Professional Documents
Culture Documents
zREINDUCCION Con Topotecan Vinolrebina Tiotepa Dexa and Gemcitabine Steinherz, Leukemia-2003 PDF
Uploaded by
erickmattosOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
zREINDUCCION Con Topotecan Vinolrebina Tiotepa Dexa and Gemcitabine Steinherz, Leukemia-2003 PDF
Uploaded by
erickmattosCopyright:
Available Formats
Leukemia (2003) 17, 19671972
& 2003 Nature Publishing Group All rights reserved 0887-6924/03 $25.00
www.nature.com/leu
A new multidrug reinduction protocol with topotecan, vinorelbine, thiotepa,
dexamethasone, and gemcitabine for relapsed or refractory acute leukemia
EA Kolb1 and PG Steinherz1
1
Department of Pediatrics at Memorial Sloan-Kettering Cancer Center, New York, NY, USA
We report the results of a phase 2 nonrandomized single-arm
trial of a combination therapy for relapsed or refractory
leukemia. From January 1999 to June 2002, 28 patients with
multiple relapsed or refractory acute leukemia received a
combination of topotecan, vinorelbine, thiotepa, dexamethasone, and, for patients with an M3 marrow on day 7,
gemcitabine. A total of 14 patients had pre-B-ALL (acute
lymphoblastic leukemia), three had T-cell leukemia, nine acute
myeloblastic leukemia (AML), and two biphenotypic leukemia.
In all, 13 patients achieved a significant response (10 complete
responses and three partial responses). Among the responders, five had pre-B-ALL, two had T-cell leukemias, five had
AML, and one had biphenotypic leukemia. In total, 10 of these
patients subsequently underwent hematopoietic stem cell
transplantation, and four are alive without disease. One patient
died, while in remission, of complications resulting from an
episode of sepsis and pneumonia that occurred during
topotecan, vinorelbine, thiotepa, dexamethasone, and gemcitabine (TVTG) reinduction. Other toxicities included grade 4
neutropenia in all patients and transient grade 2 hepatotoxicity
in 10 patients (36%). In summary, we report that 47% of heavily
pretreated pediatric patients with multiply relapsed or refractory leukemia achieved a significant response after therapy on
the TVTG protocol. Further studies are warranted to evaluate
the role of the TVTG combination in the treatment of leukemia.
Leukemia (2003) 17, 19671972. doi:10.1038/sj.leu.2403097
Keywords: topotecan; thiotepa; vinorelbine; gemcitabine; leukemia
Introduction
Topotecan is a semisynthetic water-soluble inhibitor of topoisomerase I, and acts in the S-phase of the cell cycle.15 The
unique, cell-cycle-specific effect of topotecan suggests that its
antitumor activity may be schedule dependent. Accordingly,
results in murine xenograft models of human tumors demonstrate peak activity when the drug is given as a protracted
infusion.3 Using similar schedules, excellent antitumor activity
is observed in L1210 leukemia, an aggressive murine leukemia,6
and xenografts of human poor risk acute lymphoblastic
leukemia (ALL).7 Furthermore, recent clinical trials in adults813
and children14 demonstrate that continuous infusion topotecan has antileukemia activity.
Preclinical data suggest that the inhibition of topoisomerase I
by topotecan will render the cell more susceptible to DNAdamaging agents.15 The combination of topotecan, plus either
cyclophosphamide,16 idarubicin,17 etoposide,18 cisplatin,19 or
cytarabine9,11,16,18 exhibits antitumor activity in adult patients
with leukemia9,11,1618 and solid tumors.19 In hematologic
malignancies, thiotepa is an active antileukemic agent that is
successfully used in the cytoreduction regimens preceding
allogeneic stem cell transplantion (SCT).20,21 Additionally, the
Correspondence: E Anders Kolb, Department of Pediatrics, Memorial
Sloan-Kettering Cancer Center, P.O. Box, 1275 York Avenue, New
York, NY 10021, USA; Fax: 1 212 717 3239
Received 28 March 2003; revised 28 May 2003; accepted 24 June
2003
combination of thiotepa, topotecan, and carboplatin followed
by autologous SCT offers a favorable antitumor effect for
pediatric solid tumors.22
Vinorelbine is a semisynthetic Vinca rosea alkaloid.23,24 Early
in vitro data suggest that vinorelbine may have a role in the
treatment the acute leukemias, although it appears to be less
active in acute myeloblastic leukemia (AML) when compared to
acute lymphoblastic leukemia (ALL).23,25,26 In adult solid
tumors, vinorelbine has been used successfully in combination
with both gemcitabine and topotecan,27 but there are no clinical
data to define its role in the treatment of leukemias.
Gemcitabine is a novel deoxycytidine analog with activity in
hematogenous malignancies. The structure and metabolism of
gemcitabine resemble that of cytarabine.28,29 However, after
phosphorylation, gemcitabine achieves higher relative concentrations, and is retained longer than cytarabine.3031 In vitro
cytotoxicity data suggest that gemcitabine has significant activity
in acute leukemias.3234 Furthermore, in clinical studies, either
alone,3538 or in combination with other agents,39,40 gemcitabine has activity against human leukemias.
Glucocorticoids are a mainstay in the treatment of pediatric
lymphoid and myeloid leukemias. Dexamethasone may be
preferable to prednisone due to enhanced penetration into the
cerebral spinal fluid.41 Many hypothesize that saturation of the
glucocorticoid receptor over extended periods of time with high
doses of corticosteroids will optimize the antileukemic effect of
these agents. Results of a recent trial at the Dana-Farber Cancer
Institute support this hypothesis. They observed enhanced bone
marrow and peripheral blood blast response to 18 and 150 mg/
m2/day dexamethasone when compared to the standard 6 mg/
m2/day.42
We report results of an institutional phase 2 nonrandomized
single-arm reinduction protocol, incorporating a combination of
topotecan, vinorelbine, thiotepa, gemcitabine, and high-dose
dexamethasone, for patients with multiple relapsed or refractory
acute leukemias. While the chemotherapeutic agents employed
all share the dose-limiting toxicity of myelosuppression, they
differ in mechanism of action and metabolism. Furthermore,
these are agents not commonly used in current leukemia
protocols, and they therefore offer potentially novel mechanisms
of action, either alone or in combination, against otherwise
heavily pretreated leukemia cells. The TVTG (topotecan,
vinorelbine, thiotepa, dexamethasone, and gemcitabine) protocol is designed to induce disease remission that is of sufficient
duration to identify a matched unrelated stem cell donor, and to
permit hematopoietic stem cell transplantation in a recipient
free of infections and vital organ dysfunction.
Patients and methods
Patients with acute leukemias, who had disease recurrence
despite exhausting all conventional therapeutic options, and/or
were refractory to conventional therapeutic agents, were eligible
for treatment. Between January 1999 and June 2002, 28 patients
Re-induction therapy for refractory leukemia
EA Kolb and PG Steinherz
1968
were treated with a combination of topotecan, vinorelbine,
thiotepa, and dexamethasone, with or without gemcitabine
according to the Memorial Sloan-Kettering Cancer Center TVTG
protocol. All patients had relapsed and/or refractory leukemia,
and no patient had therapeutic options of greater curative
potential. The diagnosis of ALL or AML was made according to
the FAB classification. Confirmation of immunophenotype was
available prior to treatment. All patients had a normal serum
creatinine, liver transaminases less than five times normal, and a
total serum bilirubin less than 1.5 times normal.
According to institutional guidelines, written informed consent was obtained from all patients or their guardians before the
initiation of therapy. Institutional Review Board approval was
obtained for the analysis of the results.
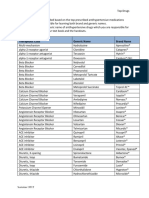
The specific schedule and dosages of the prescribed
chemotherapy is shown in Table 1. Gemcitabine was infused
on day 7 if the following criteria were met: there were greater
than 25% leukemic blasts in the day 7 bone marrow or a
persistence of circulating blasts in the peripheral blood; and
liver transaminases were less than five times normal, with a
bilirubin less than 1.5 times normal. Starting on day 7,
administration of daily subcutaneous granulocyte colonystimulating factor was initiated and continued until leukocyte
recovery. Additional courses of TVTG were offered to those
patients with a significant response to the first cycle, and
only when the absolute neutrophil count (ANC) exceeded
1000/ml and the platelet count exceeded 75,000/ml (Table 1). All
patients received either intrathecal methotrexate or cytarabine within 2 weeks of the start of each cycle of TVTG.
Subsequent intrathecal chemotherapy was administered at the
discretion of the investigator. One patient (patient 21) received
intrathecal methotrexate, cytarabine, and thiotepa on days 7,
14, and 21.
A complete response (CR) was defined as no measurable
extramedullary disease, and less than 5% blasts in the bone
marrow (M1 marrow) in a patient with an ANC greater than 500/
ml, and platelet count greater than 75 000/ml. Patients with a
partial response (PR) had 525% bone marrow blasts, with an
ANC greater than 500/ml, and platelet count greater than 75 000/
ml. It is not uncommon for heavily pretreated patients, especially
those with extensive bone marrow infiltration, to have a
significant response to therapy but have a delayed recovery of
platelet production. Therefore, patients who had an ANC greater
than 500/ml, a platelet count less than 75 000/ml, and 525%
leukemic blasts in the bone marrow were defined as having a PR
except platelets (PR-P). Patients who did not meet the above
response criteria were defined as unresponsive (n 15) and
were not offered additional courses of TVTG. Toxicities were
Table 1
graded according to the National Cancer Institute common
toxicity criteria, version II.
Results
Among the 28 patients enrolled (Table 2), 19 were male and
nine female. The mean age at the initial leukemia diagnosis was
8.1 years (range 3 months21 years), and the mean age at
enrollment was 10.8 years (124 years). A total of 14 patients
(50%) had Pre-B-cell ALL, three (11%) T-cell ALL, two (7%)
biphenotypic leukemia, and nine (32%) AML. Three of the nine
cases of AML were secondary to treatment for a previous
malignancy (t-AML). A total of 12 patients (43%) had disease
refractory to either first remission induction (n 3) or refractory
to remission reinduction after the first (n 6) or subsequent
relapse (n 3). The remaining 16 patients (57%) had a median
of two relapses (range 19) per patient, including five patients
who relapsed after myeloablative therapy and subsequent
allogeneic SCT (patients 4, 6, 10, 14, and 19). There were six
patients (21%) who received TVTG as the primary remission
reinduction therapy following a first relapse: patient 3 relapsed
while on a high-risk ALL protocol, patient 16 had relapsed AML
after only 6 weeks of remission, patients 18 and 19 experienced
an early relapse after primary refractory disease (refers to disease
that was refractory to standard initial remission induction
therapy, but ultimately these patients did achieve a first
remission with additional therapy), patient 22 had relapsed
t-AML, and patient 24 relapsed during consolidation therapy for
AML.
In all, 10 of the 28 patients (36%) achieved a CR, one patient
(4%) a PR, two (7%) a PR-P (Table 3), and 15 (53%) had no
response following the first cycle of TVTG. A total of 20 patients
(71%) had either an M3 marrow on day 7, or a persistence of
circulating blasts, and 15 subsequently received gemcitabine.
Three of these 15 patients achieved a CR (20%), one a PR (7%),
and one a PR-P (7%) after gemcitabine. Reasons to not give
gemcitabine in the remaining five patients included: hepatotoxicity (n 2), and a decision by the medical providers and
family that additional therapy would be futile due to rapid
progression of disease (n 3).
Four of the 14 patients (29%) with pre-B-ALL had a CR and
one a PR. Two of the three patients with T-cell leukemias had a
CR. Four of the nine patients (44%) with AML (including one
with t-AML) had a CR, and one a PR-P. One of the two patients
with biphenotypic leukemia had a PR-P (Table 3). Eight of the 13
patients with a response received more than one cycle of TVTG
(mean 3.6 cycles/patient, range 15 cycles).
TVTG treatment schedule
Dose
Topotecan
Vinorelbine
Thiotepa
Gemcitabine
Dexamethasone
G-CSF
a
Day
2
1 mg/m /day as a continuous i.v. infusion
20 mg/m2/day i.v. push
15 mg/m2/day i.v. over 4 h
10 mg/m2/min continuous i.v. infusion over 6 h. Total dose is 3600 mg/m2/dose
45 mg/m2/day P.O. or IV divided TID
5 mcg/kg/day SQ
15
0, 7, 14, 21b
2
7c
714
Start day 7 and continue until ANC 4500/ml
All patients had a central venous catheter with at least two lumens so the infusion of topotecan did not need to be interrupted for the administration
of other medications or blood products.
b
Day 21 vinorelbine is given only if the ANC is greater that 500/ml.
c
Administered if there are greater than 25% leukemic blasts in the bone marrow or a persistence of circulating blasts in the peripheral blood, and if
liver transaminases are less than five times normal, with a bilirubin less than 1.5 times normal.
Leukemia
Re-induction therapy for refractory leukemia
EA Kolb and PG Steinherz
1969
Table 2
Characteristics of patients treated with TVTG (n 28)
Pt. Diagnosis
Age (years) at
diagnosis/at TVTG
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
9/10
F
11/11
M
14/18
F
2/5
M
5/9
M
6/9
M
3/6
F
8/8
M
11/12
M
3/7
F
16/20
M
2/3
M
15/16
M
1/4
M
14/16
M
5 months/8 months F
23/23
M
4/5
F
2/3
F
17/18
M
8/13
M
20/22
F
3/8
M
14/17
F
2/3
M
4/6
F
21/22
M
6/8
F
T-cell ALL
Pre-B ALL
Pre-B ALL
Pre-B ALL
Pre-B ALL
Pre-B ALL
Pre-B ALL
Pre-B ALL
T-cell ALL
Bp
Pre-B ALL
AML
Pre-B ALL
Pre-B ALL
Bp
AML
t-AML
Pre-B ALL
AML
AML
T-cell ALL
t-AML
t-AML
AML
AML
Pre-B ALL
Pre-B ALL
Pre-B ALL
Sex Prior therapy
Disease status
at enrollment
V, P, As, Dn, Cp, Tg, Ac, HDM,
V, P, As, Dn, Cp, Ac, Mp, M
V, P, As, Dn, Cp, Ac, Mp, M, D, Dx, Tg
V, As, D, Cp, Ac, Mp, M, Tg, Dn, P, RT, TBI/Th/Cp SCT
V, Dx, As, D, Cp, Ac, Mp, M, Tg, HDM, VP, Flu, RT
V, Dx, As, D, Cp, P, Ac, Mp, M, Tg, Th, VP, HDM, RT, TBI/Cp SCT
V, Dx, As, D, Cp, Ac, Mp, M, Tg, P, Ida, RT
V, Dx, As, Mp, M, Ac
V, P, D, As, Mp, M, HDM
V, Dx, A, D, Cp, Ac, Mp, M, Tg, Dn, P, Ida, If, VP, HDM, TBI/Cp SCT
V, P, As, D, Cp, Ac, Mp, M, Tg, Dn, AD,
V, P, As, Dx, Ac, Tg, VP, Dn
V, P, As, Dn, Cp, Ac, Mp, M, Dx, Tg, VP, Th, CRT
V, P, As, D, Cp, Ac, Mp, M, Tg, Dn, Tm, Flu, TBI/Mel SCT
V, Dx, As, D, Cp, Ac, Mp, M, Tg, Dn, P, VP, If, Flu, RT
Dx, Ac, Tg, VP, Dn
Dx, Ac, Tg, VP, Dn
V, Dx, As, D, Cp, Ac, Mp, M, Tg, Dn, P
Dx, Ac, Tg, VP, Dn, As, Ida, Flu, V, P, Cp, M, TBI/Th/Cp SCT
Ac, Tg, Dn, VP, Mito, CSA, GO
V, Dx, As, D, Cp, Ac, Mp, M, Tg, Dn, P, If, VP, HDM
Dx, Ac, Tg, VP, Dn, Ac
Ac, As
Dx, Ac, Tg, VP, Dn, Ac, Cl, VP,
Ac, Tg, Dn, VP, Dx, As, Ida
V, P, As, Dn, Mp, M, VP, Cp, Ac, HDM,
V, P, As, Dn, Mp, M, Cp, Dx, Ep
V, P, As, M, Mp, D, Cp, Ac
11 ref
11 ref
1st rel
2nd rel
2nd rel
4th rel
3rd rel
2nd rel
1st rel, ref
2nd rel
2nd rel
1st rel, ref
2nd rel
3rd rel, ref
3rd rel, ref
1st rel
1st rel, ref
1st rel, after 1st ref disease
1st rel, after 1st ref disease
1st rel, ref
9th rel, ref
1st rel
11 ref
1st rel
1st rel, ref
2nd rel
1st rel, ref
3rd rel
Rel, relapse; ref, refactory; 11 ref, prime reference; Bp, biphenotypic leukemia; SCT, stem cell transplantation; Ac, cytarabine; AD, actinomycin D;
As, asparaginase; Cl, cladribine; Cp, cyclophosphamide; CSA, cyclosporin A; D, doxorubicin; Dn, daunorubicin; Dx, dexamethasone; Ep,
epirubicin; Flu, fludarabine; GO, gemtuzumab ozogamicin; HDM, high-dose methotrexate; Ida, idarubicin; If, ifosfamide; M, methotrexate; Mel,
melphalan; Mito, mitoxantrone; Mp, mercaptopurine; P, prednisone; RT, craniospinal radiation; TBI, total body irradiation; Tg, thioguanine; Th,
thiotepa; Tm, temozolomide; V, vincristine; VP, etoposide.
Table 3
Description of those patients who demonstrated a response
No.
Diagnosis
Response to
TVTG
1
2
3
4
7
11
12
15
20
21
22
23
24
T-cell ALL
Pre-B ALL
Pre-B ALL
Pre-B ALL
Pre-B ALL
Pre-B ALL
AML
Biphenotypic
AML
T-cell ALL
t-AML
t-AML
AML
CR
CR
CR
CR
CR
PR
CR
PR-P
CR
CR
CR
PR-P
CR
No. of
cycles
2
2
5
2
2
1
2
1
2
2
1
1
1
Gem
Yes
Yes
Yes
Yes
Yes
SCT After
TVTG
Current status
Yes
Yes
Yes
Yes
Yes
Yes
Yesb
No
Yes
Yesc
No
Yes
No
Alive
Alive
Died in remission of pneumonitis
DOD
Died of VOD, in remission
Died after graft failure
Alive
DOD
DOD
Alive
DOD
Died of disseminated Aspergillus
Died of complications
of sepsis that occurred 1 week after TVTG
Follow-up timea
(months)
32
10
13
3
3
5
9
4.5
13
50
6
17
1.6
t-AML, therapy related, or secondary AML; SCT, stem cell transplant; CR, complete response; PR, partial response; PR-P, partial response except
platelets; DOD, died of disease recurrence, VOD, veno-occlusive disease.
a
Follow-up time is measured from the start of the TVTG protocol.
b
The patient relapsed after the second cycle of TVTG. The patient subsequently achieved remission after therapy with another protocol and was
able to undergo an SCT.
c
Patient received intrathecal therapy with methotrexate, cytarabine, thiotepa, and hydrocortisone concomitantly with TVTG.
Eight of the 10 patients who achieved a CR, and two of the
three patients with a PR underwent an allogeneic hematopoietic
SCT after TVTG. The median time from achieving a CR to
transplant (n 7) was 3.9 months (range 1.510.9 months). Four
patients (patients 1, 2, 12, and 21) had a CR after TVTG,
underwent an allogeneic SCT, and are alive and disease free 8,
19, 30, and 49 months from the start of TVTG, respectively.
Patient 12 relapsed after the second cycle of TVTG. He again
achieved a remission with idarubicin and cytarabine, and is
currently alive and well after a mismatched SCT. Of the
Leukemia
Re-induction therapy for refractory leukemia
EA Kolb and PG Steinherz
1970
remaining six patients who were transplanted, two died with
relapsed disease, one viral pneumonitis, one veno-occlusive
disease, one disseminated aspergillus, and one of complications
associated with graft rejection (Table 3). All transplant-related
morbidities were within the range of that which is normally
expected in a heavily pretreated cohort of patients, and none
could be directly correlated with the prior administration of
TVTG.
Three patients were not transplanted after a response to TVTG
(patients 15, 22, and 24). Patient 24 had hematopoietic recovery
and confirmation of a CR, but the patient died of complications
of sepsis and ARDS that occurred during reinduction therapy.
This is the only TVTG-associated morbidity or mortality that
prevented SCT. After an initial PR-P on TVTG, patient 15 opted
to go off protocol and receive consolidation therapy with
fludarabine and cytarabine. No stem cell donor was identified,
and the patient died of relapsed disease 4.5 months from the
start of TVTG. Patient 22 refused additional chemotherapy after
a documented CR. This patient ultimately relapsed and died of
progressive disease.
The 13 patients who responded to therapy were evaluated for
hematopoietic recovery following TVTG. The median time to
achieve an ANC of 500/ml was 27 days (range 640 days), and
median time to achieve a platelet count of 75 000/ml (n 11)
was 30 days (range 048 days). The addition of gemcitabine
delayed the recovery of both the ANC and the platelet count
(Table 4). Transient grade 1 or 2 hepatic toxicity is documented
in 10 patients. Eight of these 10 patients received gemcitabine.
Three patients died within 1 month of starting therapy with
TVTG. All three patients had progressive disease on day 7, and
ultimately succumbed to disease and/or sepsis. One patient, as
mentioned above, developed sepsis and ARDS during cycle 1 of
chemotherapy of TVTG. This patient subsequently died 6 weeks
after initiation of TVTG, and was in remission at the time.
Discussion
Patients with multiply relapsed or refractory leukemia have a
dismal prognosis. Agents available for salvage therapy are
limited by: (1) the development of multidrug resistance in the
leukemia cells; and (2) the capacity for these heavily pretreated
patients to tolerate the side effects of additional high-dose
therapy. We present the results of 28 patients treated with a
protocol containing topotecan, vinorelbine, thiotepa, gemcitabine, and dexamethasone. A total of 13 of these patients (47%),
with multiply relapsed or refractory leukemia, achieved either a
CR (10 patients) or a PR (three patients) after one cycle of TVTG.
Additionally, 10 of the 13 patients subsequently underwent
Table 4
(n 13)a
Median hematopoietic recovery after one cycle of TVTG
Parameter
ANC greater than 500/ml
All patients (n 13)
No gemcitabine (n 8)
Gemcitabine (n 5)
27
23
32
Platelets greater than 75 000/ml
All patients (n 11)
No gemcitabine (n 7)
Gemcitabine (n 4)
30
29
32
Leukemia
Time (days)
Analysis includes only those patients with a CR, PR, or PR-P.
allogeneic SCT, and four of these are currently alive and diseasefree. It is interesting to note that remission reinduction with
TVTG was possible regardless of immunophenotype of the
leukemia cells (Table 3).
Recent clinical trials of topotecan as a single agent demonstrate that the drug has activity in relapsed leukemias.810,13,14
The maximum tolerated dose of topotecan in a heavily
pretreated cohort of pediatric patients with refractory leukemia
is reportedly 2.4 mg/m2/day for 9 days.14 However, the dose
employed in the multidrug protocols is necessarily lower and
some investigators have successfully used topotecan at a dose of
1.25 mg/m2/day in combination with other agents.11,17 In this
report, seven patients (25%) achieved a CR, and one a PR-P
when topotecan (1 mg/m2/day for 5 days) was used in
combination with vinorelbine, thiotepa, and dexamethasone
(ie without the addition of gemcitabine).
The role of gemcitabine in this combination of drugs is not
clear. In total, 15 patients had M3 marrow disease on day 7, and
received gemcitabine. Three subsequently achieved a CR, one a
PR and one a PR-P. Among the patients who received
gemcitabine, ANC recovery (see Table 3) was delayed 9 days
(32 days with gemcitabine, n 5 vs 23 days without gemcitabine, n 8), and the recovery of the platelet count was delayed
3 days (32 days with gemcitabine, n 4 and 29 days without,
n 7). However, only patients with refractory or progressive
disease received gemcitabine, and accordingly were expected
to have delayed or no recovery of hematopoiesis. Eight patients
experienced grade 2 hepatic toxicity following gemcitabine
infusion as compared to only two who did not receive
gemcitabine. Nonetheless, three CRs, one PR and one PR-P
among 15 patients with a slow response to reinduction are
encouraging. Careful consideration of acute toxicities is
necessary prior to the administration of gemcitabine.
The role of reinduction chemotherapy in multiply relapsed or
refractory patients is not an attempt at cure. Long-term remission
duration is unrealistic. Without an SCT, sooner or later these
patients will experience disease recurrence. The goal is to
administer therapy that will: (1) achieve a clinical response with
as little residual disease as possible; (2) maintain the response
long enough to identify a matched-unrelated stem cell donor;
and (3) permit the patient to undergo an SCT free of infections
and vital organ dysfunction. We were able to achieve this goal
in 47% of the patients. Unfortunately, one patient with a CR
died of complications resulting from ARDS that occurred during
induction. Additionally, two patients, with extensive disease at
the time of enrollment, experienced increased LFTs during the
first week of induction, and were subsequently unable to
potentially benefit from gemcitabine despite an M3 day 7
marrow.
In summary, we report a 47% response rate (36% CR, 11%
PR) in patients with multiple relapsed leukemia using a new
combination of chemotherapeutic agents. Toxicities primarily
include grade 4 neutropenia, which is difficult to assess in the
setting of a relapsed leukemia, and transient grade 2 hepatic
toxicity. Given the remission reinduction rate in this heavily
pretreated cohort of patients, these toxicities are acceptable.
Acknowledgements
This work would not be possible were it not for the help of many
colleagues. We are especially indebted to Maura Byrnes-Casey,
PNP, Rosemarie Corless, PNP, and Kateri Sullivan, PNP for their
skilled assistance with patient care; and Michael Kellick, RPh for
his assistance in designing and naming this protocol.
Re-induction therapy for refractory leukemia
EA Kolb and PG Steinherz
1971
References
1 Kingsbury WD, Boehm JC, Jakas DR, Holden KG, Hecht SM,
Gallagher G et al. Synthesis of water-soluble (aminoalkyl)camptothecin analogues: inhibition of topoisomerase I and
antitumor activity. J Med Chem 1991; 34: 98107.
2 Burris iii HA, Hanauske AR, Johnson RK, Marshall MH, Kuhn JG,
Hilsenbeck SG et al. Activity of topotecan, a new topoisomerase I
inhibitor, against human tumor colony-forming units in vitro. J Nat
Cancer Inst 1992; 84: 18161820.
3 Slichenmyer WJ, Rowinsky EK, Donehower RC, Kaufmann SH.
The current status of camptothecin analogues as antitumor agents.
J Natl Cancer Inst 1993; 85: 271291.
4 Creemers GJ, Lund B, Verweij. Topoisomerase I inhibitors:
topotecan and irinotecan. Cancer Treat Rev 1994; 20: 7396.
5 Potmesil M. Camptothecins: from bench to research hospital
wards. Cancer Res 1994; 54: 14311439.
6 Johnson RK, Hertzberg RP, Kingsbury WD, Boehm JC, Caranfa MJ,
Fausette LF et al. Preclinical profile of SK&F 104864, a watersoluble analogue of camptothecin. Proceedings of the Sixth NCIEORTC Symposium on New Drugs in Cancer Therapy 1991 Abstr.
301).
7 Uckun FM, Stewart CF, Reaman G, Chelstrom LM, Jin J, ChandanLanglie M et al. In vitro and in vivo activity of topotecan against
human B-lineage acute lymphoblastic leukemia cells. Blood 1995;
85: 28172828.
8 Kantarjian HM, Beran M, Ellis A, Zwelling L, OBrien S, Cazenave
L et al. Phase I study of topotecan, a new topoisomerase I inhibitor,
in patients with refractory or relapsed acute leukemia. Blood 1993;
81: 11461151.
9 Seiter K, Feldman EJ, Halicka HD, Traganos F, Darzynkiewicz Z,
Lake D et al. Phase I clinical and laboratory evaluation of
topotecan and cytarabine in patients with acute leukemia. J Clin
Oncol 1997; 15: 4451.
10 Gore SD, Rowinsky EK, Miller CB, Griffin C, Chen TL, Borowitz M
et al. A phase II window study of topotecan in untreated patients
with high risk adult lymphoblastic leukemia. Clin Cancer Res
1998; 4: 26772689.
11 Lee ST, Jang JH, Suh HC, Hahn JS, Ko YW, Min YH. Idarubicin,
cytarabine and topotecan in patients with refractory or relapsed
acute myelogenous leukemia and high-risk myelodysplastic
syndrome. Am J Hematol 2001; 68: 237245.
12 Mainwaring MG, Rimsza LM, Chen SF, Gomez SP, Weeks FW,
Reddy V et al. Treatment of refractory acute leukemia with timed
sequential chemotherapy using topotecan followed by etoposide.
Leuk Lymphoma 2002; 43: 989999.
13 Rowinsky EK, Kaufmann SH, Baker SD, Miller CB, Sartorius SE,
Bowling MK et al. A phase I and pharmacological study of
topotecan infused over 30 minutes for five days in patients with
refractory acute leukemia. Clin Cancer Res 1996; 2: 19211930.
14 Furman WL, Stewart CF, Kirstein M, Kepner JL, Bernstein ML, Kung
F et al. Protracted intermittent schedule of topotecan in children
with refractory acute leukemia: a Pediatric Oncology Group Study.
J Clin Oncol 2002; 20: 16171624.
15 Kaufmann SH, Peereboom D, Buckwalter CA, Svingen PA,
Grochow LB, Donehower RC et al. Cytotoxic effects of topotecan
combined with various anticancer agents in human cancer cell
lines. J Natl Cancer Inst 1996; 88: 734743.
16 Cortes J, Estey E, Beran M, OBrien S, Giles F, Koller C et al.
Cyclophosphamide, ara-C and topotecan (CAT) for patients
with refractory or relapsed leukemia. Leuk Lymphoma 2000; 36:
479484.
17 Pagano L, Mele L, Voso MT, Chiusolo P, Putzulu R, Mazzotta S
et al. The association of topotecan and cytarabine in the treatment
on secondary or relapsed acute myeloid leukemia. Haematologica
2001; 86: 440441.
18 Vey N, Kantarjian H, Beran M, OBrien S, Cortes J, Koller C et al.
Combination of topotecan with cytarabine or etoposide in patients
with refractory or relapsed acute myeloid leukemia: results of a
randomized phase I/II study. Invest New Drugs 1999; 17: 8995.
19 Lilenbaum RC, Miller AA, Batist G, Bernard S, Hollis DR, Rosner
GL et al. Phase I and pharmacologic study of continuous infusion
topotecan in combination with cisplatin in patients with advanced
cancer: a Cancer and Leukemia Group B study. J Clin Oncol 1998;
16: 33023309.
20 Aversa F, Pelicci PG, Terenzi A, Carotti A, Felicini R, Mencarelli A
et al. Results of T-depleted BMT in chronic myelogenous
leukaemia after conditioning regime that included thiotepa. Bone
Marrow Transplant 1991; 7 (Suppl. 2): 24.
21 Przepiorka D, Ippoliti C, Giralt S, van Beisen K, Mehra R,
Deisseroth AB et al. A phase III study of high-dose thiotepa,
busulfan, and cyclophosphamide as a preparative regime for
allogeneic marrow transplantation. Bone Marrow Transplant 1994;
14: 449453.
22 Kushner BH, Cheung NK, Kramer K, Dunkel IJ, Calleja E, Boulad F.
Topotecan combined with myeloablative doses of thiotepa and
carboplatin for neuroblastoma, brain tumors and other poor-risk
solid tumors in children and young adults. Bone Marrow
Transplant 2001; 28: 551556.
23 Toh HC, Sun L, Koh CH, Aw SE. Vinorelbine induces apoptosis
and caspase-3 (CPP3) expression in leukemia and lymphoma
cells: a comparison with vincristine. Leuk Lymphoma 1998; 31:
195208.
24 Landini I, Bartolozzi B, Banchelli I, Degli Innocenti A, Nocentini
O, Bernabei PA. In vitro activity of vinorelbine on human leukemia
cells. J Chemother 2001; 13: 309315.
25 Ashizawa T, Asada M, Kobayashi E, Okabe M, Gomi K, Hirata T.
Combination effect of navelbine (vinorelbine ditatrate) with
cisplatin against murine P288 leukemia and human lung carcinoma
xenografts in mice. Anticancer Drugs 1993; 4: 577583.
26 Bernabei PA, Landini I, Bartolozzi B, Banchelli I, Degli Innocenti o
Nocentini A, Santini V et a.l Activity of vinorelbine on B-chronic
lymphocytic leukemia cells in vitro. Adv Exp Med Biol 1999; 157:
473476.
27 Kelly K. New chemotherapeutic agents for small cell lung cancer.
Chest 2000; 117: 156S162S.
28 Lund B, Kristjansen PEG, Hansen H. Clinical and preclinical
activity of 20 20 -difluorodeoxycytidine (gemcitabine). Cancer Treat
Rev 1993; 19: 4555.
29 Plunkett W, Huang P, Searcy CE, Gandhi V. Gemcitabine
preclinical pharmacology and mechanism of action. Semin Oncol
1996; 23 (Suppl. 10): 315.
30 Bouffard DY, Momparler LF, Momparler RL. Comparison of
antineoplastic activity of 20 20 deoxycytidine and cytosine arabinoside against human myeloid and lymphoid leukemic cells. AntiCancer Drugs 1991; 2: 4955.
31 Plunkett W, Huang P, Xu YZ, Heinemann V, Grunewald R, Gandhi
V. Gemcitabine: metabolism, mechanism of action, and selfpotentiation. Semin Oncol 1995; 22 (Suppl. 11): 310.
32 Hertel LW, Boder GB, Kroin JS, Rinzel SM, Poore GA, Todd GC
et al. Evaluation of the antitumor activity of gemcitabine (20 2difluoro 20 -deoxycytidine). Cancer Res 1990; 50:
44174422.
33 Chow KU, Ries J, Weidmann E, Pourebrahim F, Napieralski S,
Stieler M et al. Induction of apoptosis using 20 ,20 difluorodeoxycytidine (gemcitabine) in combination with antimetabolites or
anthracyclines on malignant lymphatic and myeloid cells.
Antagonism of synergism depends on incubation schedule and
origin of neoplastic cells. Ann Hematol 2000; 79: 485492.
34 Lech-Maranda E, Korycka A, Robak T. Influence of gemcitabine
(20 20 -difluorodeoxycytidine) on growth of normal and leukemic
cells in vitro. Eur J Hematol 2000; 65: 317321.
35 Sallah S, Wan JY, Nguyen MP. Treatment of T-cell malignancies
using gemcitabine. Br J Hematol 2001; 113: 185187.
36 Steinherz PG, Seibel NL, Ames MM, Avramis VI, Krailo MD,
Liu-Mares W et al. Phase I study of gemcitabine (difluorodeoxycitidine) in children with relapsed or refractory leukemia (CCG0955): a report from the Childrens Cancer Group. Leuk
Lymphoma 2002; 43: 19451950.
37 Grunewald R, Kantarjian H, Du M, Faucher K, Tarassoff P, Plunkett
W. Gemcitabine in leukemia: a phase I clinical, plasma and
cellular pharmacology study. J Clin Oncol 1992; 10: 406413.
38 Gandhi V, Plunkett W, Du M, Ayres M, Estey EH. Prolonged
infusion of gemcitabine: clinical and pharmacodynamic studies
during a phase I trial in relapsed acute myelogenous leukemia.
J Clin Oncol 2002; 20: 665673.
39 Bass AJ, Gockerman JP, Hammett E, DeCastro CM, Adams DJ,
Rosner GL et al. Phase I evaluation of prolonged-infusion
gemcitabine with irinotecan for relapsed or refractory leukemia
or lymphoma. J Clin Oncol 2002; 20: 29953000.
Leukemia
Re-induction therapy for refractory leukemia
EA Kolb and PG Steinherz
1972
40 Rizzieri DA, Bass AJ, Rosner GL, Gockerman JP, DeCastro CM,
Petros WP et al. Phase I evaluation of prolonged-infusion
gemcitabine with mitoxantrone for relapsed or refractory acute
leukemia. J Clin Oncol 2002; 20: 674679.
41 Balis FM, Lester CM, Chrousos GP, Heideman RL, Poplack DG.
Differences in cerebrospinal fluid penetration of corticosteroids:
Leukemia
possible relationship to the prevention of meningeal leukemia.
J Clin Oncol 1987; 5: 202207.
42 Schwartz CL, Thompson EB, Gelber RD, Young ML, Chilton D,
Cohen HJ et al. Improved response with higher corticosteroid dose
in children with acute lymphoblastic leukemia. J Clin Oncol 2001;
19: 10401046.
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Ashton Manual English PDFDocument58 pagesAshton Manual English PDFMalissa Bowen100% (2)
- Adolescentes BFM HyperCVAD Alacacioglu2015Document5 pagesAdolescentes BFM HyperCVAD Alacacioglu2015erickmattosNo ratings yet
- BFM 2009 Colombia 0120-0011-Rfmun-64-03-00417Document9 pagesBFM 2009 Colombia 0120-0011-Rfmun-64-03-00417erickmattosNo ratings yet
- LMA BFM 2004 1-S2.0-S0006497119422519-MainDocument3 pagesLMA BFM 2004 1-S2.0-S0006497119422519-MainerickmattosNo ratings yet
- NIH Public Access: Author ManuscriptDocument15 pagesNIH Public Access: Author ManuscripterickmattosNo ratings yet
- Navy Heritage Video: General Military Training-Drug and Alcohol Abuse 1-2-1Document63 pagesNavy Heritage Video: General Military Training-Drug and Alcohol Abuse 1-2-1Kallepalli Somalingeswara RaoNo ratings yet
- Drug Scenario in The PhilippinesDocument15 pagesDrug Scenario in The PhilippinesCalix GonzalesNo ratings yet
- Pre-Filled Syringes 2014-2024 PDFDocument24 pagesPre-Filled Syringes 2014-2024 PDFVisiongainGlobal0% (1)
- Pharmaceutical Jurisprudence Sessional November 21 BP-505TDocument4 pagesPharmaceutical Jurisprudence Sessional November 21 BP-505TLloyd Institute of Management & Technology Pharm.No ratings yet
- TamsulosinDocument27 pagesTamsulosinAnna WidiaNo ratings yet
- Opioids For Acute Pancreatitis Pain (Review) : Basurto Ona X, Rigau Comas D, Urrútia GDocument49 pagesOpioids For Acute Pancreatitis Pain (Review) : Basurto Ona X, Rigau Comas D, Urrútia GYave Aro RodriguezNo ratings yet
- SYDocument54 pagesSYDimos MastroNo ratings yet
- Tapering BenzodiazepinesDocument3 pagesTapering BenzodiazepineslgiuzfgukuzfglufzNo ratings yet
- EvalGrants Letrozole Case Study Report FINALDocument66 pagesEvalGrants Letrozole Case Study Report FINALKanav GuptaNo ratings yet
- HPLC Calculation SpreadsheetDocument2 pagesHPLC Calculation SpreadsheetUmer Al-FaisalNo ratings yet
- Pharma Parenteral Dosage CalculationDocument3 pagesPharma Parenteral Dosage CalculationMaxinne RoseñoNo ratings yet
- Drugs 3Document43 pagesDrugs 3IonuțHerpeșNo ratings yet
- PCOL Maps PDFDocument11 pagesPCOL Maps PDFZinc YuloNo ratings yet
- Drugs in Ovulation InductionDocument8 pagesDrugs in Ovulation InductionJeevs Music100% (1)
- Bspha C1 Las 1Document41 pagesBspha C1 Las 1Muhammad Haroon RazaNo ratings yet
- SS II.1.1 Update On Typhoid Management - Dr. Adityo Susilo, SpPD-KPTI PDFDocument34 pagesSS II.1.1 Update On Typhoid Management - Dr. Adityo Susilo, SpPD-KPTI PDFWisnu Yudho HNo ratings yet
- PHARMACEUTICAL PLANT DESIGN ACCORDING TO CGMP GUIDELINESDocument12 pagesPHARMACEUTICAL PLANT DESIGN ACCORDING TO CGMP GUIDELINESRezwan Ahmed MahediNo ratings yet
- CLSI Pak-Antibiotic Sensitivity Panels Feb 2017-NasrullahDocument18 pagesCLSI Pak-Antibiotic Sensitivity Panels Feb 2017-NasrullahIhtisham Ul HaqNo ratings yet
- DrugsDocument155 pagesDrugsAkankshaNo ratings yet
- Accidental Epidural Injection of Atropine: Case ReportDocument2 pagesAccidental Epidural Injection of Atropine: Case ReportAida TantriNo ratings yet
- DIURETICSDocument40 pagesDIURETICSNiña Jean Tormis AldabaNo ratings yet
- Grandi 2019. Hormonal Contraception in Women With Endometriosis - A Systematic ReviewDocument11 pagesGrandi 2019. Hormonal Contraception in Women With Endometriosis - A Systematic ReviewcespersiNo ratings yet
- NPDS2011Document254 pagesNPDS2011A JWNo ratings yet
- Drug SheetDocument3 pagesDrug Sheetavause2No ratings yet
- Top Antihypertensive Drugs Generic-Brand Names PDFDocument1 pageTop Antihypertensive Drugs Generic-Brand Names PDFvidbala0% (1)
- Anticancer DrugDocument29 pagesAnticancer DrugAnjana PaudelNo ratings yet
- Final Drug StudyDocument4 pagesFinal Drug StudyBasema HashhashNo ratings yet
- Azithromycin (Zithromycin)Document2 pagesAzithromycin (Zithromycin)Adrianne Bazo100% (1)
- Part No Product Name Location Batch No Expired Date QTY OnhandDocument6 pagesPart No Product Name Location Batch No Expired Date QTY OnhandRatih SafrianiNo ratings yet