Professional Documents
Culture Documents
May-Issue 11
Uploaded by
Nephrology On-DemandOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
May-Issue 11
Uploaded by
Nephrology On-DemandCopyright:
Available Formats
Contributors: A Bansal (U of Pennsylvania) | P Dedhia (U of Cincinnati) | A Elebiary (Lahey Clinic) | X Vela (U of El Salvador) | D Thomson (ECU) | P Jawa (ECU) | S Sridharan
(Lister H ospital, UK)
F Iannuzsella (U of Parma, Italy) | D M itema (Johns H opkins U)
Courtesy: D. Divakaran | mostphotos.com/ 1987407/ human- kidney
ISSN 2372- 0824 (Print) | 2372- 0832 (Electronic)
Kidney
Konnection
Stay connected with Kidney Konnection through the N OD Plus App: http: / / goo.gl/ tfSAQT
Kidney Konnection is a monthly independent publication from N ephrology On- Demand
HEARTBROKEN WITH ACUTE
KIDNEY INJURY
by Amar Bansal (@amardbansal)
Cardiothoracic intensive care units (CT- ICU's) are a familiar setting
for nephrologists given the high rates of acute kidney injury (AKI)
after cardiac surgery. AKI can be a complication in up to 18% of
cardiac surgery patients (Thiele et al cJASN 2014). The associated
increase in healthcare costs and hospital length of stay can
substantially increase morbidity. AKI has implications not just on the
need for renal replacement therapy, but for overall mortality as well.
The sobering association between AKI after cardiac surgery is a
relevant consideration for all nephrologists that was recently
re- emphasized by a retrospective study in PLOS One.
In order to have generalizability across the literature, AKI
classification and staging systems have been developed. These systems
include RIFLE, AKI N etwork (AKIN ), and KDIGO. Although not
necessarily meant for routine clinical use, these systems allow more
uniform definitions of AKI for research purposes. These systems have
been embraced, not without criticism, by the nephrology and critical
care research communities. The study by M achado et al used the
KDIGO definition and staging criteria for AKI to evaluate the
mortality of AKI after cardiac surgery (see figure to your right). It was
a single- center, retrospective analysis of patients who underwent
CABG or cardiac valve surgery. The data show the 30- day mortality
of patients based on KDIGO classification. The 30- day mortality for
KDIGO stage 2 AKI was ~ 30%, while for KDIGO stage 3 AKI that
number rose to a staggering 55%!
There are key aspects of this study that deserve mention as far as
applicability to patients undergoing cardiac surgery in the US. First
off, this trial was conducted in a single center in Brazil. Thirty- three
percent of patients included had CKD stage 3 based on their
pre- operative baseline , and 3 percent had CKD stage 4. The median
BM I for patients in the trial (across all KDIGO stages) was about 26.
Based on my own anecdotal experience, I would guess that the BM I
of patients undergoing cardiac surgery in the US would be higher.
M edian age of all patients was about 60 and it?s possible that many
tertiary centers in the US operate on a slightly older population given
the higher prevalence of aortic valve disease with increasing age.
1
N onetheless, the study confirms many prior observations:
higher KDIGO stage was associated with increased 30- day
mortality, longer duration of mechanical ventilation, and
increased ICU stay. Interestingly, patients with KDIGO stage 3
AKI also had a substantially higher rate of needing repeat
surgery than all other patients in the study (see Table 1 in the
manuscript). The potential connections between AKI and a
higher incidence of repeat surgery warrants further study given
implications for inflammation, wound healing, and platelet
dysfunction.
These data demonstrate the vital need for a high level of
interdisciplinary care during the post- operative recovery of
these patients. Although not directly applicable to nephrology
practice, these high mortality rates warrant thoughtful and
honest informed consent for patients undergoing cardiac
surgery. The role of palliative care consultation for cardiac
surgery patients with AKI would likely be beneficial for
enhancing family- centered care given the poor outcomes
reported in these patients.
H ave a question for Dr. Bansal? Post it @
http: / / goo.gl/ 5feqvk or tweet him @amardbansal
Want a complimentary print subscription?
N ephrology On- Demand
Issue 11 | Volume 1 | 2015
Email myFellowship@ecu.edu for details
myFellowship@ecu.edu
https:/
/
www.scribd.com/
doc/
251289532/
M
ayIssue11
http: / / goo.gl/ tfSAQT
Editor: Tejas Desai | Chief: Cynthia Christiano
FIND M E...I'M LOST
This month's newest feature is a word find that focuses on renal failure in stem cell transplantation. Use the clues on
the right to find the appropriate answer. Answers can be in the traditional left- to- right layout, but also up- to- down,
down- to- up, right- to- left, and in any diagonal direction. Winners and answers will be available in a forthcoming
issue. Good luck...you're going to need it!!
Clues
1. The acronym for the condition that
occurs in up to 50% of stem cell
transplant recipients
2. This entity is indistinguishable from
hepatorenal syndrome and is a major
cause of renal failure in patients
undergoing myeloablative stem cell
transplantation
3. An antithrombotic and fibrinolytic
used in the management of
venoocclusive disease
4. The drug class of choice in the
treatment of thrombotic
microangiopathy
5. Chronic graft- versus- host disease is
associated with this nephrologic
syndrome
6. Severe forms of thrombotic
microangiopathy require this form of
therapy
7. The type of stem cell transplant
whereby the cells are from a donor
8. The type of stem cell transplant
whereby the cells are from a patient
LIT IN A M INUTE
Lit in a M inute is back and this month we celebrate by welcoming an old
friend back to the nephrology family. For years (perhaps even decades)
we've been taught that diabetic kidney disease patients with a serum
creatinine > 1.5 mg/ dl (1.4 if you're a women) should avoid metformin like
the plague. Largely an anecdotal warning, many believed that the risk of
lactic acidosis was unacceptably high if patients received metformin in the This is great news, because metformin remains a terrific drug
to treat diabetes. For years metformin has been banished
setting of moderate kidney disease.
from the nephrology world because of this fear. It's nice to
Thankfully, a new study in JAM A counters this fear with some evidence.
know that our kidney patients can, once again, avail
Investigators from Yale, UT Southwestern & Aston University (across the
themselves of this agent.
pond) looked at a large number of studies and did not find the rate of lactic
Welcome back to the family, metformin. N ot much has
acidosis to be any higher in renal failure patients taking metformin than
changed
while you were gone!
those w/ o kidney disease. Their new recommendation suggests that
Learn more @ JAM A. 2014;
metformin can be safely used in mild and moderate chronic kidney disease.
312(24): 2668
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Dr. Morse Top Videos (List - Natural Health & Healing)Document6 pagesDr. Morse Top Videos (List - Natural Health & Healing)mariyastoj100% (1)
- Medical Microbiology ReviewerDocument3 pagesMedical Microbiology ReviewerJoan BularioNo ratings yet
- Transplant Immuno - 2Document30 pagesTransplant Immuno - 2Nephrology On-DemandNo ratings yet
- 2017 #Nephmadness Tournament Selection ReportDocument24 pages2017 #Nephmadness Tournament Selection ReportNephrology On-Demand100% (1)
- Gender Gap PosterDocument1 pageGender Gap PosterNephrology On-DemandNo ratings yet
- October 2015Document2 pagesOctober 2015Nephrology On-DemandNo ratings yet
- Role of YouTube in The Same-Sex Referendums of North Carolina and WashingtonDocument1 pageRole of YouTube in The Same-Sex Referendums of North Carolina and WashingtonNephrology On-DemandNo ratings yet
- December 2015Document2 pagesDecember 2015Nephrology On-DemandNo ratings yet
- Enhancing Provider Education and Improving Healthcare Disparities in Chronic Myeloid Leukemia (CML) and Multiple Myeloma (MM) Through A Rural Regional North Carolina Hospital NetworkDocument1 pageEnhancing Provider Education and Improving Healthcare Disparities in Chronic Myeloid Leukemia (CML) and Multiple Myeloma (MM) Through A Rural Regional North Carolina Hospital NetworkNephrology On-DemandNo ratings yet
- August 2015Document2 pagesAugust 2015Nephrology On-DemandNo ratings yet
- Dialysis CalendarDocument1 pageDialysis CalendarNephrology On-DemandNo ratings yet
- Duty Hour Logs Through An AppDocument1 pageDuty Hour Logs Through An AppNephrology On-DemandNo ratings yet
- September 2015Document2 pagesSeptember 2015Nephrology On-DemandNo ratings yet
- February-Issue 8Document2 pagesFebruary-Issue 8Nephrology On-DemandNo ratings yet
- June-Issue 12Document2 pagesJune-Issue 12Nephrology On-DemandNo ratings yet
- July 2015Document2 pagesJuly 2015Nephrology On-DemandNo ratings yet
- April-Issue 10Document2 pagesApril-Issue 10Nephrology On-DemandNo ratings yet
- Outpt. Recommendation of Renal Transplant Patients.Document86 pagesOutpt. Recommendation of Renal Transplant Patients.Nephrology On-DemandNo ratings yet
- March-Issue 9Document2 pagesMarch-Issue 9Nephrology On-DemandNo ratings yet
- Seven - Jan. 2015Document2 pagesSeven - Jan. 2015Nephrology On-DemandNo ratings yet
- Liver TransplantDocument16 pagesLiver TransplantNephrology On-DemandNo ratings yet
- Pediatric Nephrology WorkforceDocument5 pagesPediatric Nephrology WorkforceNephrology On-DemandNo ratings yet
- Kidney BrochureDocument8 pagesKidney BrochureNephrology On-DemandNo ratings yet
- Medical Care 1st Year Post TransplantDocument18 pagesMedical Care 1st Year Post TransplantNephrology On-DemandNo ratings yet
- Recurrent GN After TXPDocument8 pagesRecurrent GN After TXPNephrology On-DemandNo ratings yet
- BK Virus - 1Document6 pagesBK Virus - 1Nephrology On-DemandNo ratings yet
- Infections in Solid Organ TransplantDocument14 pagesInfections in Solid Organ TransplantNephrology On-DemandNo ratings yet
- BK VirusDocument6 pagesBK VirusNephrology On-DemandNo ratings yet
- Transplant Immunology - 1Document16 pagesTransplant Immunology - 1Nephrology On-DemandNo ratings yet
- Cardio Vascular Complications After Kidney Trans.Document9 pagesCardio Vascular Complications After Kidney Trans.Nephrology On-DemandNo ratings yet
- Role of Mri in Evaluation of Suspected Spinal Dysraphism: Original ArticleDocument6 pagesRole of Mri in Evaluation of Suspected Spinal Dysraphism: Original ArticleBhayu RizallinoorNo ratings yet
- Etiological Potential of Immature Platelet Fraction in Children with ThrombocytopeniaDocument29 pagesEtiological Potential of Immature Platelet Fraction in Children with Thrombocytopeniajhanavi rajeshNo ratings yet
- The Pediatrics HO GuideDocument44 pagesThe Pediatrics HO GuideAlex MatthewNo ratings yet
- SP 16Document1 pageSP 16ray72roNo ratings yet
- Retdem 6 MarchDocument2 pagesRetdem 6 MarchCurtney PedriaNo ratings yet
- Patau Syndrome1Document5 pagesPatau Syndrome1api-346355246No ratings yet
- 5th Grade Unit 5 Health Practice Makes Perfect! 1 Worksheet 1 PDFDocument2 pages5th Grade Unit 5 Health Practice Makes Perfect! 1 Worksheet 1 PDFAmin ZakiNo ratings yet
- Respiratory Emergency First AidDocument13 pagesRespiratory Emergency First AidFaithNo ratings yet
- Thesis On Type 2 Diabetes MellitusDocument6 pagesThesis On Type 2 Diabetes Mellitusmoz1selajuk2100% (2)
- Team Aproach With Diabetes PatientsDocument5 pagesTeam Aproach With Diabetes PatientsLuis Vazquez MoralesNo ratings yet
- Origin and Treatment of Pigmentation DisordersDocument24 pagesOrigin and Treatment of Pigmentation DisordersAnita MarakNo ratings yet
- 525 FullDocument9 pages525 FulldianaNo ratings yet
- Manguiat, Ciara Loreal M. BSN 1-Y2-5 NCMA 111: Nursing Care PlanDocument3 pagesManguiat, Ciara Loreal M. BSN 1-Y2-5 NCMA 111: Nursing Care PlanCiara ManguiatNo ratings yet
- Latent Tuberculosis Infection (LTBI) : DR Wan Muhammad Farhan Bin Wan Fauzi Ukkp HKTDocument16 pagesLatent Tuberculosis Infection (LTBI) : DR Wan Muhammad Farhan Bin Wan Fauzi Ukkp HKTfarhan fauziNo ratings yet
- Peripheral Arterial DiseaseDocument38 pagesPeripheral Arterial DiseaseRessy HastoprajaNo ratings yet
- Mapeh QuizDocument6 pagesMapeh Quizdalia antolinNo ratings yet
- Types of Collagen and Associated Disorders: Osteogenesis ImperfectaDocument2 pagesTypes of Collagen and Associated Disorders: Osteogenesis ImperfectaAnjana J PrathapNo ratings yet
- Practical 2 - Health - Assessment - Prac - 2023Document5 pagesPractical 2 - Health - Assessment - Prac - 2023Sreya PNo ratings yet
- DR, DR Luh Made Mas Rusyati SPKK (K) Finsdv Dermatology and Venereology Department Medical Faculty Udayana University/ Sanglah HospitalDocument41 pagesDR, DR Luh Made Mas Rusyati SPKK (K) Finsdv Dermatology and Venereology Department Medical Faculty Udayana University/ Sanglah HospitalJohan CahyadirgaNo ratings yet
- Hospital Infection Control Manual AIIMS Raipur2019Document202 pagesHospital Infection Control Manual AIIMS Raipur2019Anjely SNo ratings yet
- Effective Herbal Remedy for Fever from Tamil NaduDocument1 pageEffective Herbal Remedy for Fever from Tamil Nadupadmaja84No ratings yet
- Pain ManagementDocument43 pagesPain ManagementThe AbyssinicansNo ratings yet
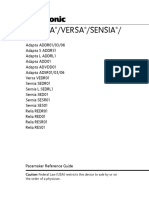
- Adapta Versa®sensiaDocument346 pagesAdapta Versa®sensiabobo samNo ratings yet
- Understanding Constipation and Faecal ImpactionDocument5 pagesUnderstanding Constipation and Faecal ImpactionKing GodwinNo ratings yet
- Risks & Benefits of Blood TransfusionDocument34 pagesRisks & Benefits of Blood TransfusionBryand KostaNo ratings yet
- Amavata KCDocument45 pagesAmavata KCBarsha Meher100% (1)
- End PointsDocument22 pagesEnd Pointsnikhil1802No ratings yet
- Systemic Sclerosis (Scleroderma)Document3 pagesSystemic Sclerosis (Scleroderma)AtiqahNo ratings yet