Professional Documents
Culture Documents
Pharmacy Technician Medication Orders Guide
Uploaded by
Alan HaoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Read this document in other languages
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacy Technician Medication Orders Guide
Uploaded by
Alan HaoCopyright:
Available Formats
Pharmacy Technician Study Guide
Chapter 1 Receiving and Verifying Medication Orders
Medication Order (Retail)
Usually includes pre-printed information.
Written information MUST BE IN INK
Information requirements on Prescription
Patients full name
Date of issue
Prescriptions are valid for 1 year since date of issue
Schedule II drugs prescriptions are valid for 6 months or less
Schedule II drugs must be filled within 3 days of prescribing
Name and Title of prescriber
Acceptable Prescribers: MD, DO, OD, DDS, DVM, PA, Nurse
Practitioner.
DEA number (for controlled substances)
Name of Drug prescribed
Strength (usually in mg or ml) and dosage form
Quantity of drug being dispensed
Instructions for Dosage (SIG) (Study Symbols, Abbreviations, and
Shorthand on website)
(Optional) Instructions for labeling
Signature of prescriber in INK (NO STAMPS)
Authorization for generic substitute or Dispense as Written (DAW)
Refill information
(Rare) Preparation Instructions
SCHEDULE II Drug patient information requirements:
Address and Phone #
Age/DOB
Allergies and concurrent meds
Insurance coverage (self-pay/copay/etc..)
Verification of DEA number:
A/B/C/D/Etc assigned to MD,DO,DDS,OD
M assigned to midlevel practitioners (PA, Nurse Practitioner)
T assigned to trainee
The second letter is the first letter of the prescribers last name.
(sum of odd-numbered digits) + 2(sum of even-numbered digits) =
(last number should match the 7th number of DEA number)
Refill Requests
Drugs other than schedule II drugs can be refilled over the phone
Schedule III-IV have specific refill spacings
Schedule II drugs dont allow refills.
Prescriptions for Schedule II drugs
Triplicate forms (DEA, Prescriber, Pharmacy) (STUDY FORMS ON
WEBSITE)
Prescription may not have errors or write overs
DONTs
No refill authorizations without prescription
Pharmacy Technician Study Guide
No receiving prescriptions through electronic means (Pharmacist and
licensed intern)
DONT ASSUME
Medication Order (Institutional)
Information on Medication Order:
Schedule for administration
Instructions for preparation
Instructions for dilution
Diluent
Dosage form
Dosage Strength
Route of administration
Total Parenteral Nutrition Solution (TPN)
Compounding instructions
Medication Administration Record
Record of administration by nursing staf
Includes the dosage schedule that replaces the SIG
Includes time of administration and initials of administrator (I.E. Nurse)
Pharmacy techs note the exact time drugs are administered
Medication order
After the order from the doctor is reviewed the pharmacy tech
Fills the order and transcribes it on the MAR
Order is filled based on the Unit Dose system
The Unit Dose System
Unit dose amount of drug for a single dose
Unit dose system the entire drug doses for an individual patient that
will be required for an entire day (24 hrs)
Technician Responsibilities:
Assessing instructions for dosage preparation Injectable Medication
Controlled
(other than controlled
Preparing the drug in the properly labeled container
substances are
substances) may be
Label should include:
allowed on the Unit
sent in a pre-filled
Patient name
dose system. It
syringe, vial, or dosette
Hospital ID number
requires:
Attending physician name
-Specifically assigned
Location of Patient
codes
Delivering drug to the Medication Cart on correct floor
- Patient name, Drug,
Pick up unused medicine (Creams, ointments, liquid oral
Form, Amount
-Accountability of
medication, prn medicine)
Unused drugs are returned to the pharmacy for credit.
Exceptions of unit dosing
Medication that cannot be accurately measured (creams,
ointments, liquid oral medication)
These medications are sent to the floor in bulk.
Patient is only charged for the medication that is used.
Pharmacy Technician Study Guide
Notable differences between Retail vs. Institutional (respectably)
SIG vs. Administration Schedule
Institutional requires more identification information
Institutional information may also include
Height and weight
Lab Tests
Diagnosis
Etc.
Controlled substances in the institution does not require a triplicate form
Schedule II drugs administered in an institution may require signatures from
the head nurse and pharmacy tech upon delivery.
Chapter 2 Forms and Routes of Administration +
Interpreting Medication Orders
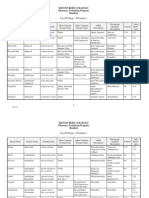
Abbreviations table (Review Abbreviations on Website)
When
Def.
Where
cc
With meals
po
ac
Before meals
od
pc
After meals
os
hs
Before sleep
ou
qd
Once a day
ad
bid
Twice a day
as
tid
Three times a day au
qid
Four times a day
IM
qod
Every other day
IV
q wk
Once a week
SC
prn
ut dict
atc
As needed
As directed
Around the clock
ID
IA
IT
qh
Every hour
With
IC
SL
Def.
By mouth
Right eye
Left eye
Both eyes
Right ear
Left ear
Both ears
Intramuscularly
Intravenously
(Bolus/Drip)
Subcutaneous
(Under skin)
Intradermal
Intra Arterial
Intrathecal (mostly
spinal)
Intracardiac
Sublingual
Without
rect
IN or NAS
TD
Drug Form
tab
Rectally
Intranasal
Transdermal
Def.
Tablet
cap
pul
Capsule
Pulvule
w or c
wo or s
How Much
cc
fl
g or gm
Def.
Cubic centimeter
(ml)
Fluid
Gram
Pharmacy Technician Study Guide
gr
Grain
syr
Syrup
gtt
Drop
susp
Suspension
mg
Milligram
elix
Elixir
mcg
Microgram (g)
ext
Extract
aa
Of each
tinct
Tincture
tsp
Teaspoon
ung or oint
Ointment
tbsp.
Tablespoon
Dosage Forms
Solid dosage forms
Tablet
Pressed powder
Depends on how hard the tablet is pressed
Less pressure = faster dissolving
Enteric tablet Has a coating to protect from stomach acids. Better
dissolved in basic pH (duodenum)
Capsule
Gelatin container filled with the drug (powder, granule, liquid, oil)
Intended to be dissolved in an acidic medium (stomach)
Others
Lozenge Designed for oral absorption. Held in mouth. Flavored based.
Drug Powders Fine powder mixed with sugar. Held in blisters. Blister
is inserted into an diskinhaler that aerosolizes the drug for inhalation
Liquid dosage forms
Syrup Sweetened liquid that contains the drug
Elixir Similar to syrup but contains a high concentration of alcohol
Extract Oil or active portion of a plant or herb that is extracted with alcohol
Solutions and suspensions
Solution - A drug completely dissolved in a liquid (syrup, elixir)
Suspension water and drug particles that do not dissolve, but remain
suspended in water.
Particles tend to sink to the bottom
Drawing of the dose must be done immediately after mixing
Doses must be drawn up quickly
Tincture Alcohol-based drug form used topically. Usually dispensed in a
dropper bottle. NOT TO BE TAKEN INTERNALLY
Semisolid dosage forms
Creams Emulsions (oil droplets suspended in water).
The drug is dissolved in the oil.
Contains less water than lotions.
Dispensed in tube/jar
Ointments Emulsions
Can vary from a thick emulsion to a drug suspended in a waxy base
(petroleum jelly)
Topically on skin/mucous membranes
Dispensed in tube/jar
Suppositories
Pharmacy Technician Study Guide
Made of soft wax and oils
Will melt at body temperature
Drug is meant to be released slowly
Inserted into body cavities
Normally large
Adhere to the cavity wall
Often used for local administration (Hemorrhoids, yeast infection, etc.)
Rectal suppositories are used to medicate those unable to ingest
medication orally
Rectal suppositories are absorbed through rectal wall into bloodstream
Should be stored in cool room with minimal handling.
Storing emulsions
Freezing/Excessive heat may separate oil and water
Should never be frozen
Administering the drug Route of Administration
Oral (PO) Most common route
Buccal Drug is absorbed through lining of the cheek. Usually in Lozenge or
buccal tablet form.
Sublingual (SL)
Allows for quick absorption of drug through the vessels under the
tongue.
Soft. Easily dissolved.
Also could be in a form of Sublingual spray.
Intranasal (IN or NAS) Administered through nose
Spray or drop form used
Transdermal (TD) Drug absorbed through surface blood vessels
Slow absorption
Patch form
Inhalants Taken directly into the lungs through inhalation
Powder or liquid form
Often requires an aerosolizing device
Administration through body cavity Drug is inserted into Rectum or Vagina
Absorption though blood vessels at site
Usually used for local administration
Medicating the Eye and Ear
Eye (ophthalmics). Ear (otics).
Administered by drops (gtt)
Droppers and containers are calibrated to give drops of particular size.
Ophthalmic ointments may sometimes be used
Ophthalmic ointments are applied to the inside of the eyelids
using the tip of the ointment tube.
Parenteral Drug Administration
Parenteral Drug In medical terms, Any drug administered by Injection
Intravenous (IV) injections Drug administered through the veins
Fast absorption
Bolus (Needle) one time single-dose injection.
Pharmacy Technician Study Guide
Rapid efect
Risks: Adverse efects of too rapid delivery.
Drug/contamination cannot be withdrawn
IV Drip A bag or bottle of liquid that allows a drug to be infused over
a long period of time.
Piggyback IV (IVPB) A solution contained in a smaller IV bat that is
infused along with the primary IV drip.
The IVPB NEVER mixes with the regular IV.
Intramuscular (IM) injections Drug injections are placed into skeletal muscle.
Slower absorption
19 25 gauge needles for adults (22-25g for children) (25-27g for
infants)
Difuses through muscle tissue then reaches bloodstream
Requires large bore needle
Aqueous solutions absorb faster
Depot preparations (in forms of ester or salt) absorb slower. Provides a
sustained dose.
Rate of absorption depends greatly on site of injection and local blood
flow
Subcutaneous (SC or Sub-cu) Injections Drug injections placed under the
skin at the fat layer.
Slow absorption
Small bore needle (25-30 gauge)
Vaccines, Insulin
Intradermal (ID) injections Drug injection placed within layers of dermis
Slow absorption
Small bore needle (25-30 gauge)
Intraarterial (IA) Injections Drug injection placed directly into an artery
Arteries are very muscular and have a high pressure flow of blood
Requires a larger bore needle.
Intrathecal (IT) Injections Drug injections place into the space between the
spinal cord and spinal meninges.
Fast action
Large bore needles
Intracardiac (IC) Injections Drug injection placed directly into the heart.
Fast action
Large bore needles
Interpreting the Prescription Order
Drug name (Proprietary or generic)
Check May Substitute line for signature or for permission in
instructions
The strength and dosage form of drug
Amount of drug to be prescribed
Instructions for the patient (SIG)
Study abbreviations
Pharmacy Technician Study Guide
Pay attention to the spacing of dosages (dosage interval) (I.E. Qid, Tid,
etc)
Dosage interval is based on the Half-life of the drug.
Half-life The amount of time taken for half of the serum
concentration of dug t be eliminated from the body.
The Half-life is generally considered to the main index of the
length of a drugs efects.
Dosage intervals are important because drugs need to be
constantly replaced as it is cleared.
Signature of prescriber and authorization to substitute
Institution (Hospital)
In INK
-there are just more
Dispense as Written or May Substitute
orders to fill at a time.
If DAW is absent substitution is permissible.
-There is a schedule
instead of a SIG
- No concurrent
medication on profile
other than medication
given at hospital.
Information Gathered by Technician to Create Patient Profile (Retail Patient
Profile):
Required for the Distribution of Schedule II drugs
Address and Phone Number
Age or DOB
Drug Allergies
Concurrent medication
Including herbal remedies
Note any physical conditions (kidney, liver problems, clotting issues,
etc.)
IMPORTANT TO DISPENSING THE CORRECT MEDICATION
Match drug labels to order.
LA
Long Acting
Extra letters and drug
SA
Sustained
label abbreviations.
Acting
Dosage conversion is
SR
Sustained
possible
Release
If dosage form is incorrect
TR
Timed Release
drug cannot be dispensed.
ER or XL
Extended
Consult Pharmacist.
Release
Chapter 3 Inpatient and
Outpatient Profiles
The Patient Profile
Identifies patients
Legal record of medication dispense
Resource of information that protects the patient against potentially harmful
drugs or procedures.
OUTPATIE
NT
PROFILE
Outpatient Profile Information collected by pharmacy tech before dispensing
drugs.
Identifying information
Pharmacy Technician Study Guide
Name, Address, Phone #, DOB.
Drug allergies and adverse reactions
Allergies to one drug could mean the same for similar drugs
Concurrent Medications
Drug-Drug interactions (Therapeutic or Toxic)
Synergism amplify one another
Antagonism reduce the efectiveness of one another
Drugs may change blood concentration of other drugs.
Drug Duplication or Therapeutic duplication
Must include herbal remedies also
Medical History
Inherited medical conditions (I.E. high blood pressure)
Certain drugs or procedures can be harmful if combined with
these conditions even if they havent developed
History of Drug Abuse
Increased Supervision
Regulated administration of drug.
Special Considerations
Physical, Mental, Cultural Handicaps need to be addressed.
Religious issues may also be taken into consideration
Insurance Information
Co-pay or self-pay
Coverage of prescribed drugs
Coverage of certain drugs under certain circumstances
Diference between generic and proprietary distribution
sometimes.
Current prescription and refill information
Shows the status of the patients various prescriptions.
Amount dispensed and amount remaining on prescription must
match.
NEEDS TO BE UPDATED REGULARLY AFTER EVERY REFILL
Outpatient Summary Table:
Name
Phone #
Drug Allergies
Concurrent Medications*
History of Drug Abuse
Insurance information
Address
Age/DOB
Adverse Reactions
Medical History
Special considerations (Physical, Mental,
Cultural)
Current prescription and Refill
information*
*not included in inpatient patient profiles.
INPATIENT
PROFILE
Inpatient Profile - Same information with added details:
Pharmacy Technician Study Guide
Height
Weight
Diagnosis
Treatment
Therapy
Diet plans
Blood tests
Lab Results
Statement of
goals
Billing
Information
Patients Billing
#
Inpatient profiles do NOT include information that is not applicable to
the institutional policy.
I.E. Refill policy and concurrent medication other than those
prescribed within the institution.
Duties of the Pharmacy Technician
New patients Obtain information and create profile
Repeat patients Update profile
Special note on Privacy of patient information:
HIPPA Information in patient profile may not be released except
for non-identifiable information. Patients are allowed to request
a copy of his or her patient profile. Pharmacies are allowed to
charge a fee for this service.
Pharmacy Technician Study Guide
Chapter 4 Handling Medications
Obtaining the Correct Medication from Inventory
Interpretation of the Manufacturers Label
ALL information on the label must match
EXCEPT for dosage strength (concentration)
Dosage strength may be converted with dimensional analysis.
Information on the Drug Label:
The NDC Number: contains codes that denote
Generic name
Manufacturer
Proprietary label
Dosage form
Strength
Type of packaging
The amount of drug in each tablet/unit of volume
For a drug in solution/suspension the concentration is
given in mg or mg/ml
The proprietary (trade) name and generic name
Dosage form
Drug Manufacturer
The Federal Legend or
Lot or control number
Expiration date
Other: Recommended dosage, safe dosage, preparation
instructions, and optimum storage conditions.
National Drug Code (NDC) Number (Ex. NDC 0049-5460-74)
Ten-digit number
Three segments
Segment 1 Identifies Manufacturer or repackager
Segment 2 Identifies specific drug
PREPARING
Segment 3 Identifies the Packaging
LIQUID AND
Preparing and Dispensing Basic Solid and Liquid Drugs
SOLID
Conversion of solid dosage forms
MEDICATION
Must be accurately converted or else it cannot be
dispensed.
Tablets may only be accurately divided with an tablet
splitter if they are scored tablets
ALL IS PERFORMED
Measuring
of Liquid Medications
IN A SANITARY
Solutions
and suspensions must be measured at room
SETTING
temperature using accurate devices
MARKINGS ON
If concentration is not listed on bottle then. (total mg of
DISPENSING
drug)/(total ml) to acquire strength (concentration)
BOTTLES OR
needed to fill order.
DOSAGE CUPS ARE
An order of almost any amount can be filled as long as
NOT ACCURATE.
the amount dispensed is appropriate. (I.E. 10ml is too
much for a IM injection)
Choosing the Proper Container for Dispensing
Pharmacy Technician Study Guide
Topical solution Bottle w/ Dropper cap
Cream or Ointment Tube or Jar
Liquid oral dosing Small neck suitable for slow pouring
Solid dosage large-mouthed dispensing container
Amber colored containers for light sensitive drugs
Humidity sensitive drugs must be packed in containers
with tight-seal caps
Drugs that react with plastic must be pack in glass
containers.
CHOOSE APPROPRIATE SIZES
Sealing the Dispensing Container
Sealed with child-proof caps.
Easy-open caps may be placed if patient signs a waiver
indicating the cap was requested
Properly Labeling the Container
Information on the container:
Name, Address, and Phone # of pharmacy
Name of patient
Name of Prescriber
Date of Dispensing
Name of drug
If the generic drug was dispensed then there
should be a generic name on the label. Same
goes for proprietary drugs.
Strength of Medication (40mg tabs, 30mg/ml, etc.)
Quantity of drug dispensed (number of tablets, ml,
etc.)
Directions for dosage
Refill information
Initials of drug dispenser
Auxiliary Labels Helpful reminders to patient to
maximize efects. Also outlines dangers of combining drug
with certain foods or alcohol.
Compounding of Prescriptions
Preparing a solution, ointment, or powder from a WRITTEN PROCEDURE
is often performed by the technician.
Legally, these dosage forms must be prepared by the technician
according to a standardized, written procedure written out by the
pharmacist.
EXTEMPORANEO Extemporaneous Compounding preparation of a dosage form for
US
drug delivery that is customized for a particular patient.
COMPOUNDING
This requires a degree of judgment therefore is performed by the
ALL IS PERFORMED
pharmacist.
IN A SANITARY
If the pharmacist generates a written protocol for the
SETTING
preparation of the dosage form, it may be prepared by the
technician.
Pharmacy Technician Study Guide
Once the protocol for preparation of the drug is in written form it
is no longer considered extemporaneous compounding.
Pharmacy Technician Study Guide
ASEPTIC
TECHNIQUE:
PREPARING
STERILE
Aseptic Technique: Preparing Sterile Solutions for Injection
SHOULD THE NEEDLE
COME IN CONTACT
WITH CLOTHES, SKIN,
OR ANY SURFACE.
THE ENTIRE SYRINGE
MUST BE DISCARDED
Precautions:
Sepsis Blood Poisioning
Aseptic technique Technique of preparing a drug without
contaminating it with bacteria or other organisms.
Perform all procedures inside a sterile laminar flow hood with
clean, disinfected hand, hair tied back and covered.
Laminar Flow Hood Creates a barrier between the workspace
and the environment.
Avoid talking, sneezing, and coughing in the hood.
Disinfect withdrawal site on the drug vial (Septum) with alcohol
before withdrawal of the drug.
Both syringe and needle must be kept sterile.
Open syringe packing from end that will attach to the needle.
DO NOT TOUCH SYRINGE OR NEEDLE
Protective cap should be left on needle unless its withdrawing or
injecting drug.
Laminar flow hood and gloves are not guaranteed sanitary.
Withdrawing the Drug:
Needle should be placed on septum beveled side up
Needle should pierce the septum at a 45 angle
Prevents rubber fragments from entering the needle
Coring when rubber fragments from septum enter
needle
When medication is being withdrawn the needle should be at a
90
Avoid touching the plunger and depositing organisms on the
plunger as it leaves the barrel of the syringe
After withdrawal of medication:
1. Place Protective cap on needle
2. Open hood.
Label should go on the plunger end of the barrel.
Re-sanitize septum with alcohol.
Drug Withdrawal Process Recap:
1. Place needle on septum
*Bevel side up
2. Pierce Septum at 45
angle
*Tilt everything up to 90. Draw
3. Draw out Medication
slowly.
*Tap on barrel
4.Remove air bubbles
*Push air bubbles out of syringe
into vial
5.Withdraw needle from vial *Do not touch the plunger
6. Place Protective cap on
*Immediately
Needle
7. Open Hood
Pharmacy Technician Study Guide
8. Label syringe
9. Re-sanitize septum w/
Alcohol
*Label goes on plunger end of
barrel
Pharmacy Technician Study Guide
Working with Hazardous Drugs
Protective clothing
Completely covers body
Lab coat (protect clothing and skin)
Safety glasses/goggles
Safety glasses must have splash guard
Additional Safeguards (Disposable body coverings)
Prevent contamination of technician and pharmacy
Coverings can be removed and discarded at the door of
the IV room
Accidental Drug Exposure
Dont touch yourself while preparing drugs
hazardous/non-hazardous.
When working with a sterile drug, particularly one that is
hazardous, keep hands at least six inches inside the hood
away from other parts of the body
Intravenous Admixtures and injections
Intravenous Injections
Goes directly into the blood
May be of small or large volume
May be a large IV drip of solution, an admixture, or a small bolus shot.
Intramuscular Injections
Injected into muscles to be absorbed
Smaller volumes (less space in muscles)
Slow release
Lessens physiological shock
May increase length of drugs efects
Large bolus needle (25 gauge)
Subcutaneous Injections
Designed for slow release
Small Volume due to limited amount of space under skin
Small bolus needle
Labels on a syringe should be as narrow as possible. Wrapped at the top of
the syringe so as to not cover the markings on the syringe.
Intravenous Admixture
A drug that is added to a large-volume parenteral.
The drug is released slowly into the blood.
Lessens the shock
Administered two ways:
Mixed directly with the bulk solution (Primary IV)
Admixture must be labeled appropriately.
Separate very small bag (Secondary Piggyback IV) that is
released slowly into the tubing with the IV drip.
Label for IV bag or admixture should be placed toward the top of
the container to not hinder the view of the mixture. Helps catch
contaminants.
Pharmacy Technician Study Guide
Chapter 5 Proper Storage and Delivery of Drug Products
Proper Storage of Drug Products
Refrigerated areas Kept at 4-18C. Measured by a calibrated thermometer
(That should be kept in place)
Room Temperature Kept at 15-30C (59-86F)
Dosage Forms and Drug Stability
Drugs last longer when kept in the right conditions
A drug packed dry lasts longer
A drugs stability greatly increases when in tablet form
Tablets and other solid dosage drugs:
Tablets last longer due to the fact less drug is exposed
Opaque glass/plastic prevents degradation caused by the suns rays.
Keep out of direct sunlight
ALWAYS
CONSULT
Tight seal container lid to protect from Humidity and Oxygen
MANUFACTURE
Refrigeration Cold temperatures slow down chemical reactions
RS LABEL
Cool, dry places prevent breakdown and development of
microorganisms
Dehydration Increases shelf life of drugs
Some injected drugs are delivered in powdered form to increase
shelf life
The powder is reconstituted right before use.
Temperatures for Proper Drug Storage
Storage
Storage
Storage
Designation
Temperature (C)
Temperature (F)
Cold
Not to exceed 8C
Not to exceed 46F
Between 8C and
Between 46C and
Cool
15C
59F
Between 15C and
Between 59C and
Room Temperature
30C
86F
Between 30C and
Between 86C and
Warm
40C
104F
Excessive heat
Above 40C
Above 104F
() will appear as warning to not expose drug to temperatures
Location
(Usually Too Cold)
Refrigerator
Pharmacy Shelf
(Drugs May lose
Potency)
(Too Hot for Drugs)
Importance of Cleanliness and Sanitation During Storage
Dust may contain molds, fungi, or bacteria that might contaminate a drug.
Clean devices before and after to prevent Cross-contamination of Drugs.
Tools: Detergent, Alcohol wipes, Washing liquid measuring equipment with
soap and water.
Use of Pharmacy Inventory as Floor Stock
The Pharmacy may send drugs to individual patient floors to use as a floor
stock
The Nurses station or emergency room staf would be responsible for
keeping a supply of the drugs and drug products on hand that is normally
needed on a routine basis.
Pharmacy Technician Study Guide
The floor staf will be responsible of keeping inventory and ordering drugs
from the pharmacy.
Pharmacy Staf Responsibilities:
Proper storage conditions: Temperature, Sanitation, following
instructions, proper capping.
Proper dispensing conditions: Clean tools, sanitary dispensing area,
unused medicine is closed, Inspecting dispensing equipment. No stray
needles, food, drink, contaminated material (Ex. Used needles)
Proper Record Keeping: Inventory of floor stock, records of drugs
dispensed, record of drugs ordered must all match. This is important
for controlled substances. Any discrepancies must be reported
immediately to the pharmacist and supervising official.
Pharmacy Technician Record and Delivery Responsibilities:
When drugs are delivered to patient care areas:
Technician must receive a signature of the person accepting the
drugs
Provide a complete inventory of drugs delivered
Additional Paperwork for controlled substances:
Exact amount of drug to be transferred
Information about that drug:
Generic name
Manufacturer
Proprietary name
Lot Number
Dosage
Expiration Date
Dosage Form
The signature of the head nurse or supervising medical
professional is REQUIRED (no other person may sign).
No signature is needed if controlled substance is delivered to a
locked secured area (computerized medication cart)
The receipt of the drug(s) by the patient care area is
acknowledged by this signature and responsibility and
appropriate records are transferred at this time.
Chapter 6 Receiving Payment for Goods and Services
Receipt of Payment for Pharmacy Services
Two ways of payment:
Self-Pay: Patient pays the pharmacy directly
Third-Party Payer:
Patient can pay out-of-pocket and the pharmacist must fill out
an insurance affidavit with drugs received, price, and other
information required by the insurance company.
Patient can pay a small Co-payment and the pharmacy will
bill the insurance company for the balance of the charge.
Third-Party Payers:
Traditional Insurance companies
Government plans (Medicare and Medicaid)
Private insurance companies
They all have their limits and types of coverage
Pharmacy Technician Study Guide
Insurance coverage must be verified at the time the prescription is
received.
Look up specific coverage information in the Pharmacys database.
After establishment of coverage or method of payment:
Forms that need to be filled out must be identified and
completed
Price of medication must be calculated
Institutional pharmacy billing Role of MAR
Medication Administration Record (MAR):
Charges are billed to patients account as soon medication is
dispensed
Unused medication is returned to the pharmacy and the MAR
account is credited. *insurance verification is done at a separate
accounting department
Beginning of Math Section
Calculation of the Price of the Medication
(Cost price) + ?%(Cost price) = Selling price
Chapter
7 aFractions,
Dispensing
fee may be
percentage ofDecimal,
price or a and Algebra Review
Notes:
flat rate.
Must include 0 place holder in case of decimals. (0.25 .25 )
Chapter 8 Systems of Measurement
ASA
325mg =
ASA 5
Common Conversion Factors
Unit of Measure Abbreviation
grains
gr i
scruples
sc i
1 lb household
fl. oz
i
drams
i
1 minim
i
teaspoon
tablespoon
1 pint
1 quart
1 gallon
1
1
1
1
1
tsp
tbsp
pt
qt
gal
Conversion
60 mg 65 mg
gr xx
454 g
30 ml
4 ml
approximately 1
gtt
5 ml
15 ml
16 fl. oz.
2 pints
4 quarts
1,200 mg
16 oz
8 drams
3 scruples
1 L
Milliequivalents and Equivalents
Milliequivalent (mEq) - refers to the number of positively charged ions
per liter of salt solution.
Normally found on solutions of salts
1 Equivalent (Eq) = 1,000 Milliequivalents
In a ratio even percentage the left number is always grams and the right
number is always milliliters (?g/?ml)
Temperature conversions:
C = (F-32)(5/9)
F = C(5/9)+32
Pharmacy Technician Study Guide
Chapter 9 Percentages and Ratios
Percentage in Pharmacy:
When given a percentage always assume n/100
?g/100ml : Weight per volume
?g/100g : Weight per weight
?ml/100ml : Volume per Volume
Study Alligations (VERY EASY)
Chapter 10 Measuring Equipment
Liquid Measurements
Tools: Syringe, Graduated Cylinder (ONLY tools allowed for dispensing)
The measuring device selected should be the closest possible size to the
volume being measured.
Solutions should be measured all at once not in pieces.
Solutions should be measured at room temperature.
Graduated Cylinder:
When reading a graduated cylinder: Read the meniscus
Calibrate a graduated cylinder by filling it with an amount of water
1 ml of water should weigh 1 g at 25C
Syringes:
When measuring with a syringe you read the black line nearest the plunger
tip not the cone that extends into the solution.
Insulin syringes are only for dispensing insulin
Calibrated in international units
These units are specific to the concentration of normal (U-100) insulin
only.
30 gauge needle.
The needle is very fine and easily bent.
100 units of normal insulin (U-100) is equal to 1 ml volume.
Solid Measurements
Weighing small amounts require a prescription balance
Weighs 5mg or 6mg accurately
Largest amount it can weigh is 100 120g
Weighing large quantities:
Torsion (solution) balance.
This only has one weighing pan that hangs at the end of the
scale
Not sensitive
Double-Pan Balance
Balances 2 pans opposite of each other
One side carries the materials to be weighed
The other side carries carefully calibrated counterweights.
Factors that afect the accuracy of weight measurements
Position of the material being weighed and counterweights
Materials and counterweights MUST be placed at the CENTER of the
weighing pan(s).
DONT TOUCH COUNTERWEIGHTS WITH OILY HANDS.
Pharmacy Technician Study Guide
Temperature of material may cause the air around the material to
warm and lift the material.
Chapter 11 Conversion of Solid Dosage Forms
Solid
Dosage Conversion
Conversion can only happen if the dosage form is correct
Tablets must be scored in order to be split.
Steps:
1. Make sure the units match. If not convert the order to match the stock.
2. Divide the order by the available stock to obtain amount dispensed
3. Make sure answer is appropriate.
Chapter 12 Conversion of Liquid Dosage Forms
Use Order/Stock
Simplify as much as possible before starting
Chapter 13 Pediatric Dosages (Child: Ages 2-12)
Computation of Doses on the Basis of Body Weight
Drug dosage for adults are often expressed on the manufacturers label
The dosages are expressed as mg/kg
Childs Dose: Adult dose/1.7
Make sure to convert pounds to kilograms
Computation of Dose by Body Surface Area (BSA)
Measurement of BSA
Use Nomogram Relates height and weight of a person to his or her
body surface area.
Height: Left scale. Weight: Right scale
Directions: Find height and weight on left and right side and draw a line
connecting them. The line will go through a scale.
THE NOMOGRAM WILL NOT BE ON THE EXAM
Pharmacy Technician Study Guide
Computing the Dose for an Individual Patient
Recommended dose is given in: drug/m 2
Dose for an individual is measured by:
m2[surface area] x mg/m2 [found on label]= (drug amount given)
mg/ml
Compare to safe-dose range on manufacturer label
Calculating a Childs dose (Ages 2-12)
Divide dose by a conversion factor of 1.7
Conversion to childs dosage is done AFTER calculating Adult dosage
Youngs Rule and Clarks Rule
Youngs Rule:
Clarks Rule:
Age of child ( years )
( Adult Dose )=Chil d ' s Dose
Age of child +12
Weight of Child
( Adult Dose )=Chil d ' s Dose
150
Note: Both will not always produce identical answers.
Safe Dosages
Safe Dose Range Presents a minimum dose at which the drug is efective
and a maximum dose (at which toxicity may be seen)
Appears on the Manufacturers Label
If calculations do not fall in the Safe Dose Range it should be brought
to the attention of the Pharmacist.
Single Dose Safe range vs. Daily Dose Safe Range
Single Dose A Single dose enters body, performs its function, leaves
the body
Cumulative/Daily Dose Taken multiple times and is utilized to replace
drug as it is eliminated from the body.
Has potential for toxic build up
The establishment of a maximum allowable daily dose prevents
build up of toxic levels.
Chapter 14 Parenteral Dosages
Parenteral Dosage forms
Enteral Medication goes into digestive tract and is then absorbed into the
blood
Parenteral Medication bypasses digestive tract. Directly into blood.
(Reference to Parenteral Dosage Forms)
Calculation of doses is the same as the calculation for oral doses
Preparation of Parenteral Dosages
The doses are prepared in sterile conditions.
Pharmacy Technician Study Guide
Choosing a Proper Syringe:
Size should be as close as possible to the volume of drug being drawn
up.
Choose size based on precision in measurements and markings.
Choosing the Appropriate needle
Large-bore Needle (16-18 G):
Will draw up and dispense liquid quickly
Used for Drug Rehydration, dilution, and admixtures
Needed to penetrate dense muscle Tissue
IM injections
Fine Needle (25-30 G):
Subcutaneous (SC) injections
Intradermal injections
Intermediate-Bore Needle (22 G):
Penetrate the smooth muscle layer of the vessel without causing
extravasation (leakage) from the vein.
IV injections
Proper Dilution of Drugs for Injection
Manufacturers label contains instructions for dilution and preparation
Determine concentration needed
Refer to Dilution table
Usually given: ml of diluent for U/ml of drug
Must know how to back-calculate to correct an error in dilution.
Diluents: Water, Saline, D5W, etc.
Chapter 15 Intravenous Calculations
Preparing Intravenous Medication for Administration
Flow Rate it is determined by a controller or an infusion set
Infusion Set a calibrated piece of equipment that is set to deliver a drop of a
certain size
Drop factor Number of drops per Milliliter (gtt/ml)
Infusion sets come in 10 gtt/ml ,15 gtt/ml (standard), and 60 gtt/ml
The rate of drops is adjusted by the nurse.
Intravenous (IV) Solutions
Common salt solutions:
Normal Saline (NS) 0.9% Sodium Chloride
Normal Saline 0.45% Sodium Chloride
Normal Saline 0.225% Sodium Chloride
Sugar solutions and commonly used Admixtures
D5W 5% dextrose (glucose) in water
Ringers solution (or lactated Ringers)
Saline solutions with Potassium Chloride are labeled in Red
Potassium overdose is fatal
Saline Solutions
Used to maintain osmotic homeostasis
Hypertonic, Isotonic, Hypotonic
and Normal Saline solutions are used for special conditions and
for admixtures
Calculation of Flow Rate
Pharmacy Technician Study Guide
Volume of fluid
Time of infusion
Sometimes the flow rate is calculated minutes rather than hours
Calculation of Flow Rate in Drops per Time
Using an Infusion apparatus
Drop-Factor is printed on the package
Volume of Fluid
of Drops
x Drop Factor=
( Time
)
of I nfusion
Time
Drops per time
ml
=(
Drop Factor
time )
Drops per time:
Drop factor:
gtt
time
gtt
ml
Chapter 16 Intravenous Admixtures
Infusing Medications Over Time
Rehydration and Reconstitution of Drugs
Injectable drugs are supplied in powder form
Must be rehydrated (reconstituted) before use
Drugs are supplied in a solution Isotonic to the body.
Concentration of drug and salt particles present in the solution is
the same as that in the body fluids.
The particles will not overhydrate or dehydrate the body cells.
Rehydration Just adding water to a drug that is already mixed with
Volume
the salts that make the solution
Dose of Drugordered
Amount
of drugwater,
the Drugs
vial
Reconstitution
Addingadd
a diluent
(saline,
distilled
or D 5have
W) a shorter
the IV =
Amount of Diluent Addedshelf life after
*Calculations will use Ratios
reconstitution.
Chapter 17 Calculation
of Dose per Time
often
Refrigeration may
increase shelf life.
Equation: Concentration(Flow rate) = Dose/time
Concentration
The amount of druggmg
=The concentration of drugthe solution
The volume of fluid IV bag
Flow Rate
The time that it takes the bag
The amount of fluid IV bag
empty =Flow Rate
Chapter 18 Compounding (all procedures listed must have
written protocol)
Compounding Drugs by Procedure
Compounding is changing the dosage form of a drug
Bulk Compounding
Extemporaneous Compounding if it doesnt have a written procedure
MUST HAVE WRITTEN PROCEDURE for tech to compound drugs.
Pharmacy Technician Study Guide
Reducing and Enlarging Formulas
Just multiply/divide all ingredients by the same factor.
Making Preparations by percentage
Convert percentage to (g/100ml)
Set up ratio for needed volume
Chapter 19 Commercial Calculations
Cost Price: Wholesale price
Markup: % of the cost price
Selling Price: Cost + Markup
Profit: Markup amount - Expenses
Dispensing fee:
Added to Price
May be a flat fee or percentage of selling price
ONLY added to drugs dispensed at the pharmacy
NOT added to medication sold over the counter.
End of Math Section
Chapter 20: Math Test
Pharmacy Technician Study Guide
Pharmacology section
Chapter 21 Introduction to Pharmacology
Introduction/Objectives
Drug information
Proprietary and Generic names
Classification
Mechanism of Action
General Uses
Side Efects
Interactions
Physiological actions of the drug
Possible Adverse efects
Possible Drug Interactions
Food and Lifestyle Contradictions
Form and Common Dosage amount
Proprietary Drug Nomenclature
Drugs may be named according to a particular quality or property of the drug
(i.e. function, classification, etc.)
Less frequently names may reflect some other property.
Fast onset, long duration, dosing interval, dosage form, etc.
Many drugs simply take part of the generic name as the trade name.
These concepts help establish patterns among drugs and associate drugs.
Allow for educated guesses.
Form vs. Use Recognizing Various Forms of a Generic Drug
Many drugs are treated with an acid or base and thus salts of the original
drug.
A salt allows the drug to be more easily utilized by the body.
Various chemical forms of a particular drug have diferent clinical uses.
Specification of the type of salt does not always exist. (Drugs are usually
referred to simply by name)
Drug salts are specified on a medication order if it is needed for efective
administration by a certain route or the patient has a particular condition.
Addition of letters to a drug name may denote a certain type of formulation.
Understanding the Pharmacology of Chemotherapeutic Agents
Drugs are presented in classes and in the order in which they would be
chosen for therapy.
Mechanism of action Various biological and biochemical changes within the
body.
Drugs within the same class usually have similar mechanisms of action,
adverse efects and contraindications. (only diferences in lipid solubility,
duration, etc. may be seen)
Choice of Drug Therapy:
First line drugs [Drug of Choice (DOC)] Very efective; acceptable
adverse efect profile
Second line drugs
These drugs are
either not as efective
or have a lot of
undesirable efects.
Pharmacy Technician Study Guide
Third line drugs
Fourth line drugs
The therapeutic efects are often nothing more than the physiological efects
of the drugs and what the drug does in the body
Pharmacokinetics and Pharmacodynamics What Happens to the Drug
after it is Administered
Pharmacokinetics a study of the movement of and changes in the drug
within the body.
Absorption: How the drug gets into the plasma
Usually refers to how the drug gets into the bloodstream from
outside of the body.
By definition drugs administered through intravenous injection
are not absorbed, as they are injected directly into the
bloodstream.
Absorption:
pH of compartment:
Likes does not dissolve likes.
Acidic drugs will be dissolved in a basic setting
(Duodenum)
Basic drugs will be dissolved in an acidic setting
(Stomach)
Lipid soluble drugs will be absorbed by fat and tend
to not remain in the plasma (composed of water).
The more vessels in a region the quicker the
absorption.
Distribution: Where the drug goes in the body
Where the drug goes and where the drug is stored in the body.
Storage:
Sites: Fat, Tissue Protein, Plasma Protein
Binding of drugs to protein stabilizes the drug
Binding of drugs to protein prevents the breakdown of the
drug by the liver or kidneys.
Drug Equilibrium:
Protein-Bound drugs and drugs existing in plasma exist in
equilibrium.
Drugs in the plasma (Free Drug) contribute to the
therapeutic efect and are free to be cleared by the kidney
or liver.
As free drugs are being cleared they are constantly being
replaced by bound drugs.
The equilibrium between Bound:Free Drugs are not
necessarily a 1:1 ratio.
Volume of distribution (Vd) The volume o space that the drug
occupies in the body.
It gives an idea of how much drug must be taken before a
state of equilibrium is reached.
Pharmacy Technician Study Guide
Large volume = The drug is distributed into many body
compartments (plasma, tissue, CNS). Smaller Plasma
concentration of drug.
Small Volume = Drug distribution is concentrated into one
place. Larger Plasma concentration of drug.
Loading dose Typically a larger first dose to fill up a large
volume and reach therapeutic levels.
Metabolism: How the drug is chemically changed in the body. This
change can result in the activation or elimination of the drug
Majority of drugs are metabolized in the liver. It can happen in
any organ though.
The Liver contains a large number of metabolic enzymes
Cytochrome Mixed Function Oxidase System (Cytochrome P250)
The most important group of metabolic enzymes. Is involved in
the metabolism of most drugs
Some drugs will alter the activity or levels of this enzyme
Alteration of this enzyme may change the rate of
metabolism of other drugs.
All enzymes, in general, may be altered by age or gender.
Elimination: How the body gets rid of the drug.
Elimination Removal of drug from the body
Kidney rids water soluble drugs
Liver processes and rids lipid soluble drugs through feces.
Clearance Removal of drug from the plasma
Accomplished by the kidney, liver, or lung
Care must be paid to the route of elimination of the drug and the
state of health of the patient. (Attention to kidney and liver
health)
Drug Half-Life(T1/2)
Half-life amount of time that is take one half of a drug dose to
be cleared from the body. (Clearance Rate)
Factors that influence Clearance Rate:
The rate of elimination of the drug.
How quickly the drug might be inactivated in the body
(e.g. by enzymes, etc.)
Alteration of drug half-life (basically changing clearance rates)
A way to alter the half-life is to alter the clearance of the
drug.
If the body is altered (consuming alcohol or acidic fluids,
etc) the drug half-life (rate of elimination) may be altered.
Illnesses may also alter a drugs half-life (rate of
elimination). (Usually a decrease of protein for a drug to
bind to therefore more free drug in the plasma).
Condition of clearance routes (liver and/or kidney)
Liver and kidney filters and clears the drug out of
the plasma
Pharmacy Technician Study Guide
Drug ionization when the drug is in a diferent pH setting
and is used
Drugs that are not ionized are reabsorbed into the body.
Ionized drugs will be cleared either through the kidney or
liver.
The Adverse Effect Profile
Adverse Efect An unwanted efect produced by a drug.
Toxic Efect - Any efect that produces end organ (target organ(s)) toxicity.
The more serious and frequent the adverse efect, the more negative the
adverse efect profile.
Anticipating an Adverse Drug Efect
Better to understand the mechanism that will lead to knowing the
adverse efects.
Knowing the mechanism of action allows you to predict the therapeutic
and adverse efects.
Drug-Drug Interactions
Other drugs can interfere with a drugs mechanism, storage, distribution, or
elimination/
Absorption, distribution (protein binding), and Clearance.
Drug-Drug Interactions at the Level of Absorption
Drugs may compete for absorption (Transport sites). (When it the drugs
have the same path of absorption)
The higher the concentration of the drug the more likely it is to gain
access and have priority
Binding interactions Some drugs decrease the absorption of
other drugs by binding to them in the stomach/intestine and
preventing their absorption into the body.
Changing the pH A drug may influence the pH of a particular
compartment and may increase/decrease the absorption of a
second drug. This may also influence the rate of clearance as
well.
Changes of local blood flow A change in blood flow may
influence the rate of absorption of a second drug.
Drug Distribution Protein Binding Interactions
Many drug interactions occur because two or more drugs bind to the
same plasma protein
The one that binds tightest and fastest wins.
The loser floats in the plasma, causing a surplus amount of free
loser drug.
The more loser drug in the plasma, the greater the therapeutic
efect, the greater adverse efects, the greater chance for toxicity. Also,
faster metabolism of free unbound loser drug.
Doses that compete for binding sites must have adjusted dosages to fit
accordingly
Drug-Drug Interactions Competition for Drug Clearance
Lungs may breakdown and/or expel a drug
Drugs that are metabolized by enzyme in the liver can go into the bile
and out through the intestine.
Pharmacy Technician Study Guide
If the enzymes make the drug water soluble they may go out with the
urine.
Some drugs are not metabolized and go out with the urine.
Lipid soluble drugs and not metabolized go out with the bile.
Drug-Drug Interactions Competition for Drug Clearance
Efects of Age, Organ Damage, and Drug Use
Age: as a person gets older the functions of the clearance organs
(kidney and liver) decrease and the dosage of the drug must be altered
to compensate.
Organ Damage: If the patient has a damaged organ (I.E. Liver) due to
disease or drug use this could potentially decrease the rate of
clearance.
The decreasing of the rate of clearance could potentially cause the
buildup of that drug in the blood system to toxic levels.
Drug Toxicity and Interactions
All drugs are, to some extent, poisons.
Dosages are established to minimize harmful efects and maximize
beneficial efects.
Sometimes by taking two drugs concurrently one drug may set up
another to produce toxic efects.
Drug Agonism and Antagonism
Agonist A drug that mimics the actions of an endogenous substance.
Stimulates a cellular or biochemical pathway
Indirect Agonism - Inhibits the breakdown of the endogenous
substance
Endogenous substance Substances that originate within the human
body.
Antagonist A drug that attaches to a receptor and stimulates it once
(or not at all) and then stays attached to the receptor, blocking any
other transmitters.
Partial Agonist Normalizes activity. They are used when there are
erratic levels of strong agonist.
When there is not enough of the agonist when its needed then
the partial agonist will act as an agonist
When there is too much of the strong agonist when its not
needed then it acts as a antagonist, blocking the receptor.
Additive, Synergistic, and Antagonistic Efects
Therapeutic Efects Physiological efects of medicine
Additive and Synergistic Drug Toxicity Additive efects may produce
drug toxicity
Efects of Alcohol with CNS Depressants
Alcohol taken with sedating drugs, antiseizure medications,
antipsychotics, and antidepressants, or barbiturates may
depress the central and autonomic nervous system to the extent
that they arent able to function.
Synergistic Therapeutic Efects Too Much of a Good Thing
Some drugs may synergize and produce too much of a beneficial
efect.
Pharmacy Technician Study Guide
Example: If Warfarin (anticoagulant) is taken with Aspirin
(anticoagulant) the synergistic efect may prevent blood clotting
to an extent that internal bleeding may occur.
Antagonism of Therapeutic Efects
Some drugs may block the efects of other drugs by physically
blocking the binding or actions of another drug
Indirect antagonism The creation of an environment in which
its unfavorable for the drug to work (I.E. Changing pH)
Drug-Food Interactions
Study and know what foods interact with what drugs.
Blood Laboratory Values
Test for renal function:
Blood Urea Nitrogen (BUN): High levels of BUN is bad
Creatinine levels Indicator of kidney function. Creatinine
is a product of muscle breakdown. High = Good. Low =
Bad.
Liver function:
Liver function is measured by means of the activity and
levels of serum enzymes. Generally the lower the level of
liver enzymes the better:
o Serum Glutamic Oxaloacetic Transaminase (SGOT)
Elevated levels may be seen in certain
conditions (I.E. Rheumatoid Arthritis,
Pancreatitis, Muscular Dystrophy, Asthma)
o Serum Glutamic Pyruvate Aminotransferase (SGPT)
o Lactate Dehydrogenase (LHD)
o Alanine Aminotransferase (ALT)
o Aspartate Aminotransferase (AST)
Elevated levels of ALT/AST may indicate liver
damage due to alcohol or Hepatitis
Blood Glucose Levels:
o Normally measured during the fasting state (no
food - 12 hours) or the prost prandial state (the
patient has recently eaten)
o High level Uncontrolled diabetic
o Low level Hypoglycemia.
* A diagnosis of either condition is not made on the
basis of one serum glucose determination, but
requires a long and involved test called the glucose
tolerance test.
o Glucose Tolerance Test A patient drinks a solution
of glucose and is tested in intervals.
Serum Blood gasses:
A determination of respiratory function
Analyzing the Partial pressures of O2 (Po2) and CO2 (Pco2)
A low oxygen level or high level of carbon dioxide may indicate
depressed respiratory function
Electrolyte levels:
Pharmacy Technician Study Guide
To check levels of : Sodium, Potassium, and calcium
Potassium level: Important because it is needed to protect the
heart function before a surgical procedure.
Blood Test
Normal Values
BUN
5 20 mg/dl
BUN/Creatinine Ratio
10:1 to 20:1
Creatinine
0.6 1.2 mg/dl
Creatinine Clearance
75-125 ml/min
Serum glucose
70 110 mg/dl (fastin)
Po2
75 105 mmhg
Pco2
35 45 mmhg
Electrolytes:
Sodium
145 147 mEq/l
Potassium
3.5 5 mEq/l
Calcium
8.8 10.4 m/dl
Chloride
95 105 mEq/dl
Enzyme
SGOT
AST
SGPT
ALT
GGT
Normal Levels of Common Liver Enzymes
Normal Range (Males)
Normal Range (Females)
5 40 IU/I
5 33 IU/I
5 40 IU/I
5 33 IU/I
7 46 IU/I
4 35 IU/I
7 46 IU/I
4 35 IU/I
4 23 IU/I
3 13 IU/I
You might also like
- PTCE: Pharmacy Technician Certification Exam Premium: 4 Practice Tests + Comprehensive Review + Online PracticeFrom EverandPTCE: Pharmacy Technician Certification Exam Premium: 4 Practice Tests + Comprehensive Review + Online PracticeNo ratings yet
- Pharmacy Technician Certified Board Preparation: Comprehensive Review Manual: Comprehensive Review ManualFrom EverandPharmacy Technician Certified Board Preparation: Comprehensive Review Manual: Comprehensive Review ManualRating: 5 out of 5 stars5/5 (1)
- Pharmacy Technician Certified Board Prep: Crossword Puzzles and Word SearchFrom EverandPharmacy Technician Certified Board Prep: Crossword Puzzles and Word SearchNo ratings yet
- The Essential Guide to Prescription Drugs, Update on RemdesivirFrom EverandThe Essential Guide to Prescription Drugs, Update on RemdesivirNo ratings yet
- PTCE - Pharmacy Technician Certification Exam Flashcard Book + OnlineFrom EverandPTCE - Pharmacy Technician Certification Exam Flashcard Book + OnlineRating: 3 out of 5 stars3/5 (9)
- Pharmacy Technician Certified Board Comprehensive Pharmacy MathFrom EverandPharmacy Technician Certified Board Comprehensive Pharmacy MathNo ratings yet
- PHARMACY TECHNICIAN CERTIFICATION EXAM (PTCE): Passbooks Study GuideFrom EverandPHARMACY TECHNICIAN CERTIFICATION EXAM (PTCE): Passbooks Study GuideNo ratings yet
- Pharmacy Technician Certification Exam Practice Question Workbook: 1,000 Comprehensive Practice Questions (2023 Edition)From EverandPharmacy Technician Certification Exam Practice Question Workbook: 1,000 Comprehensive Practice Questions (2023 Edition)Rating: 4 out of 5 stars4/5 (5)
- Revision Guide Made Simple For Pharmacy Technicians 3rd Edition: 3rd EditionFrom EverandRevision Guide Made Simple For Pharmacy Technicians 3rd Edition: 3rd EditionNo ratings yet
- Revision Guide Made Simple For Pharmacy Technicians 2nd EditionFrom EverandRevision Guide Made Simple For Pharmacy Technicians 2nd EditionNo ratings yet
- Pharmacy Calculation Workbook: 250 Questions to Prepare for the NAPLEX and PTCB ExamFrom EverandPharmacy Calculation Workbook: 250 Questions to Prepare for the NAPLEX and PTCB ExamRating: 5 out of 5 stars5/5 (1)
- Pharmacy Practice: Essentials of Hospital, Clinical and Community PharmacyFrom EverandPharmacy Practice: Essentials of Hospital, Clinical and Community PharmacyRating: 5 out of 5 stars5/5 (3)
- Pharmacy Assistant: Passbooks Study GuideFrom EverandPharmacy Assistant: Passbooks Study GuideRating: 4 out of 5 stars4/5 (1)
- Reference Guide For Pharmacy Technician Exam: Manan ShroffDocument50 pagesReference Guide For Pharmacy Technician Exam: Manan ShroffAira Gene Meneses100% (2)
- Pharmacology for Student and Pupil Nurses and Student Pharmacy TechniciansFrom EverandPharmacology for Student and Pupil Nurses and Student Pharmacy TechniciansNo ratings yet
- Pharmacy Technician Certification 8172019 ExamDocument115 pagesPharmacy Technician Certification 8172019 Examfatdaddys100% (2)
- A Unique and Simplified Approach to Pharmacy Calculations for Healthcare ProfessionalsFrom EverandA Unique and Simplified Approach to Pharmacy Calculations for Healthcare ProfessionalsNo ratings yet
- PDFDocument732 pagesPDFMahmud Eljaarani89% (9)
- Certification Study Guide Press QualityDocument142 pagesCertification Study Guide Press QualityAnonymous AjXpL58b100% (5)
- Top 300 Drugs Practice Question Workbook: 1,000 Comprehensive Practice Questions (2023 Edition)From EverandTop 300 Drugs Practice Question Workbook: 1,000 Comprehensive Practice Questions (2023 Edition)Rating: 5 out of 5 stars5/5 (2)
- Revision Guide Made Simple For Pharmacy Technicians - PTCB: 4th EditionFrom EverandRevision Guide Made Simple For Pharmacy Technicians - PTCB: 4th EditionNo ratings yet
- Pharmacy Education in the Twenty First Century and Beyond: Global Achievements and ChallengesFrom EverandPharmacy Education in the Twenty First Century and Beyond: Global Achievements and ChallengesNo ratings yet
- Basic Pharmacology And Drug Calculations [Practice Questions And Answers]From EverandBasic Pharmacology And Drug Calculations [Practice Questions And Answers]Rating: 4 out of 5 stars4/5 (1)
- Pharmacy Technician Certification Exam ReviewDocument286 pagesPharmacy Technician Certification Exam ReviewKaren Yuu75% (8)
- A Prescription for Retail Pharmacy: A Guide to Retail Pharmacy for Patients, Doctors, Nurses, Pharmacists, and Pharmacy TechniciansFrom EverandA Prescription for Retail Pharmacy: A Guide to Retail Pharmacy for Patients, Doctors, Nurses, Pharmacists, and Pharmacy TechniciansNo ratings yet
- PTCB Exam 1Document20 pagesPTCB Exam 1Amber Chen80% (5)
- MULTISTATE PHARMACY JURISPRUDENCE EXAMINATION (MPJE): Passbooks Study GuideFrom EverandMULTISTATE PHARMACY JURISPRUDENCE EXAMINATION (MPJE): Passbooks Study GuideNo ratings yet
- Pharmaceutical Dispensing and CompoundingFrom EverandPharmaceutical Dispensing and CompoundingRating: 4 out of 5 stars4/5 (2)
- NAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)From EverandNAPLEX Practice Question Workbook: 1,000+ Comprehensive Practice Questions (2023 Edition)Rating: 4.5 out of 5 stars4.5/5 (3)
- Pharmacy Terminology PDFDocument35 pagesPharmacy Terminology PDFpuputshaputra100% (1)
- Barbara Lacher Pharmacy Technician Certification Review and PracticeDocument248 pagesBarbara Lacher Pharmacy Technician Certification Review and Practicemasuod100% (2)
- Pharmacy Technician: The Ins and Outs of Becoming ADocument52 pagesPharmacy Technician: The Ins and Outs of Becoming AEsra ArgüdenNo ratings yet
- Pharmacist 101: 101 Tips to Start, Grow, and Succeed as a Pharmacist From A to ZFrom EverandPharmacist 101: 101 Tips to Start, Grow, and Succeed as a Pharmacist From A to ZNo ratings yet
- Pharm Tech Practicum WorkbookDocument72 pagesPharm Tech Practicum WorkbookSmeeta PrasaiNo ratings yet
- PHARMACY QUIZ REVIEWDocument10 pagesPHARMACY QUIZ REVIEWThanya Maya100% (1)
- Top 200 Drugs WorksheetsDocument30 pagesTop 200 Drugs WorksheetsErika Harvery100% (1)
- Medical Assistant Exam Prep: Your All-in-One Guide to the CMA & RMA ExamsFrom EverandMedical Assistant Exam Prep: Your All-in-One Guide to the CMA & RMA ExamsNo ratings yet
- HESI A2 Admission Assessment Study Guide: COMPLETE Health Information Systems A2® Study Guide and Practice Test Questions prepared by a dedicated team of test experts!From EverandHESI A2 Admission Assessment Study Guide: COMPLETE Health Information Systems A2® Study Guide and Practice Test Questions prepared by a dedicated team of test experts!No ratings yet
- Fun with Pharmacology: Pharmacology Made SimpleFrom EverandFun with Pharmacology: Pharmacology Made SimpleRating: 3 out of 5 stars3/5 (1)
- Pharmacy Technician Training Manual: Distributed by Opha 4 Edition, Jan 2006Document39 pagesPharmacy Technician Training Manual: Distributed by Opha 4 Edition, Jan 2006Martial List100% (1)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Pharmacy Technician Program Student HandbookDocument31 pagesPharmacy Technician Program Student HandbookTun Lin OoNo ratings yet
- PTCB Pratice Test and ExampleDocument16 pagesPTCB Pratice Test and Examplettwenty009100% (1)
- PTCE Review NotesDocument11 pagesPTCE Review NotesSantos WheelerNo ratings yet
- Pharmacy MathDocument7 pagesPharmacy Mathrn220562No ratings yet
- Advanced Inv MGMT SPG FINALDocument15 pagesAdvanced Inv MGMT SPG FINALseanfaria100% (1)
- Pharmacy Certification Exam Review QuestionsDocument37 pagesPharmacy Certification Exam Review QuestionsAsahota50% (2)
- Pharmacy PracticeDocument43 pagesPharmacy Practiceadilshafie100% (1)
- Exam For The Certification of Pharmacy Technicians (ExCPT) Study GuideDocument20 pagesExam For The Certification of Pharmacy Technicians (ExCPT) Study GuideMcRee Learning Center33% (3)
- Drug Distribution MethodsDocument40 pagesDrug Distribution MethodsMuhammad Masoom Akhtar100% (1)
- Entire Pharm ClassDocument173 pagesEntire Pharm ClassnancyNo ratings yet
- Medical Management of Constipation: Meredith Portalatin, M.D. Nathaniel Winstead, M.DDocument8 pagesMedical Management of Constipation: Meredith Portalatin, M.D. Nathaniel Winstead, M.DShinta UnairNo ratings yet
- A Healthy Spirit Lives in A Healthy BodyDocument3 pagesA Healthy Spirit Lives in A Healthy BodyqueencelNo ratings yet
- Formulation and Evaluation of Phenytoin Sodium Sustained Release Matrix Tablet Jbb.1000125Document6 pagesFormulation and Evaluation of Phenytoin Sodium Sustained Release Matrix Tablet Jbb.1000125NurlelaSundariZNo ratings yet
- Notice: Bischoff, James S., M.D.Document3 pagesNotice: Bischoff, James S., M.D.Justia.comNo ratings yet
- Medication ErrorsDocument5 pagesMedication ErrorsWendy EscalanteNo ratings yet
- Chapter 11 - Transdermal Drug Delivery SystemDocument4 pagesChapter 11 - Transdermal Drug Delivery SystemYoreeNo ratings yet
- Aurobindo Pharma Receives USFDA Approval For Vancomycin Hydrochloride For Injection (Company Update)Document2 pagesAurobindo Pharma Receives USFDA Approval For Vancomycin Hydrochloride For Injection (Company Update)Shyam SunderNo ratings yet
- SertralineDocument3 pagesSertralineFrenzy TaherNo ratings yet
- Medication Administration Basic Principles GuideDocument25 pagesMedication Administration Basic Principles GuideChin ChanNo ratings yet
- Pharmacology Renal DiureticsDocument24 pagesPharmacology Renal Diureticskpsuan100% (1)
- Daftar Obat Aman Dan Bahaya Ibu HamilDocument8 pagesDaftar Obat Aman Dan Bahaya Ibu HamilAnnida Nurul Haq80% (5)
- Harga Barang Medis TerbaruDocument201 pagesHarga Barang Medis TerbaruDidiek SetiaNo ratings yet
- Cosmeceuticals: Marketing vs ScienceDocument62 pagesCosmeceuticals: Marketing vs ScienceJorge TupiaNo ratings yet
- MicroencapsulationDocument10 pagesMicroencapsulationprinceamitNo ratings yet
- Indian PharmacopoeiaDocument24 pagesIndian Pharmacopoeiakamalsami150% (8)
- Er-Drug StudyDocument41 pagesEr-Drug Studyrc_lacampuinganyahooNo ratings yet
- Therapeutic: Physiologic Mechanism: Generic Name: Side EffectsDocument2 pagesTherapeutic: Physiologic Mechanism: Generic Name: Side Effectskristel_nicole18yahoNo ratings yet
- DRUG-EDUCATION-FOR-THE-YOUTH-NSTP-LECTURE (1) .OdpDocument70 pagesDRUG-EDUCATION-FOR-THE-YOUTH-NSTP-LECTURE (1) .OdpJulia Shane BarriosNo ratings yet
- OxygenationDocument7 pagesOxygenationPatziedawn Gonzalvo100% (1)
- Product Ida Foundation NigeriaDocument36 pagesProduct Ida Foundation NigeriaBhakti A MagdalenaNo ratings yet
- Guidelines For The Advertisement of Drugs, Herbal Medicines, Cosmetics, Medical Devices & Household ChemicalsDocument8 pagesGuidelines For The Advertisement of Drugs, Herbal Medicines, Cosmetics, Medical Devices & Household ChemicalssboaduappiahNo ratings yet
- ShanePDesaele&DavidPZgareick-Pharmacy Management - Essentials For All Practice Settings-McGrawHil Publishing Company, 2005 (2008)Document652 pagesShanePDesaele&DavidPZgareick-Pharmacy Management - Essentials For All Practice Settings-McGrawHil Publishing Company, 2005 (2008)Mustakim Masnur Al Biruni50% (2)
- Drug Presentation: Manisha M.Sc. Nursing 1 Year Con IlbsDocument57 pagesDrug Presentation: Manisha M.Sc. Nursing 1 Year Con IlbsManisha ShakyaNo ratings yet
- Spinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and AtropineDocument4 pagesSpinal Anesthesia in Children With Rectal Premedication With Midazolam, Ketamine and AtropineKunal YadavNo ratings yet
- نسخة 264889196 Tramadol Drug StudyDocument1 pageنسخة 264889196 Tramadol Drug StudyMeteab AlzhiryNo ratings yet
- Pharmacology BRS - Flash CardsDocument101 pagesPharmacology BRS - Flash Cardsmilap88100% (1)
- PESTLEDocument45 pagesPESTLEABHILASH KUMAR DANDIMENo ratings yet
- Respiratory System Pharmacology NotesDocument15 pagesRespiratory System Pharmacology NotesAli Rahimi100% (1)






















![Basic Pharmacology And Drug Calculations [Practice Questions And Answers]](https://imgv2-1-f.scribdassets.com/img/word_document/475660044/149x198/2c7fc45015/1691161640?v=1)