Professional Documents
Culture Documents
Geriatric Considerations For Exercise Prescription
Uploaded by
shivnairOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Geriatric Considerations For Exercise Prescription
Uploaded by
shivnairCopyright:
Available Formats
9/10/2013
Effect of Exercise on Health
Geriatric Considerations for
Exercise Prescription
Pennsylvania State Meeting
October 26-27, 2013
Bill Staples PT, DHS, DPT, GCS, CEEAA
President, Section on Geriatrics
Posing the question does exercise
prevent or treat disease in older
persons? is analogous to asking
does medication prevent or treat
disease in older persons?
Fiatarone & Singh, Journal of Gerontology, 2002, Vol. 57A
No. 5
Objectives
Objectives
Identify the factors that affect
exercise in the elderly
Identify difficulties inherent in
describing patients by their
chronological age
Compare and contrast normal aging
Describe potential impact of exercise
on the aging process
Describe age-related changes that
affect exercise
Describe special considerations for
senior clients
Describe exercise training guidelines
and additional precautions when
managing the care of older adults
Baby Boomer Exercise
Introduction
When youre young, you challenge
your body. When youre old your
body challenges you!
Unknown
http://tinyurl.com/2u3pbz
Rehab of older adults has evolved
into an area of specialty practice
Based on evidence that aging causes
the body to respond differently to:
Injury
Disease
Exercise
9/10/2013
Chronological Age
Descriptions
Introduction
Considerable growth, now and in the
future, of the older population
Tremendous increase in individuals
reaching old age
The definition of old age is
changing due to:
Life expectancy
Medical care
Social practices
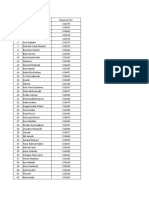
Middle age
Young old
Older
Old-old
Oldest-old
45-64 years
65-74 years
75-84 years
85-99 years
100+ years
Aging: Impact of Rehabilitation
Aging: Impact of Rehabilitation
No perfect definition of the aging
process
Aging refers to a process occurring
in living organisms
With aging comes an increased
probability of:
Elderly often contend with multiple
conditions (co-morbidities)
Physical injury and impairments are
among the most prevalent health
problems of aging
mobility independence
disability
Illness and disease
Chronic debilitating condition
Loss of function
Aging: Impact of Rehabilitation
Aging: Impact of Rehabilitation
Disability leads to increased* :
Rehab programs should be designed
to:
Mortality
Hospitalizations
SNF placement
Use of informal and formal home health
care
Cost
Restore function and mobility
Decrease pain (acute and chronic)
Decrease disability
Prolong independence
Improve quality of life
* Gill et al, 2003
9/10/2013
Aging
Is NOT homogeneous
Theories of aging differ
Genetic
Damage
Imbalance
Is aging an illness?
Death in America
50% of all deaths in U.S. due to
some sort of heart disease
70% deaths from heart disease
result from a stroke or heart attack
Much of heart disease is preventable
with healthy lifestyle including
exercise
Aging
Process differs among individuals
Variability and health status much
greater in older populations
Many adults are capable of high
degrees of activity and functional
abilities
Others display physiologic age well
beyond chronological age due to
chronic disease process
Biological Aging Changes
Normal aging changes: 0 functional
impairments or dysfunction in absence of
pathology
Maximal work capacity- gradual decline,
not noticed until critical capacity lost
Women especially susceptible due to smaller
initial muscle mass
Impacts functional status 10 years before men
Aging
Should NOT use chronological age to
determine potential for recovery or
appropriateness for rehabilitation!
Comprehensive evaluation is basis
for treatment
Clinician must recognize potential on
the individuals ability to participate
in rehab
Physiologic Reserve
Over time
Loss of adaptability
Development of impairment
Functional limitations
Disability
Loss of reserve function and
defined as frailty
Frailty Failure
Regular exercise proven to
prevent/reduce functional declines
linked to aging
9/10/2013
Exercise CapacityVicious Cycle
Usual aging- decreased
exercise capacity
Exacerbation of agerelated/disuse
declines
Increased perception
of effort/injury
Avoidance of activity
Normal vs. Pathological Aging
Pathological
Osteoarthritis
Osteoporosis
CAD
Sarcopenia
Many conditions can be prevented or
lessened with:
Normal vs. Pathological Aging
Normal aging changes occur as a
result of passage of time and are free
of pathological conditions i.e.
Presbyopia (farsightedness)
Presbycusis (hard of hearing)
Menopause
Physical Activity
However:
66% of people over 75 do nothing in
terms of physical activity*
50% of people 65-74 do nothing
42% of people 45-64 do nothing
Early and effective intervention
Appropriate patient education
Follow through
*Defined as 20 min. of exercise 3x/week
*Mokdad et al, 2001
Good Health Habits Start in
Middle Age
Consequences of Inactivity*
Hypokinetics
Middle aged adults (45-64) that began
Eating 5 servings fruit/veg per day
Exercised 2 hours per week
Kept weight down
Did not smoke
Decreased risk of heart disease by 35%
and death by 45%
Of 16,000 individuals, only 8.5% were
following these 4 guidelines at start of 6year study. By the end, another 8.4% had
joined. (still only 17%!)
King, D Amer J Med. 2007
Deconditioning
Accelerated
Loss of muscle mass & strength
Bone demineralization
Loss of neuromuscular control
Functional decline
Disuse accelerates the aging process
Heightened risk for falls
Hospitalization/SNF
*Gill et al 2004
9/10/2013
Required Tasks of Community
Dwelling Older Adults*
Cost of Sedentary Lifestyle
Estimated that U.S. could save $50
Billion per year in SNF care alone if
seniors increased activity level*
Walk a minimum of 1000 ft per errand
Often make 2-3 trips per day
Carry packages avg. 6.7 lbs while walking
Frequently encounter stairs, curbs, slopes
Engage in frequent postural transitions
Change direction, look up, reach up, move
backwards, sharp turn
Multi-tasking
So make rehab functional
*Janssen,
2004
* Shumway-Cook et al 2002
Myths about aging and
physical activity
Exercise and Health
Answer makes sense only when
exercise is described in terms of:
Modality
Dose (frequency, intensity)
Duration of exposure
Compliance with prescription
In relation to disease, syndrome,
biological aging
High intensity is not for older
persons
Resistive exercise will injure older
persons
Older persons do not have the same
functional demands as younger
persons
Older persons will accommodate
rather than challenge
Exercise??
If exercise were
a pill would
everyone take
it?
Exercise and Health
Answer makes sense only when
exercise is described in terms of:
Modality
Dose (frequency, intensity)
Duration of exposure
Compliance with prescription
In relation to disease, syndrome,
biological aging
9/10/2013
Exercise screening
Pre-screened by MD to r/o CVD, ASHD
ACSM: Stress test men >45, women >55
or known CAD, or 2 risk factors
HTN, smoking, obesity, HDL, sedentary
lifestyle, family hx of CAD, DM, known
pulmonary disease
Endurance Training
PT
Physical limitations (osteoporosis)
Goals (fitness vs. senior Olympics)
Areas of interest (gardening, walking etc.)
Role of aerobic exercise
Builds endurance
Necessary for function, ADLs
Lowers serum triglycerides
Raises HDLs
Lowers systolic and diastolic BP
Lowers blood glucose levels
Cardiovascular Exercise Slows
Biological Changes of Aging
Decrease CAD and stroke
Increases VO2 max
Lower fasting glucose and insulin levels
Lowers blood pressure
Adaptation to chronic activity can markedly
attenuate decrements in exercise capacity
due to aging
Exception: maximal heart rate
Cardiovascular Exercise Slows
Biological Changes of Aging
Improves HDL levels, lowers
triglycerides and total cholesterol
Improves body composition with 1-4%
reduction in body fat
Lowers risk for falls
Increases strength,
reduces depression
Reduces risk for diabetes
Contraindications
Recent ECG change or MI
Unstable angina
Third degree heart block
Acute CHF
Uncontrolled HTN
Uncontrolled metabolic disease (DM)
9/10/2013
Relative contraindication
Cardiomyopathy
Valvular heart disease
Complex ventricular ectopy
Cardiac rhythm originating elsewhere
than the SA node
Exercise prescription
Example
70 y.o.
Goal 60-85% PMHR for training (THR)
PMHR = 220 -70 =150 bpm
150 x 85% = 128 bpm
150 x 60% = 90 bpm
Training range 90-128 bpm
Exercise prescription
Tanaka et al 2001, hypothesized this may
underestimate HR max in older adults
Alternative 208 0.7 x age = HR max
208 0.7 x 70 (age) = ?
208 49 = 159
159 x .85 = 135
159 x .60 = 95
Target range 95-135 or slightly higher than
ACSM 2006. ACSM 2010 uses this.
Exercise prescription
ACSM (2006)
Intensity: Max HR assessed directly
thru age predicted (PMHR)
PMHR = 220-age
Training range between 60-85% max
HR
May not be accurate in the elderly
Karvonen Method
Factors in resting heart rate (HRrest) to
calculate target heart rate (THR), using a range
of 5085% intensity:
THR = ((HRmax HRrest) % intensity) + HRrest
Example for someone age 70 with a HRmax of
150 and a HRrest of 70:
50% Intensity:((150 70) 0.50) + 70 =110
bpm
85% Intensity: ((150 70) 0.85) + 70 = 138
bpm
Monitoring Endurance
Heart rate can give you a good
measure BUT because older adults
may have multiple disease processes
ongoing, in addition to medications,
that it is best to use the RPE!
ACSM 2010 has different HR
recommendations for different
diseases
9/10/2013
Anaerobic & Aerobic Exercise:
Body Composition
Reduces adipose tissue, visceral fat
Prevention & Rx of insulin resistance
syndrome, CVD, gall bladder
dysfunction, Type 2 diabetes, types of
cancer, hypertension, stoke, OA
Duration
Ranges 20-60 min (most 20-30 min)
Does not include warm up or cool
down
Typically inversely related to
intensity
May increase secondary to training
effect
Examples of moderate
intensity exercise
Fishing stand, cast
and walk along bank
Canoeing leisurely (24 mph)
Mowing the lawn with
walk behind power
mower
Home repair, painting
Frequency?
Range from 3-6 days /week to
2x/week
Dependant on intensity and duration
Dependant on functional capacity
Intensity
Cardiovascular
Moderate activity, total 30 min. per
day (sessions as short as 10 min.),
minimum 3 days/week
Requires 3-6 METS or 4-7 kcals/min
Examples of moderate
intensity exercise (cont.)
Walking briskly (3-4 mph)
Cycling leisurely (<10
mph)
Swimming with mod.
Effort
Doubles tennis
Golf, using a pull-cart
9/10/2013
Strengthening of the Older
Adult
Principles of Intervention
Overload
Task specificity
Adapt vs. challenge
Benefits
Prevent/slow strength decline
associated with aging
Decrease resting BP
Systolic 5mmHg,
Diastolic 3mmHg
Improved blood lipid profile
Weight loss
Improved wound healing
Increased bone density
Strengthening exercise
Why
Strengthening may be the most critical
parameter of exercise and may be
safer for people with
COPD (Simpson, 1992)
CHF (Pu et al, 2001; Levinger, 2005;)
Arthritis (Fransen et al 2002)
Than aerobic exercise. Especially in
the elderly.
Because aerobic exercise is typically
a whole body (running, swimming) or
minimally a half-body (cycling) which
requires a great deal of effort and
energy for an inactive person.
Strengthening is performed one
muscle group at a time for short
duration.
Loss of strength leads to:
Functional needs
Functional limitations
Gait speed LE power relationship
Bassey et al Clinical Science 1992
Sit to stand hip and leg strength
Gross et al Gait and Posture 1998
Falls risk of falls
Whipple et al JAGS 1987
Percentage strength requirements (leg
extension) in elderly
- 80% sit to stand
- 78% ascending stairs
- 88% descending stairs
- Frail 97% for sit to stand
Hortobagyi et al, J Gerentol Med Sci 2003
ADLs indices
Hyatt et al Age and Aging 1990
9/10/2013
Improved Psychological
Well-being
Participation in physical activity:
More positive psychological attributes
Decreased incidence and prevalence of
depression
Effects most noticeable in elderly with
co-morbidities
Muscle Mass and Aging
Overloading muscle can largely avert
losses of muscle mass and strength
Older men who lifted weight for 12-17
years > men 40-50 years younger
(strength)
PRE of 3-6 months can increase muscle
strength 40-150%, depending on subject
characteristics
Increase LBM (lean body mass) and
muscle fiber by 10-30%
Overload
Overload
Must be individualized and applies to:
Muscle strength is best developed by
using weights at levels that evoke
nearly maximal muscle tension with
relatively few repetitions
Any overload will result in strength
development, but higher intensity
effort at or near maximal effort will
produce a significantly greater effect
Intensity
Duration
Frequency
Speed
Intensity
Older adults gain strength similarly to the
young
2-3x in strength in 3-4 months, 11.4% in
muscle area (Frontera 1990, Fiatarone 1994)
Strength with 60-100% 1RM training
(McDonagh & Davis 1984)
Overwhelming evidence that low intensity
produces only modest gains in strength
With 80% 1RM significant gains even in the
very old (Fiatarone 1990, Evans 1999)
High intensity is safe even in the frail elderly
Relationship between strength
& Function
Leg power is powerful predictor of
functional decline (Mazzeo et al 1990)
Walking speed and LE strength
strong predictor for SNF placement
(Guralink et al, 1994)
Loss of LE strength strongest single
predictor for institutionalization
(Judge et al 1996)
10
9/10/2013
Functional strength vs.
Absolute strength
Power & Function
Often a deficit between the two
Functional strength is
usable/integrated strength and
incorporates velocity (force x velocity
= power)
Increasing functional strength
increases absolute strength
Training functionally meets the criteria
of specificity
Power was a better predictor of
physical function than isometric or
isotonic strength (Bean et al 2003)
Leg power and self-report of physical
activity had strongest correlation
with function (Foldvari 2000)
Frequency
Frequency/Duration/Intensity
ASCM: 2-3x/week
48 hour rest
Task Specificity
Low resistance, high reps lead to
endurance improvement (increase in
mitochondria), but little change in strength
(Moffroid & Whipple)
Important for function
2x/week gives 80-90% all strength
gains in untrained individuals
(compared to up to 6x/week)
1 set as effective as 2 or 3 (with proper
intensity)
75-85% of 1 repetition max
8-12 reps (set must go to muscular
failure)
1 set saves time/better compliance
Specificity
The more frail the more important
May be an alternative to intense
resistance (Page, 2003)
Multiplanar
Balance dominated
Asymmetrical
Velocity specific
Progressive
Eccentric (stairs, transfers)
Open or closed kinetic chain
11
9/10/2013
Function
Specificity includes functional task
training
Patient-centered (driven)
Meaningful
Progression
Try to keep load at 80% 1RM, 8-12
reps
Typically reps then load
McCartney 1996 suggests q 2week
eval
Early strength gains 10-15%/week
first 8 weeks may be due more to
neural factors
(Evans 1999, Bemben & Murphy 2001,
Phillips 2000)
Flexibility
ACSM recommends flexibility
training in older adults esp. shoulder,
neck, upper & lower trunk, and hip
regions.
Freland 2002 suggests hold for 60
sec in older adults
Injury
NO evidence to support higher rate
of injury in elders with intensity
(Rooks 1997, DiFabio 2001, Barnard 1999,
Coleman 1996)
No adverse cardiac events with high
resistance or Valsalva maneuver
(Gordon 1995, McCartney 1996, Barnard
1999, Vermill 1999, Kaelin 1999)
How many exercises
Henry et al, 1998 looked at elder
compliance
Study looked at 2, 5, 8 exercises
2 ex group had best compliance
ACSM recommendations
5-10 minute warm-up includes
stretching
30 min/day 3x/week
Walking bicycling, swimming, running
Resistance training: use proper body
mechanics (quality not quantity)
Include large muscle groups
Cool-down with stretching
12
9/10/2013
Summary of strengthening for
the elderly
< 5 exercises
1-3x/week
1 set, 80% 1rep max
8-12 reps
Considerations for power, eccentric
loading, closed/open chain, and
functional/task training
Summary
Several major research studies have considered
the numerous factors that seem to predict the
need for eventual institutionalization, and LACK of
leg strength was found to be the single most
important predictor. Not blood pressure, or heart
disease, or diabetes, or arthritis but rather leg
strength. The lesson is clear. If you want to avoid
the nursing home, youd better take good care of
your legs.
Walter M Bortz II MD, Professor Stanford University
Fun facts for home ex
Chronic Diseases Amenable to
Exercise
Soup can = lb
Can of tomatoes = 1lb
Jar peanut butter = 2 lbs
Bag of sugar = 5 lbs
Gallon of milk = 8 lbs
Lack of exercise contributes to chronic
disease:
Chronic Diseases Amenable to
Exercise
Prevention of Chronic Disease and
Increased Longevity
Exception: Progressive Diseases of
the CNS
However:
Lack of physical activity exacerbates
symptoms and hastens loss of
functional mobility
CVD
Stroke
Type 2 Diabetes
Obesity
Hypertension
OA
Depression
Osteoporosis
Evidence that both healthy and
chronically ill are candidates for
preventive exercise
Preventive ex appropriate for:
Community-dwelling
Institutionalized
13
9/10/2013
Adverse Effects of Exercise:
Adverse Effects of Exercise:
Community, Institutional Settings
Experienced Senior Athletes
Rare
Associated with
increase in activity
that is too sudden
and not gradual
Hamstrings, feetmost common
areas
Improper footwear
Walking programs
Jogging programs
Weight lifting (very
rare)
Adapt vs. Challenge
First responsibility is to make pt.
safe
After that need to increase challenge
Remember what is needed for
community living
Challenge with
Changing surfaces, uneven
Obstacles
Impose activities with gait
Increase speed
Complex gait activities
Heel/toe walking
Side-stepping, cross-overs, braiding
Tandem, backwards
Strains most
common
Hamstrings, calf,
adductors,
quads
Rotator cuff
muscles and
tendons
Sprains
Ankle
Knee
Fractures
Rare,
associated
with cycling
Strength changes
Early effects of ex:
Deconditioned-Neural Adaptation
(therapy)
Long-term effects of ex:
Stronger-Hypertrophy (fitness)
Age-related Musculoskeletal
Changes that affect exercise
Muscle mass and strength
Decreases 30% between ages 60-90
Muscle fiber
Type II decreases 50% between 60-90,
decreases 1% per year after age 30 with no
exercise
Motor unit
Decrease recruitment
Speed of movement
Decreases
14
9/10/2013
Age Related Changes
Bone
Tensile strength decreases, by age 70 a
decrease of 10-15% peak bone mass
Joint flexibility
Reduced by 25-30% over the age 70
Tendons
Cells
Rate of cellular division decreases
and becomes irregular
The functional effectiveness of
enzymes within the cells does not
diminish with age
Become less elastic and easier to tear
Cartilage
Collagen fibers increase cross-linkage
increasing the density of tissues reducing
movement
ELASTIN FIBERS
GLYCOPROTEIN
Dehydrate and increase cross
linkage with age
With the decreased elasticity, the
fibers become rigid and frayed
Elastin fibers are ultimately replaced
with collagen fibers which decreases
mobility leading to shortening and
distortion of the tissue
Production and release of
glycoprotein results in dehydration
of tissues
Results in water content decrease in
muscles and tendons causing
stiffness and rupture at less stress
than in younger ages
HYALURONIC ACID
Regulates the viscosity of tissues to
decrease friction between tissue
layers with movement
As this secretion decreases, greater
friction occurs resulting in the wear
and tear between tissues
MUSCLE MASS Age Changes-
Sarcopenia
Between age 20 and 80:
20-30% muscle mass loss occurs
Greatest loss is between 50 -80 years of age
Muscle strength decreases 15% per decade
between 50-70
Muscle strength decreases 30% between 70-80
Muscle mass is replaced by fat and collagen
deposits resulting in no change in overall girth
or volume measurements
15
9/10/2013
Muscle Fibers
Muscle Mass changes
As muscle fibers are lost, remaining
have to work harder to produce the
same force
Energy demands are raised resulting
in fatigue and decreased endurance
Muscle fiber hypertrophy can occur
in remaining fibers to increase
strength and function in even the
very old
Begins at age ~40: muscle mass will
decrease .5-1%/year over youth size
By age 75: there is ~30-40% decrease
in muscle mass
As one ages there is an increase in
fat and a decrease in Muscle mass
Muscle vs. Fat
CARTILAGE
As muscle fibers are lost, fat is
deposited
Fat is not as metabolically active as
muscle
Older people gain weight easier than
young
The collagen in cartilage holds less
water with age
The rate of collagen and elastin
synthesis decreases resulting in
dehydration and stiffness
fraying of cartilage.
CARTILAGE
With loss of movement, nutrition to
cartilage is reduces resulting in
thinning of cartilage and less ability
to dissipate forces across joints:
Results in damage and friction
leading to tearing and fraying of
cartilage.
Age Changes
COLLAGEN CHANGES
Main supportive protein in skin,
tendons, bone, cartilage, and
connective tissue
As we age, collagen becomes:
Irregular in shape
Less uniformed, less parallel in nature
Less mobile and slower to respond
cross linkages
nutrient movement thru tissues
16
9/10/2013
Review
MUSCLE STRENGTH DECREASE
100
Normal change
90
80
70
60
50
40
Inactive
30
Slow Twitch Type I muscles are
highly oxygenated and used in ADLs
Fast Twitch Type II muscles are used
in more intense activity/resistance
training
20
10
0
20
30
40
50
60
70
80
90
Motor Unit Level:
Decrease number of motor neurons
Decrease number of muscle fibers
Type II decreases more rapidly than Type I
By age 75, there is more Type I fibers
than Type II, EVEN in Senior athletes
Typical Changes with Aging
Reduced flexibility in the lower
extremity joints
Decreased strength of the ankles,
knees and hips
Less control of momentum
Decreased coordination and
Typical Changes with Aging
Decreased reflexes and increased
reaction time
Vision and sensory changes
Gait: slower speed, shorter step,
narrow stride width
Balance
Static:
Decreased as a result of decreased
ankle strength
Dynamic:
Decreased hip, ankle and stepping
strategies
Increase use of sway
Sway accounts for dynamic balance
in 80 y.o 50 % more than in 40 y.o.
17
9/10/2013
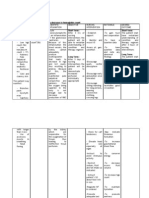
Changes
All the changes combine to cause
impairments, functional limitations
and disability
Disease/Impairment
Functional
limits/disability
1.Decrease muscle strength
Deconditioning/falls
2.Decrease aerobic capacity
Deconditioning/falls
3.Vasomotor instability
Baroreceptor insensitivity
Syncope/dizziness
4.Decrease total body H2O
Dehydration
5. Decreased bone density
Fracture risk
6. Fragile skin
Wounds
7. Altered thirst, taste, smell
Dehydration/malnutrition
Evidence
Do strength/ROM relate to function?
YES!!!!!
Musculoskeletal impairments (LE
strength and ROM), have a strong
relationship to function, especially in
older adults.
Beissner KL, et al., Muscle Force and Range of
Motions as Predictors of Function in Older Adults.
Phys Ther 2000. Jun;80(6):556-63.
Functional
Changes
Posture:
Tight knee flexors
Tight hip flexors
Increased lumbar
lordosis
Tight Pectoral
muscles
Evidence supports the idea that
exercise can overcome some of
these impairments and limitations!
Evidence
High intensity training.not just for
the young!
Average of 174% strength gains after
8 weeks of high intensity training.
This correlated improved mobility to
residents up to 96 years old!
High-Intensity Training in Nonagenarians. Effects on
Skeletal Muscle. Fiatarone M, et al., JAMA June
1990. 263(22):3029-34.
18
9/10/2013
Dynamic Exercise
Light work:
Works only Type I muscle fibers
Good for cardiac patients to start
Heavy work:
Works Type II muscle fibers
First 2 weeks it is the neural component
that is stimulated
Work at 80% of 1 rep max
Exercise and pathology
Skeletal Changes affecting
Exercise
The breakdown and eventual loss of
the cartilage of one or more joints
Osteoarthritis occurs when the
cartilage begins to fray, wear and
decay. In some cases, all the
cartilage wears away leaving the
bones of the joint to rub against each
other.
1 in 4 will develop symptomatic hip
OA by age 85; women> men
Falls
Depression
Cardiovascular
& pulmonary
CVA
Parkinsons
OA: S&S
OA
Osteoarthritis
TKA, THP
Hip fracture
Osteoporosis
Frailty
Stiffness
Joint pain
Crepitis
Inability to perform tasks
These can range from mild to severe.
Pain with weight bearing
Palpable warmth
Bony enlargement
Osteoarthritis
Muscle weakness contributes to
symptoms (esp quads) 2o joint reaction
forces
Adults > 65 with chronic knee pain
experience significant declines in
balance and LE strength over 30 month
period (Messier 2002)
19
9/10/2013
OA
Osteoarthritis
OA afflicts 20 million
Obesity risk by almost 2x
THR, TKR on the rise
2004: 431,485 TKR; 225,900 THR
2015: 1.4M TKR; 600,000 THR
Medicare wont be able to pay for all
these!
New guidelines! Require exercise
Osteoarthritis
Strongest quads show less knee
cartilage loss (Amin 2006)
Patellar/shoulder taping: reduces pain
and allows increase in function
(Quilty 2003, Hinman 2003)
Proper alignment is vital to PRE
Walking, jogging, recreational ex.
Does not risk of OA (Felson 2007)
Obesity increases risk, but no extra
increase with exercise
Differentiating age-related changes
from osteoarthritic changes
Age Related Changes
OA
Cartilage
Decreased
hydration
Increased
hydration/swelli
ng
Subchondral
Bone
Thinning
Thickening
Synovium
No Change
Swelling
proprioception contributes to
development of OA
Programs that incorporate
proprioceptive training with
strengthening decrease symptoms
better
OA
PACE: People with Arthritis Can Exercise
Program
8 weeks: decreased pain & fatigue, increase
in function (chair stand, 10# lift), increased
self-efficacy.
program that focuses on stretching,
flexibility, balance, low impact aerobics, and
strength training exercises
CDC funded
http://www.cdc.gov/arthritis/funded_science/projects/
pace-people-with-arthritis-can-exercise.htm
OA
The majority of persons over the age
of 65 and 80% over the age of 75
have radiographic evidence of OA in
at least one joint.
Can affect any joint; most commonly
seen in the hands and weight bearing
joints primarily the hips and knees.
20
9/10/2013
OA
Exercise and OA
The proper exercise program for the
elderly individual needs to consider
any underlying pathology and
modified for successful results
Strengthening ex pain, function
Exercise in water has been shown to
reduce pain.
Proper footwear pain
Musculoskeletal aging
Changes in cell and
tissue function
Sarcopenia
Joint laxity
Musculoskeletal underuse/misuse
Lack of exercise
Abnormal joint loading
TJR
Joint replacement is a last step when:
Musculoskeletal dysfunction
Risk Factors
Obesity
Joint instability
Joint injury
Genetics
Anatomy
The risk of immobility is greater than
the risk of exercise and can lead to
further aging changes.
Stronger muscles generally reduce
stress on the joint surfaces by
correcting abnormal biomechanics
Exercise can initially increase the
symptoms but not cause an increase
in the damage to the joints
OSTEOARTHRITIS
Total Knee Arthroplasty
Quad strength 62% from pre-op. at
1 month post-op
4%/day with immobilization
With high intensity ex can return to
pre-op in 2 months (Mizner 2005)
Walking and stair climbing is difficult
Pain at rest and at night is not controlled
6-week presurgical ex program can
improve post-op status (TKA & THR);
and reduce odds of requiring inpatient
rehab stay
Rooks et al. Arthrits Rheum.
2006.15;55(5):700-8.
Evidence
Strengthen quads, including leg
press if FWB
If significant quad insufficiency
present, add e-stim for 1st 6 weeks
21
9/10/2013
Gender Bias
Study from Canadian Med Assoc J.
March 2008
Orthopedic surgeons were 2x more
likely (33% to 67%) to recommend TKR
to men over women with same
symptoms
Hip Fracture
Total Hip Arthroplasty
At one year 10-18% strength deficit
around hip (Trudelle-Jackson 2004)
Hip abductor strength directly related
to return to home, risk for falls,
function, gait status
Hip Fracture
75% fail to return to previous level (Weinrich
2004)
At 2 months post: (Magaziner 2000)
98% had some dependency walking 10 feet
At 6 months post: (Magaziner 2003)
Only 8% climbed a flight of stairs
15% could walk across a room independently
6% could walk half a mile
At 24 months:
50% still had difficulty walking 10 feet independently
Hip Fracture
Post: 53.3% fell, 62,5% of these fell >2x, 18%
sustained injuries requiring re-hospitalization
Predictors for fall 6 months post (ShumwayCook 2005)
Previous use of assistive device 3.15x
Hx one fall prior to fx 8.77x
At 2 years post (Norton 2000)
4x more likely to be homebound
3x more likely dependent for ADLs
The more PT in hospital the better mobility 2
months later. (Penrod 2004)
Hip Fracture
At 8-12 weeks moderate stability
from bone callus is achieved
Time to begin aggressive strengthening
and wean from assistive device
(Weinrich 2004)
High intensity exercise for 3mo & 6
mo have been shown to gait speed,
distance, balance and function
(Binder 2004, Mangione 2005)
22
9/10/2013
Issues for acute hip injury
SLR
Greater stress on hip joint with SLR than
normal unsupported gait (Strickland
1992)
SLR = 3x body weight
Maximal isometric abduction greater
peak pressures than SLR or unsupported
gait. (Krebs 1991)
Issues for acute hip injury
Forces of hip abductors during gait =
2.5x body weight
Forces on hip joint during stair
climbing = 7x body weight
Forces on hip during
running/jumping = 10x body weight
Davy et al 1988
Spinal Stenosis
Spinal Stenosis
Degeneration of the intervertebral disc
which results in collapsing of the disc.
The collapsed disc and subsequent facet
arthrosis narrows the neuroforamen and
compresses the nerve root.
The ligamentous laxity causes vertebral
subluxation and osteophyte formation
resulting in spinal stenosis
The neuroforamen is narrower with
lumbar extension than with flexion.
The patient with spinal stenosis will
prefer to sit and flex versus standing
with extension.
The obstruction can also impair
cerebrospinal fluid circulation and
produce the neuroischemia.
Spinal Stenosis
S&S
Spinal stenosis primarily reflects disc
and facet degeneration but as time
progresses,
Spondylolisthesis can occur.
Costs $1 billion annually
Slow progression of disease
Numbness, weakness, cramping,
pain in Les, feet, buttocks
Compresses spinal nerves
Similar to disc
Stiffness in LEs
LBP
Decreased LE sensation
Loss of bladder and bowel function
in severe cases
23
9/10/2013
S&S
Often have absent lordosis
Stooped posture when standing or
walking
Prefer to use walker, grocery cart,
w/c to enable forward lean
This can increase risk for falls
Intervention
Aerobic conditioning utilizing a
stationary bike/treadmill
Aquatic exercise to reduce the stress
on the spinal joints.
Manual stretching, muscle
strengthening
Flexion decreases symptoms,
extension aggravates
The goal of should be 30 minutes of
exercise 3x/week.
Intervention
Pharmacological Interventions:
NSAIDS ; Lodine; ibuprofen
Analgesics:Hydrocodone,
acetaminophen
Education on proper body
mechanics
Restriction of aggravating activities
Spinal stabilization
Later Interventions
Epidural Steroid Injections
short term relief only
success rates are only 85%
The best results seem to occur with patients
who have had decompression surgery at one
or two levels and no spondylolisthesis
Surgical Decompression
laminectomy
X-STOP IPD procedure: less invasive, metal
implant that limits spinal extension
Complications
Osteoporosis
Patients with osteoporosis and
spinal stenosis will often develop a
compression fracture proximal to the
fusion.
Pelvic fractures are often seen after a
lumbosacrel fusion due to the
increased stress on the pubic rami
during rotation
A disease characterized by low bone
mass and structural deterioration of
bone tissue, leading to bone fragility
and increased susceptibility to
fracture.
24
9/10/2013
Bone Basics
Bone Basics
Bone grows in length up to age 25
Osteoblasts can continue to lay down
new bone until age 30
10-15% of skeleton is demineralized and
can be renewed each year
Osteoclasts take calcium out of blood to
put in blood stream
Osteoclasts take out in one month what
osteoblasts takes 3 months to replenish
Bone mass accounts for 75-85% of
bone strength
25 year olds absorb 75 % of available
calcium, 60 year olds 30-40 %
Physical inactivity can lose 1 % of
bone mass/week
Trabecular bone loss begins age 30-40
Cortical bone loss begins age 40-50
Bone Remodeling Cycle
Type I (post menopausal)
Osteoclast activity: bone
breakdown
Osteoblast activity: bone
formation
Normal balance =
turnover of 10% cortical
and 30-40% trabecular
bone remodeled per year
Trabecular Bone
Trabecular bone loss is 3x the
normal loss
Bone loss is greater in first 5 yrs
after menopause
10-15 yrs after menopause the loss
rate decreases
Most associated with vertebrate and
wrist fractures
Type II (age related)
Loss beginning at age 30
At age 40:
less bone is formed than is reabsorbed
loss is .3-.5 %/yr.
Decrease ability to absorb calcium
Associated with hip fracture
25
9/10/2013
Height
Disc height maintains or slight
increases with age
Does decrease during day, but
replenishes at night
Osteoporosis - Diagnosis
Through Bone Scan
Visualization
Arm measurement
Loss of height is a decrease in
vertebral height (body of
vertebrate)as a result of decrease
bone mass not disc
Men DO get osteoporosis
A major public health threat:
1-2 million in U.S.
8-13 Million have osteopenia
500,00 hospital admissions (fx)
Men sustain 25-30% of hip fractures
Associated with low testosterone
Healthy People 2010 identifies this as the
second focus area to address to improve
the quality of life in the USA
44 million Americans have the disease or
have low bone mass (osteopenia)
Occurs in both men and women
Arch Intern Med. 2008;168:47-54
Mortality rate is 2x
Article on Blackboard
A major public health threat:
Affects the physical independence in
daily activities
Responsible for 1.5 million fractures
annually
Direct expenditures as a result of the
fractures at $13.8 billion/year and rising
4x more likely in women. 1 in 12 men (low
estrogen)
Affects all age groups and ethnic groups
Pharmacological Interventions: To
slow bone loss
Fosamax/Boniva: in both men and
women
Actonel: in women and men
Raloxifene: in women, selective
estrogen receptor modulator
Calcitonin: in postmenopausal
women greater than 5 years and
relatively healthy
26
9/10/2013
Some problems
Use of bisphosphates (Actonel,
Fosamax) is linked to bone necrosis,
esp. jaw.
Journal of Rheumatology .Feb 2008
Fosamax may also cause chronically
irregular heartbeat (atrial firillation)
by 86%
Fractures
Fractures are more highly related to
decrease bone mass than any other
age related factor
Most common fractures (in order):
vertebral, hip, wrist
Arch Int Med. Feb 2008.
Fractures
Femoral neck
ORIF: poorer outcomes than
hemiarthroplasty
Hip fractures: DM = higher risk
despite higher BMD (bone mineral
density) (higher body weight?)
Visual impairment?, sensation?,
CVD?
Diabetes Care 2007;30:835-41.
Surgeries
THR, ORIF
Vertebroplasty: for comp. fxs
Lab
Flexicurve video
Injection of cement
+/- risk for adjacent fx
27
9/10/2013
Research shows:
Exercise can gain bone mass
dynamic bone loading exercises of
walking, jogging and stair climbing
Strength training stimulates bone at the
muscular skeletal junctions
Rest periods to prevent desensitization
may double anabolic responses to
mechanical loading
Evidence
Significant relationships were recorded
between dynamic leg strength and BMD of
the femoral neck and lumbar spine
Effects of one-year of resistance training on the
relation between muscular strength and bone
density in elderly women. Rhodes. Br J Spts Med.
2000
Contraindicated exercises include
vertebral flexion exercises
Osteoporosis
Resistive exercises appear to
increase bone mass density
Increase back muscle extensors
Women with weak back extensors are
2.7% more likely to suffer a
compression fracture
Exercise
May work best to build bone during
bone growth, with some lasting
benefits, but may erode away when
exercise stops
In adulthood, small increments
No evidence that ex fractures
Issues for osteoporosis
Avoid trunk flexion, especially with
resistance
Careful with dynamic body weight ex.
28
9/10/2013
PT Intervention
BEST exercise program
AGING JOINTS
Designed at Johns Hopkins
http://www.citracal.com/best/
Exercise videos
Foot/Ankle
Knee
80% of people 65 and older have foot
dysfunction
Loss of flexibility of the ligamentous
structure between the 26 bones of
the foot
Decrease range of motion and shape,
therefore the reason to measure your
foot when buying new shoes
Decreased ankle strength affects
balance and mobility
Degenerative changes in weight
bearing joints increases and the knee
changes are 2x as common as the
ankle or hip
Women have a 50% greater strength
loss and greater magnitude of varusvalgus deformity than men possibly
due to the decrease in estrogen after
menopause
Hip
Hip
The weight bearing surface of the hip
is covered with cartilage which crack
and shred over time resulting in
fissures
Degenerative joint disease and hip
bursitis are the common complaints
The synovial membrane thickens and
are less mobile unable to protect the
joint
Common findings include: hip
flexion contractures, weakness,
iliotibial band contractures, and
disuse atrophy from habitual sitting
60% of gait cycle is in stance and
35% in one legged stance, therefore
hip instability and weakness will
affect gait
29
9/10/2013
Spine
Cervical Spine
The spine tries to stabilize itself with
bone remodeling resulting in bone
spurs or widening of the vertebral
body
Postural changes as result of
tightening of the pectoral muscles
and habitual sitting
The disc changes by a decrease in
size and number of the collagen
resulting in less elasticity, and
posterior migration which begins the
forward head posture
Long anterior neck muscles shorten
and the suboccipital muscles tight to
keep head in vertical alignment
Cervical Spine
Shoulder
Decrease cervical range of motion
can begin as early as age 30
Bifocals/trifocals, pillows for
sleeping, computer usage can all
contribute to neck changes
Shoulder pain is more frequent in
women than men
Deltoid muscles are the most
overworked and rotator cuff the least
worked of all shoulder muscles
Shoulder
Hand
Decrease supraspinatus strength
results in superior migration of the
humerus and ultimately impingement
in the subacromial region
Increased thoracic kyphosis as a
result of back changes increases
shoulder problems.
Multitude of small joints, cartilage,
and muscles predisposes the hand
to aging effects
Routine daily stresses on the joints
of the hands add up over time
Joint protection techniques, utilizing
larger joints, energy conservation
and pacing all help to reduce hand
dysfunctions
30
9/10/2013
Frailty
Definition: 3 or more
Unintentional wt loss of > 10 lbs in last year
Self-reported exhaustion
Weakness (lowest 20% grip strength for
age
Slow walking speed (lowest 20%)
Low physical activity
1-2 of these factors signal intermediate
frailty with risk to become frail in 3-4
years (Fried 2001)
Frailty and Resistance
Exercise
Resistive ex in hospital improved
strength, sit to stand. Gait speed and
4 of 6 non-ambulatory pts. Became
ambulatory (Sullivan 2001)
Falls
Decreased incidence of falls for
those placed on exercise programs
Resistive ex.
Balance ex.
Tai Chi
Xi Gong
Yoga
Frailty and Resistance
Exercise
Appears to be a major weapon to
combat frailty
80% 1rm:
174% in 90+ older adults 3x/week for 8
weeks; 3 sets of 8 (1st week 50%)
227% gain knee flexor, 107% gain knee
extensors
Evans 1999
Falls
Resistive exercise increases balance,
gait velocity, climbing power and sit
to stand
Depression
Mod high intensity exercise improves
self scores
Depression doesnt limit gains from
physical activity
Singh 2002
More about this in lecture 5
31
9/10/2013
Cardiovascular Disease
Resistance exercise may be more
tolerable that aerobic exercise if
ischemic threshold is low due to
heart rate response to training
COPD
Exercise improves muscle strength
and endurance, dyspnea, QOL
CHF
No longer contraindicated, but must
monitor vitals signs
Diabetes
Resistance exercise is as, if not more
effective than aerobic ex. in
improving glucose intolerance and
risk reduction
COPD
Fewer repetitions are tolerated
better, single set, 2-3x/week.
Progress from 50% to 80% 1RM
Time exercise sessions after
bronchodilator med peak
Use oxygen as needed
Monitor vitals, RPE (Borg)
CVA
Overload principle (Weiss 2001)
One-year s/p
12 weeks, 2x/week, 70% 1RM
68% increase in strength, 12% balance,
sit to stand improved
Treadmill supported gait
32
9/10/2013
Parkinsons
Parkinsons
Rigidity leads to flexor
muscle and soft tissue
shortening, extensor
muscle and soft tissue
lengthening
Exaggerated exercises
Forced exercise
Boxing training
http://ptjournal.apta.org/content/suppl/2
010/12/29/91.1.132.DC1/Combs.mov
Relaxation exercises
Strengthening increases
stride length, LE strength,
gait velocity, head angle
8 weeks, 60% 1RM (Goede
2001)
Causes of Inactivity in
Seniors
Causes of Inactivity
Lack of motivation or apprehension
Lack of resources, or knowledge of
them
Social/cultural issues
Environmental barriers - e.g.,
equipment, room to exercise, place to
walk, transportation
Inability to assume positions/postures
Exercise and Older Adults
Inactivity Increases with Age
Percent
50
70-79
80+
40
Benefits of ex., proper methods for performing
ex.
Today, about 28% to 34% of adults 65
to 74 and 35% of adults 75 years and
older are INACTIVE.
By 2030, demographers expect the
number of older people to double,
from 35 million to 70 million.
70-79
60-69
10
0
Muscle soreness, shortness of breath
Lack of knowledge
60-69
30
20
Falling, getting injured, not doing it right
Acute illness
Co-existing diseases/disabilities
(incontinence)
Unpleasant sensations associated with
exercise
Inactivity
80+
60
Fear
Men
Women
33
9/10/2013
Factors that Improve Exercise
Adherence in Seniors
Motivation is the best discriminator for
older adults who enroll and adhere to
and/or drop out
Strategies to improve motivation:
Effective exercise leader
Continuity
Type of program variety, cross-training
Have FUN!!
Self-efficacy
Expected outcomes
Exercise Leader
KEY TO SUCCESS IS MOTIVATION!!!
Encourage participation, assess,
instruct
Demonstrate caring
Aware of participants differences
Well-organized
Able to establish rapport with group
Begin slow and advance slowly (to
avoid pain, SOB)
Individualized Programs
Individualized, even within groups
Some seniors prefer to exercise
alone
Find out who these individuals are
One-on-one interview
Customized program
Consulting/counseling
Assess: type/freq/intensity/duration
Advise: importance of ex
Agree: shared decision making
Assist: printed
materials/calendar/resources
Arrange: Follow-up/referral to specialist
Type of Exercise or Activity Programs
Group Programs
Strength Training
Walking
Yoga
Tai Chi
Feldenkrais
http://rehabyoga.com
Dancing
Qi gong
Chair w/c ex.
Floor ex.
Mechanical
Bicycles
Treadmills
Ellipticals
Stair steppers
Exercise and Aging
Regular exercise has been shown to
decrease morbidity in older adults
Despite this fact, less than 25% of the
older population exercises at
recommended level!
Only 37% of PT pts cont. HEP 6months
after D/C*
Why?
*Forkan Phys Ther 2006;86:401-410
34
9/10/2013
Barriers
Disability specialized
program/exercises from PT
Fear of injury/Falling initial
supervision 1 on 1
Habit need to incorporate into daily
routine
Lack of education
Income level
Barriers (cont.)
Environmental weather
Cognitive decline keep it simple
Lack of nutrition meals on wheels,
education
Ability to Manage
Perceived Barriers!
Self-Efficacy
Factors that affect self-efficacy:
Age
Gender
Previous experience
Take Care of the
Barriers to Exercise
Deal with Barriers
Fear!
Location
Transportation
Personally
appealing
Client-centered
goals
Opportunities for
success
Address
discomforts
Safety, falling
Address embarrassments
Encourage questions
Acknowledge each success
Buddy or partner system
35
9/10/2013
Deal with Barriers
Environment
Safe, pleasant, health-enhancing
Convenient
Societal/cultural issues
Customize Program
Outcome Expectations
Stronger outcome expectations
associated with starting exercise and
maintaining it
Clear and accurate
Realistic?
Favorite activities, specific goals
If co-existing disease/disability
Special for Seniors
Rely heavily on
instructor
Enjoy interaction
with a group, may
be more effective
(own age)
Contributes to
self-esteem
Physical Activity:
A Key to Wellness and
Successful Aging
Wellness
A lifelong interactive process of
becoming aware of and practicing
healthy choices to create a more
successful and balanced lifestyle.
How do I teach my seniors?
How do I stress the importance of
exercise?
How does a PT tell their
patients about the
importance of exercise?
36
9/10/2013
Physical Activity Improves
Intellectual Function by:
Helping maintain cognitive function
(e.g. memory and concentration)
Decreasing stress and anxiety
Improving mood
Reducing depression
How Do I Get Started?
Check with your doctor
Visit a physical therapist
Start slowly
Integrate different physical activity
components into your life
Choose activities you enjoy
Get a buddy
How Do I Choose an Activity?
Consider including multiple
components
Enjoyable
Accessible
Convenient
Variety
Physical Activity Improves
Social Function by:
Increasing independence
Creating a stimulating,
and often supportive,
environment
Improving family time
Increasing social
networks and
involvement
Getting Started
The National Institute on Aging has
published the 2009 version of
Exercise and Physical Activity: Your
Everyday Guide from the National
Institute on Aging. Best of all it is
free!
http://www.nia.nih.gov/HealthInforma
tion/Publications/ExerciseGuide/
Meeting Their Needs
Considerations for
group programs:
Class size
Instructor experience
Amount of assistance
they need
Intensity and variety of
program
37
9/10/2013
Physical Activity May Include:
Walking
Swimming or
participating in a
water exercise
class
Playing a sport you
enjoy
What If I Have Physical
Limitations?
Choose an activity that
accommodates your
abilities
Physical Activity May Include
Lifting weights or
exercising with
elastic bands
Taking a tai chi or
senior yoga class
Dancing
Joining a local
senior exercise
class
How Do I Begin a Physical
Activity Session?
Warm up for 10 minutes
Use something sturdy for
support
Use a cane or walker during
activities
Exercise sitting
Consult a physical
therapist to help you
choose an activity
How Much Time Do I Need to
be Active For?
How Much Time Do I Need to
Be Active For?
Warm-up should be followed by at
least 30 minutes of effortful physical
activity.
30 - 60 minutes a day of endurance,
strengthening, balance and flexibility
activities
38
9/10/2013
How Much Effort is Needed?
Begin slowly and
pace yourself.
How Do I Finish a Physical
Activity?
Finish your session with a 10
minute cool down and a tall
glass of water.
You should be able
to carry on a
conversation during
the activity.
How Many Days A Week
Should I Be Active?
How might I expect to feel?
Try to do 3x per week, more can be better
7
5
When you first begin a physical
activity program or advance your
current activities it is normal to feel:
Mild muscle stiffness, burning, or
fatigue that decreases in 24 hours
Mild increase in heart rate with
continued activity, but that returns to
normal in 5 minutes
3
1
Stop to Rest if You Experience
Shortness of breath
(cant complete sentence)
Dizziness
Heart rate that exceeds prescribed
target rate
Onset or worsening of pain
Chest pain
What Does Progress Look
Like?
Minor improvement
in 2-3 weeks
Significant improvement in 2-3
months
Can lead to improved
Lifestyle and function!
39
9/10/2013
Lifetime Goals:
Maintaining Fitness Level
Getting Back on Track
10% per week
Illness
Vacation
Injury
Lose gains
missed
Effort
Resume
when you
can
Speed
Be realistic
Be consistent
Find a buddy
Journal / chart progress
Distance
Pearls of Wisdom
Will you be
running a mini
when you are
82?
Summary
Aerobic/cardiovascular endurance
Substantial improvements in almost all
aspects of CV function
Muscular strength
Individuals of all ages and disease states
can benefit from PRE
Can help maintain independence
Balance and coordination
Prevents falls, improves gait
Other
Muscle training can hypertrophy
remaining Muscle fibers thereby
decreasing the Fat to Muscle ratio
Lower extremity muscle strength is
affected greater than upper strength
Remaining muscle still have endurance
unless co-morbidity is present
Strength training will improve balance
and decrease fall risk
Summary
Improved max aerobic capacity
Increased max voluntary ventilation
Greater A-VO2 difference and stroke
volume
Lowered vascular resistance
Increased muscle strength (slow and
reverse decline)
Reduced involutional bone loss
Increased bone mineral content
improves mental function, bone health
40
9/10/2013
Summary
Decreased body fat/increased lean
body mass
Improved glucose tolerance
Lower lipid concentrations &
elevated HDL
Improved flexibility
Improved balance
Decreased risk for falls
Improved functional performance
41
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Wearable Motion Sensors To Continuously Measure Realworld ActivitiesDocument12 pagesWearable Motion Sensors To Continuously Measure Realworld ActivitiesshivnairNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Wearable Sensors For Reliable Fall DetectionDocument4 pagesWearable Sensors For Reliable Fall DetectionshivnairNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Human Activity Monitoring With Wearable SensorsDocument9 pagesHuman Activity Monitoring With Wearable SensorsshivnairNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Low Cost Accelerometer SensorsDocument11 pagesLow Cost Accelerometer SensorsshivnairNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Wearable Sensors For Remote Healthcare Monitoring SystemDocument6 pagesWearable Sensors For Remote Healthcare Monitoring SystemshivnairNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Electronics Artists Photo Theremin AmplifierDocument5 pagesElectronics Artists Photo Theremin AmplifiershivnairNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Detecting Vital Signs With Wearable Wireless SensorsDocument27 pagesDetecting Vital Signs With Wearable Wireless SensorsshivnairNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Wearable Biosensors Presentation SummaryDocument9 pagesWearable Biosensors Presentation SummaryshivnairNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- An Amulet For Trustworthy Wearable MHealthDocument6 pagesAn Amulet For Trustworthy Wearable MHealthshivnairNo ratings yet
- Smart Wearable Body Sensors For Patient Self-Assessment and MonitoringDocument9 pagesSmart Wearable Body Sensors For Patient Self-Assessment and MonitoringshivnairNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Current Progress On Pathological Tremor Modeling and ActiveDocument6 pagesCurrent Progress On Pathological Tremor Modeling and ActiveshivnairNo ratings yet
- WOW - The World of WearablesDocument1 pageWOW - The World of WearablesshivnairNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Wearable Sensor Systems and Their Impact On Biomedical Engineering - Paolo BonatoDocument3 pagesWearable Sensor Systems and Their Impact On Biomedical Engineering - Paolo BonatoshivnairNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Occupational Therapy and Dementia-Specific ToolsDocument14 pagesOccupational Therapy and Dementia-Specific ToolsshivnairNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Life and Work in Shakespeare's PoemsDocument36 pagesLife and Work in Shakespeare's PoemsshivnairNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Rotary MotionDocument17 pagesRotary MotionshivnairNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Textile-Based Wearable Sensors For Assisting Sports PerformanceDocument5 pagesTextile-Based Wearable Sensors For Assisting Sports PerformanceshivnairNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Lessons in ElocutionDocument418 pagesLessons in ElocutionaquabuckNo ratings yet
- Analytics Reading ListDocument2 pagesAnalytics Reading ListshivnairNo ratings yet
- Cleaning & Disinfection Decontamination GuideDocument1 pageCleaning & Disinfection Decontamination GuideshivnairNo ratings yet
- Lectures On Political EconomyDocument69 pagesLectures On Political EconomyshivnairNo ratings yet
- Analytical Survey of Wearable SensorsDocument6 pagesAnalytical Survey of Wearable SensorsshivnairNo ratings yet
- The Auschwitz ProtocolDocument28 pagesThe Auschwitz ProtocolshivnairNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Predicting Cognitive Impairment in PDDocument292 pagesPredicting Cognitive Impairment in PDshivnairNo ratings yet
- Caudill 2008 Review of Sports HerniasDocument44 pagesCaudill 2008 Review of Sports HerniasshivnairNo ratings yet
- Fitness CountsDocument50 pagesFitness CountsLogan RunNo ratings yet
- What Cognitive Abilities Are Involved in Trail-Making PerformanceDocument27 pagesWhat Cognitive Abilities Are Involved in Trail-Making PerformanceshivnairNo ratings yet
- PDHBRev 09 Repr 10Document44 pagesPDHBRev 09 Repr 10dragonwNo ratings yet
- Scoliosis - Searching For The SpineDocument10 pagesScoliosis - Searching For The SpineshivnairNo ratings yet
- Cervical Cancer Literature ReviewDocument6 pagesCervical Cancer Literature Reviewaflskeqjr100% (1)
- Jadwal OktoberDocument48 pagesJadwal OktoberFerbian FakhmiNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Low Cost Portable Ventilator DesignDocument8 pagesLow Cost Portable Ventilator DesignRashmi SinghNo ratings yet
- Effectiveness of Homoeopathic Therapeutics in The Management of Childhood Autism DisorderDocument13 pagesEffectiveness of Homoeopathic Therapeutics in The Management of Childhood Autism DisorderShubhanshi BhasinNo ratings yet
- CHC VisitDocument48 pagesCHC VisitRamyasree BadeNo ratings yet
- Types and Causes of Phobias ExplainedDocument24 pagesTypes and Causes of Phobias ExplainedDebjyoti BanerjeeNo ratings yet
- Pathfit-1 2Document34 pagesPathfit-1 2Lathea Daiser TheaNise TesalunaNo ratings yet
- Esophageal CancerDocument3 pagesEsophageal CancerChanthorn SokNo ratings yet
- Prenatal CareDocument16 pagesPrenatal CareMark MaNo ratings yet
- Etiology of Eating DisorderDocument5 pagesEtiology of Eating DisorderCecillia Primawaty100% (1)
- The Complete Enema Guide: by Helena BinghamDocument10 pagesThe Complete Enema Guide: by Helena BinghamJ.J.No ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- CNS Drug StudyDocument4 pagesCNS Drug StudyMAHUSAY JOYCE CARINANo ratings yet
- PYQDocument2 pagesPYQAisyah OthmanNo ratings yet
- Case Study CKD DM Type 2Document7 pagesCase Study CKD DM Type 2Brian Cornel0% (3)
- Internal Medicine Mar 2022Document8 pagesInternal Medicine Mar 2022Sanielle Karla Garcia LorenzoNo ratings yet
- APA Eating Disorders Practice Guideline Under CopyeditingDocument139 pagesAPA Eating Disorders Practice Guideline Under CopyeditingIbrahim NasserNo ratings yet
- C105a Pre-Sea and Periodic Medical Fitness Examinations For SeafarersDocument4 pagesC105a Pre-Sea and Periodic Medical Fitness Examinations For SeafarersAbu ShabeelNo ratings yet
- Physical Education: Quarter 2 - Module 1: Strengths and Weaknesses in Skill-Related Fitness ActivitiesDocument19 pagesPhysical Education: Quarter 2 - Module 1: Strengths and Weaknesses in Skill-Related Fitness ActivitiesJoshua DoradoNo ratings yet
- AHA-ASA Guideline For Adult Stroke Rehab and RecoveryDocument73 pagesAHA-ASA Guideline For Adult Stroke Rehab and RecoveryAfifaFahriyaniNo ratings yet
- Acute Stroke TreatmentDocument77 pagesAcute Stroke TreatmentRohitUpadhyayNo ratings yet
- Phylum Class Order Genera: Apicomplexa Haematozoa Haemosporida Plasmodium Piroplasmida Coccidia EimeriidaDocument39 pagesPhylum Class Order Genera: Apicomplexa Haematozoa Haemosporida Plasmodium Piroplasmida Coccidia EimeriidaMegbaruNo ratings yet
- Guidelines For The Surgical Treatment of Esophageal Achalasia PDFDocument24 pagesGuidelines For The Surgical Treatment of Esophageal Achalasia PDFInomy ClaudiaNo ratings yet
- 1 - Spirometry Simplified With CRF's PEFR PDFDocument80 pages1 - Spirometry Simplified With CRF's PEFR PDFyayatiNo ratings yet
- Division of Tropical Medicine and Infectious Diseases at Gatot Soebroto Central Army HospitalDocument63 pagesDivision of Tropical Medicine and Infectious Diseases at Gatot Soebroto Central Army HospitalAggiFitiyaningsihNo ratings yet
- Brain: What Is A Subarachnoid Hemorrhage?Document4 pagesBrain: What Is A Subarachnoid Hemorrhage?Rashellya RasyidaNo ratings yet
- Nursing Management A. Nursing Care PlanDocument12 pagesNursing Management A. Nursing Care Planmabzbutterfly69% (13)
- HomeopathyDocument33 pagesHomeopathyPriya Illakkiya100% (2)
- Nursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"Document9 pagesNursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"jhonroks100% (7)
- Cardiovascular Physiology Applied To Critical Care and AnesthesiDocument12 pagesCardiovascular Physiology Applied To Critical Care and AnesthesiLuis CortezNo ratings yet
- Discharge PlanDocument2 pagesDischarge Plankim arrojado100% (1)
- The Yogi Code: Seven Universal Laws of Infinite SuccessFrom EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessRating: 4.5 out of 5 stars4.5/5 (104)
- Chakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.From EverandChakras and Yoga: Finding Inner Harmony Through Practice, Awaken the Energy Centers for Optimal Physical and Spiritual Health.Rating: 4 out of 5 stars4/5 (2)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingFrom EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingRating: 4.5 out of 5 stars4.5/5 (66)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (110)
- Wall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesFrom EverandWall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesNo ratings yet
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindFrom EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindRating: 4.5 out of 5 stars4.5/5 (1)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerFrom EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerRating: 4 out of 5 stars4/5 (5)