Professional Documents
Culture Documents
Fungal Diseases of the Skin: Types, Causes and Treatments
Uploaded by
putraimanullahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fungal Diseases of the Skin: Types, Causes and Treatments
Uploaded by
putraimanullahCopyright:
Available Formats
Go Back to the Top
Chapter
25
To Order, Visit the Purchasing Page for Details
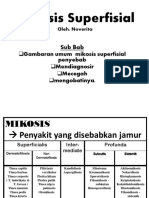
Fungal Diseases
Fungi are eukaryotic microorganisms that have a cellular wall and do not photosynthesize. They parasitize
organisms or exist as spores. In superficial mycoses, fungi invade keratinized tissue such as the horny cell
layer, hair and nails. In deep fungal infection, fungi tend to parasitize the dermis and deeper layers.
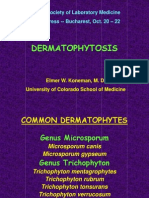
A. Dermatophytoses
Table 25.1 Classification of dermatophytes.
Trichophyton
T. rubrum
T. mentagrophytes
T. verrucosum
T. violaceum
T. schoenleinii
T. tonsurans
T. concentricum
T. equinum
Microsporum
M. canis
M. gypseum
M. audouinii
M. cookei
M. equinum
M. ferrugineum
M. gallinae
M. nanum
Epidermophyton
E. floccosum
Table 25.2 Classification of tinea.
Tinea superficialis
25
Tinea pedis
Tinea unguium
Tinea manus
Tinea cruris
Tinea corpooris
Tinea faciei
Tinea capitis
Tinea incognito
Tinea profunda
Kerion celsi
Sycosis trichophyica
Granuloma trichophyticum
Trichophytid
Outline
They
are caused by dermatophytes that parasitize the
skin, the horny cell layer in particular.
They have various common names, depending on the
affected site. The main subtypes are tinea pedis (commonly called athletes foot; it accounts for more than half
of tinea cases), tinea capitis (scald head, which occurs
frequently in childhood), tinea corporis (serpigo, which
heals in the center to present a ring shape or lesion) and
tinea cruris (jock itch, which involves the genitalia).
The causative dermatophyte is microscopically identified
from scales of the lesion or nail using KOH solution.
The treatments are topical or oral antifungal agents.
Classification
Fungi called dermatophytes parasitize the horny cell layer,
causing dermatophytosis. Dermatophytes are divided into three
genera, each with various species (Table 25.1). The most common dermatophytes are Trichophyton rubrum and Trichophyton
mentagrophytes.
Because dermatophytes feed on keratin, they usually infect the
epidermal horny cell layer, nails and hair follicles, causing
lesions (tinea superficialis). Dermatophytosis in which dermatophytes proliferate in the dermis and deep dermal layers is called
tinea profunda (Table 25.2). The name of the dermatophytosis
differs by the location.
Laboratory findings, Diagnosis
Diagnosis of dermatophytosis is confirmed when dermatophytes or segmental spores of 3 mm to 4 mm in diameter containing septum are found microscopically with KOH solution in a
specimen taken from a scale, blister covering, nail or hair (Figs.
25.1 and 25.2). For observation by light microscopy, a specimen
is placed on a slide glass with 1 or 2 drops of 20% KOH solution
and then covered with glass and heated for a few minutes. Use of
DMSO-added KOH solution makes rapid microscopic examination
468
A. Dermatophytoses
469
possible, because heating is unnecessary. Microscopy with KOH
solution is always used when dermatophytosis is suspected.
Other major tests are culture in Sabourauds glucose agar for
color tone and morphological observation of the colony, morphological observation of conidium by slide culture, molecular examination by PCR or in situ hybridization, and regular
hematoxilin-eosin stain.
Treatment
The basic treatment for all sites infected with tinea superficialis except hairy areas is topical application of antifungal
agents such as imidazole. For tinea superficialis in hairy areas,
intractable tinea, and tinea profunda with cutaneous and subcutaneous symptoms (e.g., hyperkeratotic tinea pedis, tinea unguium,
kerion celsi and granuloma trichophyticum), useful treatments
are systemic itraconazole and terbinafine hydrochloride. Griseofulvin is no longer commonly used in Japan.
Fig. 25.1 Trichophyton rubrum.
Filamentous hyphae (arrows) are microscopically
observed in the horny cell layer with the addition
of KOH solution.
a. Superficial dermatophytic infections
1. Tinea pedis
It is commonly called athletes foot. More than half of tinea
cases are tinea pedis. Multiple dermatophytes are seen in the
scales. The most common causative fungus is Trichophyton
rubrum, followed in frequency by Trichophyton mentagrophytes.
Tinea pedis is classified by clinical features into three clinical
subtypes.
Interdigital erosive: This is the most common of the three subtypes. The fourth toe cleft is most commonly affected. It begins
with erythema and vesicles on the interdigital region, leading to
scaling. The skin lesion is often infiltrative, softening to become
whitish, then exfoliating and becoming erosive (Fig. 25.3). Itching is intense. Secondary infection from erosion causes sharp
pain or cellulitis.
Vesicular scaling: The plantar arch and the base of the toes are
most frequently involved. Multiple vesicles occur and dry, leading to scaling. It tends to appear during the rainy season and subside in autumn.
Hyperkeratotic: It occurs most frequently on the heels. Hyperkeratosis causes roughness of the skin. Itching is rarely present,
but sharp pain results from cracking. This type is resistant to topical agents; oral antifungals are effective.
Fig. 25.2 Histopathology of tinea.
Filamentous hyphae (arrows) are observed in the
horny cell layer.
Clinical images are available in hardcopy only.
25
2. Tinea unguium
Clinical images are available in hardcopy only.
Synonym: Onychomycosis (referring to nondermatophytic
and dermatophytic infections of nail plate)
Tinea unguium frequently occurs on the first toe, often secondarily after tinea pedis. Usually, white nail (leukonychia) first
Fig. 25.3 Tinea pedis.
bottom: Tinea pedis with secondary infection.
470
25
Fungal Diseases
Fungi and molds
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
Clinical images are available in hardcopy only.
MEMO
Molds and mushrooms are fungi. Yeasts, which are used for food products and are mononucleated, are also regarded as fungi. A fungus is
composed of a long, thin hypha and a spore that is usually spherical
and proliferates by germination. Spores parasitize humans by becoming airborne and attaching to the body, where they form hyphae and
reproduce sexually or asexually.
Spores may be elongated, depending on the environment, resembling
hyphae (pseudohyphae). In culture media such as slide culture, hyphae
with a characteristic shape (conidiophores) and asexual spores called
conidia form. The conidium consists of the macroconidium and the
microconidium. Disease-causing fungi may be identified by the features of the hyphae.
appears at the tip of the toenail and gradually spreads to the nail
matrix. The nail becomes fragile and pulverizes when cut with
clippers (Fig. 25.4). The fungal elements occur mostly in the
deeper portions of the nail plate and in the hyperkeratotic nail
bed, rather than on the surface of the nail plate. It is often left
untreated for a long period because of its asymptomatic nature.
Dermatophytes spread in a patient from a tinea unguium skin
lesion to a tinea pedis skin lesion, causing autoinfection and
intrafamilial infection. It is sometimes difficult to improve with
topical agents. Oral antifungal drugs are more effective.
3. Tinea manus
Fig. 25.4 Tinea unguium.
The skin lesion may be hyperkeratotic, vesicular or scaling.
One hand, rather than both, tends to be involved (Fig. 25.5). The
majority of patients have tinea pedis as a complication. Topical
antifungal agents are the main treatment.
4. Tinea cruris
It is commonly called jock itch. The crotch and buttocks of
adult men are most frequently affected; the scrotum is rarely
involved. The same type of skin lesion as in tinea corporis
appears, often symmetrically. Itching is intense. The treatments
are topical and oral antifungal agents.
Clinical images are available in hardcopy only.
25
Fig. 25.5 Tinea manus.
The interdigital areas, fingers and fingernails are
frequently affected.
5. Tinea corporis
Commonly known as serpigo, it appears as small erythematous
papules on the trunk and extremities, gradually spreading centrifugally. The papule tends to heal centrally, giving the lesion a
ring shape (Fig. 25.6). Although the center of the lesion subsides
with mildly abnormal pigmentation, the periphery is elevated,
and papules, vesicles and scales form there. Itching is present. As
in tinea pedis, the causative dermatophyte in most cases of tinea
corporis is Trichophyton rubrum. Tinea corporis is occasionally
caused by Microsporum canis, which parasitizes dogs and cats.
Tinea corporis caused by Microsporum canis is characterized by
A. Dermatophytoses
471
Clinical images are available in
hardcopy only.
Clinical images are available in
hardcopy only.
Clinical images are available in hardcopy only.
Clinical images are available in
hardcopy only.
Fig. 25.6 Tinea corporis.
Erythematous lesions enlarge centrifugally. The center tends to heal and the rim elevates in a banked shape.
intense inflammatory symptoms. Topical and oral antifungal
agents are the main treatments.
6. Tinea faciei
It is a Trichophyton infection on the face. Unlike in eczema,
the plaques have a slightly elevated rim and tend to heal centrally
(Fig. 25.7).
Clinical images are available in hardcopy only.
7. Tinea capitis
Commonly known as scald head, this occurs most frequently
in children. Trichophyton infection in hair follicles results in
sharply edged alopecia of the scalp. There are dry pityroid scales
and short, broken off hairs in the lesion. Subjective symptoms
such as pain are not present. Head hair is sparse. Inflammation is
absent. Tinea capitis accompanied by itching and black dot formation at the follicles after the hairs break off is called black dot
ringworm; it is associated with misuse of topical steroid ointments, and its incidence has been increasing (Fig. 25.8). Oral
antifungal drugs are the first-line treatment. The affected site
should be kept clean and dry.
Fig. 25.7 Tinea faciei.
25
Clinical images are available in hardcopy only.
8. Tinea incognito
The tinea lesion heals centrally; however, if tinea is misdiagnosed as eczema and topical steroids are misused for treatment,
Fig. 25.8 Tinea capitis.
472
25
Fungal Diseases
Clinical images are available in hardcopy only.
the inflammation subsides and the characteristic central healing
in the lesion is not distinctly observed. This complicates diagnosis, and such manifestation is called tinea incognito. Tinea incognito presents clinically atypical cutaneous symptoms in such a
case (Fig. 25.9).
b. Deep dermatophytic infection
Instead of remaining in their usual location of the epidermal
horny cell layer or nail plate, fungi of the genus Trichophyton
invade the dermis or subcutaneous tissue, causing skin lesions.
1. Kerion (celsi)
Clinical images are available in hardcopy only.
Fig. 25.9 Tinea incognito causes different
clinical symptoms from typical tinea.
Clinical images are available in hardcopy only.
Kerion is most common on the scalp but can be produced in
other sites. Pityriatic scales appear in the scalp, as in tinea capitis.
Inflammation soon occurs, leading to erythema, follicular
papules, pustules, and flat or dome-shaped abscesses (Fig.
25.10). The lesions are accompanied by sharp pain, mild pulsation and discharge of pus. The hairs in the lesion fall out. There
are systemic symptoms such as swelling of the regional lymph
node and fever. Most cases are caused by misuse of steroid ointments on tinea capitis of the scalp, and the incidence has been
increasing in recent years. The most common causative agent of
kerion celsi is Microsporum canis, which infects humans through
their pets. Infants are most frequently affected. Histopathologically, Trichophyton infection is found in hairs; inflammatory cellular infiltration occurs in peripheral follicles. However,
Trichophyton does not proliferate in the dermis. The main treatment is oral antifungal agents. The incidence of Trichophyton
tonsurans has been increasing in recent years (MEMO).
Fig. 25.10 Kerion (celsi).
2. Tinea barbae
Clinical images are available in hardcopy only.
This is equivalent to kerion celsi at sites with barbae (mustache, beard). The upper lip and its periphery are most frequently
involved (Fig. 25.11). Reddening and swelling occur in the entire
area with barbae. Pus is discharged from the hair follicles. The
hairs come out easily when pulled. Most cases are caused by
shaving or misuse of steroids. The treatments are the same as for
kerion celsi.
Fig. 25.11 Sycosis trichophytica.
25
MEMO
Group infection of Trichophyton tonsurans occasionally occurs in
Japan. The main skin lesions caused by this fungus are kerion celsi,
black-dot ringworm, and tinea corporis. There are cases in which annular erythema, characteristic of tinea, is only vaguely seen. Athletes of
sports with much physical contact, such as wrestling and judo, are most
frequently affected; all team members should receive a medical checkup. Oral antifungal drugs are the first-line treatment, followed by the
same treatments as for tinea.
Trichophyton tonsurans
B. Candidiases
473
3. Trichophytic granuloma
Synonym: Majocchis granuloma
A nodule appears intradermally, subcutaneously, or in a skin
lesion caused by tinea superficialis. Flat infiltrative plaques or
tumorous plaques may form (Fig. 25.12). The granuloma may
occur locally (localized granuloma trichophyticum) or multiply
on the whole body (generalized ganuloma trichophyticum).
Localized ganuloma trichophyticum may be associated with misuse or abuse of topical steroids. Oral antifungal drugs are the
main treatment. The condition often occurs in immunocompromised individuals such as organ transplantation recipient.
Clinical images are available in hardcopy only.
Fig. 25.12 Granuloma trichophyticum.
Infiltrative skin lesion from prolonged use of topical steroids on granuloma trichophyticum. This
was misdiagnosed as eczema.
MEMO
Trichophytid is thought to be an allergic reaction to fungal components or metabolites. Like
tuberculid, this is an id lesion, which reflects
the intense inflammatory reaction that accompanies tinea infection. Patients with severe
tinea are most frequently affected. Erythema,
papules and vesicles occur on contralateral
sites of the body that are not affected by tinea.
Trichophytid often occurs during the exacerbation of kerion celsi or tinea pedis. Fungi of the
genus Trichophyton do not exist at sites of
eruptions.
Trichophytid
B. Candidiases
Table 25.3 The Candida species most frequently cultured from humans.
Outline
It
is an infection of the skin or mucous membrane caused
by yeasts of the genus Candida.
It is classified by location and clinical features into three
subtypes: cutaneous candidiasis (e.g., candida intertrigo,
erythema mycoticum infantile, candidal paronychia),
mucosal candidiasis (thrush, genital candidiasis), and
atypical candidiasis (e.g., chronic mucocutaneous candidiasis).
It may also occur as an occupational disease in workers
whose hands are in frequent contact with water, or as a
sexually transmitted disease or an opportunistic infection
resulting from immunodeficiency.
The affected site should be kept clean and dry. The antifungal imidazole is topically applied.
C. albicans
C. tropicalis
C. guilliermondii
C. krusei
C. kefyr
C. glabrata
C. parapsilosis
C. lusitaniae
C. zeylanoides
C. glabrata
Classification, Pathogenesis, Clinical features
There are seven to ten virulent species in the genus Candida
(Table 25.3). The main causative species is known to be Candi-
Go Back to the Top
To Order, Visit the Purchasing Page for Details
25
You might also like
- Diagnosis and Management of Common Tinea InfectionsDocument23 pagesDiagnosis and Management of Common Tinea InfectionsGiovanni AnggastaNo ratings yet
- UMR Introduction 2023Document110 pagesUMR Introduction 2023tu reves mon filsNo ratings yet
- Ignition System Spark Test DiagnosisDocument24 pagesIgnition System Spark Test DiagnosisMohamed l'Amine75% (4)
- Module A Specimen Questions January2020 PDFDocument5 pagesModule A Specimen Questions January2020 PDFShashi Bhusan SinghNo ratings yet
- Li Ching Wing V Xuan Yi Xiong (2004) 1 HKC 353Document11 pagesLi Ching Wing V Xuan Yi Xiong (2004) 1 HKC 353hNo ratings yet
- Topical Treatment of Common Superficial Tinea InfectionsDocument8 pagesTopical Treatment of Common Superficial Tinea InfectionsColate LocoNo ratings yet
- Superficial Fungal InfectionsDocument40 pagesSuperficial Fungal InfectionsMarimuthu PrabhakaranNo ratings yet
- DermatomycosesDocument32 pagesDermatomycosesp6hccq6jd7No ratings yet
- Cutaneous Mycoses Guide: Classification, Agents and Clinical ManifestationsDocument56 pagesCutaneous Mycoses Guide: Classification, Agents and Clinical ManifestationsHafsa ImranNo ratings yet
- Fungal Skin Infections ملزمةDocument6 pagesFungal Skin Infections ملزمةعبدالرحمن طارق عبدالله صالحNo ratings yet
- 1f97 PDFDocument8 pages1f97 PDFIqbal AbdillahNo ratings yet
- Dermatophyte Infections: Types, Causes, Symptoms and TreatmentDocument59 pagesDermatophyte Infections: Types, Causes, Symptoms and Treatmentحسين طاهر حاتم طاهرNo ratings yet
- Super Ficial Fungal Infections: Key PointsDocument4 pagesSuper Ficial Fungal Infections: Key PointsBagus Putra KurniawanNo ratings yet
- Fungal Infection of The SkinDocument74 pagesFungal Infection of The Skinary_puraNo ratings yet
- Dermatomycosis GuideDocument114 pagesDermatomycosis GuideQonita Qurrota AyunNo ratings yet
- M13 - Dermatology - Chapter 5Document11 pagesM13 - Dermatology - Chapter 5Idham BaharudinNo ratings yet
- Micoses Superificiais - CriançasDocument13 pagesMicoses Superificiais - CriançasJosé Paulo Ribeiro JúniorNo ratings yet
- TineaDocument4 pagesTineaFenni OktoberryNo ratings yet
- Cutaneous and Subcataneous MycosesmDocument15 pagesCutaneous and Subcataneous MycosesmMaxamed Faarax XaashiNo ratings yet
- Tinea Corporis Pedia-1Document11 pagesTinea Corporis Pedia-1Denso Antonius LimNo ratings yet
- Lesson 2 Superficial Cutaneous Mycosis HandoutsDocument8 pagesLesson 2 Superficial Cutaneous Mycosis HandoutsKhay Mae DonascoNo ratings yet
- Cutaneous Mycoses MikologiDocument10 pagesCutaneous Mycoses MikologisherinaNo ratings yet
- Medical MycologyDocument14 pagesMedical Mycologyhawkar omerNo ratings yet
- Fungal InfectionsDocument9 pagesFungal InfectionsCoral Srinivasa RamaluNo ratings yet
- The Diagnosis and Management Of: Tinea CapitisDocument4 pagesThe Diagnosis and Management Of: Tinea CapitisQuraisy jamal sahilNo ratings yet
- Tinea Capitis: Fungal Infection of the ScalpDocument16 pagesTinea Capitis: Fungal Infection of the ScalpIkram IkramNo ratings yet
- Tinea FasialisDocument8 pagesTinea FasialisFelix Tortora SekaiNo ratings yet
- Tinea CapitisDocument7 pagesTinea Capitismufidah nurfajNo ratings yet
- Superficial MycosisDocument17 pagesSuperficial Mycosisapi-19969058100% (1)
- Derma-Chronicles-issue 1 - 26-5-16 HiResDocument4 pagesDerma-Chronicles-issue 1 - 26-5-16 HiResParthMairNo ratings yet
- Dermatophytosis: EtiologyDocument6 pagesDermatophytosis: EtiologyTheresia FalentinaNo ratings yet
- Mikosis Superfisial: Penyebab, Gejala, Diagnosis dan PengobatanDocument46 pagesMikosis Superfisial: Penyebab, Gejala, Diagnosis dan PengobatanAdipuraAtmadjaEgokNo ratings yet
- Guide to Fungal Skin Infections (DermatomycosisDocument128 pagesGuide to Fungal Skin Infections (DermatomycosisDevy KurniawatiNo ratings yet
- DermatophyteDocument8 pagesDermatophyteBhuvana RajNo ratings yet
- Pharmaceutical Microbiology and Parasitology (PHMP211)Document59 pagesPharmaceutical Microbiology and Parasitology (PHMP211)Crisamor Rose Pareja ClarisaNo ratings yet
- BAHAN Tinea CapitisDocument28 pagesBAHAN Tinea CapitisYorika HafelaniNo ratings yet
- Superficial Fungal Infections (2019)Document6 pagesSuperficial Fungal Infections (2019)mustika rachmaNo ratings yet
- E Tra: Diagnosis and Management of Cutaneous Tinea InfectionsDocument8 pagesE Tra: Diagnosis and Management of Cutaneous Tinea InfectionsFuad hadyanNo ratings yet
- Superficial & Cutaneous Mycoses (50q)Document5 pagesSuperficial & Cutaneous Mycoses (50q)evelynseaaNo ratings yet
- Antifungal Therapy for Fungal InfectionsDocument186 pagesAntifungal Therapy for Fungal InfectionsRizweta DestinNo ratings yet
- Tinea - The DermatophytesDocument67 pagesTinea - The Dermatophytesmansoor aliNo ratings yet
- Dermatophytosis: LectureDocument35 pagesDermatophytosis: LectureGideon MukalaziNo ratings yet
- Defi Nition and NomenclatureDocument4 pagesDefi Nition and NomenclatureintanphNo ratings yet
- Fungal Skin Infections: Causes, Types and TreatmentsDocument67 pagesFungal Skin Infections: Causes, Types and TreatmentsMedo JT100% (1)
- Fungal Diseases of the Skin, Hair and Nails (DermatophytosisDocument48 pagesFungal Diseases of the Skin, Hair and Nails (DermatophytosisAsdfghjklNo ratings yet
- Fungal Infections of the Skin and NailsDocument22 pagesFungal Infections of the Skin and NailsDragon Gie30No ratings yet
- Tinea Corporis, Tinea Cruris, Tinea Nigra, and Piedra: Dermatologic Clinics August 2003Document7 pagesTinea Corporis, Tinea Cruris, Tinea Nigra, and Piedra: Dermatologic Clinics August 2003Dicky KurniawanNo ratings yet
- Superficial MycosesDocument26 pagesSuperficial Mycosesdhainey100% (3)
- Chapter 4Document103 pagesChapter 4tenaw100% (1)
- Superfical and CutaneousDocument53 pagesSuperfical and CutaneousmulatumeleseNo ratings yet
- Tinea BarbaeDocument4 pagesTinea BarbaeKevin EdroNo ratings yet
- Tinea pedis: More than just athlete's footDocument6 pagesTinea pedis: More than just athlete's footNyoman Arya Adi WangsaNo ratings yet
- Pityriasis Versicolor: Fungal InfectionsDocument4 pagesPityriasis Versicolor: Fungal InfectionsCoral Srinivasa RamaluNo ratings yet
- Myco - 05 - Dermatophyte & AsperagillusDocument92 pagesMyco - 05 - Dermatophyte & AsperagillusesraaNo ratings yet
- Antifungal DrugsDocument16 pagesAntifungal DrugsAmrinder SagguNo ratings yet
- Mycology: Clinical FindingsDocument5 pagesMycology: Clinical FindingsLuqman Al-Bashir FauziNo ratings yet
- Tinea Kruris BahanDocument11 pagesTinea Kruris BahanFebridayanti Nur FitriannisaNo ratings yet
- Tinea corporis causes and differential diagnoses under 40 charactersDocument4 pagesTinea corporis causes and differential diagnoses under 40 charactersHardiyanti HermanNo ratings yet
- Management of Tinea Corporis, Tinea Cruris, and Tinea Pedis: A Comprehensive ReviewDocument19 pagesManagement of Tinea Corporis, Tinea Cruris, and Tinea Pedis: A Comprehensive ReviewYovitaNo ratings yet
- Clinical Review - FullDocument6 pagesClinical Review - Fullilham thohirNo ratings yet
- (JURNAL) Update Terapy MycosesDocument51 pages(JURNAL) Update Terapy MycosesHabibah Nurla LumiereNo ratings yet
- The Kerion An Angry Tinea Capitis PBDocument7 pagesThe Kerion An Angry Tinea Capitis PBprajnamitaNo ratings yet
- 4 DermatophytesDocument40 pages4 DermatophytesGeoemilia1No ratings yet
- JurnalDocument32 pagesJurnalputraimanullahNo ratings yet
- Influence of Quality of Work Life and Job Attitude On Affective Commitment: A Study of Managerial PersonnelDocument15 pagesInfluence of Quality of Work Life and Job Attitude On Affective Commitment: A Study of Managerial PersonnelputraimanullahNo ratings yet
- BJHM 100 107 Tourette Plus Extra PDFDocument15 pagesBJHM 100 107 Tourette Plus Extra PDFputraimanullahNo ratings yet
- Vertigo: A Review of Common Peripheral and Central Vestibular DisordersDocument7 pagesVertigo: A Review of Common Peripheral and Central Vestibular DisordersPutra ImanullahNo ratings yet
- Influence of Quality of Work Life and Job Attitude On Affective Commitment: A Study of Managerial PersonnelDocument15 pagesInfluence of Quality of Work Life and Job Attitude On Affective Commitment: A Study of Managerial PersonnelputraimanullahNo ratings yet
- BJHM 100 107 Tourette Plus Extra PDFDocument15 pagesBJHM 100 107 Tourette Plus Extra PDFputraimanullahNo ratings yet
- A Review of Patient Satisfaction 1 Concepts of SatDocument6 pagesA Review of Patient Satisfaction 1 Concepts of SatputraimanullahNo ratings yet
- Recommendation LetterDocument1 pageRecommendation LetterputraimanullahNo ratings yet
- VM104 Tumors of The Pluera and MediastinumDocument26 pagesVM104 Tumors of The Pluera and MediastinumDian Permata PutraNo ratings yet
- E-Letter 1st Ed - Final2Document10 pagesE-Letter 1st Ed - Final2Suti CandraNo ratings yet
- WHOenlguideDocument2 pagesWHOenlguideOctoNo ratings yet
- WHOenlguideDocument2 pagesWHOenlguideOctoNo ratings yet
- Solids Level Measurement Application Guide en 78224 PDFDocument144 pagesSolids Level Measurement Application Guide en 78224 PDFwalcalNo ratings yet
- Very Easy Toeic Units 7 - 12 (Q1)Document39 pagesVery Easy Toeic Units 7 - 12 (Q1)Minh KhaiNo ratings yet
- The Girls Center: 2023 Workout CalendarDocument17 pagesThe Girls Center: 2023 Workout Calendark4270621No ratings yet
- Auramo Oy spare parts listsDocument12 pagesAuramo Oy spare parts listsYavuz ErcanliNo ratings yet
- Micdak BackgroundDocument3 pagesMicdak Backgroundappiah ernestNo ratings yet
- Cell City ProjectDocument8 pagesCell City ProjectDaisy beNo ratings yet
- DPW Series Profile Wrapping Application HeadDocument2 pagesDPW Series Profile Wrapping Application HeadNordson Adhesive Dispensing SystemsNo ratings yet
- Alok ResumeDocument3 pagesAlok Resumealok choudharyNo ratings yet
- Q1 Tle 4 (Ict)Document34 pagesQ1 Tle 4 (Ict)Jake Role GusiNo ratings yet
- Classification of Nanomaterials, The Four Main Types of Intentionally Produced NanomaterialsDocument5 pagesClassification of Nanomaterials, The Four Main Types of Intentionally Produced NanomaterialssivaenotesNo ratings yet
- 3 Types of Chemical BondsDocument12 pages3 Types of Chemical BondsSaediRisquéBriskeyNo ratings yet
- XDocument266 pagesXTrần Thanh PhongNo ratings yet
- B.Sc. (AGRICULTURE) HORTICULTURE SYLLABUSDocument31 pagesB.Sc. (AGRICULTURE) HORTICULTURE SYLLABUSgur jazzNo ratings yet
- Cellular Basis of HeredityDocument12 pagesCellular Basis of HeredityLadyvirdi CarbonellNo ratings yet
- Chapter 5Document16 pagesChapter 5Ankit GuptaNo ratings yet
- Neurons and Nerve Impulses: Nandika Arora and Risa Gaikwad (11 G2)Document17 pagesNeurons and Nerve Impulses: Nandika Arora and Risa Gaikwad (11 G2)RisaNo ratings yet
- Pack Alimentacion Clin in Perin 14Document194 pagesPack Alimentacion Clin in Perin 14Paz BustosNo ratings yet
- Hydrogeological Characterization of Karst Areas in NW VietnamDocument152 pagesHydrogeological Characterization of Karst Areas in NW VietnamCae Martins100% (1)
- Benefits and Limitations of Vojta ApproachDocument50 pagesBenefits and Limitations of Vojta ApproachAlice Teodorescu100% (3)
- Physical Education Worksheet AssessmentsDocument3 pagesPhysical Education Worksheet AssessmentsMichaela Janne VegigaNo ratings yet
- NCMA 217 - Newborn Assessment Ma'am JhalDocument5 pagesNCMA 217 - Newborn Assessment Ma'am JhalMariah Blez BognotNo ratings yet
- Carpentry Shop: Building, Doors, Windows, Trusses, WorkbenchesDocument105 pagesCarpentry Shop: Building, Doors, Windows, Trusses, WorkbenchesVinod KumarNo ratings yet
- Formularium ApotekDocument12 pagesFormularium ApotekNurul Evi kurniatiNo ratings yet
- Pulsar2 User Manual - ENDocument83 pagesPulsar2 User Manual - ENJanette SouzaNo ratings yet
- Model Fs CatalogDocument4 pagesModel Fs CatalogThomas StempienNo ratings yet
- Nitric OxideDocument20 pagesNitric OxideGanesh V GaonkarNo ratings yet