Professional Documents
Culture Documents
The Virtual Patient Specific-Model and The Virtual Dental Model10
Uploaded by
griffone1Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Virtual Patient Specific-Model and The Virtual Dental Model10
Uploaded by
griffone1Copyright:
Available Formats
The Virtual Patient Specific-Model and the
Virtual Dental Model
Vicente Hernndez-Soler, Reyes Enciso, and George J. Cisneros
The current trend in orthodontic records is toward an integrated virtual
3-dimensional (3D) model with soft tissue, hard tissue, and dentition. An
important part of this complete 3D record is the dental model. Cone beam
computed tomography allows the taking of all radiographic records and the
creation of virtual dental models out of a single scan. The virtual dental
models created out of cone beam computed tomography come with significant diagnostic additions, changing the way electronic casts are used.
(Semin Orthod 2011;17:46-48.) Crown Copyright 2011 Published by
Elsevier Inc. All rights reserved.
ince the early 1930s the classical orthodontic patient documentation consisted of a lateral head film, orthopantomogram, facial and
dental photographs, and plaster casts. Contemporary trends in imaging, such as cone beam
computed tomography (CBCT), allow a change
from datasets of records toward a so-called virtual patient-specific model (VPSM). The VPSM
is the integration of all datasets into a single
patient record.1
The VPSM via the use of CBCT provides 3-dimensional 1:1 accurate information, which can
be viewed as traditional CTs in a slice-by-slice
mode. This cross-sectional viewing capability
may improve orthodontic diagnosis and treatment planning. Coronal slices may better differentiate transverse problems, such as a skeletal
versus a dental cross-bite. Asymmetries can be
further classified into anterior-posterior and vertical and that could change treatment plans.
Problems, such as condylar hyperplasia or mid-
Associate Professor, Valencia University, Spain; Clinical Assistant Professor, Division of Endodontics, Oral Maxillofacial Surgery
and Orthodontics, School of Dentistry, University of Southern California, Los Angeles, CA; Professor, Department of Orthodontics,
College of Dentistry, New York University, New York, NY.
Address correspondence to Dr Vicente Hernndez-Soler, Deportista
Andres Muoz, Alicante 03003, Spain. E-mail: vicente@vicentehernandez.com
Crown Copyright 2011 Published by Elsevier Inc. All rights
reserved.
1073-8746/11/1701-0$30.00/0
doi:10.1053/j.sodo.2010.08.009
46
face asymmetry caused by maxillary canting, can
be quantified and assessed more accurately with
a 3D model.
An important part of the VPSM is the virtual
dental model (VDM). Compared with a plaster
model, the VDM has the all the advantages of a
digital format, which include, ease of access,
digital storage (which requires little physical
space), and ease of transfer to colleagues and
insurances or other offices, among others. The
VDM can be created by direct or indirect methods. Indirect methods, as the name implies, requires additional steps, such as impressions and
pouring of models in plaster, before its capture
into a digital format. The scanning of an impression or plaster cast can be done by a laser scanner, structured light, or even radiographic methods. Digital dental models created from dental
cast scans or dental impression scans have
proven to be as reliable as plasters models.2 For
the indirect methods, the transition from physical to digital records brings all the digital format
advantages but no significant additional diagnostic data. Plaster models may even offer more
diagnostic data because by holding the cast and
occluding both arches, the feel of the occlusion as stable or unstable can be assessed.
In the digital format, an attempt to replicate
such capability is represented as location and
shape of occlusal points and surfaces, but such
information may be more difficult to interpret
(Fig 1). Perhaps the major advantage of these
VDMs is the virtual setup capabilities, where ex-
Seminars in Orthodontics, Vol 17, No 1 (March), 2011: pp 46-48
Virtual Patient Specific-Model and the Virtual Dental Model
47
Figure 1. Occlusogram showing size and location of occlusal contacts between both arches. (Courtesy of
Geodigm Co, Chanhassen, MN.) (Color version of figure is available online.)
traction versus nonextraction treatment plans
can be compared, and the result visualized in a
faster and more practical way than having to use
laboratory saws and multiple dental impressions.
The direct methods for the creation of VDMs
are either the direct scan of the dentition with
an intraoral scanner using structured light, or
radiographic data, such as the CBCT. The VDM
derived from a CBCT, because the origin is radiographic data, includes not only the crowns
but also the roots of the teeth as well as any
unerupted or impacted teeth (Fig 2). The
CBCT-derived VDMs offers more than surfaceonly data because CBCT-derived VDMs allow for
3dimensional data and not only surface data.
The CBCT-derived VDM thus permits evaluation
of internal anatomy, which other methods do
not.
VDMs from CBCT have all the advantages of
the indirect method, with the additional diagnostic information of root position, root shape,
bone level, internal dental anatomy, relationship
to anatomic structures, such as the mandibular
nerve, as well as quantitative bone density information. Crown to root ratios can be estimated,
and tooth measurements can be performed even
before the teeth erupt. The virtual dental
setup now also includes the roots, which allow
for torque and labiolingual inclination in the
dental setup.
For VDMs derived from a CBCT, depending
on the scanner, the user has the choice of imaging the target area with different settings, such as
field of view, resolution (voxel size), milliamperage (mA), kilovoltage (kVp), among others. The
slice thickness from currently available scanners
ranges from 0.076 to 1 mm, depending on the
model and the manufacturer of the scanner.
Radiological machine settings used for scans
aimed at answering the same diagnostic question range from 1 to 15 mA. Scans made at
different imaging centers or offices for similar
problems, for example an impacted tooth, may
be exposed to different exposure levels depending on the brand of the scanner used. Altering
scanner parameters have a direct effect on image quality. It is essential to acquire high-quality
imaging data, because all other construction
steps depend upon these data. For higher image
quality, often greater radiation exposure is
48
Hernndez-Soler, Enciso, and Cisneros
Figure 2. Electronic model created from a CBCT
image. (Courtesy of Anatomage, Inc, San Jose, CA.)
needed. A balance between image quality and
radiation exposure is the operators responsibility. This balance means that the image should be
able to answer all required diagnostic questions,
taken with the lowest possible radiation exposure to the patient. This is referred to as the As
Low As Reasonably Achievable principle. Image
taking protocols need to be developed to
achieve the best possible balance between image
quality and radiation exposure.
Conventional lateral cephalograms are taken
with teeth in occlusion. If a CBCT is taken with
teeth in occlusion, the segmentation (separation) of maxillary and mandibular teeth becomes more difficult because the cusps of antagonist teeth would overlap. Teeth in occlusion
scans make it more difficult to build an accurate
dental model as they reduce the visibility of
teeth surfaces. Possible solutions include the use
of a thin wax-bite during scanning which may
facilitate the separation between the maxilla and
the mandible during the processing, causing little effect to the vertical dimension. If the image
is taken with the teeth in occlusion, occlusal
anatomy libraries, which match the tooth size,
can be used for more visually appealing toothlike images. The use of occlusal anatomy libraries is however more for esthetic value than
for diagnostic ability.
Dental restorations, such as amalgams or
crowns can create slight image artifacts in CBCT
images. Orthodontic appliances produce lesser
artifacts than dental restorations but also may
interfere with the views of dental occlusal anatomy. If true occlusal surface anatomy details are
necessary, the image may be supplemented with
an additional CBCT, or a hand-held oral scanning image.3 A composite or augmented model
with fusion data from different sources, because
they represent different time points, require
careful registration, verification, and validation.
The VPSM does not necessarily need to be a
static representation. The next development in
diagnostic data is the incorporation of motion to
the VPSM model. This motion can now be supplemented by dynamic records, such as jaw
tracking or video clips motions.1 To be consistent with medical image standards, and facilitate
interoperability, all images needs to be in a
DICOM format (ie, Digital Imaging and Communications in Medicine).
Conclusions
The present article describes how the virtual
dental model derived from CBCT not only incorporates all radiographic and dental cast information into a single scan, but also provides
significantly more information, adding internal
anatomy and the roots of the teeth into the
electronic dental model.
References
1. Enciso R, Memon A, Fidaleo DA, et al: The virtual cranio
facial patient: 3D jaw modeling and animation. Stud
Health Technol Inform 94:65-71, 2003
2. Dalstra M, Melsen B: From alginate impressions to virtual
digital models. J Orthod 36:36-41, 2009
3. http://www.cadentinc.com/. Accessed August 26, 2009
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CT00-000 814 36 01 02 PDFDocument246 pagesCT00-000 814 36 01 02 PDFw.h.nNo ratings yet
- Chapter 1 - Perspective DrawingDocument23 pagesChapter 1 - Perspective DrawingryanNo ratings yet
- 3D-Scanning With Structured LightDocument12 pages3D-Scanning With Structured LightDarkjak1502No ratings yet
- Robert Mealing - Hunting The True MarseilleDocument6 pagesRobert Mealing - Hunting The True MarseilleKanneryBoschNo ratings yet
- Grade 7 Art: Unit Plan: Color & Painting TechniquesDocument40 pagesGrade 7 Art: Unit Plan: Color & Painting Techniquesapi-299881434No ratings yet
- Louise Nevelson AssemblagesDocument6 pagesLouise Nevelson AssemblagesmerrufNo ratings yet
- Becuri MicroscopDocument44 pagesBecuri MicroscopsambadeeNo ratings yet
- Botanical Art and Illustration Certificate Program, Winter/Spring 2012 CatalogDocument20 pagesBotanical Art and Illustration Certificate Program, Winter/Spring 2012 CatalogMervi Hjelmroos-KoskiNo ratings yet
- 8IAOAM Program BookDocument42 pages8IAOAM Program Bookgriffone1No ratings yet
- Informed Consent and Contributory Negligence: Litigation, Legislation, and EthicsDocument3 pagesInformed Consent and Contributory Negligence: Litigation, Legislation, and Ethicsgriffone1No ratings yet
- Spiros Zinelis, William A. Brantley Auth., Theodore Eliades Eds. Research Methods in Orthodontics A Guide To Understanding Orthodontic ResearchDocument224 pagesSpiros Zinelis, William A. Brantley Auth., Theodore Eliades Eds. Research Methods in Orthodontics A Guide To Understanding Orthodontic Researchgriffone1No ratings yet
- Spiros Zinelis, William A. Brantley Auth., Theodore Eliades Eds. Research Methods in Orthodontics A Guide To Understanding Orthodontic ResearchDocument224 pagesSpiros Zinelis, William A. Brantley Auth., Theodore Eliades Eds. Research Methods in Orthodontics A Guide To Understanding Orthodontic Researchgriffone1No ratings yet
- For More Books, Periodicals and Etc. About Orthodontics, ClickDocument1 pageFor More Books, Periodicals and Etc. About Orthodontics, Clickgriffone1No ratings yet
- Erratum: Seminars in Orthodontics, Vol 17, No 1 (March), 2011: P 88Document1 pageErratum: Seminars in Orthodontics, Vol 17, No 1 (March), 2011: P 88griffone1No ratings yet
- A Few Comments On An Elegant Answer in Search of Useful Questions05Document2 pagesA Few Comments On An Elegant Answer in Search of Useful Questions05griffone1No ratings yet
- Cone Beam Computed Tomography For OrthodontistsDocument2 pagesCone Beam Computed Tomography For Orthodontistsgriffone1No ratings yet
- Seminars in Orthodontics: VOL 17, NO 1 MARCH 2011Document2 pagesSeminars in Orthodontics: VOL 17, NO 1 MARCH 2011griffone1No ratings yet
- Treatment of Class IiiDocument1 pageTreatment of Class Iiigriffone1No ratings yet
- Bonding and Debonding From Metal To Ceramic: Research and Its Clinical ApplicationDocument13 pagesBonding and Debonding From Metal To Ceramic: Research and Its Clinical Applicationgriffone1No ratings yet
- Seminars in Orthodontics: VOL 16, NO 3 September 2010Document2 pagesSeminars in Orthodontics: VOL 16, NO 3 September 2010griffone1No ratings yet
- Risk Indicators and Interceptive Treatment Alternatives For Palatally Displaced Canines2010 - 16 - 3 - 186 - 192Document7 pagesRisk Indicators and Interceptive Treatment Alternatives For Palatally Displaced Canines2010 - 16 - 3 - 186 - 192griffone1No ratings yet
- E Vidence-Based ResearchDocument1 pageE Vidence-Based Researchgriffone1No ratings yet
- Influence of Various Storage Media On Shear Bond Strength and Enamel Fracture When Debonding Ceramic Brackets: An in Vitro Study010 - 16 - 1 - 49 - 54Document6 pagesInfluence of Various Storage Media On Shear Bond Strength and Enamel Fracture When Debonding Ceramic Brackets: An in Vitro Study010 - 16 - 1 - 49 - 54griffone1No ratings yet
- Autonomous Land Vehicle in A Neural NetworkDocument13 pagesAutonomous Land Vehicle in A Neural Networkjosephkumar58No ratings yet
- Whats New in Inventor 2017Document46 pagesWhats New in Inventor 2017KarisoNo ratings yet
- Hinduism Today April May June 2015Document43 pagesHinduism Today April May June 2015jpmahadevNo ratings yet
- Tutorial 2 Solutions ECE 318Document3 pagesTutorial 2 Solutions ECE 318Tomas SmithNo ratings yet
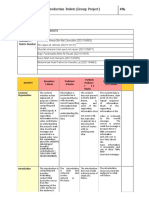
- GP3 WEBSITE Group Production Rubric (Group Project)Document3 pagesGP3 WEBSITE Group Production Rubric (Group Project)Aedil FahmiNo ratings yet
- 16-Division 2-Section 02700 CCTV Condition Survey-Version 2.Document16 pages16-Division 2-Section 02700 CCTV Condition Survey-Version 2.Avaan IvaanNo ratings yet
- TemDocument100 pagesTemviollabestariayu sabrinaputriNo ratings yet
- A Group of Tourists Wants To Learn About The Parks or Wildlife Reserves in Your AreaDocument3 pagesA Group of Tourists Wants To Learn About The Parks or Wildlife Reserves in Your Arearizki syahrifaNo ratings yet
- Nelapattu Bird SanctuaryDocument2 pagesNelapattu Bird SanctuaryPrithvi Chowdary YeddanapalliNo ratings yet
- XDL 210-240Document4 pagesXDL 210-240smallik3No ratings yet
- MIL REVIEWER For 2nd Quarter ExamDocument2 pagesMIL REVIEWER For 2nd Quarter ExamClarice Jenn MaltoNo ratings yet
- The Sweetheart ExcerptDocument26 pagesThe Sweetheart ExcerptSimon and SchusterNo ratings yet
- PDR Books Product Catalog: 2014 Physicians' Desk Reference®Document5 pagesPDR Books Product Catalog: 2014 Physicians' Desk Reference®odhiles1No ratings yet
- Chapter 4-Photogrammetry and Airphoto InterpretationDocument24 pagesChapter 4-Photogrammetry and Airphoto InterpretationAbayneh GenetNo ratings yet
- Arctic MonkeysDocument12 pagesArctic MonkeysBlueClawNo ratings yet
- Autocollimator: Product Range and SpecificationDocument10 pagesAutocollimator: Product Range and SpecificationLokesh LokiNo ratings yet
- Soal Pisa 2012 (Matematika)Document76 pagesSoal Pisa 2012 (Matematika)Anonymous fy8Wo4bNo ratings yet
- Entry CheckerDocument32 pagesEntry CheckerJosé Sánchez Ramos100% (1)
- The Mark of Athena2Document10 pagesThe Mark of Athena2srasrk11No ratings yet
- The Screen Guilds' Magazine V3 NO1 March 1936Document33 pagesThe Screen Guilds' Magazine V3 NO1 March 1936Carlos de Menezes CastroNo ratings yet
- Redefining The Image Mimesis Convention and SemioticsDocument17 pagesRedefining The Image Mimesis Convention and SemioticsfrankNo ratings yet
- Gonstead Chronology PDFDocument6 pagesGonstead Chronology PDFstansimpson1122No ratings yet