Professional Documents
Culture Documents
PCR Technique Detection of Leishmania Spp. But Not Mycobacterium Spp. in Canine Cutaneous Sterile' Pyogranuloma - Granuloma Syndro
Uploaded by
jenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PCR Technique Detection of Leishmania Spp. But Not Mycobacterium Spp. in Canine Cutaneous Sterile' Pyogranuloma - Granuloma Syndro
Uploaded by
jenCopyright:
Available Formats
Veterinary Dermatology 2005, 16, 233238
PCR technique detection of Leishmania spp. but not
Mycobacterium spp. in canine cutaneous sterile pyogranuloma/
granuloma syndrome
Blackwell Publishing, Ltd.
L. CORNEGLIANI*, D. FONDEVILA, A. VERCELLI*, G. MANTERO and A. FONDATI
*Ambulatorio Veterinario Associato, Corso Traiano 99/d, Torino, Italy
Universitat Autnoma de Barcelona, Facultat de Veterinria, Bellaterra, Barcelona, Spain
Biodiversity, via Corf 71, Brescia, Italy
(Received 2 April 2004; accepted 30 July 2004)
Abstract Cutaneous sterile pyogranuloma/granuloma syndrome (SPGS) is an uncommon canine skin
disorder of unknown aetiopathogenesis. Histopathological findings and failure to demonstrate an aetiologic
agent are suggestive of this syndrome. Nevertheless, it has been hypothesized that SPGS may be related to
an immune response against persistent endogenous or exogenous antigens. The presence of Leishmania and
Mycobacterium organisms was investigated by polymerase chain reaction (PCR) techniques in 46 canine
skin samples histopathologically diagnosed as SPGS. Concomitantly, an immunohistochemical technique
for Leishmania detection was applied on the same samples and the results were compared with those from
PCR. The PCR technique yielded positive results for Leishmania spp. in 21 out of 46 skin samples. The
results of immunohistochemical techniques were identical to those obtained by PCR. The PCR technique
gave negative results for Mycobacterium spp. in all the samples examined. These results suggest the importance
of looking for Leishmania spp. in skin biopsies with histopathological findings consistent with the diagnosis
of SPGS.
I N TRO D U C T ION
Cutaneous sterile pyogranuloma/granuloma syndrome
(SPGS) is an idiopathic canine skin disorder, characterized
clinically by nodules or plaques and histopathologically
by multifocal, nodular to diffuse, pyogranulomatous/
granulomatous dermal infiltrate.1,2 Early histopathological appearance is represented by elongated, vertically
orientated periadnexal pyogranulomas /granulomas. In
later stages, the inflammatory infiltrate coalesces into a
more diffuse infiltrate.3,4 Diagnosis of SPGS is based
on clinical appearance, histopathological findings, lack
of microorganisms visualized with special stains (PAS,
Ziehl-Neelsen and Gram), failure to demonstrate
foreign bodies by polarized light microscopy examination, and negative microbiological examination of tissue cultures.3,4 The aetiology of SPGS is currently
unknown; however, it has been hypothesized that
SPGS may be related to an immune response against
persistent endogenous or exogenous antigens, causing
a granulomatous inflammatory reaction.3,5
The cutaneous histopathological findings in canine
leishmaniosis (CL) may mimic those of SPGS and, if
only small numbers of amastigotes are present, the
This project was supported by a grant from SIDEV (Societ Italiana
di Dermatologia Veterinaria).
Correspondence: L. Cornegliani, Ambulatorio Veterinario Associato,
Corso Traiano 99/d, 10135 Torino, Italy. E-mail: gigiami@tin.it
2005 European Society of Veterinary Dermatology
histopathological differential diagnosis between the
two diseases may be difficult.6,7 In such cases, immunohistochemical and /or polymerase chain reaction (PCR)
techniques are required to rule out definitively the
presence of Leishmania organisms.811 Based on the
authors personal observations, Leishmania organisms
can be detected by immunohistochemical techniques
on skin biopsies with histological lesions suggestive of
SPGS, in which no microorganisms are visible either
on haematoxylin and eosin (H&E) or on specially
stained sections.
Similarly, canine leproid granuloma syndrome can
be characterized by a granulomatous/pyogranulomatous dermatitis1214 and, in some cases, special stains,
such as ZiehlNeelsen, may be negative even in the
presence of microorganisms, which can usually be
detected by tissue PCR.11,15 Interestingly, in humans,
mycobacteria and other microorganisms have been
detected by PCR in granulomatous diseases classically
reported as sterile, such as sarcoidosis.16,17
Leishmania and Mycobacterium organisms may represent, among others, a possible source of persistent
exogenous antigens in cases of canine SPGS. For these
reasons, the present study was designed to investigate
the presence of Leishmania spp. and Mycobacterium
spp. by means of PCR in canine skin samples diagnosed histopathologically as SPGS. This study also
evaluated the effectiveness of the PCR technique in
detecting Leishmania organisms in comparison with
the immunohistochemical technique.
233
234
L Cornegliani et al.
MATERIALS AND ME T HODS
Sample selection
Forty-six formalin-fixed, paraffin-embedded skin
biopsies were collected from 46 dogs: 32 through
the Diagnostic Pathology Service of the Veterinary
Faculty of Barcelona (Universitt Autnoma de
Barcelona, UAB, Bellaterra, Spain) and 14 through the
Pathology Service of Ambulatorio Veterinario Associato (AVA, Turin, Italy). All samples showed histological lesions suggestive of SPGS, namely multifocal,
nodular to diffuse, periadnexal and perifollicular
pyogranulomas/granulomas, in which neither microorganisms nor foreign bodies were detected by H&E
and special stains (PAS, ZiehlNeelsen and Gram) and
by polarized light examination, respectively.
Both immunohistochemical and PCR techniques
were performed on all the samples to detect the presence of Leishmania organisms,911,18,19 while the PCR
technique was applied to detect Mycobacterium spp.20,21
Immunohistochemical technique to detect
Leishmania organisms
Sections were deparaffinized, rehydrated and incubated in 3% hydrogen peroxide (H2O2). Sections were
then washed with tris buffer solution (TBS). Enzyme
digestion with 0.1% trypsin in CaCl2 solution was performed for 5 min at 37 C. Samples were rinsed with
TBS and then incubated with normal goat serum for
1 h at room temperature. Serum was removed and
rabbit polyclonal antileishmania antibody (1 : 1000)
(kindly donated by Dr Domnguez, CSIC, Madrid,
Spain) was added. Samples were incubated for 1824 h
at 4 C and subsequently washed with TBS. A biotinylated antirabbit antibody (Dako Corp., Glostrup,
Denmark) (1 : 400) was added and sections were incubated for 1 h at room temperature. After two 5-min
rinses in TBS, tissue sections were incubated with
avidin-biotin complex (ABC) (Vector Laboratories,
Burlingame, CA, USA) (1 : 100) for 1 h at room
temperature and then washed with TBS. The sections
were then incubated with the chromogen, 3,3-diaminobenzidine tetrahydrochloride (Sigma Chemical Co.,
St Louis, MO, USA), 0.035% in TBS in the presence of
hydrogen peroxide, rinsed in tap water, counterstained
with Mayers haematoxylin, dehydrated and mounted.
and SP177 (5-TTGACCCCCAACCACATTTTA-3 )
were used to amplify a 120-base-pair fragment of
Leishmania kinetoplast DNA minicircles. PCR was
carried out in a 50-L final reaction mixture containing
PCR buffer, 2.5 m MgCl2, 0.2 mL of dNTP, 0.5 of
each primer, 3 L of supernatants of proteinase-digested
tissues, and 1.25 U of Taq polymerase. The reactions
were carried out in an automated thermocycler and
25 L of PCR products (amplified fragments) were
analysed by 2.5% agarose gel electrophoresis at 50 V
for 90 min. After electrophoresis, the gel was stained in
a 0.5 g/mL ethidium bromine solution for 20 min and
visualized with ultraviolet light. Visible fluorescence
indicated positivity.
Molecular biology technique (PCR) to detect
Mycobacterium spp.
The extraction was conducted using a commercial kit
(Ampliquality, MYC-TE, AB Analitica srl, Padua,
Italy). Sections were deparaffinized, dried and resuspended in 200 L of tissue digestion solution containing 20 L of proteinase K and 10 L of lysozyme.
Samples were incubated overnight in a shaking incubator at 50 C. After centrifugation samples were added
to 400 L of binding solution and 100 L of resin
and transferred to a column for centrifugation. The
extract was washed and resuspended into 80 L of
DNAse-free water. Five microlitres of purified DNA
were used for the nested PCR amplification of a 16S
rRNA fragment. External primers (FO16S 5GATAAGCCTGGGAAACTGGGTC-3, RO16S 5TTCTCCACCTACCGTCAATCCG-3) amplifying a
fragment of 344 bp were added to the PCR mixture
containing 3 m MgCl2, 200 of each dNTP, 0.4
of each primer, 3 L of the supernatant of proteinasedigested tissue, 0.5 U of Taq polymerase and buffer B
(Promega Corporation, Wisconsin-Madison, USA)
with 500 m KCl, 100 m Tris-HCl pH 9.0 at 25 C,
and Triton (Sigma) X-100 to a final volume of 50 L.
The reactions were cycled in a thermocycler and 1 L
of the product was added as template for the second
round with the internal primers (F116S 5-CATGTCTTGTGGTGGAAAGCG-3; RI16S 5-TACCGTCAATCCGAGAGAACCC-3) under the same
conditions as the first reaction. The amplified 288-bp
fragment was visualized by ultraviolet light on 1.5%
agarose gel, using a 100 bp DNA ladder as a marker.
Molecular biology technique (PCR) to detect
Leishmania spp. organisms
Sections were deparaffinized, dried and resuspended in
tissue digestion solution, consisting of 14 L proteinase K in 1 mL of digestion buffer (59 m Tris-HCl
pH 8.5, 1 m ethylenediaminetetraacetic acid, 0.5%
[w/v] Tween 20). Resuspended tissue sections were left
overnight in Eppendorf tubes in a shaking water bath
at 37 C. Subsequent incubation of samples for 10 min
at 95 C inactivated protease K. After centrifugation, the
supernatant was subjected to PCR for DNA amplification
and detection. Leishmania spp.-specific oligonucleotide
primers SP176 (5-TCTTGCGGGGAGGGGGTG-3 )
R E SU LT S
On histopathological examination, 23 samples were
characterized by a periadnexal inflammatory infiltrate,
which was pyogranulomatous in 15 and granulomatous
in eight cases, respectively. In the other 23 samples, a
nodular to diffuse inflammatory dermal hypodermal
infiltrate was observed. Seventeen of these samples
were pyogranulomatous and six granulomatous.
Immunohistochemistry for Leishmania spp. was positive in 21 of the 46 biopsies and PCR technique gave
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 233238
PCR detection of Leishmania
235
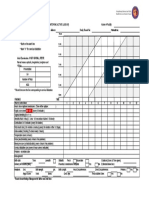
Figure 1. PCR for detection of Leishmania organisms: lines from 1
to 4 represent a group of positive PCR obtained from skin samples.
Lane 5 is negative and lines 6 and 7 are the controls.
Figure 3. Photomicrograph of the same nodular skin lesion showing
few amastigotes of Leishmania (arrows) within macrophages
(indirect immunoperoxidase stain; bar = 25 m).
Figure 2. Photomicrograph of a nodular skin lesion showing an
inflammatory infiltrate with macrophages, lymphocytes, plasma cells
and rare neutrophils. Infectious agents cannot be identified
(haematoxylin and eosin stain; bar = 100 m).
the same results (Fig. 1). Dark brown stained intracellular Leishmania amastigotes were detected in 13/
32 specimens, characterized by a pyogranulomatous
inflammatory infiltrate, and in 8/14 samples with a
granulomatous inflammatory reaction (Figs 2 and 3).
Detection of Mycobacterium spp. by PCR was negative
in all 46 samples.
D ISCU SSION
The results of the present study show that, both in Italy
and in Spain, Leishmania organisms, but not Mycobacterium organisms, are commonly encountered in
canine skin biopsies with histopathological findings
suggestive of SPGS. This raises an important diagnostic
issue on the choice of laboratory tests and their limitations. A diagnosis of SPGS is achieved by a process of
elimination.1 4,22 Methods used include examination
of bacteriological and mycological cultures from fresh
tissue samples.14,23 In the present study, detection of
microorganisms through culture examination was not
possible, as this was a retrospective study conducted
solely on samples in paraffin blocks. To eliminate this
diagnostic limitation, special stains are applied to
histological sections consistent with SPGS to detect
microorganisms that can not be seen by standard H&E
staining. The concomitant use of polarized light microscopy aids in ruling out the presence of foreign bodies
(granulomatous reaction due to vegetable, organic,
mineral and other materials). If the aetiological agent
is present in small quantities, it may remain undetected
by these methods.14
In recent years, in an attempt to deal with these diagnostic limitations, methods used in both veterinary
and human medicine have included those based on the
detection of microorganism DNA and antigens.10,11,1521
The use of PCR has allowed investigators to identify
pathogens in lesions that were diagnosed previously as
sterile. Some authors of the present study have noted
through personal observations that some apparently
sterile granulomas are actually positive for Leishmania
spp. when using immunohistochemical methods
(immunoperoxidase, IP) to detect this protozoan. In
the present study the biopsies, which were IP positive
for Leishmania, were also PCR positive. These data
allow us to draw multiple conclusions.
First, both methods gave identical results. As it is a
highly sensitive and specific technique, PCR, according to
some authors, is superior to immunohistochemistry.10,11
The greater sensitivity of PCR is due to the ability to
amplify DNA of microorganisms, thus enabling detection
in more cases. It has been suggested that PCR should
be applied to all samples where immunohistochemistry
gives uncertain or negative results. In the present study
there was no difference in sensitivity between the techniques, and the methods were comparable.10
Second, biopsies negative for microorganisms on
microscopic examination may actually contain them.
This is important with regard to Leishmania organisms
in granulomatous skin lesions with histopathological
features suggestive of SPGS. The samples were selected
from institutions operating in areas endemic for leishmaniosis. The presence of granulomatous histological
lesions does not necessarily mean that these lesions are
related to Leishmania, as the protozoan could reach
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 233238
236
L Cornegliani et al.
the sites in already infected macrophages attracted
during the inflammatory process.8,25 Based on our
present data, it is impossible to state whether the histological lesion of SPGS is subsequent to the protozoan
presence. This question may be answered by complete
physical examination, haematological, biochemical
and serological testing of dogs and evaluation of their
response to therapy. Detection of high anti-Leishmania
antibody titres might be useful to differentiate between
infected and ill dogs.26 An animal in which Leishmania
organisms are observed in tissue sections does not necessarily have or develop the disease.8,26 A prospective
study is required to understand the significance of the
protozoan. However, given the differences in treatment
between SPGS and leishmaniosis,2,6,8 PCR should be
applied to detect Leishmania amastigotes in all histological samples with the histopathologic diagnosis of
SPGS in areas endemic for the disease.
Because SPGS is a disease diagnosed by a process of
elimination, and given the similarities with other granulomatous diseases associated with mycobacteria, the
possible presence of these microorganisms requires
investigation. In both animals and humans, mycobacterial diseases may be difficult to diagnose. In humans,
diseases that were diagnosed as sterile and now proved
to be secondary to the presence of microorganisms
include sarcoidosis.17 This has some histological similarities with SPGS.2729 In recent years, PCR has
permitted identification of the presence of DNA of
Mycobacterium spp. in histological samples where
both examination of bacterial and fungal cultures of
fresh tissue and staining of paraffinized tissue were
negative for microorganisms.17,28,30 Even granulomas
of canine leproid syndrome can be negative for the
presence of mycobacteria. This disease is clinically
similar to SPGS due to the localization of nodules on
head and limbs and the lack of systemic signs of illness
in affected dogs.14 The histopathological pattern is
more similar to tuberculous granulomatous lesions,
though in some cases the number of microorganisms is
small, the lesion can be histologically compared to
SPGS.7,14,31,32 In these cases, application of PCR for
Mycobacterium spp. is essential for a correct diagnosis.14,31
In the present study, PCR for mycobacteria was negative in all biopsies. The negative results could have
been secondary to the scarcity of microbial DNA. This
possibility could be addressed by using a larger number
of histological paraffinized sections to extract and
amplify DNA or rRNA sequences. The second possible cause of negative results is the wrong specificity of
the primers. However, the 16S rRNA used is common
to all mycobacteria.30 The same technique was
repeated and compared with samples whose positivity
was already shown by special stains and the technique
confirmed the presence of mycobacteria. The results
are therefore unlikely to be negative as a consequence
of laboratory errors.30
All samples were collected in areas that are not
endemic for mycobacterial disease, so this could
explain the negativity. The lack of clinical data about
the animals does not allow us to make further comment. It would be interesting to apply this method
to samples diagnosed as SPGS in areas considered
endemic for mycobacterial disease.14
In conclusion, the use of PCR to detect microorganisms in SPGS could lead to interesting results about the
aetiology of this disease and others, which are currently considered idiopathic or sterile.
AC K N OW L E D G E M E N T S
The authors wish to thank Isabella Taboni and Alessandra Tosini for performing the molecular biology
techniques and Dr Chiara Noli for her critical review
of the manuscript.
REFERENCES
1. Torres SMF. Sterile nodular dermatitis in dogs. Veterinary Clinics of North America 1999; 29: 131123.
2. Scott DW, Miller WJ, Griffin GE. Miscellaneous skin
diseases. In: Muller and Kirks Small Animal Dermatology. Philadelphia: W.B. Saunders, 2001: 113640.
3. Gross TL, Ihrke PJ, Walder EJ. Non-infectious nodular
and diffuse granulomatous and pyogranulomatous diseases of the dermis. In: Veterinary Dermatopathology: a
Macroscopic and Microscopic Evaluation of Canine and
Feline Skin Diseases. St Louis, MO: Mosby Year Book,
1992: 1948.
4. Yager JA, Wilcock BP. Nodular and/or diffuse pyogranulomatous dermatitis. In: Color Atlas and Text of Surgical
Pathology of the Dog and Cat. St Louis, MO: Mosby
Year Book, 1994: 1413.
5. DeManuelle TC, Stannard AA. Difficult dermatologic
diagnosis. Sterile nodular panniculitis. Journal of the
American Veterinary Medical Association 1998; 213:
3567.
6. Scott DW, Miller WJ, Griffin GE. Viral, rickettsial, and
protozoal skin diseases. In: Muller and Kirks Small
Animal Dermatology. Philadelphia: W.B. Saunders,
2001: 5348.
7. Gross TL, Ihrke PJ, Walder EJ. Infectious nodular and
diffuse granulomatous and pyogranulomatous diseases
of the dermis. In: Veterinary Dermatopathology: a
Macroscopic and Microscopic Evaluation of Canine and
Feline Skin Diseases. St Louis, MO: Mosby Year Book,
1992: 16971, 1868.
8. Font A, Roura X, Fondevila D et al. Canine mucosal
leishmaniasis. Journal of the American Animal Hospital
Association 1996; 32: 1317.
9. Ferrer L, Rabanal RM, Domingo M et al. Identification
of Leishmania donovani amastigotes in canine tissues by
immunoperoxidase staining. Research in Veterinary Science 1988; 44: 1946.
10. Roura X, Fondevila D, Snchez A et al. Detection of
Leishmania infection in paraffin-embedded skin biopsies
of dogs using polymerase chain reaction. Journal of Veterinary Diagnostic Investigation 1999; 11: 3857.
11. Roura X, Sanchez A, Ferrer L. Diagnosis of canine leishmaniasis by polymerase chain reaction technique. Veterinary Record 1999; 144: 2624.
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 233238
PCR detection of Leishmania
12. Scott DW, Miller WJ, Griffin GE. Bacterial skin diseases. In: Muller and Kirks Small Animal Dermatology.
Philadelphia: W.B. Saunders, 2001: 316 19.
13. Yager JA, Wilcock BP, Panniculitis. In: Color Atlas and
Text of Surgical Pathology of the Dog and Cat. St Louis,
MO: Mosby Year Book, 1994: 204 5.
14. Foley JE, Borjesson D, Gross TL et al. Clinical, microscopic, and molecular aspects of canine leproid granuloma in the United States. Veterinary Pathology 2002;
39: 234 9.
15. Aranaz A, Libana E, Pickering X et al. Use of polymerase chain reaction in the diagnosis of tuberculosis in cats
and dogs. Veterinary Record 1996; 138: 276 80.
16. Drake WP, Pei Z, Pride DT et al. Molecular analysis of
sarcoidosis tissues for Mycobacterium species DNA.
Emerging Infectious Diseases 2002; 8: 1334 41.
17. Hsiao PF, Tzen CY, Chen HC et al. Polymerase chain
reaction based detection of Mycobacterium tuberculosis
tissues showing granulomatous inflammation without
demonstrable acid-fast bacilli. International Journal of
Dermatology 2003; 42: 281 6.
18. Brecelj M, Pikelj F, Gubensek F et al. Polymerase chain
reaction as a diagnostic tool for detecting Leishmania.
Infection 2000; 28: 11113.
19. Muller N, Zimmermann V, Foster U et al. PCR-based
detection of canine Leishmania infections in formalinfixed and paraffin-embedded skin biopsies: elaboration
of a protocol for quality assessment of the diagnostic
amplification reaction. Veterinary Parasitology 2003;
114: 22339.
20. Osaki M, Adachi H, Gomyo Y et al. Detection of mycobacterial DNA in formalin-fixed, paraffin-embedded
tissue specimens by duplexpolymerase chain reaction:
application to histopathologic diagnosis. Modern
Pathology 1997; 10: 7883.
21. Ikonomopoulos JA, Gorgoulis VG, Zacharatos PV et al.
Multiplex polymerase chain reaction for the detection of
mycobacterial DNA in cases of tuberculosis and sarcoidosis. Modern Pathology 1999; 12: 854 62.
237
22. Ihrke PJ, White SD. Difficult dermatologic diagnosis.
Journal of the American Veterinary Medical Association
1998; 213: 3567.
23. Panich R, Scott DW, Miller WH. Canine cutaneous sterile
pyogranuloma/granuloma syndrome: a retrospective
analysis of 29 cases (19761988). Journal of the American Animal Hospital Association 1999; 7: 51928.
24. Houston DM, Clarck EG, Matwichuk CL et al. A case
of cutaneous sterile pyogranuloma/granuloma syndrome
in a golden retriever. Canadian Veterinary Journal 1993;
34: 1212.
25. Fondevila D, Vilafranca M, Ferrer L. Epidermal immunocompetence in canine leishmaniasis. Veterinary
Immunology and Immunopathology 1997; 56: 31927.
26. Ferrer L, Solano-Gallego L, Arboix M et al. Evaluation
of the specific immune response in dogs infected by
Leishmania infantum. In: Thoday KL, Foil CS, Bond R
eds. Advances in Veterinary Dermatology, Vol. 4.
Oxford, UK: Blackwell Publishing Co., 2002: 929.
27. Newman LS, Rose CS, Maier LA. Sarcoidosis. New
England Journal of Medicine 1997; 336: 122434.
28. Mendel J, Weinberg SE. Clinical insights and basic science correlates in sarcoidosis. American Journal of
Medical Science 2001; 321: 99107.
29. Shapiro PE. Non infectious granulomas. In: Elder D,
Elenitsas R, Jaworsky C et al. eds. Levers Histopathology of the Skin, 8th edn. Philadelphia: Lippincott-Raven
Publishers, 1997: 31540.
30. Salian NV, Rish JA, Eisenach KD et al. Polymerase
chain reaction to detect Mycobacterium tuberculosis in
histologic specimens. American Journal of Respiratory
and Critical Care Medicine 1998; 158: 11505.
31. Hughes MS, James G, Ball N et al. Identification by 16S
rRNA gene analyses of a potential novel mycobacterium
species as an etiological agent of canine leproid granuloma syndrome. Journal of Clinical Microbiology 2000;
38: 9539.
32. Lemarie SL. Mycobacterial dermatitis. Veterinary
Clinics of North America 1999; 29: 1291301.
Rsum Le syndrome pyogranulome/granulome strile (SPGS) ou histiocytose cutane est une maladie
cutane rare chez le chien, dont ltiopathognie est inconnue. Lexamen histopathologique et labsence de mise
en vidence dun agent tiologique sont vocateurs de cette entit. Cependant, le SPGS a t suspect dtre d
une rponse immunitaire vis vis dantignes endognes ou exognes persistants. La prsence de leishmanies
et de mycobactries a t recherche par PCR dans 46 prlvements diagnostiqus comme des SPGS. Un examen
immunohistochimique pour la dtection de Leishmania a galement t ralis, et ses rsultats compars ceux
de la PCR. La technique PCR a permis dobtenir des rsultats positifs pour Leishmania spp. dans 21 des 46
prlvements cutans. Les rsultats des techniques immunohistochimiques taient identiques ceux de la PCR.
La PCR a donn des rsultats ngatifs pour Mycobacterium spp. sur tous les prlvements examins. Ces rsultats
suggrent quil est important de rechercher des leishmanies sur les biopsies cutanes dont lexamen histopathologique est compatible avec un diagnostic de SPGS.
Resumen El sndrome del piogranuloma/granuloma estril (SPGS) o histiocitosis cutnea es un trastorno de
etiopatogenia desconocida. Los hallazgos histopatolgicos y la imposibilidad de mostrar un agente etiolgico
son sugestivos de este sndrome. No obstante, existe la hiptesis de que el SPGS est relacionado con una
respuesta inmunitaria contra antgenos persistentes endgenos o exgenos. La presencia de organismos de
Leishmania y Mycobacterium fue investigada mediante tcnicas de PCR en 46 muestras de piel canina con un
diagnstico histopatolgico de SPGS. Concomitantemente, se aplic una tcnica inmunohistoqumica para la
deteccin de Leishmania sobre las mismas muestras y los resultados fueron comparados con los de la PCR. La
prueba de PCR result positiva para Leishmania spp. en 21 de las 46 muestras cutneas. Los resultados de las
pruebas inmunohistoqumicas fueron idnticas a los de la PCR. La tcnica de PCR dio resultados negativos
para Mycobacterium spp. en todas las muestras examinadas. Estos resultados sugieren la importancia de buscar
Leishmania spp en biopsias cutneas con hallazgos histopatolgicos compatibles con un diagnstico de SPGS.
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 233238
238
L Cornegliani et al.
Zusammenfassung Das cutane sterile Pyogranulom/Granulom-Syndrom (SPGS) oder cutane Histioztose ist
eine ungewhnliche Hauterkrankung des Hundes von unbekannter tiopathogenese. Histopathologische
Befunde und das Unvermgen, ein tiologisches Agens nachzuweisen, sind hinweisend auf dieses Syndrom.
Dennoch wird angenommen, dass SPGS im Zusammenhang mit einer Immunantwort auf ein persistierendes
endogenes oder exogenes Antigen steht. Bei 46 caninen Hautproben, die histopathologisch als SPGS diagnostiziert wurden, wurde durch Polymerase-Kettenreaktion (PCR) nach dem Vorhandensein von Leishmanien- oder
Mykobakterien-Organismen gefahndet. Gleichzeitig wurde eine immunhistochemische Technik zum Nachweis
von Leishmanien bei den gleichen Proben angewandt und die Ergebnisse wurden mit denen der PCR verglichen.
Die PCR-Technik zeigte positive Resultate fr Leishmania spp. in 21 von 46 Hautproben. Die Resultate mit der
immunhistochemischen Technik waren mit denen der PCR identisch. Die PCR-Technik ergab in allen untersuchten Proben negative Resultate fr Mycobacterium spp. Diese Resultate weisen auf die Wichtigkeit hin, bei
Hautproben mit Vernderungen, die mit denen von SPGS bereinstimmen, nach Leishmania spp zu suchen.
2005 European Society of Veterinary Dermatology, Veterinary Dermatology, 16, 233238
You might also like
- Effects of Dietary Flax Seed and Sunflower Seed Supplementation On Normal Canine Serum Polyunsaturated Fatty Acids and Skin and Hair PDFDocument7 pagesEffects of Dietary Flax Seed and Sunflower Seed Supplementation On Normal Canine Serum Polyunsaturated Fatty Acids and Skin and Hair PDFjenNo ratings yet
- Isolation of Microsporum Canis From The Hair Coat of Pet Dogs and Cats Belonging To Owners Diagnosed With M. Canis Tinea Corporis (Pages 327-331)Document5 pagesIsolation of Microsporum Canis From The Hair Coat of Pet Dogs and Cats Belonging To Owners Diagnosed With M. Canis Tinea Corporis (Pages 327-331)jenNo ratings yet
- Feline Plasma Cell Pododermatitis - A Study of 8 Cases (Pages 333-337) PDFDocument5 pagesFeline Plasma Cell Pododermatitis - A Study of 8 Cases (Pages 333-337) PDFjenNo ratings yet
- Oestrogen Receptor Evaluation in Pomeranian Dogs With Hair Cycle Arrest (Alopecia X) On Melatonin Supplementation (Pages 252-258)Document7 pagesOestrogen Receptor Evaluation in Pomeranian Dogs With Hair Cycle Arrest (Alopecia X) On Melatonin Supplementation (Pages 252-258)jenNo ratings yet
- Patch Testing of Experimentally Sensitized Beagle Dogs - Development of A Model For Skin Lesions of Atopic Dermatitis (Pages 95-102)Document8 pagesPatch Testing of Experimentally Sensitized Beagle Dogs - Development of A Model For Skin Lesions of Atopic Dermatitis (Pages 95-102)jenNo ratings yet
- The Impact of Body Site, Topical Melatonin and Brushing On Hair Regrowth After Clipping Normal Siberian Husky Dogs (Pages 45-50)Document6 pagesThe Impact of Body Site, Topical Melatonin and Brushing On Hair Regrowth After Clipping Normal Siberian Husky Dogs (Pages 45-50)jenNo ratings yet
- Mouse Epidermal Development - Effects of Retinoic Acid Exposure in Utero (Pages 36-44)Document9 pagesMouse Epidermal Development - Effects of Retinoic Acid Exposure in Utero (Pages 36-44)jenNo ratings yet
- Immunolocalization of Aquaporin-5 Expression in Sweat Gland Cells From Normal and Anhidrotic Horses (Pages 17-23)Document7 pagesImmunolocalization of Aquaporin-5 Expression in Sweat Gland Cells From Normal and Anhidrotic Horses (Pages 17-23)jenNo ratings yet
- A Retrospective Study of Cutaneous Equine Sarcoidosis and Its Potential Infectious Aetiological Agents (Pages 51-62)Document12 pagesA Retrospective Study of Cutaneous Equine Sarcoidosis and Its Potential Infectious Aetiological Agents (Pages 51-62)jenNo ratings yet
- Generalized Calcinosis Cutis Associated With Probable Leptospirosis in A Dog (Pages 401-406)Document6 pagesGeneralized Calcinosis Cutis Associated With Probable Leptospirosis in A Dog (Pages 401-406)jenNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Poecilia Reticulata Domestic Breeder Tra PDFDocument18 pagesPoecilia Reticulata Domestic Breeder Tra PDFAdrian BercanNo ratings yet
- Clinical Study: Overjet and Overbite Influence On Cyclic Masticatory Movements: A CT StudyDocument7 pagesClinical Study: Overjet and Overbite Influence On Cyclic Masticatory Movements: A CT Studyarya091193No ratings yet
- Aeromonas Hydrophila and Motile: Aeromonad Septicemias of FishDocument26 pagesAeromonas Hydrophila and Motile: Aeromonad Septicemias of Fishnhimdoc2016No ratings yet
- K15 - Infeksi Sistem Saraf PusatDocument65 pagesK15 - Infeksi Sistem Saraf PusatZikri Putra Lan LubisNo ratings yet
- Istory of Jellyfish Envenomation: 3.1.1. Class Cubozoa - Cubozoan JellyfishDocument16 pagesIstory of Jellyfish Envenomation: 3.1.1. Class Cubozoa - Cubozoan JellyfishRangsiyo BeabeoNo ratings yet
- Clinical Exemplar Deborah Ogunrinde University of South FloridaDocument4 pagesClinical Exemplar Deborah Ogunrinde University of South Floridaapi-402469727No ratings yet
- A Level Biology CAIE Topic 14 Control and CoordinationDocument75 pagesA Level Biology CAIE Topic 14 Control and CoordinationADEEL AHMAD100% (1)
- Partograph: (Use This Form For Monitoring Active Labour)Document1 pagePartograph: (Use This Form For Monitoring Active Labour)Omar Khalif Amad PendatunNo ratings yet
- Goat Housing and Fencing PDFDocument43 pagesGoat Housing and Fencing PDFmary anthoneth bayle100% (1)
- The Nervous System, NotesDocument6 pagesThe Nervous System, NotesnadshinkNo ratings yet
- NERVOUS SYSTEM (IB-DP BIOLOGY) - Multiple Choice Type QuestionsDocument5 pagesNERVOUS SYSTEM (IB-DP BIOLOGY) - Multiple Choice Type QuestionsVishnu SharmaNo ratings yet
- Jurnal 4Document5 pagesJurnal 4Nindita RahmaNo ratings yet
- Adoptive Immunotherapy Ludewig Hoffmann (Methods Molec Medicine 109 Humana 2005)Document517 pagesAdoptive Immunotherapy Ludewig Hoffmann (Methods Molec Medicine 109 Humana 2005)Cristian PopaNo ratings yet
- Pharyngeal ArchDocument6 pagesPharyngeal ArchRajsandeep SinghNo ratings yet
- Antonio Damasio, Hanna Damasio - Fear and The Human AmigdalaDocument13 pagesAntonio Damasio, Hanna Damasio - Fear and The Human AmigdalaAna Victoria Casillas ZapataNo ratings yet
- CHEESE - Dairy Processing Handbook PDFDocument30 pagesCHEESE - Dairy Processing Handbook PDFVVNo ratings yet
- 2.manajemen Gawat Nafas Pada Bayi Dan Anak - DrlizaDocument89 pages2.manajemen Gawat Nafas Pada Bayi Dan Anak - DrlizayuniayuNo ratings yet
- Efficacy of The Herbal Formulation Av/Epp/14 Against Ectoparasites On PetsDocument3 pagesEfficacy of The Herbal Formulation Av/Epp/14 Against Ectoparasites On PetsAmit Kumar PandeyNo ratings yet
- Compositae FamilyDocument23 pagesCompositae FamilyA.H. Lammert Holdijk100% (1)
- The Sensitive Gut Harvard HealthDocument57 pagesThe Sensitive Gut Harvard HealthDayhanna Guzman100% (7)
- Diagnostic Test For Endocrine DisordersDocument4 pagesDiagnostic Test For Endocrine DisordersjesperdomincilbayauaNo ratings yet
- Cat PDFDocument6 pagesCat PDFAnonymous GxMazRCNo ratings yet
- Coagulation Situation Analysis PFA FinalDocument27 pagesCoagulation Situation Analysis PFA FinalSudesh GungadinNo ratings yet
- Farmakodinamik Nsaid 2018Document57 pagesFarmakodinamik Nsaid 2018kiki rawitriNo ratings yet
- Spinal Cord and Spinal NervesDocument46 pagesSpinal Cord and Spinal Nerveskombat13_708353334No ratings yet
- Tetracycline Antibiotics: Medical UsesDocument2 pagesTetracycline Antibiotics: Medical UsesHanumant SuryawanshiNo ratings yet
- Resolving Negative Life ExperiencesDocument19 pagesResolving Negative Life ExperiencessoriboNo ratings yet
- (Timothy B-1. Westland, Robert N. Calton) Handbook oDocument431 pages(Timothy B-1. Westland, Robert N. Calton) Handbook oImmer Armendáriz Betancourt100% (1)
- Neck TrianglesDocument6 pagesNeck TrianglesJay-arh SebusaNo ratings yet
- Appendicitis PathophysiologyDocument4 pagesAppendicitis PathophysiologyAngelica Cassandra VillenaNo ratings yet