syndrome (IRIS) : V. LuviraKrittin NaravejsakulNo ratings yet
- Osce Ecg 110401044906 Phpapp01Document28 pagesOsce Ecg 110401044906 Phpapp01Krittin NaravejsakulNo ratings yet
- Reign Over Me Movie ReviewDocument1 pageReign Over Me Movie ReviewJohn Bryan Jamison0% (1)
- Vasa Praevia RCOG GTGDocument13 pagesVasa Praevia RCOG GTGMariaBrincatNo ratings yet
- Moran Precis Authority EstrangementDocument4 pagesMoran Precis Authority EstrangementGabriel RosenNo ratings yet
- This Study Resource Was: Originality (Low)Document3 pagesThis Study Resource Was: Originality (Low)Mary MAy MatabangNo ratings yet
- Mishaps MCQDocument8 pagesMishaps MCQBesHo TwadroUsNo ratings yet
- System Analysis and DesignDocument11 pagesSystem Analysis and DesignDhana SeganNo ratings yet
- Special Release 3 - Women and Men in Western Visayas PDFDocument8 pagesSpecial Release 3 - Women and Men in Western Visayas PDFJing PanganibanNo ratings yet
- Construction Risk AssessmentDocument2 pagesConstruction Risk Assessmenttrader123No ratings yet
- Use Only: Factors Affecting Exclusive Breastfeeding Practices Among Working-Class Women in Osun State, NigeriaDocument7 pagesUse Only: Factors Affecting Exclusive Breastfeeding Practices Among Working-Class Women in Osun State, Nigeriahenri kaneNo ratings yet
- Daily Time Record Daily Time Record: Hazel Mae A. Monterde, RN Hazel Mae A. Monterde, RNDocument1 pageDaily Time Record Daily Time Record: Hazel Mae A. Monterde, RN Hazel Mae A. Monterde, RNTyler BertNo ratings yet
- NRSG 780 - Health Promotion and Population Health: Module 3: EpidemiologyDocument34 pagesNRSG 780 - Health Promotion and Population Health: Module 3: EpidemiologyjustdoyourNo ratings yet
- NSAT Mathematics and English Scores RelationshipDocument2 pagesNSAT Mathematics and English Scores RelationshipSoriano AnjelynNo ratings yet
- Study Questions Chapter 3: Health Risk BehavioursDocument3 pagesStudy Questions Chapter 3: Health Risk BehavioursZakariaNo ratings yet
- Continuous Pericapsular Nerve Group Block For Hip Surgery: A Case SeriesDocument17 pagesContinuous Pericapsular Nerve Group Block For Hip Surgery: A Case SeriesVivek Vishal SahNo ratings yet
- English 10 Q2 Summative TestDocument9 pagesEnglish 10 Q2 Summative Testchronickler75No ratings yet
- Projects in the Autonomous Region in Muslim MindanaoDocument4 pagesProjects in the Autonomous Region in Muslim MindanaoMark montebonNo ratings yet
- ASEAN TMHS GMP Training Chapter 10 Self Inspection FD 28 Nov 2016 1Document31 pagesASEAN TMHS GMP Training Chapter 10 Self Inspection FD 28 Nov 2016 1Bambang PriyambodoNo ratings yet
- Nursing PhilosophyDocument6 pagesNursing Philosophyapi-547791491No ratings yet
- Muscular SystemDocument13 pagesMuscular SystemAgfa LundangNo ratings yet
- Jasper ReportDocument49 pagesJasper ReportOkeh JasperNo ratings yet
- What Is Your Reflection About The Current ECQ? How Do People Behave and Communicate During This ECQ?Document3 pagesWhat Is Your Reflection About The Current ECQ? How Do People Behave and Communicate During This ECQ?Allijah Trish HernandezNo ratings yet
- Dermoid Cyst of Nasal Septum in An Adult Patient: 1. IntroductionDocument7 pagesDermoid Cyst of Nasal Septum in An Adult Patient: 1. IntroductionMANASA AswathNo ratings yet
- Operation & Service Manual: Model: 18-4208-0010 Four Bottle Nitrogen Cart With Booster and Manifold/RegulatorDocument49 pagesOperation & Service Manual: Model: 18-4208-0010 Four Bottle Nitrogen Cart With Booster and Manifold/Regulatorhb Corp100% (2)
- Comm 1500 ReflectionDocument2 pagesComm 1500 Reflectionapi-242372492No ratings yet