Professional Documents
Culture Documents
Febrile Child Without Aq Focus - Management PDF
Uploaded by
erickmattosOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Febrile Child Without Aq Focus - Management PDF
Uploaded by
erickmattosCopyright:
Available Formats
Pediatr Infect Dis J, 2002;21:5842
Copyright 2002 by Lippincott Williams & Wilkins, Inc.
Vol. 21, No. 6
Printed in U.S.A.
Management of the febrile child without a
focus of infection in the era of universal
pneumococcal immunization
JEROME O. KLEIN, MD
Should strategies of management of invasive
disease in the febrile child without focus of infection (occult bacteremia) be reconsidered in communities with universal immunization of infants
with the conjugate vaccines for Haemophilus
influenzae type b and Streptococcus pneumoniae
(PCV7)? The incidence of occult bacteremia is
likely to decrease with the virtual elimination of
H. influenzae type b and vaccine serotype pneumococcal invasive diseases. The number of children with fever coming to physicians offices,
however, is unlikely to change. The challenge of
distinguishing the febrile child with invasive
bacterial disease who requires aggressive therapy from the febrile child who has a viral infection and requires only symptomatic therapy will
persist. The bacteriology of invasive disease in
infants and young children in 2002 will include
pneumococcal serotypes not in PCV7; serotypes
in PCV7 that occur in the unimmunized, partially
immunized or fully immunized child (vaccine
failures); Neisseria meningitidis; Salmonella
spp., group A Streptococcus, Staphylococcus aureus and Gram-negative enteric bacilli. Management plans published in the 1990s suggested an
aggressive diagnostic approach to the febrile
child 3 to 36 months old who was toxic or had a
temperature of >39C. Diagnostic tests included
white blood cell counts, cultures of blood and
urine and chest radiograph and lumbar puncture
as indicated by clinical signs and administration
of parenteral ceftriaxone. Although PCV7 was
extraordinarily effective in prevention of serotype-specific invasive pneumococcal disease in
clinical trials, pediatricians need to know
whether the results based on 38 000 enrollees
will be maintained as millions of children are
immunized. In addition questions about change
in serotype of pneumococci causing invasive disease (serotype switching), herd immunity and
durability of protection after immunization need
to be answered. Until more experience is available to answer these questions, the febrile child
without focus of infection should be managed
without consideration of immunization with
PCV7. Evaluation of the organism (serotype) and
the host (acute and convalescent sera) should be
undertaken for each case of invasive pneumococcal disease in this era of universal pneumococcal
immunization.
INTRODUCTION
The management of the febrile child without a focus
of infection, occult bacteremia, has been a subject of
controversy for decades. Radetsky1 noted that more
than 300 articles on management of the febrile infant
had been published in the 36 years beginning in 1960.
Streptococcus pneumoniae is responsible for the vast
majority of episodes of occult bacteremia. With the
availability and demonstrated efficacy of the heptavalent conjugate pneumococcal vaccine (PCV7) in prevention of invasive pneumococcal disease, does the strategy for management of the febrile child who is
immunized with PCV7 need to be reconsidered? The
purpose of this article is to review the microbial
changes that are likely to occur in the era of universal
pneumococcal immunization and the implications of
these changes for altering management strategies for
the febrile child.
MICROBIOLOGY OF OCCULT BACTEREMIA
Bacteriology of occult bacteremia in the 1990s.
The bacterial pathogens responsible for occult bacteremias before the introduction of the conjugate polysaccharide Haemophilus influenzae type b vaccine in 1990
and PCV 7 in 2000 included S. pneumoniae, Haemophilus influenzae type b (Hib), Neisseria meningitidis,
group A Streptococcus, Staphylococcus aureus, Salmonella spp. and Gram-negative enteric bacilli (Fig. 1). S.
From Pediatric Infectious Diseases, Boston Medical Center,
and Department of Medicine, Boston University School of Medicine, Boston, MA.
Key words: Febrile child, management, occult bacteremia,
pneumococcal vaccine.
Address for reprints: Jerome O. Klein, M.D., Maxwell Finland
Laboratory for Infectious Diseases, Boston Medical Center, 774
Albany Street, Boston, MA 02118. Fax 617-414-7230. E-mail
jerome.klein@bmc.org.
DOI: 10.1097/01.inf.0000016385.94483.52
584
Vol. 21, No. 6, June, 2002
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
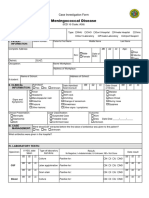
FIG. 1. Estimated proportions of pathogens responsible for
occult bacteremia, 1990 and 2002.
pneumoniae was responsible for 80% of all episodes of
occult bacteremia2; of the pneumococcal bacteremias
80% were caused by serotypes in PCV 73; thus 64%
of the occult bacteremias were caused by PCV 7 serotypes, and 16% were caused by serotypes not in PCV 7.
Hib was responsible for 10% of the invasive episodes
of occult bacteremia, and N. meningitidis was responsible for 2 to 5%, with only a small proportion of cases
of the other bacterial pathogens.
After introduction of the Hib vaccine, the number of
episodes of Hib bacteremia diminished. Studies from
Boston4 and Philadelphia5 examined the microbiology
of occult bacteremia for the period 1993 to 1996. In the
Boston cohort the rate of occult bacteremia in febrile
children 3 to 36 months of age with a temperature of
39C or greater was 1.57%. The pneumococcus was
responsible for 92% of the positive cultures of blood.
The Philadelphia study used similar criteria for infants
2 to 24 months of age. The prevalence of bacteremia
was 1.9%; S. pneumoniae was responsible for 82.9% of
the bacteremias, Salmonella spp. 5.4% and group A
streptococci 4.5%.
Bacteriology of occult bacteremia in 2002. In
2002 with almost universal use of the conjugate Hib
and pneumococcal vaccines in infants in the United
States, the incidence of invasive disease is likely to
decrease, and the pattern of bacterial pathogens responsible for occult bacteremia will change. Without an
available vaccine, the incidence of meningococcemia,
invasive disease caused by Salmonella, group A Streptococcus, Staphylococcus aureus and Gram-negative
enteric bacilli, is likely to remain constant. Given that
microbial ecology is constantly changing, we need to be
alert for the possibility that one of these pathogens will
become more important as a cause of occult bacteremia.
Invasive disease caused by Hib has been almost
eliminated in communities with high rates of immunization with the conjugate vaccine. The organism may
persist in communities with low rates of immunization
such as those with religious reasons for refusal to
immunize.
585
Although still uncommon the appearance of invasive
disease caused by H. influenzae type a6 and type f7
suggests the possibility that non-b serotypes could
replace Hib as a serious pathogen.
Influence of the conjugate pneumococcal vaccine on the bacteriology of occult bacteremia.
The success of PCV7 in prevention of invasive disease
caused by serotypes in the vaccine in the Northern
California clinical trial8 will likely be replicated as
millions of children are immunized. There are data
that suggest a herd effect; an average of 34% of all
children younger than age 5 years were vaccinated in
Northern California between October, 1995, and
March, 2001; during this time period there was a 62.4%
reduction in invasive disease among children younger
than 5 years.9 Although problems with vaccine supply
occurred in the summer and fall of 2001, by December,
2001, 23 million doses of PCV7 had been distributed in
the United States (M Boken, Wyeth Lederle Vaccines,
personal communication). If the vaccine proves to be
97% effective for prevention of pneumococcal disease
caused by serotypes in the vaccine in fully immunized
children (as occurred in the clinical trial), there will be
a substantial decrease in episodes of occult bacteremia.
Nevertheless invasive pneumococcal disease will persist in infants: (1) disease will occur caused by serotypes not in the vaccine; (2) disease will occur caused
by serotypes in the vaccine and represent vaccine
failures; (3) some children will not have protective
antibodies because they were unimmunized or incompletely immunized; (4) some children will not have
protective antibodies because of immune deficits. The
possibility of vaccine switching in immunized children
exists, i.e. increased incidence of invasive disease
caused by serotypes not in the vaccine. Alternatively
there might be protection for serotypes not in the
vaccine but related to vaccine serotypes. The results of
the microbiologic studies of otitis media in Finnish
children10 identified a reduction in the frequency of
episodes caused by serotypes that cross-reacted with
those in the vaccine (serotypes 6A, 9N, 18B, 19A and
23A). However, there was also a 33% increase in
serotypes not in the vaccine causing otitis media. Thus
even though the PCV7 is likely to be very effective, the
nonvaccine serotypes of pneumococcus (and the uncommon cases of vaccine serotypes of pneumococcus) will
persist as the most frequent pathogen associated with
occult bacteremia (Fig. 1).
SHOULD THE MANAGEMENT OF INFANTS WITH
FEVER WITHOUT SOURCE WHO ARE
IMMUNIZED WITH PCV7 CHANGE?
Fever without source in infants will continue to be a
common cause of office visits to physicians. About
two-thirds of children between the ages of birth and 2
years visit the physician for an acute febrile illness.11
586
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
Fever without source is the diagnosis in 14% of office
visits. Because the overall incidence of invasive disease
among febrile infants was low, the introduction of the
conjugate vaccines will not diminish the number of
office visits for fever without source. The challenge to
the practitioner of distinguishing the few children with
invasive bacterial disease who require aggressive management from the many children who have presumably
viral and spontaneously resolving disease that can be
managed with symptomatic treatment will remain.
The guidelines below are suggestions for current management of the infant with fever without source in the
era of universal Haemophilus and pneumococcal immunizations.
Management of the febrile neonate. Fever in the
first weeks of life is relatively uncommon. However,
when fever does occur the incidence of severe disease
including sepsis is sufficiently high to warrant careful
evaluation and conservative management. Invasive
disease caused by S. pneumoniae, H. influenzae (usually nontypable) and N. meningitidis occurs but is
uncommon. Practice guidelines prepared by Baraff et
al.2 for management of febrile infants younger than 28
days suggest that all should be considered for hospitalization and parenteral antibiotic therapy unless there
is a recognizable alternative and benign diagnosis. The
differential diagnosis of fever in the first month of life
includes five categories based on pathogenesis: in utero
infections; infections acquired at delivery (early and
late onset sepsis); infections acquired in the nursery;
infections acquired in the household; and infections
acquired because of underlying anatomic or physical
disabilities (e.g. urinary tract infections). For presumed bacterial sepsis in the neonate, initial therapy
with ampicillin and gentamicin continues to be appropriate
Management of the infant 29 to 90 days old
with fever without source. Invasive disease after
the first month includes a mix of late onset disease
associated with organisms acquired at delivery including group B streptococci, Gram-negative enteric bacilli
and uncommonly Listeria monocytogenes and enterococci as well as the invasive organisms acquired in the
household, pneumococci, meningococci and H. influenzae. Febrile infants in this age group may be categorized as toxic or nontoxic, and among the nontoxic
group low risk or high risk for invasive bacterial
disease.12 Low risk criteria include: previously being
healthy; having no focal bacterial infection on physical
examination; and having negative laboratory screening. Negative laboratory screening is defined as a white
blood cell (WBC) count of 5000 to 15 000/mm3, 1500
band forms/mm3, normal urinalysis, and when diarrhea is present, 5 WBC per high power field in stool.
The percent of serious bacterial infections in infants 90
days of age or less by clinical and laboratory findings is
Vol. 21, No. 6, June, 2002
1.4% contrasted with 17.3% if the patients appears
toxic. For the toxic or nontoxic but high risk patient,
ceftriaxone (50 mg/kg once daily in the absence of
meningitis) was recommended by Baraff et al.2 and is
still the regimen of choice. Parenteral ampicillin should
be added for the rare cases of invasive disease caused
by enterococci or L. monocytogenes. Because febrile
infants in this age group would have received none or
one dose of PCV7, the vaccine status of the child is
irrelevant to therapeutic decisions.
Management of the child 3 to 36 months of age
with fever without source. The risk of occult bacteremia in children 3 to 36 months of age without source
was reported in the review of Baraff and colleagues to
vary from 1.6 to 11% with a mean probability of 4.3% in
children with a temperature of 39C or more.2, 12 Bacteremia is more frequent in children with higher temperatures and elevated WBC counts. A summary of
studies of WBC counts in children with fever without
source by Baraff et al.2 identified a mean probability of
2.6% in children with WBC 15 000 and 13% in children with WBC 15 000. Recent reports suggest that
C-reactive protein has a better predictive value for
occult bacteremia and serious bacterial infection than
WBC counts.13
An algorithm for management of children 3 to 36
months of age with fever without source was proposed
by Baraff et al.2 and is frequently cited as a useful
guide. Children who were toxic were hospitalized for
sepsis workup and parenteral antibiotics; ceftriaxone
50 mg/kg/day in a single dose was recommended. Children who were not toxic but who had a temperature of
39C or greater had WBC count; cultures of blood,
urine and stool; and chest radiograph if clinical signs of
lower respiratory tract infection were present. Empiric
use of ceftriaxone was recommended for all children
with temperature of 39C or greater or for such febrile
children if the WBC count was 15 000. These guidelines generated much discussion, and viewpoints varied among experts.14 16 Some argued that the expense
and pain for the child of diagnostic tests and parenteral
therapy were unwarranted because the incidence of
invasive bacterial disease was low and many of the
episodes of pneumococcal and Haemophilus influenzae
bacteremia cleared without use of antimicrobial
agents. Other experts countered that the role of the
physician was as gatekeeper to protect the previously
healthy child from the uncommon invasive event that
had potential serious outcomes and that treating many
to protect the few with severe disease was warranted.
The purpose of this article is not to reconcile these
viewpoints but to question whether or not the introduction of the conjugate pneumococcal vaccine alone warrants a change in the concepts of management of
children who are fully immunized and have fever
without source.
Vol. 21, No. 6, June, 2002
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
The history of vaccine safety and efficacy after approval and recommendations by authoritative groups
is replete with surprises, most of which are unanticipated adverse events. The most recent example is the
unexpected increased incidence of intussusception associated with rotavirus vaccine. PCV 7 had an excellent
safety record during the clinical trials, but physicians
still need to be alert for the rare adverse event that
may be identified only after hundreds of thousands of
children are immunized. The efficacy documented in
the clinical trials must be corroborated as millions of
children are immunized. In addition questions about
the possibility of serotype switching, incidence of nonvaccine serotypes causing invasive disease and duration of protection will be answered only after sufficient
experience has accumulated. For all these reasons the
strategy of management of the child with fever without
source should be the same irrespective of the history of
PCV immunization. With the passage of time and
greater experience, we can reassess these recommendations and consider change as directed by the data.
Careful and skilled observation remains the
key to management of the febrile child. The key to
management decisions of the febrile child without
source remains the ability of the physician/nurse to
distinguish the child who is toxic from the child who is
not toxic; to distinguish the child who has altered affect
including decreased state of alertness, decreased responsiveness, has difficulty in being consoled from the
child who is playful, responsive, maintains eye contact
and is readily consoled. The art of pediatrics, the
powers of observation of the astute clinician, remains
the key to management of the febrile child. The febrile
illness is dynamic; the child will appear different, for
better or worse, hours after the office visit. The physician needs to maintain contact with the family until
the clinical episode is resolved. Selected laboratory
tests, particularly WBC counts and differential, are of
value if there is ambiguity in the clinical diagnosis, but
if the test is performed the physician must respond to
the results. None of these clinical issues changes in the
era of universal pneumococcal immunization.
RESPONSIBILITY OF THE PHYSICIAN IN
ASSESSING THE CHILD WITH PNEUMOCOCCAL
BACTEREMIA
Physicians will continue to encounter children with
episodes of invasive pneumococcal disease. To further
document the efficacy of PCV 7 as millions of doses are
administered to infants throughout the United States,
thorough evaluation of each child with invasive pneumococcal disease will be necessary. The physician responsible for such a child should consider the following
steps: (1) document the history of immunization with
PCV 7 or pneumococcal polysaccharide vaccine: include
dates of immunization, source of the vaccine and lot
587
number; (2) obtain the pneumococcal isolate and submit for serotyping and susceptibility tests; (3) obtain
acute and convalescent samples of blood: the acute
serum will provide information about protective antibody at the onset of disease and whether or not the
child responded to PCV 7 (if received). The convalescent serum will provide information about the ability of
the patient to respond to the disease causing strain.
If the child has had prior episodes of pneumococcal
disease or syndromes suggesting pneumococcal disease, an assessment of immune functions should be
considered.
The Centers for Disease Control and Prevention has
established a report form for tracking cases of invasive
pneumococcal disease among vaccinated children. The
instruction sheet and case report form can found at
www.cdc.gov/nip.
SUMMARY AND CONCLUSIONS
(1) Fever without source will continue to be a frequent reason for visits to physicians. (2) The microbiology of occult bacteremia will likely change in the era
of universal pneumococcal conjugate vaccine immunization. Nevertheless pneumococcal disease caused by
serotypes not in the vaccine, due to vaccine failure or
occurring in children who were not immunized or
partially immunized or have immune defects will continue to be the most frequent cause of occult bacteremia. The incidence of meningococcemia or bacteremia
caused by group A Streptococcus, Salmonella, Staphylococcus aureus or Gram-negative enteric bacilli will
likely continue at recent rates of disease unless
changes in the ecology of the pathogen occurs. (3) Fever
in the infant to 28 days of life should be aggressively
managed as in the past. (4) Fever in the first 3 months
of life should be aggressively managed. Because the
infant will have received at a maximum one dose of
PCV 7, vaccine history is irrelevant to management
decisions. (5) Management of the febrile infant without
source of infection during ages 3 months to 3 years
should not be changed until more extensive experience
with PCV 7 is available. The history of vaccines is
replete with surprises, and it is still too early in our
understanding of the safety and efficacy of PCV 7 to
warrant a change in strategy of the uncommon but
potentially severe consequences of invasive bacterial
disease in the occult bacteremia syndrome.
REFERENCES
1. Radetsky, M. The febrile infant and the assumption of risk.
Curr Opin Infect Dis 1996;9:1715.
2. Baraff LJ, Bass JS, Fleisher GR, et al. Practice guideline for
the management of infants and children 0 to 36 months of age
with fever without source. Pediatrics 1993;92:112.
3. Hausdorff WP, Bryant J, Paradiso PR, Siber GR. Which
pneumococcal serogroups cause the most invasive disease:
Implications for conjugate vaccine formulation and use, Part
I. Clin Infect Dis 2000;30:100 21.
588
THE PEDIATRIC INFECTIOUS DISEASE JOURNAL
4. Lee GM, Harper MB. Risk of bacteremia for febrile young
children in the post-Haemophilus influenzae type b era. Arch
Pediatr Adolesc Med 1998;152:624 8.
5. Alpern ER, Alessandrini EA, Bell LM, Shaw KN, McGowan
KL. Occult bacteremia from a pediatric emergency department: prevalence, time to detection and outcome. Pediatrics
2000;106:50511.
6. Adderson E, Byington C, Spencer L, et al. Invasive serotype a
Haemophilus influenzae infections with a virulence genotype
resembling Haemophilus influenzae type b: emerging pathogen in the vaccine era? Pediatrics 2001;108:e18.
7. Urwin G, Krohn JA, Deaver-Robinson K, Wenger JD, Farley
MM, and the Haemophilus influenzae Study Group. Invasive
disease due to Haemophilus influenzae serotype F: clinical
and epidemiologic characteristics in the H. influenzae serotype b vaccine era. Clin Infect Dis 1996;22:1069 76.
8. Black S, Shinefield H, Fireman B, Lewin D, et al. Efficacy,
safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Pediatr Infect Dis J 2000;19:187
95.
9. Shinefield H, Black S, Elvin L, et al. Impact of the introduction of pneumococcal conjugate vaccine on the epidemiology of
invasive disease in children less than 5 years of age within
Northern California Kaiser Permanente: Session 78. Pre-
10.
11.
12.
13.
14.
15.
16.
Vol. 21, No. 6, June, 2002
sented at the 39th Annual Meeting of the Infectious Diseases
Society of America, October 25 to 28, 2001.
Eskola J, Kilpi T, Palmu A, Jokinen J, et al. Efficacy of a
pneumococcal conjugate vaccine against acute otitis media.
N Engl J Med 2001;344:4039.
Soman M. Characteristics and management of febrile young
children seen in a university family practice. J Fam Pract
1985;21:11722.
Baraff LJ, Oslund S, Schriger DL, Stephen ML. Probability of
bacterial infections in infants less than three months of age:
a metaanalysis. Pediatr Infect Dis J 1992;11:257 65.
Pulliam, PN, Attia MW, Cronan KM. C-reactive protein in
febrile children 1 to 36 months of age with clinically undetectable serious bacterial infection. Pediatrics 2001;108:
12759.
Kramer MS, Shapiro ED. Management of the young febrile
child: a commentary on recent practice guidelines. Pediatrics
1997;100:128 34.
Baraff LJ, Bass JW, Fleisher GR, Klein JO, McCracken GH,
Powell KR. Commentary of practice guidelines. Pediatrics
1997;100:134 6.
Bauchner H, Pelton SI. Management of the young febrile
child: a continuing controversy. Pediatrics 1997;100:137 8.
You might also like
- Valentini ErrartumDocument1 pageValentini ErrartumerickmattosNo ratings yet
- Toxo Afp 2003Document2 pagesToxo Afp 2003erickmattosNo ratings yet
- Treatment of Recurrent Erythema Nodosum Leprosum With InfliximabDocument1 pageTreatment of Recurrent Erythema Nodosum Leprosum With InfliximaberickmattosNo ratings yet
- ICC Inh Peptido Natriuretico IndianJPharmacol353139-6497827 - 180258Document7 pagesICC Inh Peptido Natriuretico IndianJPharmacol353139-6497827 - 180258erickmattosNo ratings yet
- ZZ Deshidratacion 1Document1 pageZZ Deshidratacion 1erickmattosNo ratings yet
- Herpes AFP 2002 03mar 15 Herpes en NeonatosDocument5 pagesHerpes AFP 2002 03mar 15 Herpes en NeonatoserickmattosNo ratings yet
- Journal of The New Zealand Medical AssociationDocument4 pagesJournal of The New Zealand Medical AssociationerickmattosNo ratings yet
- ZLLA y Hemorragia CerebralDocument3 pagesZLLA y Hemorragia CerebralerickmattosNo ratings yet
- Malignant Peritoneal Mesothelioma: Brian W. Loggie, MDDocument1 pageMalignant Peritoneal Mesothelioma: Brian W. Loggie, MDerickmattosNo ratings yet
- LLA VandetanibDocument12 pagesLLA VandetaniberickmattosNo ratings yet
- ReviewDocument5 pagesReviewerickmattosNo ratings yet
- AmpC Seleccionados Por Cipro Antimicrob. Agents Chemother.-2007-Wolter-2997-00Document4 pagesAmpC Seleccionados Por Cipro Antimicrob. Agents Chemother.-2007-Wolter-2997-00erickmattosNo ratings yet
- Repeating Blood Cultures in Neutropenic Children With Persistent Fevers When The Initial Blood Culture Is NegativeDocument5 pagesRepeating Blood Cultures in Neutropenic Children With Persistent Fevers When The Initial Blood Culture Is NegativeerickmattosNo ratings yet
- FTP PDFDocument6 pagesFTP PDFerickmattosNo ratings yet
- Review Antifungal Prophylaxis in Pediatric Hematology/Oncology: New Choices & New DataDocument6 pagesReview Antifungal Prophylaxis in Pediatric Hematology/Oncology: New Choices & New DataerickmattosNo ratings yet
- Respiratory Syncytial Virus Infections in Children With Acute Myeloid Leukemia: A Report From The Children's Oncology GroupDocument3 pagesRespiratory Syncytial Virus Infections in Children With Acute Myeloid Leukemia: A Report From The Children's Oncology GrouperickmattosNo ratings yet
- Invasive Fungal Infections in Pediatric Oncology: MD MD MD MD MD MDDocument6 pagesInvasive Fungal Infections in Pediatric Oncology: MD MD MD MD MD MDerickmattosNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Pidsr CifDocument17 pagesPidsr CifAbraham Asto100% (4)
- Case Investigation Form - Meningococcal DiseaseDocument2 pagesCase Investigation Form - Meningococcal Diseaseclaverialc10No ratings yet
- Acute Febrile Illnesses: Solomon Bekele Sirak Melkeneh Sonia Worku Fri. May 15, 2014Document124 pagesAcute Febrile Illnesses: Solomon Bekele Sirak Melkeneh Sonia Worku Fri. May 15, 2014ashuNo ratings yet
- Meningococcal Infection in ChildrenDocument6 pagesMeningococcal Infection in ChildrenAdrian KhomanNo ratings yet
- Neurological DiseasesDocument91 pagesNeurological Diseasesrabia khalidNo ratings yet
- Questions For Community Medicine MD 4Document11 pagesQuestions For Community Medicine MD 4Bindashboy0No ratings yet
- Group I Group II Group IIIDocument67 pagesGroup I Group II Group IIIYamlak NegashNo ratings yet
- Admission LetterDocument4 pagesAdmission LetterYasir KNNo ratings yet
- Lecture 5 MicrobiologyDocument89 pagesLecture 5 Microbiologyjessenia.tutor2010No ratings yet
- Gram Negative Bacteria of Medical Importance - PPTX, MONDAYDocument113 pagesGram Negative Bacteria of Medical Importance - PPTX, MONDAYGeorge C. KasondaNo ratings yet
- Special Microbyology1Document142 pagesSpecial Microbyology1Sheba RoymonNo ratings yet
- CNS InfectionsDocument9 pagesCNS InfectionsriabaxterNo ratings yet
- Meningococcemia: Neisseria Meningitidis - Is An EncapsulatedDocument19 pagesMeningococcemia: Neisseria Meningitidis - Is An EncapsulatedcarolinecayasaNo ratings yet
- NBHS2332 Learning KitDocument36 pagesNBHS2332 Learning Kitshinichi kudoNo ratings yet
- Neisseria MeningitidisDocument3 pagesNeisseria MeningitidishedstrongNo ratings yet
- Meningitis CompleteDocument26 pagesMeningitis CompleteMayom MabuongNo ratings yet
- UW (Step 1) Neurology - Educational ObjectivesDocument86 pagesUW (Step 1) Neurology - Educational ObjectivesDrbee100% (1)
- Bacterial MeningitisDocument2 pagesBacterial MeningitisSpideyPacerNo ratings yet
- Dermatology Videos by DR RihamDocument31 pagesDermatology Videos by DR Rihamengr_shazzNo ratings yet
- Microbiology Viriology and ImmunologyDocument44 pagesMicrobiology Viriology and ImmunologyRoseline AdebisiNo ratings yet
- The Courier September 7 2017Document41 pagesThe Courier September 7 2017Boki VaskeNo ratings yet
- Neisseria Species and Moraxella Catarrhalis: Lauren RobertsDocument21 pagesNeisseria Species and Moraxella Catarrhalis: Lauren RobertsPrinces MaeNo ratings yet
- 33 MeningitisDocument71 pages33 MeningitisKaif KhanNo ratings yet
- Priority Disease ReportDocument24 pagesPriority Disease ReportalirrehmanNo ratings yet
- MODULE 2: Types of Vaccine and Adverse ReactionsDocument29 pagesMODULE 2: Types of Vaccine and Adverse ReactionsnandaNo ratings yet
- Bacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceDocument18 pagesBacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceZarwo Black UstadzNo ratings yet
- Infectious Diseases - BacteriaDocument9 pagesInfectious Diseases - Bacteriamiguel cuevas100% (1)
- 2021 - l4 Medical Bacteriology - Gram Negative Bacteria (I)Document52 pages2021 - l4 Medical Bacteriology - Gram Negative Bacteria (I)Tonny YuliantoNo ratings yet
- Objectives: at The End of This Activity, You Should Be Able ToDocument3 pagesObjectives: at The End of This Activity, You Should Be Able ToArriane AndayaNo ratings yet