Professional Documents
Culture Documents
Ulcerative Colitis
Uploaded by
pipotoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ulcerative Colitis
Uploaded by
pipotoCopyright:
Available Formats
ULCERATIVE COLITIS
Author: Dr Sandro Ardizzone1
Creation date: September 2003
Scientific Editor: Prof Gabriele Bianchi Porro
1
Chair of Gastroenterology , L. Sacco University – Hospital, Via GB Grassi, 74 20157 Milan, Italy.
samari1@tin.it
Abstract
Introduction
Epidemiology
Etiology
Pathophysiology
Symptoms, signs, and laboratory findings
Diagnostic methods
Differential diagnosis
Therapy
Prognosis
Surgery
References
Abstract
Ulcerative colitis (UC) is an inflammatory chronic disease primarily affecting the colonic mucosa; the
extent and severity of colon involvement are variable. In its most limited form it may be restricted to the
distal rectum, while in its most extended form the entire colon is involved. UC belongs to the inflammatory
bowel diseases (IBD), which is a general term for a group of chronic inflammatory disorders of unknown
etiology involving the gastrointestinal tract. UC is usually associated with recurrent attacks with complete
remission of symptoms in the interim. In Western Europe and in the USA, UC has an incidence of
approximately 6 to 8 cases per 100.000 populations and an estimated prevalence of approximately 70 to
150 per 100.000 populations. The leading initial symptom of UC is diarrhea with blood and mucus,
sometimes with pain. Fever and weight loss are less frequent. Extra intestinal symptoms can be an initial
manifestation or can occur later in the course of the disease. Eighty percent of the patients have only
proctitis or proctosigmoiditis, and only 20% have extensive colitis. However, in about 50% of patients with
initial proctosigmoiditis, proximal extension occurs later, and in some patients the opposite takes place.
Depending of the stage of the disease, endoscopy reveals reddening of the mucosa, increased
vulnerability, mucosal bleeding, irregular ulcers, pseudopolyps, granularity, and loss of vascular
architecture. Several drugs interacting with various points along the immune and inflammatory cascades
are currently available for the treatment of UC. Corticosteroids, aminosalicylates, immunomodulators are
the mainstay of medical treatment.
Keywords
Ulcerative colitis, inflammatory bowel diseases, colonic mucosa, gastrointestinal tract, proctitis,
proctosigmoiditis, corticosteroids, aminosalicylates, immunomodulators
Introduction manifestations often resulting in an
Inflammatory bowel disease (IBD) is a general unpredictable course.
term for a group of chronic inflammatory Ulcerative colitis is an inflammatory chronic
disorders of unknown etiology involving the disease primarily affecting the colonic mucosa;
gastrointestinal tract.Chronic IBD may be divided the extent and severity of colon involvement are
into two major groups, ulcerative colitis (UC) variable. In its most limited form it may be
and Crohn's disease (CD), clinically restricted to the distal rectum, while in its most
characterized by recurrent inflammatory extended form the entire colon is involved.
involvement of intestinal segments with several However, 80% of the patients present with
Ardizzone S. Ulcerative colitis. Orphanet encyclopedia. September 2003:
http://www.orpha.net/data/patho/GB/uk-UC.pdf 1
disease extending from the rectum to the splenic role of environmental factors in the appearance
flexure, and only 20% have pancolitis. and progression of CD and UC.
Although the causes of IBD remain unclear, The effect of cigarette smoking or the opposite
considerable progress has been made recently effect of this factor on the outcome of each form
in the identification of important pathophysiologic of IBD represents the most intriguing connection
mechanisms, and further and newer knowledge between environmental factors and IBD. Most
has been obtained from recent studies reports have shown that non-smoking is a
concerning their epidemiology, natural history, feature of patients with UC, whereas smoking is
diagnosis and treatment. a feature of patients with CD. Smoking is an
independent risk factor for clinical, surgical, and
endoscopic recurrence in CD but influences
Epidemiology disease activity after surgery. On the contrary,
Ulcerative colitis is usually associated with the relative risk of developing UC in heavy ex-
recurrent attacks with complete remission of smokers, all ex-smokers, non-smokers, and
symptoms in the interim. The disease is more smokers has been evaluated to be respectively
common in Caucasians than in Blacks or 4.4, 2.5, 1.0 and 0.6. Nicotine is probably the
Orientals with an increased incidence (three to main active ingredient in this association, but the
six fold) in Jewish. Both sexes are equally mechanisms remain unknown. Cigarette
affected. In Western Europe and in the USA, UC smoking has been shown to affect cellular and
has an incidence of approximately 6 to 8 cases humoral immunity, and increase colonic mucus
per 100.000 populations and an estimated production; both smoking and nicotine have
prevalence of approximately 70 to 150 per been shown to reduce colonic motility. Finally,
100.000 populations. While peak occurrence of results from in vivo studies have shown that
both diseases (UC and CD) is between ages 15 nicotine also has an inhibitory effect on T-helper-
and 35, it has been reported in every decade of 2 cell (Th2) function, which predominates in UC,
life. A familial incidence of IBD is currently but has no effect on Th-1 cells, predominant in
recorded. CD.
Epidemiological data indicate that non-steroidal
anti-inflammatory drugs can trigger
Etiology exacerbations of UC and even, occasionally,
The cause of UC is unknown. Although less induce de novo disease. Possible mechanisms
evident than in CD, it is clear from twin studies include decreased production of protective
that a genetic background is also present in UC. mucosal prostanoid and increased leukocyte
Indeed, a stronger association exists between adherence and migration. Although these effects
genes of the human leucocyte antigen region - were initially thought to be due to inhibition of
involved in regulating the immune response - cyclo-oxygenase-1 (COX-1), selective COX-2
and UC. Despite unclear effects due to ethnic inhibitors seem as potent as indomethacin in this
origin and disease heterogeneity, this context.
association is strongest in patients with Psychological stress by some 40% of patients
extensive UC; a positive association with DR2 with UC, has been reported to be a potential
(in particular, DRB1*1502 subtype) and the rare trigger. Substantial evidence links psychological
alleles DRB1*0103 and DRB1*12, and a stress with increased illness and, possibly,
negative association with DR4 and Drw6 have increased susceptibility to infection through
been reported. However, genes associated with stress-related impairment of functional immune
susceptibility to UC are probably not within the responses. Duration of stress might also be
human leucocyte antigen region, and genome- important since long-term but not short-term
wide scanning studies have shown a linkage stress seems to increase the risk of
between UC and regions of chromosomes 3, 7, exacerbations of disease.
and 12. Moreover, there are genes that appear Another very interesting environmental factor
to affect the severity and extent of the disease, conditioning UC is appendicectomy. Indeed,
steroid response, steroid requirements, and appendicectomy, at a young age, has the
extra - intestinal manifestations. Finally, strongest preventive effect on the development
polymorphisms of the IL-1 receptor antagonist of UC. This finding has been corroborated by
that might affect severity and extent of disease case-control studies, and a very large
have been reported, particularly in patients population-based study recently confirmed the
positive for pANCA, as well as for MUC3, a gene inverse relationship between appendicectomy
encoding intestinal mucins that might also be and UC in patients submitted to surgery before
associated with the pathogenesis of UC. age 20 years. In the latter study, the risk of UC
Among the many puzzles concerning IBD was reduced only in patients who underwent
etiology, one of the least understood and, appendicectomy for appendicitis or mesenteric
perhaps, most difficult to tackle, presently, is the
Ardizzone S. Ulcerative colitis. Orphanet encyclopedia. September 2003:
http://www.orpha.net/data/patho/GB/uk-UC.pdf 2
lymphadenitis, but not in those who underwent extension occurs later, and in some patients the
incidental appendicectomy or appendicectomy opposite takes place. A change in the extent of
for non-specific abdominal pain. This finding disease should be suspected when new
suggests that an inflammatory condition at a symptoms arise. The course of the disease can
young age that results in appendicectomy, rather vary widely. Spontaneous remission from a flare-
than appendicectomy itself protects against later up occurs in 20 to 50% of the patients, but 50 to
development of UC. Another possible 70% have a relapse during the first year after
explanation for this inverse association is that diagnosis.
genetic predisposition to UC might protect
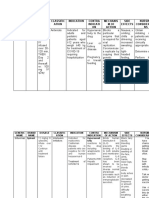
against development of appendicitis. Table1: Initial symptoms of UC
Diarrhea 96.4%
Pathophysiology Blood in stool 89.3%
While the cause of UC remains unknown, a Pain 81;3%
number of findings in recent years point to an Generally unwell 40.2%
over stimulation or inadequate regulation of the Weight loss 38.4%
mucosal immune system as a major Arthralgia 27.7%
pathophysiologic pathway, and particular Fever 20.5%
emphasis has been given to either the study of Skin changes 20.5%
mucosal inflammation or immunologic reactions. Loss of appetite 15.2%
When the disease is active, the lamina propria of Ophtalmopathies 7.1%
the mucosa becomes heavily infiltrated with a Nausea 6.3%
mixture of acute and chronic inflammatory cells. Vomiting 4.5%
There is a predominant increase in mucosal IgG Abscesses 3.6%
production, evidence of complement activation, Fistulae 3.6%
and activation of macrophages and T cells. This Lymphe node swelli 1.8%
immunological activity is associated with the
release of a vast array of cytokines, kinins,
leukotriens, platelet activating factor (PAF) and The relapse rate is higher in the younger
reactive oxygen metabolites. These mediators patients and seems to decrease with increasing
not only serve to amplify the immune and age. In a large cohort analysed over 25 years,
inflammatory response, but they also have direct 50% of the patients were able to work after 10
effects on epithelial function, on endothelial years.
function (which may increase permeability and
lead to ischaemia), and on repair mechanisms, Table 2: Frequency of extraintestinal
thus increasing collagen synthesis. In addition, manifestations of the course of UC
many of the cytokines (interleukins 1 and 6,
tumor necrosis factor) will activate an acute All 64-66%
phase response, resulting in fever and a rise in
serum acute phase proteins. Some of the clinical Skin 15.9%
features of acute ulcerative colitis may explain Erythema nodosum 8.0%
by these mechanisms. It follows, therefore, that Pyoderma gangrenosum 7.1%
any treatment which is able to inhibit the Aphtae 6.2%
activation of these immunological and
inflammatory effector mechanisms is likely to Eyes 9.7%
lead to an improvement in the patient’s Conjunctivitis 5.3%
symptoms and to a decrease in the inflammatory Iritis 4.4%
activity. Uveitis 0.9%
Symptoms, signs, and laboratory findings Joints 39%
The leading initial symptom of UC is diarrhea Arthralgia 38.4%
with blood and mucus, sometimes with pain Arthritis 11.3%
(Table 1). Fever and weight loss are less Ankylosing spondylitis 0.8%
frequent. Extra intestinal symptoms can be an
initial manifestation or can occur later in the Liver/pancreas 16.8%
course of the disease (Table 2). In proctitis, Fatty liver 10.6%
rarely, obstipation can be the initial symptom. Hepatitis 1.8%
Eighty percent of the patients have only proctitis Pericholangitis primary 3.5%
or proctosigmoiditis, and only 20% have Sclerosing cholangitis
extensive colitis. However, in about 50% of Pancreatitis 2.7%
patients with initial proctosigmoiditis, proximal
Ardizzone S. Ulcerative colitis. Orphanet encyclopedia. September 2003:
http://www.orpha.net/data/patho/GB/uk-UC.pdf 3
In all patients with severe UC an acute phase Differential diagnosis
response is present, including an elevated Diagnosis of UC should not be established
erythrocyte sedimentation rate, elevated C- before excluding a large number of intestinal
reactive protein level, microcytic anaemia, and, inflammatory disorders (Table 3).
less frequently, thrombocytosis. Until a few years
ago no specific laboratory abnormalities were Table 3: Differential diagnosis of IBD
known. More recently it has been found that
about 65% of patients with UC have positive Infections Invasive: Salmonella,
perinuclear antineutrophil cytoplasmatic (classic) Shigella, Campylobacter
antibodies (pANCA). These antibodies also species, Yersina
occur in almost all patients with primary enterocolitica, mycobacteria
sclerosing cholangitis. It is not clear whether Toxic: C. difficile, E. Coli
they have a pathophysiologic role, are Parasitic : Entamoeba H,
subclinical genetic markers, or are simply an Balantidium coli, Giardia l.
epiphenomenon. Sexual transmitted: Neisseria
gonorrheae, T. pallidum,
Diagnostic methods Herpes simplex, CMV, C.
Depending of the stage of the disease, thachomatis
endoscopy reveals reddening of the mucosa, Infections (new) Immunocompromised ( HIV)
increased vulnerability, mucosal bleeding, Histoplasma,CMV, M avium
irregular ulcers, pseudopolyps, granularity, and Vascuolar Ischemia, vasculitides,
loss of vascular architecture. The changes are Behcet disease
continuous, and the rectum is always involved if Malignant Lymphoma, sarcoma,
no effective local treatment has been applied. leukemias
Biopsy specimens show crypt irregularity, crypt Drug-induced Pseudomembranous, colitis,
abscess, and destruction of the epithelial border contraceptive-induced colitis,
in addition to immune cell migration. Histology is NSAID-induced colitis
however, not specific, and can be used only as a Others Radiation and chemically
supplementary diagnostic finding. induced colitis, collagenous
Abdominal transcutaneous ultrasonography may colitis, sarcoidosis
demonstrate bowel wall thickening of the
involved area, but it is non-specific. The same This can be achieved by microbiologic analysis
applies for computed tomography and magnetic of fecal samples and by biopsy analysis.
resonance imaging. Sometimes serologic analysis - for example, for
Since the advent of the endoscopy, double blind Yersinia enterocolitica - is helpful.
contrast barium enema is rarely used. It does,
however, show typical findings and can be Table 4: Differential diagnosis between CD
prescribed if endoscopy is not possible or is not and UC according to endoscopic findings
accepted by the patient.
Because inflammation in UC is limited to the
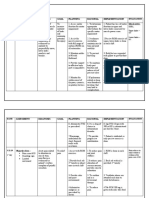
CD UC
colon, no imaging studies of the upper
gastrointestinal tract and small bowel are
Involvement Discontinous Continous
necessary once the diagnosis has been
Rectal 20% Always
established.
Involvement
Treatment options for extensive colitis are
Vessels Often Abnormal/lacking
different from those in distal colitis, and therefore
normal
the extent of the disease should be assessed.
Eryhthema/edema ++ +++
This best done by endoscopy with biopsy. Once
Vulnerability (+) +++
the extent of disease has been defined, repeat
Bleeding (+) +++
endoscopy is necessary only in the advent of
Pus/mucus + +++
new symptoms. However, after 10 years,
Local ulcers +++ (+)
endoscopy surveillance for carcinoma
Fissural ulcers +++ (+)
development should be considered.
Granularity (+) +++
Disease activity can be assessed clinically and
Clobbestone +++ ---
endoscopically. Since the rectum is invariably
pattern
involved, flexible rectosigmoidoscopy is
Pseudopolyps ++ +++
sufficient.
Strictures ++ (+)
It should be kept in mind that a flare-up of UC
can be induced by a microbial superinfection.
Ardizzone S. Ulcerative colitis. Orphanet encyclopedia. September 2003:
http://www.orpha.net/data/patho/GB/uk-UC.pdf 4
Thus, infection should be excluded before anemia, hypokalemia, hypocalcemia and
treatment is instituted. hypomagnesemia;
The differentiation between UC and CD can - structural abnormalities such as strictures and
usually be done using endoscopic, radiologic, perforations.
and histologic criteria (Table 4 and Table 5). In Priority of therapy is usually to control the
particular, continuous of the mucosal and rectal consequences of inflammation by transfusion,
involvements are critical to the diagnosis. replacement of losses, minerals, vitamins and so
on.
Table 5: Differential diagnosis between CD For a disease such as UC, characterized by
and UC according to histologic findings recurrent attacks of symptoms with complete or
partial remission of clinical manifestations, the
CD UC primary aims of medical treatment must be the
induction of remission of inflammatory activity
Crypt Injury ++ ++ and the prevention of recurrences. Moreover,
Granuloma ++ -- considering the frequent development of
Transmural inflammation +++ -- extraintestinal complications, often severely
Mucosal inflammation -- +++ affecting the patient’s quality of life, another
Lymphoid hyperplasia ++ -- important objective of the medical therapy is to
Deep ulcers ++ (+) control the impact of these complications on the
Microscopic focality +++ -- patient’s life.
Crypt abscess (+) +++
Globet cells depletion + +++
Flat ulcers (+) ++ Extent and anatomic distribution of UC
Establishing the extent and localization of UC is
Histologic differentiation without clinical an important diagnostic and clinical step in the
information is difficult and rarely used. Testing evaluation of patients suffering from UC,
for pANCA can be helpful, since a positive because of its therapeutic implications and
reaction is found in only 10% of patients with CD relative tolerability. Colonoscopy and radiology
but in 60 to 70% of those with UC. (barium enema) are the primary diagnostic tools
Biopsy specimens sometimes show typical used to define the extent and anatomic
findings. However, this is not always the case, distribution of the disease.
and the analysis of the same specimen by In UC, the extent of colon involvement during the
different pathologists may lead to different first attack has been found to be reasonably
results. uniform in several large series of patients. As
Involvement of the small bowel as seen at mentioned before, approximately 30% of UC
endoscopy or small bowel X-ray excludes UC, patients have disease that is limited to the
since the small bowel is not involved in this rectum, in about 40% the disease extends above
disease. the rectum but not beyond the hepatic flexure
(so-called sub-total colitis), and the remaining
Therapy 30% develop total colitis. However, in some
To reduce toxicity and maximize the therapeutic population-based surveys, more than half of the
benefit of the different drugs available for the patients present with disease extending from the
treatment of UC, thus improving their risk/benefit rectum to the splenic flexure. In this context,
ratio, several important criteria should be while UC may be classified into proctitis,
considered when choosing the most appropriate proctsigmoiditis, or left-sided colitis, the term
therapeutic approach: a) aims of the treatment; “distal colitis” is a working classification, which
b) extent and the localization of disease; c) implies that the inflammation is amenable to
disease activity; d) clinical pattern, and e) proven topical treatment, by means of intrarectal drug
efficacy of the current therapies. administration. Thus, giving pharmacological
therapy, this way may reduce potential
toxicity.Establishing the extent and localization of
Aims of therapy UC is an important diagnostic and clinical step in
The clinical status of a patient with active UC the evaluation
reflects many different factors:
- the primary disease process of gut
inflammation, confined to the mucosa in Grading of disease activity
ulcerative colitis; Disease activity indices are prediction rules
- metabolic consequences, such as protein- used to measure the activity of disease
losing enteropathy and hypoalbuminemia, objectively in order not only to judge response in
clinical trials, but also and especially to choose
which drug to administer and its optimal dose
Ardizzone S. Ulcerative colitis. Orphanet encyclopedia. September 2003:
http://www.orpha.net/data/patho/GB/uk-UC.pdf 5
regimen. However, the use of these indices in tumor necrosis factor, nicotine, heparin, etc.) but
clinical practice is limited, since they are their effectiveness needs to be established in
intended to make the clinical global assessment controlled clinical trials. In order to limit toxicity
objective, a prerogative most clinicians do not and optimize the therapeutic effects of the
agree with. current pharmaceutical treatment, thorough
In UC, the activity of the disease is usually understanding of the indications of drug therapy
assessed primarily on the basis of clinical is essential.
features. The Truelove and Witts classification in
mild, moderate or severe disease, based on the Practical guide to the management of UC
some clinical parameters and laboratory findings (see table 3)
(number of bowel movements, fever, presence Based on the data available, patients with mild to
of tachycardia, anemia, sedimentation rate) is moderate distal UC colitis may be treated with
the most widely used clinical activity index in either oral 5-ASA, topical 5-ASA, or topical
gastroenterological practice. However, although steroids. Patients refractory to all of the above
clinically useful, these criteria do not allow agents may require treatment with oral
sufficient discrimination for the purpose of prednisone in doses up to 40-60 mg/day. For
clinical studies. Expansion of the clinical profile maintenance of remission, 5-ASA suppositories
by Powell-Tuck et al has improved clinical trials or enemas are effective, as well as oral 5-ASA or
but lacks correlation with sigmoidoscopic sulfasalazine (SSZ), whereas topical
appearance. Sutherland et al have proposed a corticosteroids have not proven effective for
useful disease activity index for UC including a maintaining remission in distal UC.
grading of clinical and endoscopic signs (Table Patients with mild to moderate extensive UC
6). However, other clinical, endoscopical, and should begin therapy with oral SSZ or 5-ASA.
histological indices are available for grading Oral corticosteroids are generally useful for
disease activity in UC. patients who are refractory to oral 5-ASA with or
without topical therapy. 6-Mercaptopurine (6-MP)
Table 6: Ulcerative colitis disease activity or azathioprine (AZA) are effective for patients
index. who do not respond to oral prednisone but are
not so acutely ill as to require intravenous
1. Stool frequency 0-3: normal therapy. In these patients, when the acute attack
1-3: 1-2 stools daily > is controlled, a maintenance regimen is usually
normal required. SSZ or 5-ASA are effective in reducing
2-3: 3-4 stools relapses. As a rule, patients should not be
3-3: 4 stools treated chronically with corticosteroids. AZA or
6-MP may be useful as steroid-sparing agents
2. Rectal bleeding 0-3: None
for steroid-dependent and steroid-resistant
1-3: Streaks of blood
patients, and for maintenance of remission not
2-3: Obvious blood
adequately sustained by 5-ASA.
3-3: Mostly blood
Patients with severe UC refractory to maximal
3.Mucosal appearance 0-3: Normal
oral treatment with prednisone, oral salicylates,
1-3: Mild friability
and topical medications, or patients who present
2-3: Moderate friability
with toxicity, should be treated for 7-10 days with
3-3: Exudation,
intravenous corticosteroids. Failure to
spontaneous bleeding
demonstrate significant improvement within 7-10
4. Physician's rating of 1-3: Normal
days is an indication for either colectomy or
disease activity 2-3: Mild
treatment with intravenous cyclosporine A (Cy A)
3-3: Moderate
in specialized centers.
4-3: Severe
Maximum score 3 13
Complications
Drug classes Major complications of UC include toxic
Several drugs interacting with various points megacolon, intestinal perforation, mostly in the
along the immune and inflammatory cascades, setting of the toxic megacolon, and massive
are currently available for the treatment of UC. bleeding. Toxic megacolon is characterized by a
Corticosterid, sulfasalazine and its derivatives sepsis-like syndrome and extensive distension of
the 5-amino salicylic acids (5-ASA) and the colon (>6 cm). It usually appears later in the
immunosuppressants are the mainstay of course of the disease, but it can also occur early.
medical treatment. Effective in inducing Chronic blood loss leads to microcytic anemia,
remission, some of them are largely used to which may be severe. Drug-induced bone
prevent disease recurrence. Other drugs may marrow suppression and sulphasalazine-induced
also have a potential role in this context (anti- hemolytic or folate deficiency can cause anemia
Ardizzone S. Ulcerative colitis. Orphanet encyclopedia. September 2003:
http://www.orpha.net/data/patho/GB/uk-UC.pdf 6
as well. No other deficiency states have been relatively wide indication for colectomy have led
described, in contrast to CD. Severe to reduction of carcinoma risk.
extraintestinal complications or manifestations
include primary sclerosing cholangitis, and Prognosis
pyoderma gangenosum. An important problem is The prognosis for UC has improved significantly
the increased cancer risk in patients with long- over the past 60 years. This the result of an
standing and extensive colitis. The risk increases increased rate of colectomy and better timing of
statistically after 10 years in patients with surgery as well as of improved surgical
pancolitis, and to a lesser degree in those with knowledge of complications and a better
left-sided colits. Rarely, carcinoma can be the understanding of prophylaxis. The long-term
initial symptom in patients with unrecognized study of Copenaghen group showed that after 10
UC. years 25% of the patients had been colectomy;
Toxic or drug-induced megacolon can be treated 93% were able to work, and there was no
for up 3 days conservatively. High doses of increased carcinoma risk. Ten-year survival was
glucocorticoids in combination with total in the range of 96% of that of the normal
parenteral nutrition and antibiotics are used. If no population; it was better for those with proctitis
improvement occurs or the patients’s condition (98%) than for those with pancolitis (93%). The
deteriorates, immediate surgery is required. risk is particularly high for the rare patients who
Endoscopy and barium enema should not be develop UC later in life and initially present with
used because of the high risk of perforation. In a complication such as toxic megacolon. The
patients in whom toxic megacolon has been good long-term prognosis in the majority of
treated successfully, elective colectomy should patients requires that we focus on quality-of.life
be discussed, since this complication seems to aspects and on choosing treatment options with
carry an increased risk of recurrence. regard to all aspects of daily life and not only to
Severe refractory bleeding also must be treated medical outcomes.
by surgery; interventional endoscopic treatment
generally is not useful, since bleeding is diffuse
in almost all patients. For the indication of Surgery
surgical treatment of bleeding, the amount of In UC, three situations are absolute indications
daily necessary blood substitution and the time for surgery: exsanguinating hemorrhage, frank
to response on medical treatment must be perforation, and documented or strongly
known. suspected carcinoma, i.e., high grade dysplasia
There is no proven treatment of primary or low grade dysplasia in a mass lesion. Massive
slerosing cholangitis. The administration of hemorrhage in UC is due to diffuse mucosal
ursodeoxycholic acid may improve laboratory ulceration. If the hemorrhage is exsanguinating
values but does not seem to have any effect on or even persisting despite maximal medical
long-term prognosis. If extrahepatic duct therapy, it is an indication for surgical treatment.
stenosis occurs, this can be treated Perforation (occurring in only 2-3 % of
endoscopically. However, cholangiocarcinoma hospitalized UC patients at tertiary referral
must be considered. Liver transplantation is the centers), is the most lethal complication of toxic
final treatment of choice if liver function megacolon. When colon cancer is identified, the
deteriorates or recurrent complications of bile need for surgery is obvious; similarly, the
duct stenosis occur. coloscopic biopsy diagnosis of high grade
Pyoderma gangrenosum normally is treated with dysplasia is often indicative of a concomitant or
glucocorticoids, and in refractory cases other future cancer and is an indication for colectomy.
immunosuppressants such as azathioprine or Severe UC unresponsive to an intensive medical
cyclosporine are used. Most other extraintestinal regimen, or toxic megacolon, are others
manifestations react to improvement of disease indications for surgery.
activity in the colon and therefore are not treated
independently.
Surveillance for carcinoma development is References
widely used after 10 years of disease. The need
for surveillance is underscored by the fact that Ardizzone S, Bianchi Porro G. A practical guide
25% of strictures in patients with UC have been to the management of distal ulcerative colitis.
found to be malignant. However, it is not entirely Drugs,1998;55:519-42.
clear whether the current strategy of yearly Ardizzone S, Bianchi Porro G. Comparative
colonoscopy can indeed improve the outcome, tolerability of therapies for ulcewrative colitis.
though carcinoma-related mortality has been Drug Safety 2002;25:561-582.
reduced in some studies. Maintenance therapy
after remission, regular patients visits, and a
Ardizzone S. Ulcerative colitis. Orphanet encyclopedia. September 2003:
http://www.orpha.net/data/patho/GB/uk-UC.pdf 7
Ardizzone S, Bianchi Porro G. Inflammatory Nicholls RJ. Review article: ulcerative colitis--
bowel disease: new insights into pathogenesis surgical indications and treatment. Aliment
and treatment. J Intern Med 2002;252:475-496. Pharmacol Ther. 2002 Jul;16 Suppl 4:25-8
Ardizzone S, Molteni P, Bollani S, Bianchi Porro Powell-Tuck J, Brown RL, Lennard-Jones JE.
G. Guidelines for the treatment of ulcerative Acomparison of oral prednisone given as a
colitis in remission. Eur J Gastroenterol single or multiple daily doses for active proctitis.
1997;9:836-841. Scand J Gastroenterol 1978; 13 833-7
Blumberg D, Beck DE. Surgery for ulcerative Powell-Tuck J, Day Wbuckell NA, et al.
colitis. Gastroenterol Clin North Am. 2002 Correlation between defined sigmoidoscopic
Mar;31(1):219-35. appearances and other measures of disease
Eaden JA, Mayberry JF. Colorectal cancer activity in ulcerative colitis. Dig Dis Sci 1982; 27:
complicating ulcerative colitis: a review. 533-7
Am J Gastroenterol. 2000 Oct;95(10):2710- Schölmerich J, Herfarth C. Ulcerative colitis. In:
9.Evans S, Ciclitira PJ. Managing Crohn's Gastroenterology and Hepatology. Ed: G Bianchi
disease and ulcerative colitis. Practitioner. 1999 Porro. McGraw-Hill International (UK) Ltd.
Apr;243(1597):307 London 1999:381-393.
Farrell JR, Peppercorn MA. Ulcerative colitis. Sutherland L, MacDonald JK. Oral 5-
Lancet 2002;359:331-340. aminosalicylic acid for induction of remission in
Farrell RJ, Peppercorn MA. Ulcerative colitis. ulcerative colitis. Cochrane Database Syst Rev.
Lancet. 2002 Jan 26;359(9303):331-40. 2003;(3):CD000543.
Geboes K. Crohn's disease, ulcerative colitis or Sutherland L, Martin F, Greer S et al. 5-
indeterminate colitis--how important is it to Aminosalicylic acid enema in the treatment of
differentiate? Acta Gastroenterol Belg. 2001 Apr- distal ulcerative colitis, proctosigmoiditis and
Jun;64(2):197-200.Ghosh S, Shand A, proctitis. Gastroenterology 1987; 92 1894-8
Ferguson A. Ulcerative colitis. BMJ. 2000 Apr Rizzello F, Gionchetti P, Venturi A, Campieri M.
22;320(7242):1119-23.Gionchetti P, Amadini C, Review article: medical treatment of severe
Rizzello F, Venturi A, Campieri M. Review ulcerative colitis. Aliment Pharmacol Ther. 2003
article: treatment of mild to moderate ulcerative Jun;17 Suppl 2:7-10
colitis and pouchitis. Aliment Pharmacol Ther. Truelove SC, Witts LJ. Cortisone and
2002 Jul;16 Suppl 4:13-9. corticotropin in acute ulcerative colitis. BMJ
Greig E, Sandle GI. Diarrhea in ulcerative colitis. 1959; 2: 387-94
The role of altered colonic sodium transport. Truelove SC. Medical management of ulcerative
Ann N Y Acad Sci. 2000;915:327-32. colitis and indications for colectomy.
Gremse DA, Crissinger KD. Ulcerative colitis in World J Surg. 1988 Apr;12(2):142-7
children: medical management. Paediatr Drugs. Tuelove SC, Witts LJ. Cortisone in ulcerative
2002;4(12):807-15 colitis: a final report on therapeutic trials. BMJ
Guslandi M. Nicotine treatment for ulcerative 1955: 2: 1041-8
colitis. Br J Clin Pharmacol. 1999 Oct;48(4):481- Willoughby CP, Truelove SC. Ulcerative colitis
4. and pregnancy. Gut. 1980 Jun;21(6):469-74.
Hanauer SB. Update on medical management
of inflammatory bowel disease: ulcerative colitis.
Rev Gastroenterol Disord. 2001;1(4):169-76.
Katz JA, Pore G. Inflammatory bowel disease
and pregnancy. Inflamm Bowel Dis 2001;7:146-
157.
Langholz E. Ulcerative colitis. An
epidemiological study based on a regional
inception cohort, with special reference to
disease course and prognosis.
Dan Med Bull. 1999 Nov;46(5):400-15.Lee EC,
Truelove SC. Proctocolectomy for ulcerative
colitis. World J Surg. 1980;4(2):195-201.
Michell NP, Lalor P, Langman MJ. Heparin
therapy for ulcerative colitis? Effects and
mechanisms. Eur J Gastroenterol Hepatol. 2001
Apr;13(4):449-56.Miller M, Windsor A.
Ulcerative colitis. Hosp Med. 2000
Oct;61(10):698-702.
Ardizzone S. Ulcerative colitis. Orphanet encyclopedia. September 2003:
http://www.orpha.net/data/patho/GB/uk-UC.pdf 8
You might also like
- Heart Failure and CAD Case StudyDocument38 pagesHeart Failure and CAD Case StudyAbno NavarreteNo ratings yet
- Pug BookDocument152 pagesPug BookArtemio SotomayorNo ratings yet
- Comparison and Summary of Types of ArthritisDocument2 pagesComparison and Summary of Types of ArthritisShaz Chindhy50% (2)
- Acute Renal FailureDocument33 pagesAcute Renal FailureAqsa Akbar AliNo ratings yet
- Nursing Care Plan (COPD - IMBALANCE NUTRITION)Document2 pagesNursing Care Plan (COPD - IMBALANCE NUTRITION)Kathleen MartinezNo ratings yet
- Case 16 Pediatric t1dmDocument12 pagesCase 16 Pediatric t1dmapi-501730091No ratings yet
- Managing Nause and Vomiting-Crit-Care-Nurse-2003-Garrett-31-50 PDFDocument22 pagesManaging Nause and Vomiting-Crit-Care-Nurse-2003-Garrett-31-50 PDFpmuftiaNo ratings yet
- Wilms TumorDocument10 pagesWilms TumorRoscelie KhoNo ratings yet
- MCQ (Endocrine)Document7 pagesMCQ (Endocrine)aminata680% (5)
- CRH Radiology Policies and ProceduresDocument60 pagesCRH Radiology Policies and ProceduresAbdul Saeed Shah100% (1)
- ST - Lukes Casepress.Document31 pagesST - Lukes Casepress.Justin EduardoNo ratings yet
- Predisposing Conditions, Management and Prevention of Chronic Kidney DiseaseDocument52 pagesPredisposing Conditions, Management and Prevention of Chronic Kidney DiseaseSaad MotawéaNo ratings yet
- HemorrhoidsDocument15 pagesHemorrhoidspologroNo ratings yet
- Guide to Diagnosing and Treating CholecystitisDocument12 pagesGuide to Diagnosing and Treating CholecystitisMariela HuertaNo ratings yet
- Acute Abdominal Pain Case: AppendicitisDocument70 pagesAcute Abdominal Pain Case: AppendicitisVenny VeronicaNo ratings yet
- DVT Guide: Symptoms, Risks and TreatmentDocument9 pagesDVT Guide: Symptoms, Risks and TreatmentGladys YaresNo ratings yet
- Esophageal CancerDocument40 pagesEsophageal Cancerapi-282115150No ratings yet
- Multiple SclerosisDocument35 pagesMultiple SclerosisJc SeguiNo ratings yet
- Signs and Symptoms of Bowel ObstructionDocument6 pagesSigns and Symptoms of Bowel ObstructionKryza Dale Bunado BaticanNo ratings yet
- Diabetic KetoacidosisDocument4 pagesDiabetic KetoacidosisHasan A. AsFourNo ratings yet
- Pathophysiology of DiarrheaDocument3 pagesPathophysiology of DiarrheaFathur RahmatNo ratings yet
- Abdominal AssessmentDocument11 pagesAbdominal Assessmentasa100% (1)
- Pyelonephritis: Departemen Ilmu Penyakit Dalam FK Uii YogyakartaDocument33 pagesPyelonephritis: Departemen Ilmu Penyakit Dalam FK Uii YogyakartaAndaru Tri Setyo WibowoNo ratings yet
- Pediatric Appendicitis Clinical Presentation - History, Physical ExaminationDocument5 pagesPediatric Appendicitis Clinical Presentation - History, Physical ExaminationBayu Surya DanaNo ratings yet
- Angina PectorisDocument17 pagesAngina PectorisRacel HernandezNo ratings yet
- Acute Renal Failure: Dr. Bobi Ahmad S, S.KPDocument62 pagesAcute Renal Failure: Dr. Bobi Ahmad S, S.KPdr.Bobi Ahmad Sahid, S.KepNo ratings yet
- ConceptMap AMLDocument1 pageConceptMap AMLnursing concept mapsNo ratings yet
- Acute BronchitisDocument38 pagesAcute BronchitisNikko MelencionNo ratings yet
- Nursing Care PlansDocument16 pagesNursing Care PlansSantos Kyla Patricia T.No ratings yet
- LISTERIOSISDocument15 pagesLISTERIOSISCedric VillalbaNo ratings yet
- Day 2 - Ulcerative Colitis PDFDocument14 pagesDay 2 - Ulcerative Colitis PDFMaria Charis Anne IndananNo ratings yet
- Narratives Case NotesDocument4 pagesNarratives Case NotesKnigh RiderNo ratings yet
- MARCOS - Legal Issues of ElderlyDocument2 pagesMARCOS - Legal Issues of ElderlyArian May MarcosNo ratings yet
- Drug Study CovidDocument5 pagesDrug Study CovidR Hornilla Arcega0% (1)
- Mushtaq Ahmad: Running Head: REFLECTIVE LOG 1Document5 pagesMushtaq Ahmad: Running Head: REFLECTIVE LOG 1Shafiq Ur RahmanNo ratings yet
- Diabetes MellitusDocument44 pagesDiabetes MellituslkristinNo ratings yet
- Case Study For Chronic Renal FailureDocument6 pagesCase Study For Chronic Renal FailureGabbii CincoNo ratings yet
- Cystitis in Females Clinical Presentation - History, Physical Examination, Acute Urethritis Versus CystitisDocument6 pagesCystitis in Females Clinical Presentation - History, Physical Examination, Acute Urethritis Versus CystitisotakmesumNo ratings yet
- CellulitisDocument15 pagesCellulitisSujatha J JayabalNo ratings yet
- Cystic FibrosisDocument203 pagesCystic FibrosisAren SongcoNo ratings yet
- Whitening Injection Informed ConsentDocument3 pagesWhitening Injection Informed ConsentCalix Jr Rambuyon0% (1)
- Small Bowel ObstructionDocument2 pagesSmall Bowel ObstructionSrividya PushpalaNo ratings yet
- Diabetis MellitusDocument25 pagesDiabetis Mellituscdamasco18No ratings yet
- Pathophysiology of Acute CholecystitisDocument2 pagesPathophysiology of Acute CholecystitisKush KhannaNo ratings yet
- Case 052: Biliary ColicDocument4 pagesCase 052: Biliary ColicZauzaNo ratings yet
- Lesson Plan On Anemia: Register NoDocument16 pagesLesson Plan On Anemia: Register NoJyothi RameshNo ratings yet
- HydronephrosisDocument6 pagesHydronephrosisJamaluddin Ahmad A.MNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Goal Planning Rational Implementation Objective DataDocument8 pagesNursing Care Plan: Assessment Diagnosis Goal Planning Rational Implementation Objective DataMoonNo ratings yet
- Hepatic Encephalopathy: Prof. Huiling Yang Dept. PathophysiologyDocument46 pagesHepatic Encephalopathy: Prof. Huiling Yang Dept. PathophysiologyAshish PandeyNo ratings yet
- Nursing Care Plan for Fluid Volume DeficitDocument9 pagesNursing Care Plan for Fluid Volume DeficitGayu Patel0% (1)
- DM Case StudyDocument21 pagesDM Case StudyBern TolentinoNo ratings yet
- Nursing Care For Patients With HivDocument16 pagesNursing Care For Patients With HivAhmed HamedNo ratings yet
- Chronic Renal FailureDocument54 pagesChronic Renal Failuresanjivdas100% (3)
- Anal Canal: Fissure in Ano HaemorrhoidsDocument37 pagesAnal Canal: Fissure in Ano Haemorrhoidsyash shrivastavaNo ratings yet
- Kidney Stones: Causes, Symptoms and TreatmentDocument26 pagesKidney Stones: Causes, Symptoms and TreatmentPatrascu CristiNo ratings yet
- Nusing CareplanDocument3 pagesNusing Careplanardec_143No ratings yet
- Teaching Plan 7Document61 pagesTeaching Plan 7dinman_rituraj1683No ratings yet
- GBS Management, Medications and Nursing ConsiderationsDocument4 pagesGBS Management, Medications and Nursing Considerationssouledg3100% (1)
- Ulcerative Colitis: DR Syed Ubaid Associate Professor of SurgeryDocument71 pagesUlcerative Colitis: DR Syed Ubaid Associate Professor of SurgeryFachry Al RafiqiNo ratings yet
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Mucosa-Associated Bacteria in The Human Gastrointestinal Tract Are Uniformly Distributed Along The Colon and Differ From The Community Recovered From Feces.Document7 pagesMucosa-Associated Bacteria in The Human Gastrointestinal Tract Are Uniformly Distributed Along The Colon and Differ From The Community Recovered From Feces.pipotoNo ratings yet
- Development of The Human Infant Intestinal MicrobiotaDocument18 pagesDevelopment of The Human Infant Intestinal MicrobiotapipotoNo ratings yet
- Towards The Human Intestinal Microbiota Phylogenetic CoreDocument11 pagesTowards The Human Intestinal Microbiota Phylogenetic CorepipotoNo ratings yet
- IL10 Inhibits Cytokine Synthesis by Human MonocytesDocument12 pagesIL10 Inhibits Cytokine Synthesis by Human MonocytespipotoNo ratings yet
- Molecular Microbial Ecology of The Gastrointestinal-TractDocument19 pagesMolecular Microbial Ecology of The Gastrointestinal-TractpipotoNo ratings yet
- Aetiology of IBD - Role of Intestinal Microbiota and GALT Immune ResponseDocument14 pagesAetiology of IBD - Role of Intestinal Microbiota and GALT Immune ResponsepipotoNo ratings yet
- Colonic Bacterial Flora - Changing Understandings in The Molecular Age1Document6 pagesColonic Bacterial Flora - Changing Understandings in The Molecular Age1pipotoNo ratings yet
- Aetiology of IBD - Role of Intestinal Microbiota and GALT Immune ResponseDocument14 pagesAetiology of IBD - Role of Intestinal Microbiota and GALT Immune ResponsepipotoNo ratings yet
- Clinical Usefulness of Pro Bio Tics in IbdDocument11 pagesClinical Usefulness of Pro Bio Tics in IbdpipotoNo ratings yet
- Composition and Activity of Gut Microbiota in Inflammatory Bowel DiseaseDocument119 pagesComposition and Activity of Gut Microbiota in Inflammatory Bowel DiseasepipotoNo ratings yet
- Alterations in Intestinal Barrier Function Do Not Predispose To Trans Location of Enteric BacteriaDocument5 pagesAlterations in Intestinal Barrier Function Do Not Predispose To Trans Location of Enteric BacteriapipotoNo ratings yet
- Abnormal Fatty Acid Status in Patients With Crohn DiseaseDocument12 pagesAbnormal Fatty Acid Status in Patients With Crohn DiseasepipotoNo ratings yet
- Smart Health Prediction SystemDocument5 pagesSmart Health Prediction SystemInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Food For The BrainDocument34 pagesFood For The BrainKristine Mae AbrasaldoNo ratings yet
- 5388 Tech ManualDocument198 pages5388 Tech ManualMichal SzymanskiNo ratings yet
- Nursing Care Plan Neonatal PneumoniaDocument2 pagesNursing Care Plan Neonatal Pneumoniaderic93% (41)
- E Book Coffee Leaf TeaDocument18 pagesE Book Coffee Leaf TeaAsun ArceNo ratings yet
- IPDocument35 pagesIPxxsunflowerxxNo ratings yet
- Turkish Angora CatDocument6 pagesTurkish Angora CatprosvetiteljNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaAlmira PutriNo ratings yet
- Hiv Awareness Project ProposalDocument17 pagesHiv Awareness Project ProposalPrincess Gesa Macula100% (1)
- Kelas 3Document5 pagesKelas 3RojNo ratings yet
- Family Case Study For HydrocephalusDocument9 pagesFamily Case Study For HydrocephalusjaegergranNo ratings yet
- Effectiveness of 6 Step Prevention and Control For Dengue Hemorrhagic Fever in Rural Community of ThailandDocument142 pagesEffectiveness of 6 Step Prevention and Control For Dengue Hemorrhagic Fever in Rural Community of ThailandMendoza Alech ChelaNo ratings yet
- Physiology of Sleep: Michael Schupp MD FRCA Christopher D Hanning MD FRCADocument6 pagesPhysiology of Sleep: Michael Schupp MD FRCA Christopher D Hanning MD FRCArichie_ciandraNo ratings yet
- Imaging of Nasopharyngeal CarcinomaDocument9 pagesImaging of Nasopharyngeal CarcinomayohanasmjtNo ratings yet
- Sas 1# - CHNDocument16 pagesSas 1# - CHNZymer Lee Perez AbasoloNo ratings yet
- Olive Leaf and Cordy CepsDocument14 pagesOlive Leaf and Cordy CepsHakeem Zamano100% (2)
- Cystic HygromaDocument12 pagesCystic Hygromaraymond onyekaNo ratings yet
- IAS CSAT Question Paper 2011 (General Studies IIDocument76 pagesIAS CSAT Question Paper 2011 (General Studies IIAadil AnsariNo ratings yet
- Ranula: A Review of LiteratureDocument6 pagesRanula: A Review of LiteratureNicco MarantsonNo ratings yet
- Test-11 (Current Affair-2)Document86 pagesTest-11 (Current Affair-2)Pavansaikumar DasariNo ratings yet
- Case Scenario: Self-Risk AssessmentDocument2 pagesCase Scenario: Self-Risk AssessmentAlyanna Alcazar CapateNo ratings yet
- Adhd SD 550 Graphic Organizer 3 PDFDocument4 pagesAdhd SD 550 Graphic Organizer 3 PDFapi-534368950No ratings yet
- Sermon On Spirituality & Mental Illness by Rev Laura MancusoDocument12 pagesSermon On Spirituality & Mental Illness by Rev Laura MancusoRev. Laura L. MancusoNo ratings yet
- Acute and Chronic PyelonephritisDocument7 pagesAcute and Chronic PyelonephritisMatthew Ryan100% (1)
- Diploma of Otolaryngology Head & Neck Surgery Course: St. Mary's Hospital LondonDocument16 pagesDiploma of Otolaryngology Head & Neck Surgery Course: St. Mary's Hospital LondonTamer Alseiry0% (1)
- Elevated LDL Triglycerides and Atherosclerotic Risk: BackgroundDocument17 pagesElevated LDL Triglycerides and Atherosclerotic Risk: BackgroundRoxana MariaNo ratings yet