Professional Documents
Culture Documents
Economic Burden of MRSA, C.difficile, Enterococcus
Uploaded by
Ani IoanaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Economic Burden of MRSA, C.difficile, Enterococcus
Uploaded by
Ani IoanaCopyright:
Available Formats
Mitchell et al.
Antimicrobial Resistance and Infection Control 2013, 2(Suppl 1):P67
http://www.aricjournal.com/content/2/S1/P67
POSTER PRESENTATION
Open Access
P067: Economic burden of methicillin-resistant
Staphylococcus aureus, Clostridium difficile, and
vancomycin-resistant enterococci in hospitals
A Mitchell1*, R Rohde2, P Mallow3, D Buskirk1
From 2nd International Conference on Prevention and Infection Control (ICPIC 2013)
Geneva, Switzerland. 25-28 June 2013
Introduction
Methicillin-Resistant Staphylococcus aureus (MRSA),
Clostridium difficile (C. Diff) and Vancomycin-Resistant
Enterococci (VRE) are a significant source of HAIs.
Recently, significant attention has been given to community acquired strains of these infections. However,
HAIs with these pathogens remain a significant cause of
infections and associated costs to the health system.
Objectives
The purpose of this study is to estimate economic burden of MRSA, CDI, and VRE HAIs among inpatients in
US acute care hospitals.
Methods
The economic burden of MRSA, C. Diff, and VRE were
calculated based on incidence rates and costs attributable
to the pathogen rates from the published literature.
Studies included were those that estimated national incident rates of one or more of the HAIs. Cost estimates
were used from studies that specifically stated direct
costs associated with the HAIs. The median incidence
rate and cost were derived for the base estimate.
Results
The 2010 estimated total number of HAIs attributed to
the three pathogens was 1.325 million and an economic
burden attributable to the pathogens of $13.1 billion.
There were 1.046 million MRSA HAIs, 219,000 C.Diff
HAIs, and 59,000 VRE HAIs. Sensitivity analysis of
the incidence rate revealed that the total number of
HAIs ranged from 844,000 to 1.81 million and the
1
Johnson & Johnson, Irvine, USA
Full list of author information is available at the end of the article
associated economic burden ranged from $8.46 billion to
$17.73 billion. Sensitivity analysis of the costs ranged
from $9.8 billion to $16.4 billion.
Conclusion
MRSA, C. Diff, and VRE result in significant HAIs and
economic burden in patients hospitalized in US acute
care hospitals. For hospitals to remain profitable, one
important step should be a rigorous analysis of HAIs and
comprehensive preventative programs to reduce their
occurrence. Quality improvement programs to reduce
preventable HAIs such as MRSA, C. Diff, and VRE will
not only improve patient quality, but will increase hospital profitability by reducing HAIs that are subject to
financial disincentives.
Disclosure of interest
A. Mitchell Employee of Johnson & Johnson, R. Rohde:
None declared, P. Mallow Consultant for Johnson &
Johnson, D. Buskirk Employee of Johnson & Johnson.
Author details
1
Johnson & Johnson, Irvine, USA. 2Texas State University, San Marcos, USA.
3
S2, Irvine, USA.
Published: 20 June 2013
References
1. Kohn LT, Corrigan J, Donaldson MS: To err is human: building a safer health
system Washington, D.C.: National Academy Press; 2000.
2. Premier Research Services Premier I:, http://www.preimier-inc.com/prs
[Accessed March 2, 2012].
doi:10.1186/2047-2994-2-S1-P67
Cite this article as: Mitchell et al.: P067: Economic burden of methicillinresistant Staphylococcus aureus, Clostridium difficile, and vancomycinresistant enterococci in hospitals. Antimicrobial Resistance and Infection
Control 2013 2(Suppl 1):P67.
2013 Mitchell et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Trauma-Informed Care For Behavioral Health Service ProvidersDocument159 pagesTrauma-Informed Care For Behavioral Health Service ProvidersAlguémNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Activity 26 Assessment and Care of Antenatal Woman Ante Natal Case Record - 2Document5 pagesActivity 26 Assessment and Care of Antenatal Woman Ante Natal Case Record - 2A J FathimaNo ratings yet
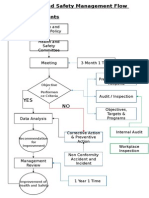
- Health and Safety FlowDocument6 pagesHealth and Safety Flowzaki0304No ratings yet
- Principles of Epidemiology in Public Health PracticeDocument512 pagesPrinciples of Epidemiology in Public Health PracticeAdare Oluwafemi Thomas100% (3)
- I. Introduction To Special EducationDocument9 pagesI. Introduction To Special EducationJennylyn Boiser100% (1)
- Human Factor QuizDocument5 pagesHuman Factor QuizSherif AL-KammashNo ratings yet
- Set 5Document18 pagesSet 5Dick Morgan FerrerNo ratings yet
- Case Presentation EncephalitisDocument30 pagesCase Presentation EncephalitisDimpal Choudhary100% (3)
- NEBOSH IG1 Open Book Mock Examination For Sept. 2022Document5 pagesNEBOSH IG1 Open Book Mock Examination For Sept. 2022m.naNo ratings yet
- Complementarity of Flow Cytometry and Fluorescence MicrosDocument2 pagesComplementarity of Flow Cytometry and Fluorescence MicrosAni IoanaNo ratings yet
- Next Generation DNA Sequencing MethodsDocument18 pagesNext Generation DNA Sequencing MethodsAni IoanaNo ratings yet
- Chapter 10: Pertussis: I. Disease DescriptionDocument10 pagesChapter 10: Pertussis: I. Disease DescriptionAni IoanaNo ratings yet
- Essential Cell Biology An Introduction TDocument14 pagesEssential Cell Biology An Introduction TAni IoanaNo ratings yet
- Comparison of High Throughput Next GenerDocument12 pagesComparison of High Throughput Next GenerAni IoanaNo ratings yet
- Chemical Composition Antibacterial Activity and Mechanism of Action of Essential Oil From Seeds of Fennel Foeniculum Vulgare Mill 2014 Food ControlDocument8 pagesChemical Composition Antibacterial Activity and Mechanism of Action of Essential Oil From Seeds of Fennel Foeniculum Vulgare Mill 2014 Food ControlAni IoanaNo ratings yet
- Attending Physician Statement (APS) - TPD - FamilyDocument3 pagesAttending Physician Statement (APS) - TPD - FamilyTaufik Hameed SultanNo ratings yet
- 07 English Ocd BookletDocument27 pages07 English Ocd BookletJona JoyNo ratings yet
- Food AdjunctDocument15 pagesFood AdjunctRoby martinus bayaNo ratings yet
- Pe Quiz 2Document4 pagesPe Quiz 2France Aldrin YagyaganNo ratings yet
- Cmca Activity 1 AliamenDocument5 pagesCmca Activity 1 AliamenJasmine AliamenNo ratings yet
- Term Paper (Issues)Document18 pagesTerm Paper (Issues)Joseph GratilNo ratings yet
- Brochure ISDocument4 pagesBrochure ISJAYESH VIKRAM RastogiNo ratings yet
- Immunization HandbookDocument200 pagesImmunization Handbooktakumikuroda100% (1)
- InfluenzaDocument7 pagesInfluenzaGionne Carlo GomezNo ratings yet
- Calcium CarbideDocument8 pagesCalcium CarbidetaraNo ratings yet
- Cognitive Behavioral Guided Self Help For The Treatment Od Recurrent Binge EatingDocument19 pagesCognitive Behavioral Guided Self Help For The Treatment Od Recurrent Binge EatingIsmael RodriguezNo ratings yet
- CH 06Document7 pagesCH 06john mwangiNo ratings yet
- Lesson 1 Physical Fitness and Related ActivitiesDocument31 pagesLesson 1 Physical Fitness and Related ActivitiesKaiNo ratings yet
- Donor Milk Banking and Breastfeeding in NorwayDocument6 pagesDonor Milk Banking and Breastfeeding in NorwayFrieta Diaz AstutiNo ratings yet
- Challenges Facing People With Disabilities and Possible Solutions in TanzaniaDocument8 pagesChallenges Facing People With Disabilities and Possible Solutions in TanzaniaKo ReaNo ratings yet
- 1 Script200302090903033030Document9 pages1 Script200302090903033030gever29816No ratings yet
- Verify Category B2 Report V6.35 Rev 1.0Document39 pagesVerify Category B2 Report V6.35 Rev 1.0Roger SchulpNo ratings yet
- QMDocument12 pagesQMGs AbhilashNo ratings yet
- Case Study 2Document12 pagesCase Study 2api-336539272No ratings yet
- Curahealth Hospitals Completes The Purchase of Specialty Hospital of JacksonvilleDocument2 pagesCurahealth Hospitals Completes The Purchase of Specialty Hospital of JacksonvillePR.comNo ratings yet
- Vasculitis When To Consider This DiagnosisDocument15 pagesVasculitis When To Consider This DiagnosisAndres PortesNo ratings yet
- Assignment On-: "Pharmacokinetics of Drug Molecules in Different Disease Condition"Document19 pagesAssignment On-: "Pharmacokinetics of Drug Molecules in Different Disease Condition"Susmoy SinhaNo ratings yet