Professional Documents
Culture Documents
Digoxin
Uploaded by
Falaq2Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Digoxin
Uploaded by
Falaq2Copyright:
Available Formats
Digoxin
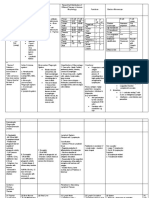
Pharmacokinetics
Digoxin can be given orally or intravenously. Th e
average volume of distribution is approximately
7.3 L/kg; this is decreased in patients with renal
disease, hypothyroidism and in patients taking quinidine.
It is increased in thyrotoxicosis. Clearance
varies from individual to individual and is the result
of both renal and metabolic elimination mechanisms.
In healthy adults, the metabolic component
is of the order of 4060 mL/min per 70 kg, and the
renal component approximates creatinine clearance.
Metabolic clearance is reduced in congestive cardiac
failure. Clearance in any individual can be calculated
by the equations discussed elsewhere (Chapter 1). In
patients with normal renal function, the elimination
half-life is approximately 2 days. Th is is increased to
approximately 46 days in severe renal disease.
Adverse effects
Adverse eff ects are determined in part by plasma
concentration (>2.5 g/L for digoxin) and in part by
electrolyte balance. Digoxin and potassium compete
for cardiac receptor sites and hypokalaemia can precipitate
digitalis adverse eff ects. Hypercalcaemia also
potentiates toxicity.
Th e common extracardiac adverse eff ects are anorexia,
nausea, diarrhoea, vomiting, fatigue or weakness.
Less commonly, neurological symptoms occur,
including diffi culty in reading, confusion or even
psychosis. Abdominal pain is another less common
manifestation.
Th e cardiac adverse eff ects may include depression
of automaticity or conduction resulting in sinus
bradycardia, sinus arrest, junctional rhythm or various
degrees of AV block, including complete heart
block. Additionally, digoxin may produce excitatory
eff ects, resulting in ventricular ectopic beats, atrial
or ventricular tachycardia, or ventricular fi brillation.
Th e typical eff ects of digitalis glycosides on the ECG,
i.e. prolonged PR interval and ST segment depression,
do not indicate toxicity. Cardiac signs precede
extracardiac signs in about 50% of cases of toxicity.
Drug interactions
Digoxin absorption is decreased by drugs that
increase intestinal motility (e.g. metoclopramide),
and increased by drugs that decrease motility (e.g.
propantheline). Many antacids, particularly magnesium
trisilicate, reduce digoxin absorption.
Digoxin levels increase if quinidine or amiodarone is
co-administered and toxicity can occur. Th e potential
for toxicity is enhanced for all cardiac glycosides
when diuretics are co-administered because of
hypokalaemia.
Clinical use and doses
Th e principal use of digoxin is in the control of ventricular
rate in atrial fi brillation, particularly when a
return to sinus rhythm is not expected (e.g. chronic
mitral valve disease). Combination therapy with
verapamil or beta-blockers provides better control of
exercise heart rate with a lower risk of toxicity than
high-dose digoxin. Th e onset of action even after
intravenous administration is delayed for several
hours. Th us if clinical circumstances require urgent
control of ventricular rate, other approaches such
as cardioversion or intravenous amiodarone may
be more appropriate. Acute digitalisation has been
superseded by the use of intravenous adenosine or
verapamil in the termination of supraventricular
tachycardias. Th e use of digoxin in patients with heart
failure in sinus rhythm is discussed elsewhere.
Th e dosing schedule used with digoxin depends
not only on its pharmacokinetic properties, but
also on factors that determine individual susceptibility.
Th e loading dose is determined by the
volume of distribution and the desired plasma
concentration; the maintenance dose by clearance
(Chapter 1). Nomograms and simple equations are
available for dose calculation. However, these must
remain approximations and the patients clinical
response must infl uence long-term management. If
a maintenance dose is employed without a loading
dose, drug accumulation and activity develop slowly
because steady state is not reached for four to fi ve
half-lives. Th e major determinant of digoxin clearance
is renal function and the maintenance dose
must be reduced if renal function is impaired. Th e
average loading dose of digoxin is 1.01.5 mg orally,
or 0.31.0 mg intravenously. Th e usual oral maintenance
dose in the presence of normal renal function
is 0.1250.250 mg/day.
Th e use of drug monitoring of digoxin plasma levels
has been useful, particularly in renal impairment
and toxicity. Th e normal therapeutic range of digoxin
is 12 g/L. Venous sampling should be performed
34 hours after an intravenous dose or 68 hours after
an oral dose. If blood levels are low then compliance
should be checked, and possible causes of malabsorption
considered.
You might also like
- Diagnosis and Treatment of Digoxin Toxicity: Review ArticleDocument3 pagesDiagnosis and Treatment of Digoxin Toxicity: Review ArticleJameela FayezNo ratings yet
- Diagnosis and Treatment of Digoxin Toxicity PDFDocument3 pagesDiagnosis and Treatment of Digoxin Toxicity PDFRozi AbdullahNo ratings yet
- DigoxinDocument6 pagesDigoxinZiedTrikiNo ratings yet
- Digoxin ElixirDocument8 pagesDigoxin ElixirUlfha NurhamidahNo ratings yet
- ConclusionDocument1 pageConclusionSamNo ratings yet
- Digoxin Monitoring and Toxicity ManagementDocument11 pagesDigoxin Monitoring and Toxicity ManagementWinsome Chloe Rara-BuñoNo ratings yet
- Faculty of Physical TherapyDocument15 pagesFaculty of Physical TherapyDr Abdallah BahaaNo ratings yet
- Cardiovascular Agents FarklinDocument66 pagesCardiovascular Agents FarklinBundo NaqueNo ratings yet
- Welcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinDocument16 pagesWelcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinUmair MazharNo ratings yet
- Digoxin PharmacokineticsDocument15 pagesDigoxin PharmacokineticsLama SaudNo ratings yet
- Meds DiabetesDocument5 pagesMeds DiabetesAnjangsari 'aRie' WijayantiNo ratings yet
- Lanoxin: (Digoxin) InjectionDocument35 pagesLanoxin: (Digoxin) InjectionZainNo ratings yet
- Digoxin Overdose: History & ExamDocument38 pagesDigoxin Overdose: History & ExamMicija CucuNo ratings yet
- Drug Information Questions - WK 4Document2 pagesDrug Information Questions - WK 4qzt5t6fwvgNo ratings yet
- Cardiovascular System Pharmacology: Pharmacology Ii DR E KeziaDocument15 pagesCardiovascular System Pharmacology: Pharmacology Ii DR E KeziaJohnNo ratings yet
- Lanoxin (Digoxin)Document3 pagesLanoxin (Digoxin)E100% (5)
- Drug Study On DigoxinDocument8 pagesDrug Study On DigoxinDonald BidenNo ratings yet
- 0006F PDFDocument13 pages0006F PDFreioctabianoNo ratings yet
- Digoxine PoisoningDocument4 pagesDigoxine PoisoningRanjith KumarNo ratings yet
- Obat Yang Bekerja Pada Sistem KardiovaskulerDocument18 pagesObat Yang Bekerja Pada Sistem KardiovaskulerMuhammad IkbalNo ratings yet
- CKD Dan DM (Modul 4)Document6 pagesCKD Dan DM (Modul 4)Nurul AwaliahNo ratings yet
- Drug Round - DigoxinDocument4 pagesDrug Round - DigoxinErvinaDamayantiNo ratings yet
- Digoxin Immune Therapy: ComplicationsDocument15 pagesDigoxin Immune Therapy: ComplicationsDaryl Jacob BigayNo ratings yet
- AH PharmaII v2Document35 pagesAH PharmaII v2bankai2992No ratings yet
- Product Name: New Zealand Data Sheet Apo-PrednisoneDocument13 pagesProduct Name: New Zealand Data Sheet Apo-PrednisonedomNo ratings yet
- Cardiac Glycosides Poisoning: by Rebeccah Barasa MBCHB Iv Umb/15-A/060 Moderator:Dr C.Wafula (Clinical Pharmacologist)Document23 pagesCardiac Glycosides Poisoning: by Rebeccah Barasa MBCHB Iv Umb/15-A/060 Moderator:Dr C.Wafula (Clinical Pharmacologist)Ahmed Ben BellaNo ratings yet
- Alternative Therapies For DM 2Document14 pagesAlternative Therapies For DM 2Ferc27No ratings yet
- Putri RamadhanDocument44 pagesPutri RamadhanRama MulyadiNo ratings yet
- Meglitinide Analogues Are Classified As Insulin Secretagogues and Have Actions andDocument6 pagesMeglitinide Analogues Are Classified As Insulin Secretagogues and Have Actions andRifqoh Aulia AlthofunnisaNo ratings yet
- Cardiac ArrhythmiaDocument101 pagesCardiac ArrhythmiaYuvraj ChauhanNo ratings yet
- USPI - Med Guide - Feldene - Piroxicam - CapsulesDocument15 pagesUSPI - Med Guide - Feldene - Piroxicam - CapsulesDini FarhatunnabilahNo ratings yet
- Digoxin ToxicityDocument25 pagesDigoxin ToxicitywasimNo ratings yet
- Theophylline.: BNF DrugsDocument2 pagesTheophylline.: BNF Drugsgege0% (1)
- Thiazolidinediones (NCBI) : Go ToDocument5 pagesThiazolidinediones (NCBI) : Go ToPatrick CommettantNo ratings yet
- Drugs Increased Risk of DiabetesDocument5 pagesDrugs Increased Risk of Diabetesk9cfxtdfqmNo ratings yet
- Practical Clinical Pharmacy II - Lab. 4Document6 pagesPractical Clinical Pharmacy II - Lab. 4Ali AbrahimNo ratings yet
- Approach ConsiderationsDocument12 pagesApproach ConsiderationsTyna Mew-mewNo ratings yet
- Glucocorticoid Withdrawal - UpToDateDocument7 pagesGlucocorticoid Withdrawal - UpToDateGiancarlos GuzmanNo ratings yet
- Pharmacological Management of Type 1 DiabetesDocument6 pagesPharmacological Management of Type 1 DiabetesMI RFNo ratings yet
- Drugs and Kidney DiseasesDocument46 pagesDrugs and Kidney Diseasesمرتضى محمد فاضل جرجوكNo ratings yet
- Aminoglycoside Notes by SDocument4 pagesAminoglycoside Notes by SSharan SahotaNo ratings yet
- Variability in Drug Dosage Requirements: Identify Knowledge GapsDocument3 pagesVariability in Drug Dosage Requirements: Identify Knowledge GapsAriyaniNo ratings yet
- Glucocorticoid Withdrawal PDFDocument9 pagesGlucocorticoid Withdrawal PDFSérgio HenriqueNo ratings yet
- Practical Diabetes International - November December 1996 - Dunning - Corticosteroid Medications and Diabetes MellitusDocument3 pagesPractical Diabetes International - November December 1996 - Dunning - Corticosteroid Medications and Diabetes MellitusAura DiscyacittaNo ratings yet
- Drug Prescribing in Renal Impairment Information. Patient PatientDocument13 pagesDrug Prescribing in Renal Impairment Information. Patient PatientEffy AngeLi LomocsoNo ratings yet
- Digoxin Concept MapDocument1 pageDigoxin Concept MapEmily Chiaravalloti100% (1)
- Dostinex: Prescribing InformationDocument9 pagesDostinex: Prescribing InformationasdwasdNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Screening: DM Tipe 1 Practice EssentialsDocument20 pagesScreening: DM Tipe 1 Practice Essentialskuchaibaru90No ratings yet
- LECTURE 9 Positive InotropicDocument5 pagesLECTURE 9 Positive InotropicanaNo ratings yet
- Diazoxide 50mg DatasheetDocument6 pagesDiazoxide 50mg DatasheetarifpharmjuNo ratings yet
- Sunitha - Drug InteractionsDocument49 pagesSunitha - Drug InteractionsSunitha Katta100% (1)
- Amlodipine-10mg TabletDocument7 pagesAmlodipine-10mg TabletMd. Abdur RahmanNo ratings yet
- Management of Diabetes Mellitus in Surgical PatientsDocument12 pagesManagement of Diabetes Mellitus in Surgical PatientsAnggoro Bayu Agung DjangkaruNo ratings yet
- DigoxinDocument1 pageDigoxinDedeoendutz Lovelly-brother SsiiCeueembemNo ratings yet
- Glycemia and Kidney RDocument27 pagesGlycemia and Kidney RMARIA VICTORIA VELARDE ALIAGANo ratings yet
- Metformin 1 METFORMIN (500mg, 850mg and 1000mg Tablets) : New Zealand Data SheetDocument11 pagesMetformin 1 METFORMIN (500mg, 850mg and 1000mg Tablets) : New Zealand Data SheetAfifa ZainNo ratings yet
- Digitalisanditstoxicity 150130110602 Conversion Gate02Document78 pagesDigitalisanditstoxicity 150130110602 Conversion Gate02Balaji BscRTNo ratings yet
- Geriatrics Department BookDocument69 pagesGeriatrics Department BookHazemAbu-BakrNo ratings yet
- Inhibitors of Viral NeuraminidaseDocument1 pageInhibitors of Viral NeuraminidaseFalaq2No ratings yet
- Inhibition of Intracellular Synthesis byDocument1 pageInhibition of Intracellular Synthesis byFalaq2No ratings yet
- Non-Nucleoside Reverse TranscriptaseDocument1 pageNon-Nucleoside Reverse TranscriptaseFalaq2No ratings yet
- A. Mechanism. (1) (2) B. Therapeutic Uses.: Arbs: Prototype Drug-ValsartanDocument1 pageA. Mechanism. (1) (2) B. Therapeutic Uses.: Arbs: Prototype Drug-ValsartanFalaq2No ratings yet
- Imiquimod, Podofilox, and SinecatechinsDocument1 pageImiquimod, Podofilox, and SinecatechinsFalaq2No ratings yet
- Treatment of TachyaarrhythmiaDocument1 pageTreatment of TachyaarrhythmiaFalaq2No ratings yet
- Synthetic Catecholamine: Dobutamine DobutamineDocument1 pageSynthetic Catecholamine: Dobutamine DobutamineFalaq2No ratings yet
- Vitamin K AntagonistsDocument1 pageVitamin K AntagonistsFalaq2No ratings yet
- Antiarrhythmic Drugs: Causes of ArrhythmiasDocument1 pageAntiarrhythmic Drugs: Causes of ArrhythmiasFalaq2No ratings yet
- Treatment of Tachyarrhythmias1Document1 pageTreatment of Tachyarrhythmias1Falaq2No ratings yet
- Fusion InhibitorsDocument1 pageFusion InhibitorsFalaq2No ratings yet
- SalicylatesDocument1 pageSalicylatesFalaq2No ratings yet
- ATova QuoneDocument1 pageATova QuoneFalaq2No ratings yet
- TerbinafineDocument1 pageTerbinafineFalaq2No ratings yet
- Direct Thrombin InhibitorsDocument1 pageDirect Thrombin InhibitorsFalaq2No ratings yet
- Phosphodiesterase InhibitorsDocument1 pagePhosphodiesterase InhibitorsFalaq2No ratings yet
- Adenosine Diphosphate InhibitorsDocument1 pageAdenosine Diphosphate InhibitorsFalaq2No ratings yet
- Heparins: Unfractionated HeparinDocument2 pagesHeparins: Unfractionated HeparinFalaq2No ratings yet
- MebendazoleDocument1 pageMebendazoleFalaq2No ratings yet
- GriseofulvinDocument1 pageGriseofulvinFalaq2No ratings yet
- Artemether and LumefantrineDocument1 pageArtemether and LumefantrineFalaq2No ratings yet
- Treatment Options For MycobacterialDocument2 pagesTreatment Options For MycobacterialFalaq2No ratings yet
- 13 - Digestive System - FullDocument29 pages13 - Digestive System - FullSamson Lee Yun ShenNo ratings yet
- TCM Acupoint TheoryDocument57 pagesTCM Acupoint Theorydishku100% (2)
- Failure of Weaning:: According To The European Respiratory Society (ERS) Task ForceDocument12 pagesFailure of Weaning:: According To The European Respiratory Society (ERS) Task ForceAmr El Taher0% (1)
- Ontogeny and Phylogeny of Immune SystemDocument3 pagesOntogeny and Phylogeny of Immune SystemPM Basiloy - AloNo ratings yet
- Isolation and Identification of Avibacterium Paragallinarum From Layer Chickens in Gazipur, BangladeshDocument3 pagesIsolation and Identification of Avibacterium Paragallinarum From Layer Chickens in Gazipur, BangladeshMd. Ehsanul Haque100% (1)
- Package Insert - Varivax (Refrigerator)Document14 pagesPackage Insert - Varivax (Refrigerator)Jose Eduardo Oliva MarinNo ratings yet
- Psychological Complication in PuerperiumDocument17 pagesPsychological Complication in Puerperiumbaby100% (2)
- Triage Assessment of Psychiatric Patient LectureDocument31 pagesTriage Assessment of Psychiatric Patient Lectureهشام عفانه100% (1)
- Case Study Endometrial PDFDocument17 pagesCase Study Endometrial PDFapi-279886264No ratings yet
- Research Revision Version 10 (Clean Copy)Document27 pagesResearch Revision Version 10 (Clean Copy)Nesty Perez IIINo ratings yet
- Community Nursing Care PlanDocument6 pagesCommunity Nursing Care Plantansincos93% (14)
- ISSN: 0975-833X: Case StudyDocument4 pagesISSN: 0975-833X: Case StudyantonNo ratings yet
- It Just Makes Sense 2012Document25 pagesIt Just Makes Sense 2012Emf RefugeeNo ratings yet
- Diarrhoea Patient InformationDocument3 pagesDiarrhoea Patient InformationIgor DemićNo ratings yet
- Hypernatremia From HarrisonDocument3 pagesHypernatremia From HarrisonNobel LaureateNo ratings yet
- Infectious DiseasesDocument4 pagesInfectious Diseasesapi-484776271No ratings yet
- SOAP Vs HOPSDocument2 pagesSOAP Vs HOPSJehiah HopeNo ratings yet
- Typhoid Fever: DR Bharat D. ZinjurkeDocument17 pagesTyphoid Fever: DR Bharat D. ZinjurkeDr Bharat ZinjurkeNo ratings yet
- Cerebral Palsy in ChildrenDocument7 pagesCerebral Palsy in ChildrenKelvin FundiNo ratings yet
- RADIOTHERAPHYDocument20 pagesRADIOTHERAPHYMuhammad Hafiz KarimNo ratings yet
- Functional Gastrointestinal Disorders History Pathophysiology Clinical Features and Rome IVDocument20 pagesFunctional Gastrointestinal Disorders History Pathophysiology Clinical Features and Rome IVwenyinriantoNo ratings yet
- LabReportNew - 2023-06-23T171149.608Document1 pageLabReportNew - 2023-06-23T171149.608B AZAD SIMHANo ratings yet
- Eye and Ears AssessmentDocument17 pagesEye and Ears AssessmentPrincess AñabezaNo ratings yet
- The Development of Science and Organ Donation - Abin AndrewsDocument4 pagesThe Development of Science and Organ Donation - Abin AndrewsABIN ANDREWS BNo ratings yet
- Name: - Ecol, Shenna C. - Date: - November 16, 2020 - Year/Section: BS-Criminology IIIDocument3 pagesName: - Ecol, Shenna C. - Date: - November 16, 2020 - Year/Section: BS-Criminology IIIJoenetha Ann ApariciNo ratings yet
- PPT-"Services and Benefits For Gulf War Veterans" - Anthony HardieDocument98 pagesPPT-"Services and Benefits For Gulf War Veterans" - Anthony HardieAnthony Hardie100% (5)
- Walking: The 'Wonder Drug': VocabularyDocument3 pagesWalking: The 'Wonder Drug': VocabularyLiveLaugh LoveNo ratings yet
- Malunggay Leaf ResearchDocument3 pagesMalunggay Leaf ResearchEj KasimNo ratings yet
- Regional AnesDocument36 pagesRegional AnesMay Anne BuenafeNo ratings yet
- Drug Study: Nursing DepartmentDocument2 pagesDrug Study: Nursing Departmentrica sebabillones100% (1)