Professional Documents
Culture Documents
6
Uploaded by
Rusida LiyaniCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
6
Uploaded by
Rusida LiyaniCopyright:
Available Formats
Open Access Articlewww.njcmindia.
org
pISSN 0976 3325eISSN 2229 6816
Original article
AN EPIDEMIOLOGICAL STUDY ON HAND WASHING
PRACTICES AMONG HEALTH CARE WORKERS IN
HOSPITALS OF MANGALORE CITY
Harsha Kumar H N1, Devi Dileep2
Financial Support: ICMR_STS_
2011-01225
Conflict of interest: None declared
Copy right: The Journal retains the
copyrights of this article. However,
reproduction of this article in the
part or total in any form is permissible with due acknowledgement of
the source.
How to cite this article:
Harsha Kumar HN, Dileep D. An
epidemiological study on hand
washing practices among Health
Care Workers in Hospitals of
Mangalore City. Natl J Community
Med 2013; 4(2): 261-266.
Authors Affiliation:
1Associate Professor, Department of
Community Medicine; 2Intern,
Kasturba Medical College, Mangalore
Correspondence:
Dr. Harsha Kumar H N
Email: drhnhk@rediffmail.com
Date of Submission: 08-03-13
Date of Acceptance: 29-04-13
Date of Publication: 30-06-13
ABSTRACT
Introduction: There is very little published information on hand
washing practices of Health Care Workers (HCWs), their knowledge, perceived barriers & facilities for practicing hand washing
in hospitals from India. So this study was undertaken. Such
studies give important inputs for further research, policy &
planning.
Materials & Methods: This cross-sectional study conducted in
hospitals of mangalore city had two components: 1) Direct observation of hand washing pre & post patient contact followed by 2)
administration of anonymous questionnaire testing knowledge. A
total of 142 hand washing opportunities were studied. The study
was conducted in consenting hosptials affiliated to medical
schools, nursing homes, corporate hospitals. Two study tools
based on used were: 1) Proforma to record practices; and 2)
Questionnaire to test knowledge of HCWs.
Results: Only 129 observations could be made. Though the
HCWs had general awareness about Hand Washing Practices
(HWPs), they lacked information about specific aspects & the
practices were poor. Low hand washing rates (%) were observed
among nurses (28) & doctors (23).There was gap between knowledge and practice. Knowledge of doctors on various aspects of
hand washing was inadequate though it was better than nurses.
High Work Load & Lack of Time were perceived to be important barriers for HWPs. Shortage of sinks was noticed in
hospitals.
Conclusion: There is a need to evolve guidelines for hand washing practices & the facilities for it in hospitals of India.
Keywords: Hand washing, health care worker, hospital
INTRODUCTION
Health Care Workers (HCW) hands become
progressively colonized with commensal flora as
well as with potential pathogens during patient
care. 1 Contaminated hand could be vehicles for
the spread of certain viruses and bacteria.1 Nosocomial infections constitute a major challenge of
modern medicine. On an average, infections
complicate 7% to 10% of hospital admissions.2
Transmission of microorganisms from the hands
of Health Care Workers (HCWs) is the main
cause of nosocomial infections, and hand washing remains the most important preventive
measure.3
A review on Hand hygiene practices suggests
that the compliance of HCW to recommended
hand hygiene procedures ranges from 5% to 89%
with an average compliance rate of less than
50%.1 There is evidence that hand antisepsis
reduces the transmission of health care asso-
National Journal of Community MedicineVolume 4Issue 2Apr June 2013
Page 261
Open Access Articlewww.njcmindia.org
ciated pathogens and the incidence of Health
Care Associated Infection (HCAI).4
A study on hand washing practices (HWPs)
would help in understanding 1) Problems that
need to be addressed in this area; 2) Identify the
training needs for planning intervention; 3) Give
inputs for policy makers; and 4) Areas that need
further research. This information would help in
reducing the magnitude of HCAIs. There are two
published studies from India. One reports the
compliance rates of HWPs in ICUs of tertiary
care centers. 5 Other reports the facilities for
HWPs in OPD Complexes of PGIMER Chandigarh.6 There is no published study that examines
the HWPs, knowledge of HCWs, perceived
barriers & facilities available in nursing homes,
hospitals (including smaller ones). Hence this
study was undertaken with the following objectives: 1. To know the knowledge of HCWs with
regard to hand washing techniques and choice of
agents used for antisepsis before and after contact with patients. 2. To observe the hand washing practices among HCWs before and after
contact with patients. 3. To identify the barriers
for practicing hand hygiene.
MATERIALS & METHODS
Study Setting: Mangalore city located in coastal
Karnataka has got 8 hospitals affiliated to 5
medical schools. There are also Private Corporate
Hospitals, Nursing Homes & Polyclinics. These
health care facilities not only provide services
not only to the local population but also for
neighboring state of Kerala.
Study Design: This is a cross sectional study
with two components. Firstly direct observation
of HWPs among HCWs before and after patient
care followed by administration of an anonymous questionnaire to test their knowledge.
Study Units: Corporate Hospitals &, Nursing
Homes with in the city. The health care facilities
with following criteria were included: 1. Inpatient admissions. 2. Intensive Care Unit (ICU). 3.
Facilities for performing minor surgeries. Those
excluded were: 1. Diagnostic Centres and Laboratories. 2. Hospitals that refuse to give consent.
Study period: The study was conducted between
July 1st to September of 2011.
Sample size: The only published study about
compliance rates for HWPs from India 5 reported
the compliance rate of 74.8% among HCWs of
the hospitals. Using the formula for infinite
pISSN 0976 3325eISSN 2229 6816
population, at 5% allowable error, 90% power &
10% non-response the sample size was computed
to be 142 hand washing opportunities pre & post
contact with the patients.
Sampling: As hospitals affiliated to medical
schools are offer the maximum opportunities for
observation of hand washing practices, 4 out of
the 8 medical college hospitals were selected
using simple random sampling. To get representative sample a list of corporate hospitals /
multispecialty hospitals / Nursing homes were
obtained from the local chapter of Indian Medical Association, Mangalore. The hospitals were
approached & consenting hospitals were selected
one at a time by simple random sampling. The
data was collected. The process was repeated till
the required sample size was obtained.
Operational definitions: Based on World Health
Organization (WHO) guidelines1 the following
operational definitions were used: 1. Handwashing: Washing hands with plain or antimicrobial
soap and water. 2. Antiseptic agent: An antimicrobial substance that inactivates microorganisms or inhibits their growth on living tissues.
Eg: alcohol, chlorhexidine, iodine etc. 3. Compliance with hand washing: defined as either
washing hands and wrists with water and plain
soap or rubbing with an antiseptic solution
before and after patient care. 4. Non Compliance:
Any deviation from the above mentioned definition of compliance & departure from the room
after patient care without handwashing. 5.
Health care worker: A Nurse or doctor involved
with patient care
Study Instruments: Based on WHO guidelines1,
two instruments were devised.
1. An anonymous questionnaire to test the
knowledge of HCW. It covered the following
components of information (Scoring Range): 1)
Indications (0-11); 2) Choice of agents (0-5); 3)
Duration (0-1); and 4) Barriers of handwashing.
The questionnaire had a mix of open and close
ended questions (including single and multiple
response questions).
2. A Proforma to observe and know handwashing practices. It covered the following components: 1) Areas scrubbed; 2) Agent used; 3) Time
taken for hand washing; and 4) Methods of
drying hands. The areas scrubbed and the washing techniques were encircled on a pictorial scale
consisting of 12 steps devised by the WHO.1 This
contains pictures of correct and wrong tech-
National Journal of Community MedicineVolume 4Issue 2Apr June 2013
Page 262
Open Access Articlewww.njcmindia.org
niques. Presence / Absence of certain facilities
for HWPs in these hospitals were also included.
Pre-Testing & Modification: The English version of Questionnaire was translated to two local
langauges (Tulu & Kannada). They were, back
translated to English and checked for conceptual
equivalence. When the Proforma & questionnaires were pretested in neighbouring Udupi
City, the following circumstances compelled us
to make certain modifications: 1. As per the
WHO guidelines, HCWs should wash their
hands even before recording the pulse or blood
pressure. As this was not practiced in many of
the hospitals we omitted it from our proforma.
So, certain activities which had a higher risk of
microbial transmission like: all contacts with
mucous membrane, non intact skin, any secretions and excretions and manipulations (opening
or disconnecting) of patients vascular lines or
other tubes were observed. For example, in
surgical wards we observed wound dressing,
debridement, insertion of urinary catheter etc. 2.
Certain wrong practices like washing of hands
only once before attending to many patients in
the ward, cleaning of visibly soiled hands with
alcohol based handrubs, concomitant use of soap
and alcohol based handrubs etc were observed.
So questions about the appropriateness of these
practices were included in questionnaire (in true
/ false format) & scored on 5 point scale (Range
0-30).
Data Collection: From each hospital included,
the data was collected from a maximum of two
HCWs from ICU, each ward and minor OT. The
practices were observed before and after contact
with the patients and the proforma were filled.
This was followed by administration of questionnaire in the language of the preference
(English/Kannada) of the HCW. If both the
activities could not be performed on the same
day, a revisit was made.
pISSN 0976 3325eISSN 2229 6816
Data Analysis: Information obtained was analyzed by SPSS version 10. Results have been
expressed as proportions. The knowledge component has been expressed as total scores, mean
and standard deviation. Significance of difference in Mean knowledge scores was assessed
using students independent t test. Comparison
of proportion of doctors and nurses with inadequate/ satisfactory and good knowledge was
done. p <0.05 was considered significant.
RESULTS
Only 129 observations could be made from 4
medical school hospitals, 3 private hospitals & 1
Nursing Home giving us a response rate of
90.8%. the number of observations from each of
these are as follows (%): Medical school hospitals
91 (70.5), private hospitals 33 (25.6), Nursing
Homes 5 (3.9). the breakup of the HCWs are as
follows (n): Interns (32), Post-Graduate Students
(51), Nurses (46).
Knowledge on various aspects of hand washing
Overall knowledge of the HCWs for various
indications of Hand washing are as follows
[Correct answers (%)]: Before touching the
patient (100), after touching patient (97.7), Before
handling an invasive device for the patient (86.7),
Working in ICU (96.1), After handling blood or
other body products with gloves (83.7),While
examining patients in OPD (76.7), After using a
hand sanitizer (58.1), Attending to a patient after
being interrupted by a phone call (57.4). Most of
them (46.5) had satisfactory knowledge about the
choice of agents used & inadequate knowledge
(34.1) about duration of hand washing. Knowledge about certain common wrong practices are
presented in Table 1. Comparison of knowledge
between doctors & nurses (Table 2) on various
aspects of hand washing reveals that doctors had
better knowledge though the knowledge of
doctors on some aspects is inadequate.
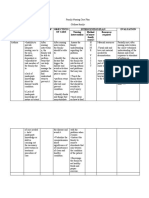
Table 1: Knowledge of HCWs regarding certain wrong practices
Knowledge about wrong practices
Hand washing should be practiced only before touching a patient
It is sufficient to wash hands only once before attending to many patients in the
ward.
Visibly soiled hands can be cleansed using an alcohol based hand rub
Soap and alcohol based hand rub can be used concomitantly
Generally it is not essential to wash hands after patient contact to prevent health
care associated infections.
Gloves should be changed or removed if moving from a contaminated body site to
either another body site within the same patient or the environment.
National Journal of Community MedicineVolume 4Issue 2Apr June 2013
Correct
Answer (%)
96 (74.4)
109 (84.5)
Wrong
Answer (%)
33 (25.6)
20 (15.5)
73 (56.6)
56 (43.4)
106 (82.2)
56 (43.4)
73 (56.6)
23 (17.8)
100 (77.5)
29 (22.5)
Page 263
Open Access Articlewww.njcmindia.org
pISSN 0976 3325eISSN 2229 6816
Table 2: Comparison of knowledge between Doctors and Nurses
Grading of Knowledge on Hand
washing (Scores)
Indications
Inadequate (< 5 )
Satisfactory (6 to 9)
Good (10 - 11)
Choice of Agents
Inadequate (< 2)
Satisfactory (3-4)
Good (5-6)
Knowledge of certain wrong practices
Inadequate (< 15)
Satisfactory (16 to 24)
Good (25-30)
Doctors (%) Nurses (%)
Mean Scores (Standard Deviation)
1 (1.2)
59 (71.1)
23 (27.7)
3 (7.0)
34 (79.1)
6 (14)
Doctors 8.69 (1.23)
Nurses 7.65 (1.46)
4.19 (0.000)
6 (7.2)
34 (41)
43 (51.8
12 (27.9)
26 (60.5)
5 (11.6)
Doctors 4.41 (1.14)
Nurses 3.19 (1.16)
5.68 (0.000)
0 (0)
63 (75.9)
20 (24.1)
4 (9.3)
33 (76.7)
6 (14)
Doctors 23.04 (2.77)
Nurses 20.47 (3.80)
4.33 (0.02)
Hand washing Practices
Use of gloves before contact with patients, disposing it and walking away without washing
hands after contact was the common practice in
these hospitals (Table 3). Less or inadequate time
was spent on hand washing (12.36%). Most of
the times (78%) the areas scrubbed were not
adequate. Rubbing palm to palm was the
common practice (68%). Missed areas included:
1. Dorsum of the hand. 2. Interdigital spaces. 3.
Tips of the fingers. Enough soap was not applied
to cover all the areas (83%). Wiping the hands to
Non-Sterile cloth was the most common (57%)
method of drying. These cloths were not single
use cloths. Uses of other methods for drying are
as follows (%): Sterile cloth (19), Tissue paper
(16), Not drying (8). Those who used alcohol
hand rubs did not apply it completely on the
entire palm (42%). Long nails could be seen on
the hands of some (14%) HCWs. Proportion of
nurses (28%) who followed hand hygiene practices was higher than doctors (23%).
Table 3: Practices Pre & Post contact with
patients
Hand washing Practices
Use of Gloves
Soap & Water
Alcohol based agents
No Hand washing
Pre-Contact
(%)
81 (62.8)
13 (10.1)
16 (12.4)
19 (14.7)
Post-Contact
(%)
--NA-23 (17.82)
18 (13.95)
88 (68.21)
Barriers & facilities for hand washing
HCWs perceive that high work load, shortage of
time & not enough sinks are some important
barriers for practising hand washing (Table 4).
Though the hospitals made available gloves,
soap, water there were inadequate number of
sinks (Table 5).
Students Independent t Test (p)
Table 4: Perceptions on the barriers of hand
washing
Perceived Barriers for
practising hand washing
Increased workload
Lack of time
Location and shortage of sinks
Lack of encouragement
Irritation and dryness of hand
Lack of role model from senior
staff
Shortage of water
Low risk of acquiring infection
from patient
Yes (%)
No (%)
92 (71.3)
86 (66.7)
81 (62.8)
78 (60.5)
71 (55.0)
70 (54.3)
37 (28.7)
43 (33.3)
48 (37.2)
51 (39.5)
58 (45.0)
59 (45.7)
58 (45.0)
43 (33.3)
71 (55.0)
86 (66.7)
DISCUSSION
The knowledge of doctors on various aspects of
hand washing is better than nurses. There are no
comparable studies from India. Poor knowledge
about hand washing practices are reported from
turkey.7 Though the level of knowledge of doctors is better than nurses, it is inadequate regarding choice of agents. Many HCWs do not
recognize the inappropriateness of certain wrong
practises (Table 1). Information about hand
hygiene is generally limited to antiseptic /
disinfecting agents in the undergraduate medical
curriculum. Though the nurses study it in detail,
knowledge acquired during student days seem
to have been forgotten. There is a need to reorient the interns, postgraduates & nursing students before they begin their work in the
hospitals.
Practices of the HCWs reflect that it is not in tune
with their knowledge. They do not practice what
they know. Use of gloves is not a substitute for
hand washing.1 so, the use of gloves without
associated hand washing amounts to noncompliance. Low proportion of HCWs practiced
hand washing with soap & water. But when we
National Journal of Community MedicineVolume 4Issue 2Apr June 2013
Page 264
Open Access Articlewww.njcmindia.org
include glove users the proportion is higher.
Higher rates of hand washing are reported by
Mehta et al.5 Their study was conducted in ICUs
of tertiary care centres where the compliance
rates are likely to be higher. Our study is the first
one to be conducted including the nursing
homes / small hospitals. We included ICUs and
also other sites in a hospital. So it reflects the
poor state of hand hygiene practices in smaller
hospitals which is more likely to be case in many
such hospitals in India.
Table 5: Facilities for hand washing available at
the site of patient care
Presence of following facilities
Number (%)
Antimicrobial Soap
1. Yes
106 (82.2)
2. No
23 (17.8)
Alcohol Based Agents
1. Yes
115 (89.1)
2. No
14 (10.9)
Sinks
1. Yes
117 (90.7)
2. No
12 (9.3)
Sterile Towel
1. Yes
72 (55.8)
2. No
57 (44.2)
Sterile Gloves
1. Yes
126 (97.7)
2. No
3 (2.3)
Hand Drier
1. Yes
4 (3.1)
2. No
125 (96.9)
Continuous water supply at sinks
1. Yes
103 (79.8)
2. No
26 (20.2)
Posters Explaining Hand washing technique
1. Yes
63 (48.8)
2. No
66 (51.2)
Sink Bed Ratio (n=95)
1. Less than 1:10
44 (46.3)
2. Atleast 1:10
44 (46.3)
3. More than 1:10
7 (7.4)
The pattern of perceived barriers for practicing
hand washing practices has not been explored in
both the studies conducted in India. The pattern
reflects that the HCWs seem to consider hand
washing as burdensome. The nature of facilities available is reasonable considering the fact
that this study included not only hospitals affiliated to medical schools but also smaller ones.
The sink bed ratio is less in these hospitals.
Problems with sinks &, water has been reported
from a premier institute like PGIMER,6 the
existence of such a problems in smaller hospitals
comes as no surprise.
pISSN 0976 3325eISSN 2229 6816
There are some limitations in our study. The
number of hospitals included in our study is
small. These kind of studies are considered
sensitive by the private hospitals so it is difficult to conduct such studies on a large scale.
The findings provide important inputs for policy
makers. Absence of standard guidelines for hand
hygiene & facilities for practicing it for our small
hospitals in our country compelled us to develop
our own tools which may have limited the extent
of facilities studied in hospitals. There do not
exist clear cut guidelines for what constitutes
adequate hand washing facility for Nursing
Homes & / Corporate Hospitals. So we could
only report the presence / absence of facilities
for hand washing.
CONCLUSION
Though the HCWs have a general awareness
about the HWPs they lack specific information.
Incorrect HWPs were observed.
Recommendations
There is a need to reorient the HCWs before they
begin the hospital work about hand hygiene
practices. There is a need to evolve national
guidelines on standard hand washing practices
and facilities in hospitals in our country.
Acknowledgements
We are grateful to those hospitals who consented
to the study on the condition of maintaining
anonymity. We are also thankful to the HCWs
who did not mind us observing their practices
and filled up the questionnaires subsequently.
Source of funding: This research was funded by
ICMR under the STS scheme for the year 2011.
The reference ID is : ICMR_STS_ 2011-01225.
REFERENCES
1.
World Health Organisation. WHO guidelines on hand
hygiene in health care. WHO Press, Geneva, Switzerland
2009.
Available
form
URL:
http://whqlibdoc.who.int/hq/2009/WHO_IER_PSP_2
009.07_eng.pdf (Cited on 30th july 2011)
2.
Haley RW, Culver DH, White JW, Morgan WM, Emori
TG, Munn VP, et al. The efficacy of infection surveillance and control programs in preventing nosocomial
infections in US hospitals. Am J Epideiol 1985;121:185205
National Journal of Community MedicineVolume 4Issue 2Apr June 2013
Page 265
Open Access Articlewww.njcmindia.org
3.
Larson EL. APIC guideline for hand washing and hand
antisepsis in health-care settings. Am J Infect Control
1995;23:251-69.
4.
Boyce JM, Pittet D. Guideline for Hand Hygiene in
Health-Care Settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee
and the HICPAC/SHEA/APIC/IDSA Hand Hygiene
Task Force. Society for Healthcare Epidemiology of
America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep 2002;51:145.
pISSN 0976 3325eISSN 2229 6816
5.
Mehta Y, Chakravarthy M, Nair R, Jawali V, Pawar M,
Rosenthal VD. Prospective study to evaluate handwashing compliance in two Indian hospitals. Am J infect control 2005;33: e73-4
6.
Mahesh Devnani, Rajiv Kumar, Rakesh KS, Anil KG. A
survey of hand-washing facilities in the outpatient department of a tertiary care teaching hospital in India. J
Infect Dev Ctries 2011;5:114-18.
7.
Asiye D. Akyol RN. Hand hygiene among nurses in
Turkey: opinions and practices. Journal of Clinical Nursing 2005;16:431-37.
National Journal of Community MedicineVolume 4Issue 2Apr June 2013
Page 266
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- NCP Rheumatoid ArthritisDocument3 pagesNCP Rheumatoid ArthritisJanieross Lamboso100% (1)
- National Core Standards 2011 1Document52 pagesNational Core Standards 2011 1yos_peace86No ratings yet
- A Research Study On Attitude of Nurses Towards Relapse Prevention Among Psychiatric Patients in Federal Neuropsychiatric HospitalDocument66 pagesA Research Study On Attitude of Nurses Towards Relapse Prevention Among Psychiatric Patients in Federal Neuropsychiatric HospitalUsman Ahmad Tijjani100% (2)
- Sandra Johnson - Updated ResumeDocument2 pagesSandra Johnson - Updated ResumeSandra Orlick JohnsonNo ratings yet
- OJPsych 2014011010170851 PDFDocument4 pagesOJPsych 2014011010170851 PDFRusida LiyaniNo ratings yet
- Proo Fonly: Healthcare Providers ' Knowledge of Standard Precautions at The Primary Healthcare Level in Saudi ArabiaDocument8 pagesProo Fonly: Healthcare Providers ' Knowledge of Standard Precautions at The Primary Healthcare Level in Saudi ArabiaRusida LiyaniNo ratings yet
- Hand Disinfectant Practice: The Impact of An Education InterventionDocument5 pagesHand Disinfectant Practice: The Impact of An Education InterventionRusida LiyaniNo ratings yet
- INFECTION CONTROL: CAN NURSES IMPROVE HAND HYGIENE PRACTICES? by Jacqueline M. Smith, RN, BN, Dyan B. Lokhorst, RN, CHPCN (C), BN (November, 2009) University of Calgary, Faculty of Nursing June, 2009Document6 pagesINFECTION CONTROL: CAN NURSES IMPROVE HAND HYGIENE PRACTICES? by Jacqueline M. Smith, RN, BN, Dyan B. Lokhorst, RN, CHPCN (C), BN (November, 2009) University of Calgary, Faculty of Nursing June, 2009Rusida LiyaniNo ratings yet
- Elaziz & Bakr 2008 PDFDocument12 pagesElaziz & Bakr 2008 PDFRusida LiyaniNo ratings yet
- Genentech 2019 Oncology Trend Report Digital VersionDocument110 pagesGenentech 2019 Oncology Trend Report Digital VersiontheoNo ratings yet
- M7 - Post Task - CaparasDocument8 pagesM7 - Post Task - CaparasGretta CaparasNo ratings yet
- Abstract BookDocument30 pagesAbstract BookAnonymous b0Jujx6kpNo ratings yet
- Medical Affairs Ophthalmology Consultant in Orange County CA Resume Ana Mercedes TribinDocument8 pagesMedical Affairs Ophthalmology Consultant in Orange County CA Resume Ana Mercedes TribinAnaMercedesTribinNo ratings yet
- Introduction To Research - CompleteDocument34 pagesIntroduction To Research - CompleteAudi Kyle SaydovenNo ratings yet
- Extending The Role of Pharmacists in Patient Care Are Pharmacists in Developing Nations Ready To ChangeDocument12 pagesExtending The Role of Pharmacists in Patient Care Are Pharmacists in Developing Nations Ready To Changebirhane gebreegziabiherNo ratings yet
- Second Level of Assessment Jamaica Delos SantosDocument6 pagesSecond Level of Assessment Jamaica Delos SantosNikey SapineNo ratings yet
- Depression and Thalassemia in Children Adolescents and AdultsDocument8 pagesDepression and Thalassemia in Children Adolescents and AdultsKennyShelva266No ratings yet
- Lesson 3 Patient Classification SystemDocument22 pagesLesson 3 Patient Classification SystemTanya WilliamsNo ratings yet
- HYPERLIPIDEMIADocument16 pagesHYPERLIPIDEMIARoessalin PermataNo ratings yet
- Adherence To TreatmentDocument147 pagesAdherence To TreatmentLo LoloNo ratings yet
- Patients' Socio-Demographic Variables and Adherence To Antihypertensive Therapy in Southern Senatorial District of Cross River State, NigeriaDocument8 pagesPatients' Socio-Demographic Variables and Adherence To Antihypertensive Therapy in Southern Senatorial District of Cross River State, Nigeriaprincess ferrerNo ratings yet
- Ais YesDocument15 pagesAis YesLauriz Dillumas MachonNo ratings yet
- PRINSIP TERAPI PADA PASIEN GERIATRI - Dr. Fita Rahmawati, SP - FRSDocument60 pagesPRINSIP TERAPI PADA PASIEN GERIATRI - Dr. Fita Rahmawati, SP - FRSLhyNa AiNun SofiaNo ratings yet
- Wearable Sensors and SystemsDocument14 pagesWearable Sensors and SystemsArulkarthickNo ratings yet
- Understanding Nursing Research Building An Evidence Based Practice 7th Edition Grove Test BankDocument13 pagesUnderstanding Nursing Research Building An Evidence Based Practice 7th Edition Grove Test BankRobertSmithgezya94% (18)
- Tell Me About Yourself PDFDocument7 pagesTell Me About Yourself PDFAndré MussiNo ratings yet
- Improving Health in Saudi Arabia: Through Population Health ManagementDocument27 pagesImproving Health in Saudi Arabia: Through Population Health Managementiyad.alsabiNo ratings yet
- Letter To Treatment ProviderDocument1 pageLetter To Treatment ProviderAshley McGuffinNo ratings yet
- Drug Information Handbook A Comprehensive ResourceDocument5 pagesDrug Information Handbook A Comprehensive ResourceInmelda AbdulrahmanNo ratings yet
- 2014 Article 240Document12 pages2014 Article 240Ilham RamadhanNo ratings yet
- Nutrients 11 00655Document20 pagesNutrients 11 00655Ibtidau NiamilahNo ratings yet
- TB PDFDocument66 pagesTB PDFKyaw Zin HtetNo ratings yet
- Kepatuhan Pasien HIV Dan AIDS Terhadap Terapi Antiretroviral DiDocument10 pagesKepatuhan Pasien HIV Dan AIDS Terhadap Terapi Antiretroviral DiNaufal Fadli AmzarNo ratings yet
- Benefits of SMART Therapy For Asthma ManagementDocument4 pagesBenefits of SMART Therapy For Asthma ManagementREDANo ratings yet
- Accenture No Time Waste Value Based Care POVDocument15 pagesAccenture No Time Waste Value Based Care POVkhgggNo ratings yet