Professional Documents
Culture Documents
Lectura 1 PDF
Uploaded by
groudon_18Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lectura 1 PDF
Uploaded by
groudon_18Copyright:
Available Formats
The Cardiac Action Potential
THE CARDIAC ACTION POTENTIAL
Tom Shannon
tom_shannon@rush.edu
Yahoo: tshanno
iMessage: tshanno@me.com
Resource Material: (Recommended reading assignments)
Reading: Berne and Levy Principals of Physiology, 4th Edition, p. 208-222
Lecture objectives:
1. Learn the obvious differences between action potentials in cardiac muscle and those in nerve
and skeletal muscle.
2. Define the phases (0-4) of the cardiac action potential; understand how these phases apply to
both ventricular and atrial myocytes and to pacemaker cells (e.g., SA node here only
consider phase 4 and phase 0).
3. List the most important types of ionic channels involved in each phase of the cardiac action
potential and describe their basic functions.
4. Understand the unusual behavior of the IK1 potassium channel as a function of membrane
potential. Consider how this behavior is physiologically important to the action potential
plateau, rapid repolarization (phase 3) and pacemaker activity (phase 4 in pacemaker cells).
5. Understand the behavior and role of the pacemaker channel, particularly at the SA and AV
nodes.
6. Understand what is meant by inotropic drugs and be able to describe their basic effects on
the heart.
7. Understand the basic roles of the most important of the many regulatory (or modulatory)
channels that occur in the heart (e.g., IK,ACh, IK,ATP, ICl,cAMP).
8. Recognize that the electrical and mechanical behavior of cardiac muscle (and of smooth
muscle) is modulated in a graded way (very unlike skeletal muscle)
Key Words:
AV nodal delay
phase 0
phase 1
phase 2
phase 3
phase 4
The Cardiac Action Potential
This page intentionally left blank
The Cardiac Action Potential
I. The Cardiac Action Potential
The action potential of cardiac muscle cells is very different from the action potentials of
nerve and skeletal muscle that were described in Lecture 3. In nerve and skeletal muscle
only 2 types of ionic channels are important to the production of action potentials; these are
the voltage-gated Na+ channels and the voltage-gated (delayed rectifier) K+ channels
(although the roles of other background channels e.g., Cl- and K+ channels should not
be forgotten). In cardiac muscle, many more types of ionic channels (most of which were
introduced in the Heart Lectures) contribute to the action potential, and the action potential
is much longer in duration. In addition action potentials in the heart differ significantly in
different locations; some of the underlying channels responsible for action potentials in
different locations are also different.
We will begin by considering the action potential of ventricular myocytes. The ventricles
are normally the last part of the heart to undergo an action potential during each cardiac
cycle. The ventricular action potential is nevertheless the classical cardiac action potential
described in almost all textbooks, and it is therefore a reasonable place to start.
1.
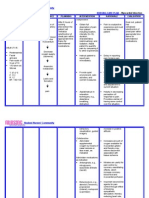
The ventricular muscle cell action potential. An almost bewildering array of ionic
channels contribute to the normal action potential in ventricular myocytes and
elsewhere in the heart. In addition, several other types of channels can become
involved in terms of autonomic nervous system or hormonal regulation and in some
abnormal situations. The best present list of all of these channels is presented in Table
4.1; however, you will NOT be held responsible for all of these in this course. The
channel types that you need to learn about will be clearly described below (and
particularly see Take Home Messages).
The Cardiac Action Potential
The Cardiac Action Potential
2.
Figure 4.1 illustrates a typical ventricular muscle cell action potential. As already
described, the action potential of a ventricular myocyte is characterized by:
a.
b.
c.
d.
e.
a very rapid upstroke (phase 0) reaching a peak overshoot of about +20 to +45 mV
in about a msec.
a fairly rapid decline from the peak of the action potential to about 0 to +10 mV;
this is called phase 1, and takes place over a period of a few tens of msec.
a prolonged plateau (phase 2) at a level of membrane potential around 0 to +10
mV that can typically last from roughly 100 to 300 msec.
membrane repolarization (phase 3) to the resting level. This is a fairly rapid
process, but not nearly as rapid as the upstroke of the action potential.
In ventricular and atrial myocytes, phase 4 simply refers to the period when the
membrane is at its resting potential. In myocytes that display pacemaker activity
(e.g., cells of the SA node, AV node, some Purkinje fibers as well as a few cells is
the atria and ventricles), phase 4 refers to the period of spontaneous depolarization
that leads to the initiation of the next action potential.
We will now consider the processes underling the action potential in greater detail.
3.
Rapid upstroke (phase 0): The rapid upstroke of the action potential of ventricular and
atrial myocytes, as well as Purkinje fiber cells, results from the activation (opening) of
voltage-gated Na+ channels. These channels behave essentially the same as those of
skeletal muscle and nerve (see e.g., Figures 3.3 and 3.4), but it is important to
remember that they are encoded by different genes. Thus, as already noted, a disease
can be specific to Na+ channels of just heart (e.g., some forms of long QT syndrome) or
just skeletal muscle (e.g., paramyotonias).
In addition the T-type (transient) Ca2+ channel, ICa,T is often mentioned in regard to this
phase. This channel type is of greatest importance for pacemaker cells, but may also
occur in ventricular and atrial muscle cells. Its importance to the upstroke in ventricle
and atria is limited, since it is overwhelmed by the voltage-gated Na+ channels.
The Cardiac Action Potential
The Cardiac Action Potential
4.
Early partial repolarization (phase 1): During phase 1 repolarization (partial) the
membrane potential moves from the action potential peak (near +40 mV) to a level in
the neighborhood of 0 to +10 mV. This phase lasts from roughly 1-2 msec after the start
of the action potential up to roughly 50 msec (see Figure 4.1).
Two major processes are involved in this early phase of repolarization. These are:
a.
b.
c.
inactivation of voltage-gated Na+ channels (INa). This process generally takes
only roughly 1-2 msec..
activation of transient outward K+ channels (Ito1). This process takes only a
few msec. These channels are called transient because they also inactivate
over a relatively short period of time. Both their activation and inactivation are
due to membrane depolarization.
activation of a transient outward Cl- current (Ito2 in Table 4.1) is also involved;
this current is activated by increased myoplasmic Ca2+ concentrations.
However, no known diseases are related to defects of this channel, and you
are NOT responsible for this current for the midterm exam.
Other ionic currents (channels) oppose the tendency of the membrane to return towards
its resting potential, thereby helping to hold the membrane potential at its plateau level
of 0 to +10 mV. The most important of these is the opening (activation) of L-type Ca2+
channels (ICa,L). These channels open (activate) at potentials more positive than about
30 mV; they require several msec to activate. L-type Ca2+ channels inactivate very
slowly, typically over a period of several hundreds of msec. These channels allow Ca2+
to enter the myoplasm which is the trigger for the initiation of contraction; in addition,
they are important to maintaining the membrane potential at its plateau level near 0 mV.
Despite the extreme importance of these channels to the cardiac action potential and to
the contractile function of the heart, it is important to realize that Ca2+ channels occur in
densities that are very small (typically about 1/20th to 1/50th) relative to the of the
density of voltage-gated Na+ channels.
The Cardiac Action Potential
The Cardiac Action Potential
It is also important to understand the characteristics of IK1, the inward rectifier K+
channel that is primarily responsible for establishing the resting potential in cardiac
myocytes. The I-V (current-voltage) relationship for this channel is illustrated in
Figure 4.2, and is compared to what would be expected for simple facilitated
diffusion from a K+ selective channel. This sort of relationship is probably not familiar
to you, so I will explain it and what is generally going on in words. In general, the
term rectifier simply means that the channel passes current (i.e., ions) more easily in
one direction than in the other (i.e., inward versus outward). The situation here is more
complex. The cell membrane is always less negative than EK under natural conditions,
so we are only concerned about potentials less negative than about 95 mV in Figure
4.2. However, the current through an individual open channel of this type (i.e., IK1)
does not obey the simple laws of diffusion even in this physiological range of potentials.
If the open channel did obey these simple rules, then the equation IK = gK(Vm EK)
(which is what is expressed by the straight dashed line in Figure 4.2) would hold at all
potentials. It does not. Instead, what is seen is that as the voltage becomes less
negative than about 80 mV, the current through an individual inward rectifier K+
channel (IK1) decreases. This is quite the opposite of what would be expected for simple
diffusion through an open pore. The implications of this for cell function are very
important, and are clinically relevant. What you are seeing is that the current through
these open channels decreases as the membrane potential becomes less negative. This
means that the K+ current that is primarily responsible for establishing the cardiac
myocyte resting potential is actually less during the action potential than when the cell
is at rest. This is not only important in understanding the plateau of the action potential,
but it is also vital to an understanding of the slow (phase 4) depolarization that goes on
in pacemaker cells between action potentials (see below).
5.
Phase 2: The Action Potential Plateau: The plateau of the action potential of
ventricular myocytes (as well as the atrial myocytes and cells of the Purkinje fiber
network) is a prolonged period when the membrane potential is generally in the range of
about -10 to +10 mV. This period can go on for roughly 100 to 300 msec depending on
the cell type and its location in the heart.
This phase of the cardiac action potential is determined by a variety of different
channels; in addition the Na+/Ca2+ exchanger also plays a role in the plateau.
The Cardiac Action Potential
Commentary
Students always wish to know why the IK1 channel is known as an inward rectifier. This is
because, as can be seen in Figure 4.2, the channel does not prefer to conduct outward current
(current at potentials less negative than -95 mV) as much as it prefers to conduct inward current
(current at potentials more negative than -95 mV). Hence the name inward rectifier. This bias
against positive current is why the current actually decreases once you get less negative than -80
mV or so.
The name is confusing because the potentials found within most cells are nearly always less
negative than -95 mV. Therefore, although the channel is known as the inward rectifier and
although it prefers to conduct inward current, you should be aware that it almost never actually
does so. Instead, this channel is nearly always conducting positive current (i.e. K+ is nearly always
The Cardiac Action Potential
The Na+/Ca2+ exchanger usually moves 3 Na+ ions INTO the cell for each Ca2+ ion
moved OUT OF the cell (the 3/1 ratio is always preserved, but due to the fact that this
exchanger is electrogenic, the direction of transport can be reversed i.e., at large
membrane depolarizations the exchanger can actually move Na+ out of the cell and Ca2+
into the cell but dont worry about this). Because of this, this exchanger usually
moves net positive charge INTO the cell this represents an inward (depolarizing) ionic
current.
The magnitude of this inward current depends on myoplasmic Ca2+
concentration, increasing as internal Ca2+ concentration increases (as occurs during the
action potential). Thus the Na+/Ca2+ exchanger contributes to maintaining the plateau at
a depolarized potential.
It is important to recognize that the ionic currents (conductances) during the plateau are
much smaller than those that occur during the rapid upstroke (phase 0) of the action
potential; in fact, they are generally comparable to (but obviously different than and
somewhat larger than) the conductances which occur at rest. Because of this, relatively
small changes in ionic currents (i.e., in the number of open channels of various types)
can have profound effects on the amplitude, shape and duration of the plateau phase of
the cardiac action potential. This can be of great importance clinically. The most
important channels involved in the plateau are:
a. The L-type Ca2+ channel: As already noted, this channel activates over the first few
msec following the rapid upstroke to the action potential. Since this channel type
requires several hundred msec to completely inactivate, an elevated (relative to rest)
calcium current occurs throughout the plateau. This current (which strives to bring
the membrane potential to ECa), is very important to maintaining the membrane
potential near 0 mV throughout the plateau. It is also vital in triggering contraction,
as already described in the Heart lectures.
The Cardiac Action Potential
The Cardiac Action Potential
b. K+ channels:
1.
The behavior of IK1 (the inward rectifier K+ channel that is primarily
responsible for establishing the resting potential) has already been described;
this channel conducts less current during the plateau than when the membrane
is at rest.
2.
Other K+ channels are also involved in the plateau. These include (see Table
4.1) three types of delayed rectifier K+ channels, that differ primarily in the
rate in which they activate in response to membrane depolarization (all of these
open more gradually than the voltage-gated K+ channels in nerve and skeletal
muscle described in the last lecture):
a.
b.
c.
IKs (s stands for slow). This is probably the most important K+ channel
accounting for the gradual decline in the plateau potential and for the
initiation of rapid repolarization to the resting potential (phase 3). This
channel activates very slowly in response to membrane depolarization.
IKr (r stands for rapid). These channels are also activated by membrane
depolarization. However, the term rapid is a very relative one in this
case. These channels activate rapidly by comparison with IKs, but their
activation is still quite slow by comparison to Na+ or Ca2+ channels, and
they are less numerous than the slower (IKs) channels.
IKur (ur stands for ultra rapid). Here the terminology becomes really
confusing since these channels still typically activate more slowly than
either Na+ or Ca2+ channels. Nevertheless, they are rapid in comparison to
either of the other two K+ channels just described, requiring ten msec or so
to become completely activated (on average).
They are relatively
infrequent in ventricular myocytes, but much more common in atrial
myocytes. This probably accounts (at least in part) for the shorter duration
of action potentials in atrial myocytes.
Although it is important to distinguish between these three channel types in
some clinical situations (see, e.g., Clinical Correlation concerning long QT
syndrome), for the purposes of this course it is sufficient to remember that
voltage-gated delayed rectifier K+ channels gradually open during the
plateau of the cardiac action potential, eventually leading to membrane
repolarization.
The Cardiac Action Potential
The Cardiac Action Potential
Finally, it is very important to remember that during the plateau of the cardiac
action potential in ventricular, atrial and Purkinge fiber cells the TOTAL
membrane conductance is quite low essentially comparable to (but somewhat
larger than) the membrane conductance at rest. This means that the plateau is a
period of time when the cardiac membrane potential is finely balanced, and
that small changes in the function of any of the channels involved can have
large effects. This can be important clinically in the use of various drugs, but
can also be dangerous when abnormal situations occur.
6.
Phase 3: Rapid Repolarization to the Resting Potential: After a period that is
typically 100 - 300 msec long, the ventricular action potential ends with a relatively
rapid return to the resting membrane potential. Although this is usually referred to as
rapid repolarization, the process is much more gradual that the rapid (phase 0)
upstroke of the action potential. Rapid repolarization usually requires several tens of
msec to be complete. The most important ionic channels involved are:
Gradual inactivation (and deactivation) of L-type Ca2+ channels. Although these
channels inactivate very slowly, by the end of the cardiac action potential many of
the L-type Ca2+ channels have inactivated. In addition, as the potential during the
plateau and repolarizing phase of the action potential gradually moves back toward
the resting potential, L-type Ca2+ channels that have not inactivated will deactivate
i.e., their activation gates close (the activation gates of these channels begin to
open at about 30 mV and reach a 50% probability of being open near 0 mV),
This, of course, reduces the influx of Ca2+ and thus reduces the tendency for the
membrane to remain depolarized.
b. Gradual increase of the current (number of open channels) through voltage-gated
(delayed rectifier) K+ channels. The most important of these in ventricular
myocytes (according to the best present information) is IKs (see Table 4.1).
c. In addition, the I-V characteristic of the inward rectifier K+ channel (IK1) is
important to rapid repolarization. As you should recall, this channel (which is
normally open and NOT voltage-dependent in terms of its open probability)
conducts less current as the membrane depolarizes from its resting level. Thus as
the membrane repolarizes, more and more current flows through these channels.
This tends to repolarize the membrane. This is an example of positive feedback
the more the membrane repolarizes (moves toward its resting potential) the more
current flows through these channels. This contributes to phase 3 repolarization.
d. The cAMP activated chloride channel (ICl,cAMP, see below) is also involved in
membrane repolarization. Although this channel is generally thought of in terms of
the fact that it is stimulated by sympathetic nervous system (SNS) activity, it is
important to realize that there is some tonic level of SNS activity even under
resting conditions.
a.
The Cardiac Action Potential
The Cardiac Action Potential
It is also important to recognize that the ionic currents involved in repolarization of
cardiac myocytes are small relative to those considered in nerve and skeletal
muscle action potentials, and that the delicate balance between inward
(depolarizing) and outward (hyperpolarizing) currents can easily be altered by
small changes in the currents involved. This has important clinical consequences,
both in understanding the origins of some diseases and in the actions of many
drugs.
7.
Phase 4: In ventricular (as well as atrial) myocytes, phase 4 simply refers to the resting
potential, which is typically near 90 mV. When the membrane is at rest (i.e., between
periodic action potentials) the membrane permeability is highest to K+; this is primarily
because of the inward rectifier (IK1) channels already described. There are also smaller
permeabilities to other ions (mostly Na+ and Cl-).
8.
The Atrial Muscle Cell Action Potential: The atrial action potential is very similar to
the action potential of ventricular myocytes, but is of shorter duration. The basic
appearance of the action potential in atrial myocytes is compared to that of ventricular
myocytes in Figure 4.3.
Of the channels described above, the distribution is more or less the same in the atria in
the ventricles, with the exception of IKur, which is a relatively rapidly activating voltagegated K+ channel; this channel is much more common in the atria than in the ventricles,
and probably partially accounts for the shorter duration of the atrial action potential. It
should also be noted that T-type Ca2+ channels seem to be more common in the SA and
AV nodes than elsewhere in the heart.
The Cardiac Action Potential
The Cardiac Action Potential
Take Home Message
For Action Potentials of Ventricular and Atrial Myocytes
1. Know the characteristics of the action potential that are referred to as phases 0-4.
These are rapid depolarization (phase 0), partial repolarization (phase 1), the plateau
(phase 2), rapid repolarization (phase 3) and the resting potential (phase 4). Realize
that in pacemaker cells, phase 4 refers to the slow depolarization that occurs
between periodic action potentials
2. Learn the most important ionic channels involved in each of these phases and
understand the roles they play. For ventricular myocytes these are:
a. For phase 0, the rapid activation of voltage-gated Na+ channels is normally by
far the most important mechanism for the rising phase of the action potential.
b. For phase 1, the inactivation of Na+ channels and the activation of Ito (most
importantly transient outward K+ channels) accounts for the repolarization; the
relatively gradual activation of L-type Ca2+ channels opposes repolarization and
helps lead to the plateau.
c. For phase 2 (the plateau) there is a delicate balance between inward and
outward membrane currents that holds the transmembrane potential in the
general range of -10 to +10 mV. The primary inward (depolarizing) current is
through L-type Ca2+ channels, many or most of which remain open during this
phase (although net inward positive current carried by the Na+/Ca2+ exchanger
is also involved). The outward currents are almost exclusively carried by K+.
Remember that the inward rectifier (IK1) potassium channel actually carries less
current during the plateau than when the membrane is at rest. There are several
other K+ channels involved during this phase. You may well need to become
familiar with these individually in the future because certain diseases have now
been linked to mutations in the genes encoding individual ionic channels of this
group; however, for this course, it is sufficient to realize that during the plateau
the membrane permeability to K+ gradually rises and helps to bring about phase
3 (repolarization i.e., the end of the action potential).
d. Phase 3: repolarization is brought about by the slow inactivation and
deactivation (closing of activation gates due to membrane repolarization) of Ltype Ca2+ channels and by the gradual increase in the membrane permeability to
K+; eventually K+ wins. You should also remember that as the membrane
repolarizes the current through IK1 potassium channels increases, and helps in
repolarization. The effects of ICl,cAMP will be described below.
e. Phase 4 in ventricular and atrial myocytes is simply the period when the
membrane is at its resting potential. K+ permeability is relatively higher than
the membrane permeability to other ions (primarily due to IK1). However, there
are also smaller background permeabilites to Na+ and Cl-.
3. The major difference between action potentials in atrial and ventricular myocytes is
the fact that action potentials in the atria are of shorter duration than those in the
The Cardiac Action Potential
ventricle. This appears to be due to a more rapid increase in the membrane
permeability of atrial myocytes to K+ during the plateau phase.
The Cardiac Action Potential
Clinical Correlation 1:
Myocardial Infarct. Myocardial infarct (MI, heart attack)
remains one of the leading causes of death on earth. Its causes are simple enough, but
the consequences are varied and extremely complex. The cause is the blockage of all or
part of the blood flow to some branch of the coronary arteries. This, of course, leads to
decreased blood flow (ischemia) to some portion of the heart. The results depend on
the portion of the heart that is deprived of normal blood flow, and the degree of
coronary artery perfusion (mild situations are simply called ischemic heart disease,
where coronary blood flow is dangerously reduced, but not eliminated for any portion
of the heart). MI is a condition when a portion of the heart receives so little blood flow
that irreversible necrosis of certain regions of heart muscle results from prolonged
ischemia. About 1.5 million Americans suffer from MI each year; and of these nearly
1/3rd (500,000) die each year.
Despite these disturbing statistics, there has been very significant progress in dealing
with this condition over the 25 years since I finished school. Most of this progress has
been due to more understanding of the underlying pathophysiology and due to
numerous therapeutic advances. Here we will only study a few of the basic disorders
that are associated with MI. Blockage of particular branches of the right and left
coronary arteries lead to different sites of infarct. The location and extent of an MI can
often be reasonably estimated via the ECG.
Reversal of underlying cause by
thrombolytic therapy can often be decisive in determining patient survival.
Here I only want to consider some affects in the region that has insufficient coronary
blood flow: These include:
1. Insufficient production of ATP by the affected cells.
2. Loss of ATP-dependent functions such as the Na+/K+ pump of the surface
membrane and the Ca2+ pump of the SR and surface membranes. These lead to
elevated myoplasmic concentrations of Na+ and Ca2+, and to elevated extracellular
K+.
3. One result of this is a less negative resting potential and the resting inactivation of
many Na+ (and eventually Ca2+) channels.
4. Moreover, the lack of ATP causes the opening of IK,ATP channels (see below) that are
initially protective, but eventually destructive.
5. Low levels of ATP force myocardial cells to utilize their limited glycolitic capacity.
pH falls. In addition cytoplasmic Ca2+ is rising. Both of these factors lead to
decreased coupling via gap junctions.
Increased cytoplasmic Ca2+ activates
damaging proteases.
6. Everything that can go wrong is going wrong. Cells have fewer available Na+
channels, and their connections via gap junctions are declining. Both of these
factors cause slower action potential propagation (think about why this is the case).
7. Slow conduction and reduced duration of the action potential can predispose the
affected region of the heart to arrhythmias. Remember that the affected region is
rapidly becoming a mosaic of sick and healthy cells. The factors described above
are a formula for disaster when it is considered that the normal function of the heart
The Cardiac Action Potential
relies on synchronization and an orderly progression of electrical and mechanical
events.
The Cardiac Action Potential
Two other forms of LQTS are also known to differ from those described above (LQT4
and LQT5), but at present their underlying causes are not completely understood.
If the condition is diagnosed (which unfortunately remains unlikely), then differential
diagnosis can lead to differential treatment. For LTQ3 (involving abnormal Na+
channels), Na+ channel blockers are the treatment of choice, and so-called open
channel blockers (e.g., mexiletine) presently seem to be a promising therapy. If the
condition involves K+ channels then different therapies are appropriate. These include
drugs that help to open K+ channels. The effectiveness of such drugs is presently
greater in cases that involve IKs (LTQS1) than in those which involve IKr. Hopefully
future research will find new and more effective treatments.
9.
The Action Potential of the Sino-Atrial (SA) Node: You should remember that the SA
node is located in the right atrium near the entry of the superior vena cava. Under
normal circumstances it is the pacemaker for the entire heart. The basic appearance of
the SA nodal action potential is shown in Figure 4.6. It can be seen that the rising
phase (phase 0) of this action potential is much more gradual than that that which
occurs in ventricular and atrial myocytes. In addition, the peak amplitude of the action
potential is smaller, and there is no well-defined plateau. Finally, for SA nodal cells
(and cells of the AV node) there is no real resting potential; instead, the membrane
potential is constantly changing, with phase 4 depolarization leading to periodic action
potentials.
It should not be surprising that the underlying channels responsible for the action
potential in the SA (and AV) node are in many cases different from those described
above for ventricular and atrial myocyte action potentials. I will briefly summarize the
main differences as a preview of what is described in greater detail below:
a.
SA nodal cells (like those of the AV node) do not have any significant number of
voltage-gated Na+ channels.
The Cardiac Action Potential
The Cardiac Action Potential
b.
The membranes of SA nodal cells contain pacemaker channels (If). These
channels are important to pacemaker depolarization leading to periodic spontaneous
action potentials in these cells. Pacemaker channels also occur in the AV node and
at least some Purkinje fiber cells. However they are absent (or uncommon) in most
ventricular and atrial myocytes.
c.
The variety of K+ channels involved in the action potential of SA node (and AV
node) may not be as large as that which contributes to the action potentials of
ventricular and atrial myocytes, and is less well understood.
d.
T-type Ca2+ channels play a more important role in the upstroke of the SA nodal
action potential than is the case in ventricular and atrial myocytes.
10. Phase 4 Depolarization: Unlike the myocytes of the ventricles and atria, during phase
4 the membrane potential of cells in the SA node (and AV node) is continuously
depolarizing. The most negative potential achieved during phase 4 is about 60 to 65
mV and takes place just after the end of the action potential. There are at least two
basic underlying mechanisms involved in this process. These are:
a.
The opening (activation) of pacemaker channels (I). All (or almost all) other
known voltage-gated channels activate (open) when the membrane potential
depolarizes.
However, pacemaker channels activate when the membrane
hyperpolarizes. It is because of this unusual behavior that this current goes by the
name of If f stands for funny since their voltage dependent behavior is so
unusual. These channels are closed when the membrane potential is less negative
than about 35 mV. Thus during most of the action potential these channels are
closed. However, as the action potential ends and the membrane potential becomes
more negative than 35 mV, pacemaker channels begin to gradually open. Opening
is a slow process, requiring several hundred msec to become complete. However,
as soon as they begin to open, these pacemaker channels tend to depolarize the
membrane. Their opening becomes more rapid as the membrane potential moves to
its most negative value of about 60 mV. These are relatively non-selective cation
channels, i.e., they allow both Na+ and K+ to cross the membrane. The effect of
letting both Na+ and K+ cross the membrane is to drive the membrane potential
toward about 0 mV. Thus the membrane begins to depolarize. Since these channels
both open and close slowly, even though the membrane potential is becoming less
negative (which should close the channels), pacemaker channels remain open until
well into the rising phase of the next action potential.
b.
At the end of the action potential, voltage-gated K+ channels in the SA nodal cells
are closing as the membrane hyperpolarizes. Since these channels will not again
open until the next action potential, they soon become unrelated to the evolving
membrane potential.
The Cardiac Action Potential
The Cardiac Action Potential
c.
However, the behavior of IK1 (inward rectifier) K+ channels remains very
important. Remember that these channels are NOT voltage-dependent in terms of
their open probability; they are essentially open all of the time. But their ability to
pass current (K+ ions) depends on membrane potential. Specifically, these channels
pass less current (allow fewer K+ ions to cross the membrane) as the membrane
potential depolarizes to potentials less negative than about 80 to 70 mV. Current
through these channels helps to keep the membrane potential near EK. When these
channels pass less current, there is less of a tendency to keep the membrane
hyperpolarized (i.e., near EK). As the membrane depolarizes during phase 4, these
channels pass less and less K+ current, and this contributes to phase 4 membrane
depolarization. Once again, note that this is another example of positive feedback.
The more the membrane depolarizes the less current these channels allow to cross
the membrane, thereby augmenting further depolarization.
d.
The role of T-type Ca2+ channels (ICa,T, T stands for transient) channels involves
both the last part of phase 4 depolarization and the first part of phase 0 (i.e., the
upstroke of the SA nodal action potential). These Ca2+ channels activate (open) at
more negative potentials than do L-type Ca2+ channels. Activation begins when the
membrane potential becomes less negative than about 50 mV, whereas L-type
Ca2+ channels do not significantly begin to activate until the membrane potential
becomes less negative than about 35 to 30 mV. These channels are called
transient because they inactivate much more rapidly than L-type channels. The
importance of T-type Ca2+ channels to the action potential of the SA node (and AV
node) is simple: they give a rapid boost to membrane depolarization once the
membrane has depolarized to 50 to 45 mV. Thus they are not only responsible
for the end of phase 4; they are also responsible for the start of phase 0, i.e., the
action potential upstroke.
11. Phase 0, The Action Potential Upstroke: As already noted, SA and AV nodal cells do
not have significant numbers of voltage-gated Na+ channels. Thus the upstroke of the
action potential in these cells must be supported by other types of ionic channels. These
are the T-type and (more importantly) L-type Ca2+ channels. As already described, Ttype Ca2+ channels activate first (i.e, at more negative membrane potentials), but these
channels are fewer in number than L-type Ca2+ channels and also inactivate fairly
rapidly. Once the membrane potential reaches about 35 to 30 mV, L-type Ca2+
channels begin to open. They open quite gradually in comparison to Na+ channels
(requiring a few msec), but as they open they drive the membrane potential toward ECa.
Despite the fact that these L-type channels are more numerous than T-type Ca2+
channels, their density is far lower (roughly 20-50 to 1) than that of Na+ channels found
in the membranes of ventricular and atrial myocytes. The low density of these
channels, coupled with their relatively slow activation, accounts for the much more
gradual upstroke of the action potential in SA and AV nodal cells in comparison with
action potentials in ventricular and atrial myoctyes and Purkinje fiber cells.
The Cardiac Action Potential
The Cardiac Action Potential
12. The action potentials of SA and AV nodal cells end due to the gradual inactivation and
deactivation of L-type Ca2+ channels and the delayed activation of voltage-gated K+
channels; the behavior of IK1 potassium channels should also be remembered in this
process.
13. A few other aspects of the action potentials of the SA and AV nodes are also clinically
important and will be briefly described here.
a. Conduction velocity of the action potential in these tissues is quite slow by
comparison with the velocity elsewhere in the heart. This is of greatest importance
in the AV node, and accounts for AV nodal delay. Even though the AV node is a
very small structure, about 0.1 second is required for the action potential to spread
from the atria to the ventricles through this tissue. There are three basic reasons for
this slow conduction. These are: 1) the absence of Na+ channels, 2) the relatively
low density of Ca2+ channels, and 3) relatively fewer gap junctions between cells in
the AV node.
b. Although both the SA node and AV node show intrinsic pacemaker activity, the rate
of spontaneous action potentials is normally faster in the SA node (typically about
70 per minute under resting conditions) than in the AV node (typically about 50 per
minute at rest). Thus under normal conditions the SA node is the pacemaker for the
entire heart. Other tissues in the heart also exhibit pacemaker activity (e.g., some
Purkinje fiber cells as well as some cells in the ventricles themselves), but this is at
a rate even slower than that of the AV node.
The Cardiac Action Potential
The Cardiac Action Potential
TAKE HOME MESSAGE
For Action Potentials of the SA and AV Nodes:
1. The action potentials of the SA and AV node differ significantly from those described for
ventricular and atrial myocytes. The most important phases of these action potentials to
consider are phase 4 and phase 0.
2. Pacemaker activity (phase 4): When the action potential ends in the cells of the SA node
and AV node, the membrane potential usually does not become more negative than about
60 mV and it then promptly begins to depolarize leading to another action potential. There
are two main membrane permeabilities (channels) that are presently believed to underlie this
phenomenon in normal tissue. These are 1) the activity of the pacemaker channel (If), and 2)
the characteristics of the inward rectifier K+ channel (IK1). You should understand the
characteristics of both types of channels and how they contribute to pacemaker activity. But
the take home message is fairly simple: current through pacemaker channels generally
increases during phase 4, while current through IK1 potassium channels decreases during this
period. In addition to these channels, when the membrane potential reaches about 50 mV,
T-type Ca2+ channels begin to open. These channels are only open for a relatively brief
period of time, but they provide an added boost which helps begin phase 0 depolarization.
3. Phase 0 depolarization: This is the upstroke of the action potential in SA or AV nodal cells.
It is considerably more gradual than the rapid upstroke of the action potential seen in
ventricular, atrial and Purkinje fiber cells. The reason for this is that cells in the SA and AV
nodes lack any significant number of voltage-gated Na+ channels. Instead the action
potential upstroke primarily results from the activation of L-type Ca2+ channels, which
typically begins when the membrane potential depolarizes to near 35 mV. However, the
activation of these channels is (on average) much slower; and their density is much lower
than that of Na+ channels in ventricular and atrial tissue. These are the reasons why the
upstroke of the action potential is much slower in the SA and AV node than in other
locations in the heart.
4. The end of the action potential results (as usual for heart) from the gradual inactivation of Ltype Ca2+ channels combined with the delayed activation of voltage-gated K+ channels, plus
the actions of IK1 that have already been described.
5. The conduction velocity of the action potential in the SA node and especially the AV node is
slower than elsewhere in the heart.
6. Normally the SA node is the pacemaker for the entire heart.
The Cardiac Action Potential
Clinical Correlation 1:
A variety of normal physiological inputs can affect the behavior of the SA node and AV node; in
addition, many drugs can also affect these tissues. Many of these have already been summarized
during the Heart lectures, and will be reviewed in the ANS and Muscle lectures which follow.
Thus they will not be reviewed at this time. However, it is important to realize that these are
very important sites for clinical intervention in many cardiac diseases.
Clinical Correlation 2: More about Hyperkalemia and the Heart
The effects of hyperkalemia (elevated extracellular K+ concentration) have already been
introduced, and their affects on the ECG were illustrated in a clinical correlation at the end of
Lecture 2. Here we will consider these affects in greater detail, since the information of more
recent lectures should now allow you to understand them at a cellular/molecular level (which is
often the level at which you treat many diseases). Figure 4.7 once again (it is the same as
Figure 2.6) shows the progressive changes in the ECG as the extracellular K+ concentration rises
to higher and higher levels.
These changes are primarily due to decreased availability of voltage-gated Na+ channels
(resting inactivation) due to progressive depolarization of the resting membrane potential by
elevated [K+]e. To understand the ECG changes you must remember that the P wave represents
the time that the leading edge (phase 0) of the action potential spreads across the atrium and that
the QRS complex represents the time required for the leading edge of the action potential to
spread throughout the ventricles. In addition, you must remember that fewer Na+ channels mean
(among other things) a slower propagation velocity.
Finally note that elevated [K+]e can happen locally in regions with restricted blood flow. This
can occur, for example, to regions of the heart affected by myocardial infarct. Also note that
moderately elevated extracellular potassium has less effect on the SA node and AV node than on
atrial and ventricular tissue because the SA and AV nodes do not have significant numbers of
voltage-gated Na+ channels.
The Cardiac Action Potential
14. Regulatory (Modulatory) Channels of the Heart: In addition to the channel types
described above that underlie the normal action potentials at various locations in the
heart, there are also several types of regulatory (or modulatory) channels that can
modify the action potential and serve other vital functions. These channels can be
categorized as either potassium or chloride channels. We will begin by considering the
modulatory potassium channels.
Modulatory K+ channels: There are at least 4 types of modulatory K+ channels (in
addition to the K+ channel types already described) that serve important roles in the
function of the heart. These are:
a. IK,Ach, the K+ channel that is stimulated by the release of acetylcholine from
parasympathtic (vagal) nerve terminals that innervate the atria and nodal tissue of
the heart.
b. IK,ATP, which are potassium channels that are inhibited by normal levels of
intracellular ATP, but which open when ATP levels are below normal.
c. IK,Ca2+, which are K+ channels that are activated by elevated levels of cytosolic
Ca2+. The role of these channels and their prevalence in heart is controversial,
although it is clear that they would accelerate repolarization in a calcium-overloaded
heart.
d. IK,Na+, which are potassium channels that are activated by high cytosolic
concentrations of Na+. Once again, the role of these channels is not entirely clear,
although they could be expected to promote repolarization in a sodium-overloaded
heart (e.g., as is likely to occur during digitalis treatment).
Here we will only consider IK,ACh and IK,ATP, and these are the only two channels of
this group that you are responsible for.
1.
The ACh activated K+ channel (IK,AC): The function of this channel has already
been introduced in the Heart Lectures (pages 52-53). This is a critical modulator of
the excitability of the SA node, AV node and atrial tissue; the channel is essentially
absent in ventricular myocytes. When these channels are opened (by ACh or by
drugs) they cause a hyperpolarization of the tissues in which they occur (most
importantly SA and AV node) that slows the rate of spontaneous (phase 4)
depolarization and therefore slows heart rate. These channels are important in both
normal physiological (parasympathetic) control of the heart and in therapeutic
control of supraventricular tachycardias.
2.
ATPsensitive K+ channels (IK,AT): These channels are normally closed. They
open in response to low intracellular levels of ATP, as occurs most commonly
during periods of ischemia. Surprisingly these are apparently the most common K+
The Cardiac Action Potential
channels in the heart even though they have no significant role in most normal
physiological situations. If intracellular ATP levels fall, then these channels will be
activated, and that their activation shortens the action potential Pacemaker activity
is also slowed. This reduces further depletion of vital ATP reserves. These are
clearly beneficial effects. But other effects are definitely NOT beneficial, and
become more pronounced as the period of time that these channels are open
increases.
These include increased K+ current which leads to increased
accumulation of K+ in the extracellular spaces surrounding cardiac myocytes (this
problem is particularly severe in ischemic regions because reduced or eliminated
blood flow means that potassium that accumulates will not be removed and thus
distributed throughout the body by the blood).
Thus IK,ATP can be both beneficial and harmful. Its major benefits are obvious in
short periods of ischemia (followed by normal blood flow); its most damaging
effects become apparent during prolonged periods of ischemia.
Membrane
+
depolarization associated with elevated external K concentration, as can result
from prolonged opening of IK,ATP channels, leads to the inactivation of many
(ultimately most or all) Na+ channels, and also begins to inactivate Ca2+ channels as
well. These affects not only change the shape and duration of action potentials at
various locations in the heart, but also slow action potential conduction, cause
complete failure of conduction in localized regions, and can predispose the heart to
dangerous arrhythmias. The control of IK,ATP by various drugs is presently being
investigated and is likely to soon become clinically important.
15. Modulatory Chloride Channels: There is only a small contribution of chloride current
to the normal cardiac action potential under resting conditions. Part of this results from
a current denoted by Ito2 (see Table 4.1); however, malfunctions of this channel are not
associated with any known disease and you are NOT responsible for this channel/
current.
However, there are other Cl- channels that are recruited by the sympathetic nervous
system (ICl,cAMP) and by cell swelling (ICl,swell). The equilibrium potential for chloride
(ECl) in normal cardiomyocytes is typically between about 45 and 65 mV, which is
near, but certainly not equal to the resting potential. Because of this, chloride channels
are very well suited to fine-tune the cardiac action potential. All other ionic channels
that we have considered pass current in only one direction under normal physiological
conditions; e.g., Na+ and Ca2+ ALWAYS flow into the cell and K+ ALWAYS flows out
of the cell through open ionic channels. This is because the cell membrane potential
never crosses ENa (about +60 mV), ECa (about +100 mV) or EK (about 95 to 100
mV). However, this is not always the case for chloride channels. At membrane
potentials more negative than ECl, Cl- leaves the cell and causes a membrane
depolarization (inward current). At potentials more positive than ECl, Cl- enters the cell
(outward current) and causes membrane hyperpolarization. Thus these channels
provide novel targets for antiarrhythmic agents.
The Cardiac Action Potential
Why should the equilibrium potential for Cl- fall in the range of 45 to 65 mV? Chloride is not
actively transported across most cell membranes, including those of the heart. Because of this
cells that spend most of their time at their resting potential will have values of ECl that are very
near the resting membrane potential. However, cardiomyocytes typically spend about 1/3 of the
time undergoing action potentials and it is the AVERAGE membrane potential over time that
determines ECl in this situation. If a typical ventricular myocyte spends about 1/3 of its time at
+10 mV (during the action potential) and 2/3 of its time at 90 mV (the resting potential), then
the average potential and ECl will be about 57 mV. This value can change as the result of a
variety of factors, including sustained changes in heart rate and diseases such as long QT
syndrome.
ICl,cAMP is physiologically activated by the sympathetic nervous system through the
same pathways illustrated in Figure 3.11 of the Heart Lectures (although this channel is
not shown in the figure because I was too lazy to put it in). In the human heart, this
channel occurs in both ventricular and atrial tissue, but is most common in ventricular
myocytes. When activated, this channel leads to a shortening of the cardiac action
potential. You should be aware that even under resting conditions there is some
sympathetic output (tone) to the heart, so that this channel contributes somewhat to
the cardiac action potential under these situations. With increased sympathetic activity
due to exercise, stress, etc., the activity of these channels greatly increases. Although
some of these channels are apparently open at the resting potential, membrane
depolarization is also required to fully activate ICl,cAMP.
16. In addition to the channels just described that do not generally play major roles in the
cardiac action potential under normal resting conditions (although there is some
activity of IK,ACh and ICl,cAMP under resting conditions, due to maintained sympathetic
and parasympathetic activity in this situation), it is also important to remember that
other channels are also modulated by autonomic inputs and various drugs. Those
modulated by the autonomic nervous system have already been described in the Heart
Lectures (see Fig. 3.11) and include L-type Ca2+ channels, pacemaker channels, and
certain delayed-rectifier K+ channels (most importantly IKs). Of course the roles of
these channels in various locations in the heart have already been described.
The Cardiac Action Potential
TAKE HOME MESSAGE
For Regulatory Channels of the Heart
1. The only modulatory channels that you will be held responsible for are:
a. The ACh-activated K+ channel (IK,ACh)
b. The ATP-dependent K+ channel (IK,ATP), and
c. The cAMP-dependent chloride channel (ICl,cAMP)
2. You should know the basic behavior of these channels and their role in the heart. Each of
these channels has important clinical implications for both the normal and abnormal
function of the heart.
3. Remember that L-type Ca2+ channels, pacemaker channels and certain voltage-gated
delayed rectifier K+ channels are also modulated by the autonomic nervous system. Also
remember that although IK,ACh is activated by parasympathetic activity and ICl,cAMP is
activated by sympathetic activity, there is enough discharge from both branches of the
ANS under resting conditions so that these channels also play some role in this situation.
The Cardiac Action Potential
17. Summary Figures of the Most Important Currents/Channels Involved Cardiac Action
Potentials. Figure 4.8 shows a typical action potential from a ventricular myocyte and
the most important currents/channels which produce it. Inward currents go downward
from baseline and outward currents go upward. The same basic currents also underlie
the action potentials of atrial myocytes and Purkinje fibers. Note that different currents
are NOT always drawn at the same scale.
The Cardiac Action Potential
FIGURE 4.8 Not all channels/currents are illustrated in this Figure (but the ones you are
responsible for are shown). IK,dr is the sum of all delayed rectifier K+ channels (IKs, IKr, IKur).
Note that INa (relative to the other currents shown) is about 50 times larger than shown in the
Figure; the other currents are shown roughly to scale.
The Cardiac Action Potential
A bit of commentary: So have I placed so much emphasis on all of these channels and
membrane properties in this lecture? The answer is simple: Membranes are the site at
which you will do battle with many types of disease. The protein molecules embedded in
membranes are the site of action of many or most of the drugs you will prescribe. The life
and death of your patients will often hinge on events that take place at the membrane level.
This certainly does not mean that ALL diseases have an origin at the membrane level but
many do, and an understanding of events at this level is absolutely vital to your practice of
medicine.
Almost every channel mentioned is now known to be involved in one disease or another
(several examples have already been presented). As medicine progresses, diseases that
were once believed to have a single underlying cause (due to more or less uniform
symptoms) are frequently recognized to have numerous distinct causes. And as these
causes come to be understood at the molecular/genetic level (which is occurring at an ever
increasing rate), distinct therapies are also beginning to emerge. At the start of my career I
could never have imagined all that has been learned in the past 25 years. You are now at the
start of your careers, and I am sure that 25 years from now neither you nor I will have
imagined all the new knowledge that will be learned, and the new clinical approaches and
treatments that will result.
By that time, some of you will be spending a significant
fraction of your time teaching yet another generation to become physicians. And like my
generation wants to prepare you for the future, you will want to prepare them. And it will
get harder and harder as the body of knowledge continues to grow at a faster and faster
pace. So why all the channels, receptors, etc? Because I think that the more you learn
about such things now, the better prepared you will be for the rapidly changing future.
The Cardiac Action Potential
FIGURE 4.9 shows the action potential of myocytes in the SA (or AV) node. The most
important currents/channels that produce this action potential are illustrated below the action
potential (not all currents are shown). Once again, inward currents go downward and
outward currents go upward from the baselines.
The Cardiac Action Potential
II. Modulation of the Electrical and Mechanical Activity of Cardiac and
Smooth Muscle
1.
Smooth muscle occurs in many organs/tissues, including the walls of most blood
vessels, the gastrointestinal tract, the reproductive and urinary tracts, the airways of the
lungs, the iris of the eye and in the skin surrounding hair follicles. The smooth muscle
in all of these tissues has certain common features, but there are also large differences
between smooth muscle in different organs/tissues, and even within a single organ
system. Most of your knowledge of the specifics of smooth muscle in different tissues
will come from the study of these tissues as the course proceeds. During the Muscle
Lectures, I will introduce you to many general features of smooth muscle. Here it is
sufficient to recognize that smooth muscle is innervated by the autonomic nervous
system (ANS) and that its contractile behavior is modulated by many factors including
ANS inputs, circulating hormones and numerous local chemical factors (e.g., changes in
O2, CO2, pH, osmolarity).
2.
An important distinction between skeletal muscle and cardiac and smooth muscle is that
the electrical and contractile behavior of cardiac and smooth muscle is modulated by
many external influences, while, under normal circumstances, the behavior of skeletal
muscle is very stereotyped.
3.
In the first place, unlike skeletal muscle, cardiac muscle and many (but not all) types of
smooth muscle do not require nervous system inputs to produce action potentials (and
hence contraction).
Instead, these tissues display spontaneous rhythmic action
potentials (e.g., the pacemaker activity of the SA node). By contrast, under normal
circumstances, skeletal muscle will only produce an action potential and the resulting
contraction if it is stimulated by a motoneuron.
4.
Cardiac and smooth muscle (again unlike skeletal muscle) are innervated by the
autonomic nervous system (ANS) and affected by various circulating hormones. The
ANS typically does not initiate an action potential or contraction in cardiac or many
types of smooth muscle, but instead it modulates the electrical and contractile behavior
of these tissues.
The Cardiac Action Potential
5.
In the case of cardiac muscle you have already been introduced to the modulatory
affects of the ANS, so these will not be repeated here (see pages 48-54 of the Heart
Lectures). This subject will also be reviewed in the ANS and Muscle Lectures.
6.
Several modulatory influences on smooth muscle were listed above (but recognize that
not all of these may affect all types of smooth muscle). Here I will just present a very
brief overview of autonomic nervous system (ANS) affects on smooth muscle (and, in
some cases, cardiac muscle).
Most smooth muscle is innervated by both the
sympathetic and parasympathetic branches of the ANS (although there are important
exceptions, such as most vascular smooth muscle which only receives sympathetic
inputs).
The mode of transmission between the ANS and both cardiac and smooth muscle also
differs in some ways from that which you will learn about in the next lecture for
synapses between nerves and between motor neurons and skeletal muscle cells. What
follows is in some senses a brief preview to what you will learn soon. In synapses
between nerves and between nerve terminals and skeletal muscle fibers, the synapsing
cells come into very close contact in the region of the synapses and the receptors in the
postsynaptic cell are clustered in the region of the synaptic junction (they generally do
not occur in other parts of the cell membrane). On the other hand, ANS nerve terminals
generally travel across the surface of cardiac and smooth muscle cells forming periodic
varacosities that are the site of release of transmitter molecules (norepinephrine or
acetylcholine in the case of the ANS). These varacosities are often at a much greater
distance (up to about a micron) from the surface of the cells innervated by the ANS, and
the ANS receptors ( and adrenergic receptors and muscarinic receptors) are
generally dispersed over the entire surface of the post-synaptic cell (e.g., smooth muscle
cell) the overall affect is a slower but more global response. This emphasizes an
important point about both the ANS and smooth muscle: neither one is concerned with
extremely rapid and precise responses; both usually have a more leisurely pace and are
more often than not interested in highly graded responses.
The Cardiac Action Potential
TAKE HOME MESSAGE
For Modulation in Cardiac and Smooth Muscle
1. Unlike skeletal muscle, cardiac muscle and many types of smooth muscle do not
need nervous system inputs to generate action potentials. ANS innervation of
cardiac and smooth muscle does not usually initiate electrical and contractile events,
but instead it modulates these events.
2. Understand the main differences (structural and functional) between synaptic
transmission between the ANS and its target organs and neuron-neuron or nerveskeletal muscle synapses (this will be clearer after Lecture 5).
3. Review the ANS affects on the heart described in the Heart lectures.
4. Remember that smooth muscle is usually designed to provide very finely graded
(highly modulated) contractile responses.
The Cardiac Action Potential
MEMBRANE PHYSIOLOGY QUIZ FOR THE CARDIAC ACTION POTENTIAL
Note that this and other Membrane Physiology quizzes are simply provided to you to help you to
test your understanding of the content of each lecture. They are not substitutes for studying the
lecture notes (including Objectives and Take Home Messages), Practice Exams or other
material intended to guide your learning. These Quizzes have NOT been designed to mimic the
Midterm in terms of style or level of difficulty.
MULTIPLE CHOICE QUESTIONS:
1.
Phase 0 of the ventricular cell action potential results from:
a.
b.
c.
d.
e.
2.
Phase 2 of the cardiac action potential is primarily due to:
a.
b.
c.
d.
e.
3.
b.
c.
d.
e.
produces an inward (depolarizing) current that helps maintain the membrane
potential near 0 mV
produces an outward (hyperpolarizing) current that helps to initiate phase 3
repolarization
moves Na+ out of the cytoplasm and moves Ca2+ into the cytoplasm
has no effect on the membrane potential because it does not produce any net
transmembrane movement of charge
both b and c are correct
Pacemaker channels in the heart:
a.
b.
c.
d.
e.
5.
the closing of voltage-gated Na+ channels
the opening of voltage-gated Na+ channels
the opening of T-type Ca2+ channels
the opening of Cl- channels
none of the above is correct
During the plateau phase of the cardiac action potential the Na+/Ca2+ exchanger:
a.
4.
the closing of voltage-gated K+ channels
the activation (opening) of voltage-gated Na+ channels
the activation (opening) of L-type Ca2+ channels
the inactivation of pacemaker channels
all of the above contribute to phase 0 in ventricular myocytes
open very rapidly (< 10 msec) in response to membrane depolarization (Vm less
negative than 35 mV)
open slowly in response to membrane depolarization
open slowly in response to membrane hyperpolarization (Vm more negative than
35 mV)
close slowly in response to membrane hyperpolarization
both b and d are correct
The inward rectifier potassium current (IK1):
The Cardiac Action Potential
a.
b.
c.
d.
e.
6.
is primarily responsible for establishing the resting potential of ventricular and
atrial cardiac myocytes
is smaller during the plateau phase of the cardiac action potential than when the
membrane is at rest
decreases as the membrane potential becomes less negative than about 80 to
70 mV and therefore contributes to phase 4 depolarization in SA and AV nodal
cells
b and c only are correct
a, b and c are all correct
The opening of ACh-activated K+ channels in the heart cause (or help to cause):
a.
b.
c.
d.
e.
decreased action potential propagation velocity in the ventricles
increased action potential propagation velocity in both the atria and ventricles
increased action potential propagation velocity in the AV node
decreased heart rate
increased heart rate
TRUE-FALSE QUESTIONS:
7.
Phase 2 of the ventricular action potential is also known as the plateau.
8.
Phase 3 repolarization of the action potentials of atrial and ventricular myocytes results
primarily from the inactivation of voltage-gated Na+ channels.
9.
In order to contract under normal physiological circumstances cardiac muscle cells must
always produce action potentials.
10.
Hyperkalemia will cause the resting potential of cardiac muscle cells (and many other
cells in the body) to become more negative.
11.
The equilibrium potential for Cl- (ECl) in cardiac myocytes is always within 5-10 mV of the
resting membrane potential.
12.
IK,ATP channels in the heart open when intracellular ATP concentrations decrease below
normal levels.
13.
The opening of IK,ACh channels in the atria and SA and AV nodes is due to activation of
sympathetic nerves that innervate the heart.
14.
The rising phase (upstroke) of action potentials in SA node and AV node cells is caused
by the activation of voltage-dependent Na+ channels.
The Cardiac Action Potential
15.
Greatly reduced numbers of voltage-dependent Na+ channels that are available to
activate in ventricular myocytes (e.g., due to a less negative membrane resting potential)
will result in a prolonged QRS complex in the ECG.
Answers: 1. b, 2. e, 3. a, 4. c, 5. e, 6. d,
7. T, 8. F, 9. T, 10. F, 11. F, 12. T, 13. F, 14. F, 15. T
The Cardiac Action Potential
FREQUENTLY ASKED QUESTIONS
These are questions regarding this material which have often been asked of me in the
past. They are frequently copied and pasted directly from emails. Most of them cover
topics I consider it to be important for you to know.
1.
Do Na+ channels have an effect on actions potentials of the pacemaker cells if an effect at
all?
There are very few of the classic voltage-gated Na channels in pace maker cells. For
our purposes they play no role in the phase 0 depolarization. It's practically all Cadependent. Note that funny channels (If) do pass Na in phase 4.
2.
I've been "spinning my wheels" trying to understand the Inward Rectifier channel and hope
you can help. If potassium is leaving the cell through this channel (outward current) why is
it called an "inward" rectifier? I thought "inward" implied that current flows into the cell
easier than outward.
If you look at the IV curve in the Membrane syllabus, you will see that the current is
normal when it is negative to the K reversal potential. That is, its a linear function of
voltage. However, above that line, the current curves off at about -70 mV after going
a somewhat positive, eventually returning to near 0. The channel is always open but it
passes very little current less negative than about -30 mV or so. The channel lives
more or less in this area, positive to the reversal potential. So it passes outward
current but it passes less and less of it as depolarization takes place. Thats why its
an inward rectifier. The inward current is fine and it prefers to pass that. But it rarely
sees voltages less than the reversal potential to K physiologically (if ever). It also
doesnt like passing K outward very much and eventually it almost completely stops as
voltage goes up.
3.
I understand how the inward rectifier channel can help re-polarize the cell at the end of the
action potential but don't understand why this channel would help in pacemaker
depolarization.
Also, which channel is primarily responsible for re-polarization...the inward rectifier or the
delayed rectifier channel? I had always thought that the delayed rectifier channel was
primarily responsible but this channel is really throwing me for a loop.
Delayed rectifiers help with repolarization. Its their primary function. That is why they
are delayed. Their opening takes place with depolarization but they open more
slowly, gradually adding their effect to the AP until they eventually overwhelm the
inward currents and reploarization takes place (as positive K ions pass outward).
Inward rectifiers do help with repolarization. But not until the delayed rectifiers get the voltage
down into an area where they better pass current, say more negative than about -30 or so. They
perform a similar function in pacemaker APs.
What we did emphasize was the role these channels play in keeping the membrane voltage
down once repolarization takes place. Inward currents have to overcome the outward currents
for depolarization to take place. If theres allot of outward current, this will be more difficult.
4.
After careful consideration I cannot determine why significantly decreased aortic pressure
will increase left ventricular stroke volume. This actually seems counter intuitive.
There are two potential ways to look at this. The first has to do with the concept of
afterload on the heart. There are actually 3 things which change cardiac output
The Cardiac Action Potential
though effects upon force of contraction: the inotropic state of the heart, the preload
and the afterload. Stroke volume increases with decreasing afterload on the heart
because the muscle itself is contracting against less pressure. This will be explained in
more depth in the CV lectures.
What actually happens is that the muscle contracts to a greater extent, emptying the ventricle to
a greater extent. The ventricle, being more empty at the beginning of diastole, fills less with
blood over the period of filling. This decreases the preload (the cardiac stretch) and the force of
contraction. This is why most data indicates that afterload has only a relatively minor effect on
stroke volume. Decreasing afterload does increase stroke volume and cardiac output but the
decreased preload limits that increase.
You dont need to know all that, yet, as it will be covered in detail in cardiovascular. The easy
answer is increased afterload -> decreased extent of contraction against the higher pressure ->
decreased stroke volume and vice versa.
5.
During the plateau (phase 2) of the action potential of ventricular cardiomyocytes:
a. the total membrane conductance is much larger than the membrane conductance at
the resting potential
b. L-type Ca2+ channels are gradually activating
c. the Na+/Ca2+ exchanger produces an inward current that helps sustain the membrane
potential near 0 mV
d. no delayed rectifier K+ channels have yet opened
e. inward rectifier K+ channels (IKdr) pass more current than when the membrane is at rest
The Na/Ca exchanger is important in phase 2, but are L-type Ca not also open at this time
to contribute to plateau? Answer is c.
The Ca channels open quickly during phase 1 and are gradually inactivating during phase
2. The better answer is c. See figure 4.8 in the syllabus.
6.
I just completed the first half of the practice midterm and noticed that there were quite a
few questions regarding "clinical correlations" from our syllabus. I am concerned about
this as I did not focus on those while doing the reading...will there be the same proportion
of those on the actual exam?
I will not consciously add any questions directly from clinical correlations unless it was
covered in the workshops. For instance, anything on the answer sheet from the long
QT workshop is fair game. I will look at the practice exam and if I find questions which
are found in the clinical correlations and nowhere else, they will be eliminated and I
thank you for bringing it to my attention.
If you find any on my exam on Wednesday, you have a legitimate complaint and you may bring
it to me to discuss it. Please be warned, however, that if it is something which you should have
been able to figure out from the regular material, I probably wont give the points. But it should
not be necessary for you to directly study these sections. For instance, I would never just
assume that you knew what a disease was from one of these sections and what causes it. But I
might introduce the disease as an example of physiology gone awry, give you all the information
you need, then expect you to figure out the answer to the problem. It wouldnt hurt to look at
these sections if you have the time but you should not under any circumstances need to know
them going in to answer my questions. You certainly should not concentrate on them.
7.
Which of the following currents increases in absolute amplitude as the membrane potential
hyperpolarizes from 0 mV to -70 mV:
a. open voltage gated Na+ channels
b. open L-type Ca2+ channels
The Cardiac Action Potential
c. open inward rectifier K+ (IK1) channels
d. open delayed rectifier K channels
e. all of the above except d
Could you please thoroughly explain answer e.
The current through an open channel gets bigger the further you get from its
equilibrium potential. So both a and b are correct.
c is correct because inward rectifiers are always open. The open channels simply
dont allow K to pass at high voltages. The current through any open IK1 channel is
very low at 0.
8.
I am having trouble understanding a particular aspect of hyperkalemia. I understand that
an elevated extracellular concentration of K+ will change the value of Ek as calculated by
the Nernst equation and therefore lead to a corresponding increase in the resting
membrane potential of the cell. What I do not understand, however, is how the increase in
the resting potential leads to less sodium channels being open. I thought that as the
membrane depolarized, sodium channels were more likely to be open, and that is what
lead to the rising phase of the action potential. Can you please explain where my
reasoning is going wrong?
A good, sharp, fast increase in Vm does, indeed, lead to more Na current. This is, of
course, how you get an action potential. You hit threshold when enough Na channels
open for the increase in voltage to be self-sustaining.
The problem is that were talking about the resting potential. Recall that the reason you get Na
current at all is because the activation gate opens very fast and the inactivation gate closes
more slowly. If you hold the voltage at a higher value, you allow inactivation gates to close and
they stay closed until you get back to the normal resting potential (which you wont do with
chronically high K outside). So when you have a higher resting potential, or even if you just
slowly increase the voltage instead of giving a sharp, fast depolarization, you effectively
decrease the available channels by inactivating them.
9.
I have a quick question about Cl regulatory channels in the heart...I know you mentioned
something about this in class but cannot seem to get it straight in my head. I am hoping
you can help me resolve my confusion!
Why is it that as membrane potentials are more negative than ECl, Cl leaves the cell and
this causes and INWARD current? Obviously, I have the same question when the situation
is reversed...when the membrane potential becomes more positive than ECl it causes Cl
to enter the cell and this causes and OUTWARD current?
The problem with currents is that you are actually counting charges, not molecules.
Cl- carries a negative charge. A negative charge going out is essentially the same as
a positive charge coming in. It is therefore a negative current
10.
2004 Midterm #71: The inotropic state (or contractility) of cardiac myocytes will be
increased if:" The answer is b) more Ca enters the myoplasm than usual during the
cardiac AP. I understand that, however, I wondered why
a) the muscle fiber is stretched to a longer length prior to contraction wouldn't be correct
too? On page 37 of the ANS workbook states: "Additional stretch leads to generation of
additional force. Thus if for whatever reason the heart fills with more blood than usual
(which stretches the muscles fibers more than usual), the force generated by the next
heartbeat will automatically be increased, resulting in increased ejection of blood."
The Cardiac Action Potential
The force of contraction is altered by 3 things. These are preload, afterload and
inotropic state. Stretching the muscle fiber increases the force of contraction (by
increasing preload). It does not, however, increase the inotropic state. Inotropic
state is a change in the force of contraction which is independent of changes in
length and afterload.
11.
I took the practice midterm for 2008 and on #73 there are some terms in the answer
choices that I was not familiar with (specifically, choice (d)). I looked in the syllabus (vol 2)
and these terms (calponin, caldesmon) are discussed under a section that apparently we
are not responsible for (You are not responsible for this still controversial section.)
Please refer to p. 43 in the smooth muscle section for reference. Should we expect other
surprises of the sort on the real exam tomorrow?? Please do let me know I am quite
worried.
If the information is not in the syllabus, you dont need it.
originates from a previous lecturer.
This is an old question, which
Dont panic. Trust me. You can make an appointment to talk to me about unfair questions the
week after the exam as you go over if you wish. But there should not be any.
The Cardiac Action Potential
PRACTICE MIDTERM EXAM QUESTIONS
These questions reflect the level of difficulty which you will find in many if not most of
the exam questions relevant to Dr. Shannons material. I have provided explanations for
the answers.
The next three questions (1, 2 & 3) refer to the figure below showing left ventricular pressure
(solid line) and aortic pressure (dashed line) as a function of time:
1.
Isovolumetric (or isovolumic) relaxation begins at time:
a.
A
b.
B
c.
C
d.
D
e.
E
2.
Blood is ejected from the left ventricle into the aorta during interval:
a.
b.
c.
d.
e.
3.
AB
BC
BD
BE
AE
The T wave of the electrocardiogram (ECG or EKG) normally begins during interval:
a.
b.
c.
d.
e.
AB
BC
CD
DE
EA
The Cardiac Action Potential
4.
Under normal conditions, the value of the cardiac output:
a.
b.
c.
d.
e.
5.
In the figure above, the period during which the rising phase of the action potential of
ventricular muscle cells will occur is represented by:
a.
b.
c.
d.
e.
6.
1
2
3
4
5
At NO TIME in the normal cardiac cycle are:
a.
b.
c.
d.
e.
7.
is directly proportional to heart rate (HR) if stroke volume is constant.
increases with increasing preload (greater end-diastolic ventricular volume, assume
constant HR).
increases with increasing afterload (high aortic pressure, assume constant HR).
a and b are correct.
a, b and c are correct.
all heart valves closed.
all heart valves open.
only the atrioventricular valves open.
only the semilunar valves closed.
only the atrioventricular valves closed.
Suppose that you know that the stroke volume (SV) of a patient has increased, but you do
not know what (if any) change has occurred in heart rate. Relative to the situation prior to
the increase in SV, what can you conclude with certainty?
a.
b.
c.
d.
e.
heart rate MUST have also increased
heart rate MUST have decreased
cardiac output MUST have increased
cardiac output MUST have remained the same
none of the above can be concluded with certainty
The Cardiac Action Potential
8.
The aortic semilunar valve opens:
a.
b.
c.
d.
e.
9.
A heart murmur can be caused by either a stenotic (narrow) valve or an insufficient (leaky)
valve. If you hear a murmur throughout most of SYSTOLE, it could be caused by?
a.
b.
c.
d.
e.
10.
P wave
QRS complex
T wave
QRS complex or T wave
P wave, QRS complex or T wave
Mutations in the genes encoding the Cl channel which decrease its conductance in cardiac
muscle would cause:
a.
b.
c.
d.
12.
a stenotic atrioventicular (AV) valve
an insufficient semilunar valve
a stenotic semilunar valve
a or b
a, b or c
Atrial fibrillation is characterized by rapid, irregular, uncoordinated depolarizations of the
atria. The ECG (or EKG) of a patient with atrial fibrillation will show no definite:
a.
b.
c.
d.
e.
11.
when the pressure in the left ventricle is greater than the pressure in the aorta
when the left atrium contracts
as soon as the left ventricle begins to contract
at the end of the period of isovolumetric (or isovolumic) relaxation
when the mitral valve closes
lengthening of the action potential plateau
shortening of the action potential plateau
a shift in the resting potential to slightly more negative values
a and c are true
Sympathetic stimulation of the heart has several different effects on cardiac muscle.
Which of the following is a correct list of some of these effects?
a.
b.
c.
d.
e.
increased heart rate, increased force of contraction and increased action potential
duration
decreased action potential duration and decreased duration of contraction
increased AV nodal delay and increased force of contraction
decreased AV nodal delay and decreased heart rate
none of the above are correct
The Cardiac Action Potential
13.
Normally the sinoatrial (SA) node is the pacemaker for the entire heart because:
a.
b.
c.
d.
e.
14.
The current through individual inward rectifier potassium channels (IK1) of cardiac muscle
cells:
a.
b.
c.
d.
e.
15.
decreases as the membrane potential becomes less negative than about -80 mV
increases as the membrane potential becomes less negative than about -80 mV
decreases as the membrane repolarizes at the end of the cardiac action potential
is larger during the plateau phase of the cardiac action potential than it is when
cardiomyocytes are at rest
b, c and d are all correct
The ECG of a patient with severe hyperkalemia ([K+]e = 10 mM) is likely to display (relative
to normal):
a.
b.
c.
d.
e.
16.
the SA node contains both 1 adrenergic receptors and M2 muscarinic receptors.
the SA node is the only site in the heart that will produce spontaneous action
potentials.
SA node cells have a smaller amount of Sarcoplasmic reticulum (SR) than other cells
in the heart.
the SA node is normally the only electrical connection between the atria and the
ventricles.
the SA node has a higher rate of spontaneous action potential generation than any
other location in the heart.
a shortened, but larger than normal, P wave
a prolonged QRS complex
no discernable T wave
a decreased PR interval
all of the above are correct
Shortly (with a period of a few hours or less) following a severe myocardial infarct to a
significant region of the left ventricle it is expected that:
a.
myocardial cells in the affected region will have reduced membrane permeability to K
b.
the activity of the Na+/Ca2+ exchanger will increase to help remove Ca2+ from the
myoplasm
the duration of action potentials and their propagation velocity in the affected region
will decrease
the contractile force of the affected region will increase because of increased
myoplasmic Ca2+ concentration
K+ concentration in the extracellular space surrounding cells in the affected
(ischemic) region will decrease
c.
d.
e.
The Cardiac Action Potential
17.
The channels underlying the cardiac action potential are often different in different
locations in the heart. Which of the following is a correct statement concerning the
distribution of ionic channels in the heart?
a.
b.
c.
d.
e.
18.
T-type Ca2+ channels are common in ventricular myocytes but are very rare in the
cells of the SA and AV nodes.
L-type Ca2+ channels are common in the cells of the SA and AV nodes but are
absent from ventricular and atrial myocytes.
Voltage-gated Na+ channels only occur in ventricular myocytes.
Inward rectifier potassium channels (IKl) only occur in cells of the SA and AV nodes.
None of the above are correct.
KATP channels are found in most cardiac muscle cells (as well as in some cells elsewhere
in the body). In heart these channels serve a cardioprotection function in ischemic
regions, but can also lead to dangerous arrhythmias. Of the following list of possible
characteristics, which correctly describe the KATP channel? KATP channels are:
1
2
3
4
5
6
a.
b.
c.
d.
e.
19.
mostly closed in normal cardiac muscle cells
mostly open in normal cardiac muscle cells
opened by increases in intracellular TP
opened by decreases in intracellular ATP
opened in cardiac cells that receive inadequate coronary blood supply
closed in cardiac cells that receive inadequate coronary blood supply
1, 4 and 5 are correct
2, 3 and 6 are correct
1, 3 and 5 are correct
1 and 3 only are correct
2 and 4 only are correct
A previously unknown toxin from a new strain of antibiotic resistant bacteria causes a large
and continuous elevation of the cAMP levels in cardiomyocytes but nowhere else in the
body. For an individual infected by this bacterium which of the following is/are expected?
a.
b.
c.
d.
e.
prolonged action potential duration in the atria and ventricles due to the facilitation of
L-type Ca2+ channels
decreased Ca2+ release from the SR due to resting inactivation of L-type Ca2+
channels
prolonged AV nodal delay due to resting inactivation of L-type Ca2+ channels
decreased action potential duration in the atria and ventricles due to the facilitation or
opening of K+ and Cl- channels
both b and c are correct
The Cardiac Action Potential
20.
At the sino-atrial (SA) node, parasympathetic nerves release ACh that bind to M2
muscarinic receptors in these cardiac cells. Which of the following is among the effects of
binding of ACh to these receptors?
a.
b.
c.
d.
e.
activation of G proteins which case the opening of K+ channels in CA nodal cell
membranes.
activation of G proteins which then activate adenylyl cyclase, producing incr5eased
cytoplasmic cAMP. cAMP activates protein kinase A, which phosphorylates Ca2+
channels in SA nodal cell membranes.
activation of G proteins which then activate phopholipase C, resulting in the
formation of IP3 and DAG, which activate K+ channels in SA node cell membranes.
opening of cation-selective pores in the receptors themselves; these pores allow
both Na+ and K+ to cross the SA nodal cell membrane.
activation of G proteins which ultimately cause Ca2+ to be released from the SR and
ER of SA nodal cells.
The Cardiac Action Potential
ANSWERS
1.
Answer = d.
Isovolumetric relaxation (also called isovolumic relaxation) of the left ventricle begins when the
aortic semilunar valve closes (point D, marked by the dicrotic notch). At this time the mitral
valve is, of course, closed since the left ventricular pressure is greater than the left atrial pressure.
Isovolumetric relaxation continues until the pressure in the left ventricle has fallen to a value less
than the pressure in the left atrium, when the mitral valve opens and filling of the left ventricle
begins.
2.
Answer = c.
Ejection of blood from the left ventricle starts when left ventricular pressure has risen
sufficiently to exceed the pressure in the aorta and open the semilunar valve; this occurs at time
B. Ejection ends at time D, and is associated with the dicrotic notch. Note that the onset of heart
sound 2 (not shown in the figure) arises from the closure of the semilunar valves and also marks
the end of ventricular ejection of blood.
3.
Answer = c.
See Figure 2.4 of the Heart lectures (page 24, Syllabus Volume 1). The T wave begins during
interval C-D, near or shortly after the time when the ventricular pressure has reached its peak.
Remember that the T wave represents the entire period when the muscle cells of the ventricle are
repolarizing; its total duration is typically somewhat more than 0.1 second. Also remember that
contraction of cardiac muscle cells continues for about 50 msec after the end of the cardiac
action potential.
4.
Answer = d.
Cardiac output (CO) depends directly on both heart rate (HR) and stroke volume (SV); recall that
CO = HR x SV. Stroke volume will increase with increasing preload (end diastolic ventricular
volume) due to the length-tension relationship of cardiac muscle. This is called Starlings Law
of the Heart. Increased afterload will decrease stroke volume and (with heart rate constant)
decrease cardiac output.
5.
Answer = b.
Period 2 contains the QRS complex. The QRS complex is the period when the action potential
spreads through the muscle cells of the ventricle, beginning as the action potential propagates
from the AV node into the bundle of His and ending with the depolarization of the cells at the
epicardial surface of the ventricles.
The Cardiac Action Potential
6.
Answer = b.
There is no time when all of the heart valves are open at the same time in the normal heart. When
the AV valves are open the pressure in the ventricles is low (ventricles are filling) and the
semilunar valves are closed. When the semilunar valves are open the pressure in the ventricle is
high (ventricular ejection of blood) and the AV valves are closed.
7.
Answer = e.
If you only know the value of SV, you can not el with certainty anything about the cardiac output
(CO), since cardiac output also depends on heart rate (remember: CO = HR x SV). Changes in
SV are not necessarily related to changes in heart rate.
8.
Answer = a.
The aortic semilunar valve will open as soon as the pressure in the left ventricle exceeds the
pressure in the aorta. Note that there is a delay between the beginning of contraction of the left
ventricle and the beginning of ejection of blood into the aorta. This is the period of isovolumic
(or isovolumetric) contraction.
9.
Answer = c.
During systole the pressure in the ventricles is high much higher than the pressure in the atria.
For most of this time the ventricles are ejecting blood (into the aorta from the left ventricle and
into the artery eon1 the right ventricle). A stenotic semilunar valve or an insufficient AV valve
will produce a murmur during systole. In the case of the stenotic semilunar valve the murmur
results from the narrowing of the valve which results in high velocity turbulent flow. For an
insufficient (leaky) AV valve a systolic murmur results from blood flowing back into the atrium
during systole producing turbulence (normally the Av value is closed during this period). Note
that a diastolic murmur could result from turbulent flow through either a stenotic AV valve or an
insufficient semilunar valve.
10.
Answer = a.
During atrial fibrillation there will be no definite P wave because the electrical (and contractile)
behavior of the atria is chaotic and asynchronized. The QRS complex and T wave should have
essentially normal shape, but ventricular contractions are likely to be irregularly spaced in time
(arrhythmia).
The Cardiac Action Potential
11.
Answer = d.
Cl has a reversal potential of approximately -55 mV in the cardiac cell. It therefore normally
pulls the voltage down during the plateau and more positive during rest. This effect is removed,
thus prolonging the plateau and making the resting potential more negative.
12.
Answer = b.
Sympathetic stimulation of the heart produces: 1) increased heart rate, 2) increased force of
contraction of the heart (increased contractility or inotropic state), 3) increased action potential
velocity through the Av node, and 4) decreased action potential duration (and thus decreased
duration of contraction). The decrease in duration of the action potential is brought about by
facilitation (due to phosphorylation) of the delayed rectifier K+ channel and the opening of
cAMP dependent Cl- channels. This effect is important when the heart rate is very high. Normal
heart rate is somewhat more than 1 beat per second; with the total duration of contraction of the
ventricle being roughly 300-350 msec. This leaves about 500-600 msec for diastole and the
filling of the ventricles. However, heart rate can reach at least 180 beats per minute (3 beats per
second). In this situation if the period of contraction remained the same there would be
essentially no time for diastole and no time for the ventricles to fill with blood. The decreased
duration of ventricular systole at very high heart rates allows time for diastole and the filling of
the ventricles.
13.
Answer = e.
While some of the other responses are correct descriptions of the SA node (e.g., response a),
response e is the reason that the SA node is the pacemaker for the entire heart. Normally the
rate of generation of spontaneous action potentials is high at the SA node than in any other
location in the heart. Remember, however, that other cells (e.g., AV node cells, Purkinje system
cells) also exhibit pacemaker activity but at a slower rate than the SA node.
14.
Answer = a.
The inward rectifier K+ channel (IKl) of cardiac muscle cells has a current voltage (I-V)
relationship that is illustrated in Figure 4.2 on page 77 of the Membrane Physiology notes.
Current through this channel type decreases as the membrane potential becomes less negative
than about -80 mV. Thus the current through these channels is less during the plateau than when
the membrane is at rest, and these channels pass more and more current as the membrane
repolarizes at the end of the action potential.
15.
Answer = b.
The Cardiac Action Potential
A patient with severe hyperkalemia ([K+]e = 10 mM) will have decreased action potential
propagation velocity in the heart and elsewhere. This is primarily due to resting inactivation of
voltage-gated Na+ channels due to membrane depolarization. This will result in a prolonged P
wave (and hence a prolonged PR interval, which is defined as the time from the start of the P
wave to the start or peak of the QRS complex) and a prolonged QRS complex. The T wave is
enlarged (peaked) by hyperkalemia.
The Cardiac Action Potential
16.
Answer = c.
Within a short time after the first signs of a severe myocardial infarct (MI) it is expected that O2
supply to the affected region will be severely reduced or eliminated. Since cardiomyocytes
depend almost exclusively on aerobic metabolish to produce ATP, the levels of ATP within the
cell will rapidly fall. This will reduce or eliminated the activity of the Na+/K+ pump and the Ca2+
pump. As the result of this the myoplasmic levels of both Na+ and Ca2+ will both rise; the rise in
Ca2+ concentration in the cytoplasm is contributed to by the decline in the activity of the Na+/
Ca2+ exchanger. Low ATP level open IK.ATP channels, increasing the membrane permeability to
K+ and eventually contributing to elevate extracellular K+ concentration. Elevated [K+]e causes
membrane depolarization which leads to resting inactivation of many (or all) Na+ channels. This
causes the duration and propagation velocity of action potentials in the affected regions to
decreases (answer c). Despite the increased myoplasmic Ca2+ concentration, the contractile force
in the affected region will decrease due to low levels of ATP.
17.
Answer = e.
T-type Ca2+ channels are common the cells of the SA node and AV node; they may also occur in
other cardiac cells, but they are of less importance in such cases. L-type Ca2+ channels and
inward rectifier K+ channels (IKl) occur in essentially all cardiomyocytes. Voltage-gated Na+
channels occur in the cells of the ventricles, atria and Purkinje fiber cells. This none of the
answers (a-d) are correct.
18.
Answer = a.
KATP channels in cardiac muscle are opened by low levels of intracellular ATP. Thus they are
mostly closed in normal cardiac muscle cells. They will open in cells in ischemic regions (i.e.,
regions that do not receive adequate coronary blood flow) because this will lead to decreased
AATP levels in the affected cells.
19.
Answer = d.
Under normal physiological conditions, increased cytoplasmic levels of cAMP in
cardiomyocytes result from the activation of 1-adrenergic receptors that are stimulation by the
sympathetic branch of the autonomic nervous system. There are many effects of increased levels
of cAMP (which lead to increased cytoplasmic levels of protein kinase A). Among these are the
facilitation of delayed rectifier K+ channels and the opening of cAMP-dependent Cl- channels.
Both of these channels (when activated) cause the action potential duration to decrease, since
they both strive to bring the membrane potential back toward it resting level. This overcomes
the facilitation of L-type Ca2+ channels (which, by itself would prolong the action potential). The
importance of shortening the action potential (particularly in the ventricles) should become clear
when you consider that increased sympathetic activity will lead to increased heart rate (up to 180
The Cardiac Action Potential
beats per minute) and that the heart must both eject blood and fill with blood in whatever time is
available between each heartbeat.
20.
Answer = a.
M2 muscarinic receptors in the membrane of SA nodal cells are activated by ACh released from
parasympathetic nerve terminals that innervate this region of the heart. An important effect of
parasympathetic activity is to decrease the heart rate. This is accomplished in part by the
following mechanism. Once the M2 muscarinic receptors have bound ACh, they activate G
proteins. The activated G proteins directly cause the opening of K+ channels in the membranes
of SA nodal cells. The K+ channels opened in the SA node membrane cause hyperpolarization
(moving the membrane potential further from threshold) and slow the rate of spontaneous
depolarization between action potentials. The result is that the rate of spontaneous action
potential generation by cells in the SA node is reduced. Remember that when ACh binds to M2
muscarinic receptors in the SA node membrane (and elsewhere in heart) the activated G protein
also has an inhibitory effect o adenylyl cyclase.
The Cardiac Action Potential
OLD EXAM QUESTIONS
These are actual questions from old exams. You should expect many, if not most, of the
questions on the block exam related to this material to be of a similar level of difficulty.
You should use these questions to study the material. If you dont know the answer, go
back and look it up. We generally do not test over material which we do not consider to
be important for you to know.
1.
Which of the following are effects of enhanced sympathetic activity to the heart:
a.
b.
c.
d.
e.
2.
Phase 0 of a normal ventricular action potential is caused by:
a.
b.
c.
d.
e.
3.
the opening of voltage-gated Ca2+ channels
the opening of inward rectifier (IK1) K+ channels
the activation of voltage-gated Na+ channels
the closing of pacemaker channels
the inactivation of delayed rectifier K+ channels
Long QT syndrome may result from a small portion of voltage-gated Na+ channels in the
heart failing to inactivate. Which of the following would be an ideal drug for blocking the
effects of Long QT syndrome in this case?
a.
b.
c.
d.
e.
4.
increased force of contraction
decreased myofilament sensitivity to Ca2+
decreased action potential duration
increased heart rate
all of the above are correct
a drug that completely blocked all Na+ channels
a drug which only blocks open Na+ channels (and unblocks when these channels
close) with a delay of a msec or so
a drug which blocks the L-type Ca channel
a drug which completely blocks inward rectifier (IK1) K+ channels
a drug that blocks open Na+ channels immediately and for a period of about 5-10
msec (and then unblocks these channels slowly as their activation gates close).
Blockage of a coronary artery supplying a significant portion of the left ventricle will:
a.
b.
c.
d.
e.
reduce the overall inotropic state of the heart
cause increases in myoplasmic Ca2+ concentration
cause increases in local extracellular K+ concentration
cause the opening of IK,ATP channels
all of the above are correct
The Cardiac Action Potential
5.
T-type Ca2+ channels in heart:
a.
b.
c.
d.
e.
6.
The K+ current through inward rectifier (IK1) K+ channels in ventricular myocytes is:
a.
b.
c.
d.
e.
7.
are responsible for setting the threshold potential of ventricular myocytes
are more common throughout the ventricles than L-type Ca2+ channels
provide the majority of current that initiates contraction in ventricular myocytes
open at more negative potentials than do L-type Ca2+ channels
both c and d are correct
smaller during the plateau than when the membrane is at rest
maximum during early phase 2
greater when the cell is in its plateau phase than when the cell is at rest
maximum during phase 1
unrelated to ventricular repolarization
During severe hyperkalemia the QRS complex of the ECG may be prolonged in duration
by as much as a factor of about 3 relative to its duration in the normal ECG. This is
primarily due to:
a.
b.
c.
d.
e.
complete inactivation of L-type Ca2+ channels
prolonged AV nodal delay
slowed propagation of the action potential through the ventricles
failure of the SA node to remain the pacemaker for the heart
decreased current through delayed rectifier Ca+ channels
===============================================================
For questions 21 and 22: Ventricular myocytes in hearts that are in chronic failure
typically have longer action potential plateaus.
8.
This could be due to:
a.
b.
c.
d.
e.
9.
more inactivated L-type Ca channels during the plateau (where Ca is being
transported inward)
a small, persistent inward (Na coming into the cell) Na current during the plateau
a higher outward (K going out of the cell) delayed rectifier K current during the
plateau
a higher outward IK1 (inward rectifier current) during the plateau
a, c & d are all correct
Assuming the heart rate is the same as a normal heart you would expect:
a.
b.
c.
d.
e.
ECl to rise, making it easier to depolarize the myocytes
ECl to fall, making it harder to depolarize the myocytes
ECl to always be at the resting potential
ECl to go up and down rapidly during each individual action potential, changing from
the resting potential to the action potential peak as the voltage rises and falls
none of the above
===============================================================
The Cardiac Action Potential
10.
Threshold potential for a typical ventricular myocyte is:
a.
b.
c.
d.
e.
11.
Which of the following will cause the greatest decrease in left ventricular stroke volume:
a.
b.
c.
d.
e.
12.
b.
c.
d.
e.
the left ventricle during diastole
the right ventricle during systole
the left atrium during systole
the right ventricle during diastole
the aorta during diastole
During DIASTOLE which of the following has the lowest pressure:
a.
b.
c.
d.
e.
16.
increased Ca2+ current across the surface and transverse tubule (T-tubule)
membrane during an action potential
phosphorylation of phospholamban causing increased rate of activity of the
sarcoplasmic reticulum (SR) Ca2+ pump
increased myofilament sensitivity to Ca2+
increased inotropic state
increased current through delayed rectifier K+ channels
Which of the following normally has the highest pressure:
a.
b.
c.
d.
e.
15.
both the aortic and the pulmonary semilunar valves are open
the aortic semilunar valve is closed but the pulmonary semilunar valve is open
both the mitral and the tricuspid valves are open
the tricuspid valve is open but the mitral valve is closed
both the mitral and tricuspid valves are closed
Which of the following is NOT a result of activation of -adrenergic receptors in heart:
a.
14.
decreasing the systolic aortic pressure from 140 to 120 mm Hg
decreasing the filling of the left ventricle by 40%
phosphorylating surface membrane Ca2+ channels
very slightly (<5%) decreasing the activity of the Na+/K+ pump
both a and b will have essentially equal effects
During most of the duration of ventricular diastole:
a.
b.
c.
d.
e.
13.
not a fixed membrane potential even in a particular cell or tissue.
dependent upon resting membrane permeability to K
dependent upon the number of Na channels available to open
all of the above are true
none of the above are true
the left ventricle
the left atrium
the pulmonary artery
the pulmonary veins
the aorta
Pressures developed by the right ventricle during systole are:
a.
much smaller than pressures developed by the left ventricle during systole
The Cardiac Action Potential
b.
c.
d.
e.
17.
If the cardiac output is 5.4 L/min, then which of the following value(s) for heart rate (HR, in
beats per minute) and stroke volume (SV in ml) is/are possible:
a.
b.
c.
d.
e.
18.
both electrically couple and mechanically bind neighboring cells together
electrically couple neighboring cells but do not mechanically bind the cells together
only function during the cardiac action potential (AP)
only function during ventricular diastole
increase in number over prolonged periods of elevated heart rate
The first heart sound normally begins:
a.
b.
c.
d.
e.
20.
HR
SV
70
70
72
75
108
50
85
60
either b or c are correct
The intercalated disc between cardiac muscle cells:
a.
b.
c.
d.
e.
19.
very close to the pressure developed in the pulmonary artery during systole
less than the pressure developed by the left atrium during systole
a and b only are correct
a, b and c are all correct
during the QRS complex of the ECG
at the start of the period of isovolumic (isovolumetric) contraction
during a period when there is no blood flow into the aorta from the left ventricle
a and b only are correct
a, b and c are all correct
Which of the following directly or indirectly contributes to the low myoplasmic Ca2+
concentration during diastole:
a.
b.
c.
d.
e.
the SR Ca2+ pump
the Na+/Ca2+ exchanger
the Na+/K+ pump
a and b only are correct
a, b and c are all correct
The Cardiac Action Potential
21.
The activity of which of the following channels is directly modulated by autonomic nervous
system (ANS) activity:
a.
b.
c.
d.
e.
22.
During phase 2 (the plateau) of the action potential of a ventricular action potential:
a.
b.
c.
d.
e.
23.
open voltage gated Na+ channels
open L-type Ca2+ channels
open inward rectifier K+(IKl) channels
open delayed rectifier K channels
all of the above except d
The rising phase of the sinoatrial (SA) nodal and atrioventricular (AV) modal action
potential is more gradual than that of the ventricular action potential because:
a.
b.
c.
d.
e.
25.
delayed rectifier K+ current is decreasing
current arising from the Na+/Ca2+ exchanger is mostly outward
current through inward rectifier K+ channels is less than when the membrane is at
rest
current through L-type Ca2+ channels is increasing
all of the above are correct
Which of the following currents increases in absolute amplitude as the membrane potential
hyperpolarizes from 0 mV to -70 mV:
a.
b.
c.
d.
e.
24.
Na+ channel
L-type Ca2+ channel
Pacemaker channel
b and c only are correct
a, b and c are all correct
there are essentially no voltage-gated Na+ channels in the SA or AV nodes
L-type Ca2+ channels open more gradually than voltage-gated Na+ channels
the density of L-type Ca2+ channels in SA and AV node is far lower than the density
of voltage-gated Na+ channels in ventricular myocytes
T-type Ca2+ channels also occur in low density in SA and AV node
all of the above contribute
If the T wave of the electrocardiogram (ECG or EKG) has a longer duration than normal
this indicates that:
a.
b.
c.
d.
e.
the repolarization of the ventricular action potential (AP) is more rapid than usual
the temporal and spatial repolarization of the ventricular AP is less uniform than
usual
the atrial AP repolarizes later than usual
the spread of depolarization through the ventricles MUST be abnormal
the direction of repolarization of the ventricle (e.g., base to apex or apex to base)
must be opposite than normal
The Cardiac Action Potential
26.
Pacemaker channels (If) are unusual relative to any other channels because:
a.
b.
c.
d.
e.
27.
Which of the following will increase left ventricular stroke volume:
a.
b.
c.
d.
e.
28.
the ventricles will stop beating
the ventricles will beat at a slower than normal rate
the atria will beat at a slower than normal rate
the atria will beat at the normal rate
both the atria and ventricles will beat at the normal rate
Blood flow into the aorta as it leaves the normal heart:
a.
b.
c.
d.
e.
30.
increased inotropic state (contractility)
increased filling of the left ventricle
decreased aortic pressure
a and b only are correct
a, b and are all correct
If the AV (atrioventricular) node is destroyed (e.g., by a localized myocardial infarct) then it
is expected that:
a.
b.
c.
d.
e.
29.
they open in response to membrane hyperpolarization
they allow both Na+ and K+ to cross the membrane
they only allow Ca2+ to cross the membrane
they cause membrane to hyperpolarize
both a and b are correct
begins at the start of the 1st heart sound
begins at the start of the QRS complex of the ECG
ends at the start of the T wave of the ECG
ends at the start of the 2nd heart sound
ends when the mitral valve opens
A patient is given a drug that causes reduced heart rate, decreased force of contraction in
the atria only, and increased AV nodal delay. This drug could have been:
a.
b.
c.
d.
e.
an M2 muscarinic agonist
an M2 muscarinic antagonist
a 1 adrenergic agonist
a 1 adrenergic antagonist
either a or d could have produced the effects described
The Cardiac Action Potential
The following diagram of the ECG of a normal subject is used in the next two questions (5 and
6). Five periods have been labeled (1-5).
31.
During which interval does isovolumic (isovolumeteric) contraction occur?
a.
b.
c.
d.
e.
32.
1
2
3
4
5
Repolarization of atrial myocytes occurs during period:
a.
b.
c.
d.
e.
1
2
3
4
5
===============================================================
33.
Cardiac glycosides inhibit the Na+/K+ pump. In cardiac muscle cells this leads to an
increase in the intracellular Na+ concentration. The effect of this on cardiac muscle is to:
a.
b.
c.
d.
e.
inhibit the SR Ca2+ pump leading to slower relaxation following the action potential
(AP), but more forceful contraction during the AP
stimulate the Na+/Ca2+ exchanger and thereby increase the influx of Ca2+ into the
myoplasm during the AP
inhibit the Na+/Ca2+ exchanger with the ultimate effect that the sarcoplasmic
reticulum (SR) stores and releases more Ca2+
inhibit the Na+/Ca2+ exchanger with the ultimate effect that inotropic state is reduced
stimulate the SR Ca2+ pump, thereby decreasing the duration of the AP
The Cardiac Action Potential
34.
If a patient has a cardiac output of 6.4 liters/min and a heart rate of 80 beats per minute,
then the patients stroke volume is:
a.
b.
c.
d.
e.
35.
In the initiation of contraction in normal cardiac muscle:
a.
b.
c.
d.
e.
36.
most of the Ca2+ that enters the myoplasm comes from the sarcoplasmic reticulum
(SR)
most of the Ca2+ that enters the myoplasm comes from the extracellular fluid via Ltype Ca2+ channels
essentially equal amounts of Ca2+ come from the extracellular fluid and from the SR
most of the Ca2+ enters the myoplasm via the Na+/ Ca2+ exchanger
Ca2+ only enters the myoplasm from the SR
A right bundle branch block (i.e., blockage of the large branch of the Purkinje fiber network
that goes to the right ventricle) will:
a.
b.
c.
d.
e.
37.
60 ml
70 ml
80 ml
86 ml
90 ml
cause the right ventricle to contract after the start of contraction in the left ventricle
produce a split 2nd heart sound
cause the P wave to be abnormal
a and b only are correct
a, b and c are all correct
A heart murmur produced by a stenotic or insufficient heart valve is a sound produced by
turbulent flow. A stenotic valve causes a murmur when it is open; an insufficient valve
causes a murmur when it should be closed. If a murmur is heard during ventricular systole
it could be caused by:
a.
b.
c.
d.
e.
a stenotic AV valve
an insufficient semilunar valve
a stenotic semilunar valve
a stenosis of both a semilunar valve and an AV valve is required to produce a
systolic murmur
either a or be can produce a systolic murmur
The Cardiac Action Potential
The following figure is used for the next 2 questions (12 and 13). The figure show left
ventricular pressure (solid line) and aortic pressure (dashed line) of a normal subject as a
function of time. 5 points in time (A, B, C, D and E) have been labeled.
38.
The aortic semilunar valve opens nearest in time to:
a.
b.
c.
d.
e.
39.
A
B
C
D
E
The period of time during which isovolumic relaxation occurs is best described by:
a.
b.
c.
d.
e.
A-B
B-C
B-D
D-E
E-A
===============================================================
40.
A patient with a severe aortic valve stenosis is expected to have:
a.
b.
c.
d.
e.
41.
A phosphodiesterase inhibitor will have which of the following effects on cardiac muscle
and smooth muscle:
a.
b.
c.
d.
e.
42.
elevated left ventricular systolic pressure
reduced aortic systolic pressure
reduced left ventricular systolic pressure
increased stroke volume
both a and b are correct.
Cardiac Muscle
Smooth Muscle
increased force of contraction
decreased force of contraction
decreased force of contraction
increased force of contraction
increased force of contraction
increased contraction
decreased contraction
increased contraction
decreased contraction
no change in force of contraction
Which of the following statements is/are true about a patient who had severe ischemia for
a period of 2 hours in a region of the felt ventricle:
The Cardiac Action Potential
a.
b.
c.
d.
e.
the extracellular K+ concentration is increased in the affected region
the resting potential of muscle cells in the affected region has become less negative
ATP-sensitive K+ channels (IK,ATP) are mostly open in the affected region
a and be only are correct
a, b and c are all correct
The Cardiac Action Potential
Answers
1. e
2. c
3. b
4. e
5. d
6. a
7. c
8. b
9. a
10. d
11. b
12. c
13. c
14. e
15. a
16. d
17. e
18. a
19. e
20. e
21. d
22. c
23. e
24. e
25. b
26. a
27. e
28. b
29. d
30. a
31. b
32. b
33. c
34. c
35. a
36. d
37. c
38. b
39. d
40. e
41. d
42. e
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Psychiatric HistoryDocument63 pagesPsychiatric HistoryStarlet Rhonadez Bito-onon Oriel0% (1)
- Body MeridianDocument65 pagesBody Meridiandcf67my100% (1)
- Ra Lightning Protection SystemDocument16 pagesRa Lightning Protection SystemamalNo ratings yet
- Siemens Mri Magnetom Mreadings Prostate PDFDocument100 pagesSiemens Mri Magnetom Mreadings Prostate PDFnanaa02No ratings yet
- Maternal and Child Health Nursing TestDocument21 pagesMaternal and Child Health Nursing TestAt Day's Ward50% (2)
- TableDocument6 pagesTablemanuNo ratings yet
- Case Study - 4 FractureDocument35 pagesCase Study - 4 FracturekavindukarunarathnaNo ratings yet
- Talasemia HemoglobinopatiDocument103 pagesTalasemia Hemoglobinopatisanti kristianiNo ratings yet
- Intrathecal Morphine Single DoseDocument25 pagesIntrathecal Morphine Single DoseVerghese GeorgeNo ratings yet
- Human Biology Laboratory 4: Body Tissues and Organization List The 4 Tissue Types and Give A General Function: Pg. 40Document4 pagesHuman Biology Laboratory 4: Body Tissues and Organization List The 4 Tissue Types and Give A General Function: Pg. 40bugyourselfNo ratings yet
- Informed ConsentDocument1 pageInformed Consentapi-107381417No ratings yet
- 95 Formulation and Evaluation of Diclofenac Sodium Gel by Using Natural PolymerDocument3 pages95 Formulation and Evaluation of Diclofenac Sodium Gel by Using Natural PolymerJulian Kayne100% (1)
- Moran CORE - How To Use The Direct OphthalmoscopeDocument1 pageMoran CORE - How To Use The Direct OphthalmoscopeSamsung M20APNo ratings yet
- Viagra Connect Checklist - 4 PDFDocument2 pagesViagra Connect Checklist - 4 PDFClarenceNo ratings yet
- WarfarinDocument2 pagesWarfarinWAHYU NOFANDARI HERDIYANTINo ratings yet
- Contract For External SupervisionDocument2 pagesContract For External SupervisionMarkTLFNo ratings yet
- Daftar Harga Pengujian Dan Kalibrasi Alat KesehatanDocument3 pagesDaftar Harga Pengujian Dan Kalibrasi Alat KesehatanVIDYA VIRA PAKSYA PUTRANo ratings yet
- Sds Methode LimitationsDocument8 pagesSds Methode LimitationsorinadeesfuerzoNo ratings yet
- Oral Wound Healing Efficacy of 1% Myristica Fragrans (Nutmeg) Determined Using MTT Assay: An in Vitro StudyDocument5 pagesOral Wound Healing Efficacy of 1% Myristica Fragrans (Nutmeg) Determined Using MTT Assay: An in Vitro StudyDeepthi ManjunathNo ratings yet
- Diagnostic Peritoneal Lavage (DPL)Document10 pagesDiagnostic Peritoneal Lavage (DPL)hatem alsrour100% (2)
- Graseby 3100 Syringe Pump - Service ManualDocument89 pagesGraseby 3100 Syringe Pump - Service ManualRamanjaneya goud100% (1)
- Physiology of The Pleural SpaceDocument78 pagesPhysiology of The Pleural SpaceAhmad RafiqiNo ratings yet
- Cesarean Surgical Techniques - GLOWMDocument36 pagesCesarean Surgical Techniques - GLOWMOana BalintNo ratings yet
- Order Denying NHL Motion To DismissDocument33 pagesOrder Denying NHL Motion To DismissNHL Concussion LawsuitNo ratings yet
- XareltofinalDocument2 pagesXareltofinalMuniba NasimNo ratings yet
- Screenshot 2564-04-16 at 09.45.04Document95 pagesScreenshot 2564-04-16 at 09.45.04Sarunpong ImampaiNo ratings yet
- Kosmetik BatalDocument5 pagesKosmetik BatalNurul AtikNo ratings yet
- 08 Chapter 3 Pyrazole AppDocument100 pages08 Chapter 3 Pyrazole AppSaima KhanNo ratings yet
- Introduction To Anatomy and Homeostasis Within The BodyDocument24 pagesIntroduction To Anatomy and Homeostasis Within The BodyTrinity SherNo ratings yet
- Nursing Care Plan Myocardia InfarctionDocument3 pagesNursing Care Plan Myocardia Infarctionaldrin1920No ratings yet