Professional Documents
Culture Documents
Beta-Lactam Antibiotics-Newer Formulations and Newer Agents
Uploaded by
Yampold Estheben ChusiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Beta-Lactam Antibiotics-Newer Formulations and Newer Agents
Uploaded by
Yampold Estheben ChusiCopyright:
Available Formats
Infect Dis Clin N Am 18 (2004) 603619
Beta-lactam antibiotics: newer
formulations and newer agents
Stanley I. Martin, MDa, Kenneth M. Kaye, MDb,*
a
Division of Infectious Diseases, Massachusetts General Hospital,
55 Fruit Street, Boston, MA 02114, USA
b
Division of Infectious Diseases, Harvard Medical School, Channing Laboratory,
Brigham and Womens Hospital, 181 Longwood Avenue, Boston, MA 02115, USA
Since 1928, when Alexander Fleming rst noted the inhibition of
staphylococcus from a mold belonging to the genus Penicillium, b-lactam
antibiotics have led the ght against infectious diseases. These drugs all
share a common structure and mechanism of action, but have evolved into
various classes with diering spectrums of antimicrobial activity and unique
qualities. They include the penicillins, the penicillinase-resistant penicillins,
the extended-spectrum penicillin derivatives, the cephalosporins, the carbapenems, and the monobactams. The landscape lled by this diverse group of
antibiotics is always shifting, with the use and value of certain drugs
changing depending on the pharmacoeconomic scenarios of the time and
susceptibility patterns of microbes. Newer antibiotics continue to be
introduced, whereas others fall out of use. This article focuses on the
newest of the b-lactams to be approved for use in the United States and
includes ertapenem, the third carbapenem now available; cefditoren, one of
the newest oral third-generation cephalosporins; a newly approved highdose formulation of amoxicillin-clavulanate; and the only fourth-generation
cephalosporin available for use, cefepime.
Ertapenem
The production of plasmid-encoded extended-spectrum b-lactamase
enzymes by increasing numbers of gram-negative bacteria is becoming
a more signicant source of microbial resistance in health care settings and
* Corresponding author.
E-mail address: kkaye@rics.bwh.harvard.edu (K.M. Kaye).
0891-5520/04/$ - see front matter 2004 Elsevier Inc. All rights reserved.
doi:10.1016/j.idc.2004.04.006
604
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
is providing an impetus for developing novel antibiotics. In November 2001,
the Food and Drug Administration (FDA) approved a new long-acting,
parenteral carbapenem called ertapenem (formerly MK-0826). Ertapenem,
like the other carbapenems, imipenem and meropenem, demonstrates much
resistance to hydrolysis by bacterial plasmid and chromosomally mediated
extended-spectrum b-lactamase enzymes [1]. Despite this and many other
similarities, ertapenem does have some features that may preclude it from
the same category of use as other carbapenems but also place it in a more
unique position in the antibiotic armamentarium for other uses (Table 1).
Like meropenem, ertapenem contains a b-methyl group on the rst
carbon, protecting it from hydrolysis and making it unnecessary to coadminister with cilastatin. It is the largest of the three carbapenems and
exhibits a high degree of plasma protein binding at roughly 92% to 95%, as
compared with imipenem at 20% and meropenem at only 2%. This and its
inherent resistance to human renal dehydropeptidase give it a long plasma
half-life of 3.8 to 4.4 hours, allowing for only once-a-day dosing [2].
The usual dose of ertapenem is 1 g every 24 hours. It can be administered
either by intravenous [2] or intramuscular routes when mixed with 1%
lidocaine [3]. The drug is approximately 80% eliminated by the kidneys
through both glomerular ltration and renal tubular secretion [2]. Half is
excreted as the native drug, whereas the other half as an open-ring
derivative. Only 10% of the drug is excreted in the feces, and because
ertapenem does not undergo hepatic metabolism or inhibit cytochrome P450 drug clearance, dose reduction is not necessary in hepatic insuciency
and drug-drug interactions are less likely [4]. Decreasing the dose to 0.5 g
once a day is advised, however, for patients with severe renal insuciency
and a creatinine clearance less than 30 mL/min.
Like other carbapenems, ertapenem binds to the penicillin-binding
proteins (PBPs) of bacteria, inhibiting cell wall synthesis and making it
rapidly bactericidal [1]. The spectrum of ertapenem is similar to the other
carbapenems, extending to cover a broad array of gram-positive and gramnegative aerobic and anaerobic pathogens [5,6]. Like other carbapenems,
slow-growing mycobacteria, Enterococcus faecium, methicillin-resistant
Staphylococcus aureus, and some nonfermenting gram-negative organisms,
such as Stenotrophomonas maltophilia, show complete resistance. An
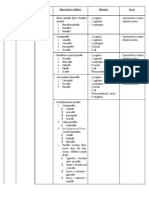
Table 1
Features of the dierent carbapenems
Antimicrobial coverage
Dosage/
Intervals
Coadminstered Half- Gram- Gramagents
life positive negative Anaerobes Nonfermenters
Imipenem 1 g q 68 h Cilastatin
Meropenem 1 g q 8 h
None
Ertapenem 1 g q 24 h None
1h
1h
4h
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
605
important distinction, however, is ertapenems lack of activity toward other
nonfermenters, particularly Pseudomonas and Acinetobacter species. Evaluation of its in vitro activity against 3478 miscellaneous bacterial isolates
from Europe and Australia revealed higher susceptibilities of some gramnegative pathogens, such as Enterobacteriaceae, Moraxella, Haemophilus,
and Neisseria species, compared with imipenem based on mean inhibitory
concentration (MIC)50 and MIC90 values. Meropenem seemed equal to
ertapenem in activity against these organisms. Against anaerobic isolates,
ertapenem was equal to imipenem, but seemed to have slightly less activity
for gram-positive organisms, such as streptococci and staphylococci. This
dierence, however, may be negligible because the MIC values were below
the likely resistance breakpoints for both drugs [5]. Cross-resistance between
ertapenem, imipenem, and meropenem can be assumed regarding most
organisms, although there are some in vitro surveillance data that suggests
this may not be entirely complete. Enterobacteriaceae resistant to imipenem
are uncommon, although they may not be entirely predictive of resistance to
ertapenem [7].
Among 130 Pseudomonas isolates, 33% were resistant to ertapenem as
compared with 17% resistant to imipenem. For Acinetobacter strains, 109
isolates showed an MIC50 of only 0.5 mg/L for imipenem and a much higher
4 mg/L for ertapenem. Thirty percent of the Acinetobacter strains were
resistant to ertapenem as compared with 18%, which were resistant to
imipenem [5]. This inherent lack of activity against Pseudomonas and
Acinetobacter spp is a distinct dierence between other carbapenems and
ertapenem.
The current FDA recommendations for the use of ertapenem include
treatment of complicated intra-abdominal infections, skin and soft tissue
infections, community-acquired pneumonia, complicated urinary tract
infections, and acute pelvic infections. The safety and ecacy of ertapenem
was evaluated for each of these indications in seven double-blind,
randomized trials comparing ertapenem with either ceftriaxone for pneumonia [8,9] or urinary tract infections [10,11] or piperacillin-tazobactam for
the intra-abdominal [12], skin and soft tissue [13], and pelvic infections [14].
Ertapenem seemed to have equal ecacy with the comparative agents. Side
eects recorded in the phase III trials included diarrhea and nausea in up to
7% of patients; headache in up to 6.5%; and localized infusion reactions of
3.2% to 15.3%, with the most common reaction being local erythema.
Hepatic transaminase elevations were noted in up to 9% and platelet count
increases were also seen in up to 3.2%. None of these were signicantly
dierent with the comparative agents in each trial. Seizures were rarely
recorded with a cumulative frequency of 0.2% in these patients. Again, no
signicant dierence was seen compared with the other b-lactams, piperacillin-tazobactam (0.3%) and ceftriaxone (0%) [4].
Although ertapenem may be seen as another carbapenem, it does have
several unique features separating it from both meropenem and imipenem.
606
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
Classically, the carbapenems have been used in the treatment of complicated
infections, particularly resistant nosocomial infections, or as broad-spectrum agents as drugs of last resort. Ertapenem may not t into the same
category because of some of its limitations in coverage. Ertapenems lack of
activity against nonfermenting organisms, particularly Pseudomonas and
Acinetobacter species, when compared with imipenem and meropenem, may
preclude it from this standard role. The otherwise broad-spectrum of
activity against most gram-positive, gram-negative, and anaerobic organisms makes it suitable for treatment of a whole host of infections as
mentioned previously. This use may be more appropriate for infections
acquired in the community, including mixed pathogens and pretreated
patients [4].
The most obvious advantage ertapenem oers is in its once-daily dosing.
Not only does this oer more convenience and less chance of nursing error
and drug-interaction problems during infusions, but it lends itself toward
outpatient and home intravenous antibiotic use. As the use of outpatient
intravenous therapy increases because of cost and patient preference issues,
the need for easily administered and eective agents increases. Polymicrobial or gram-negative infections, where ceftriaxone may have been used
before because of its once-daily dosing, may be better treated with the
broader-spectrum activity of ertapenem, which also includes anaerobes.
Osteomyelitis or intra-abdominal or pelvic infections involving mixed
bacteria are examples of situations in which ertapenem may be particularly
useful. There are no long-term data published to date, however, on the
eects of extended-duration of therapy or regarding bone penetration.
Cefditoren
Cefditoren is a third-generation orally administered cephalosporin.
Although available in Japan for a number of years, it was approved by
the FDA in September of 2001 for use in the United States by adults and
children 12 years of age or older. With the increase in multidrug-resistant
respiratory pathogens, particularly Streptococcus pneumoniae, the availability of an eective oral third-generation cephalosporin may be of use in
ambulatory settings for the treatment of respiratory tract infections.
The prodrug cefditoren pivoxil, formerly ME-1207, is an esteried
aminothiazolyl cephalosporin that passively diuses through the intestinal
membranes after ingestion. There it is hydrolyzed by esterase enzymes into
the active form cefditoren and an inactive metabolite, pivalate. The prodrug
does not enter the circulation intact, and seems to have no antimicrobial
activity [15]. Tablets come in 200-mg increments and also contain sodium
caseinate, a protein that may cross-react with patients who have milk
hypersensitivity. Once absorbed, dosages of 200 and 400 mg achieve plasma
concentrations of 2.46 mg/L [15] and 4.1 mg/L, respectively [16]. Although
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
607
food may have little eect on the rate of absorption itself, the fat content of
a meal can increase the plasma concentrations and bioavailability of the
drug, a phenomenon also common to other cephalosporin esters [17].
Various trials show that administering the drug after a meal increases the
peak plasma concentrations to a range of 2.62 to 3.1 mg/L for a 200-mg
dose, and 3.84 to 4.57 mg/L for a 400-mg dose [15]. Without the aid of fat in
absorption, cefditoren seems to have a bioavailability of only 14%. With
a low-fat meal (14 g of fat), this can increase to roughly 16%, and with
a high-fat meal (up to 64 g of fat), it can reach levels of almost 25% [18].
Direct drug-drug interactions seem minimal. The use of intravenous
antihistamine H2 blockers that decrease acid secretion led to a decrease in
drug levels. Likewise, oral antacids, such as aluminum and magnesium
hydroxide, also lower plasma concentrations [19]. Studies with proton pump
inhibitors are lacking, but it is recommended to avoid concomitant
administration based on the previously mentioned data.
Cefditoren does not seem to undergo any signicant metabolism, and is
excreted into the urine largely unchanged with a half-life of roughly 1.5
hours [15]. In the serum, it is highly protein-bound at 88% [20]. The inactive
metabolite, pivalate, is also renally excreted, but as the modied pivaloyl
carnitine. The binding of pivalate to carnitine can result in decreased levels
of the latter in patients. As such, it is generally not recommended for
patients with carnitine deciency or inborn errors of metabolism that result
in low levels of carnitine. Studies of 14-day regimens resulted in signicant
drops of serum carnitine levels, but the drops were less than 10% of total
body stores, an amount that is not expected to result in adverse clinical
eects in the average patient [21]. Moderate to severe renal insuciency
increases plasma concentrations of the drug and extends the half-life up to
a little over 5 hours depending on the extent of renal dysfunction [22].
Testing in mild to moderate hepatic insuciency has yielded no statistical
dierences in blood levels compared with healthy volunteers. Severe hepatic
dysfunction has yet to be tested [23].
Currently, the FDA has approved cefditoren pivoxil for use in treating
pharyngitis and tonsillitis, acute exacerbations of chronic bronchitis, and
uncomplicated skin and soft tissue infections. Like all cephalosporins,
cefditoren acts by binding to PBPs and interfering with the synthesis of
peptidoglycan cell wall synthesis of bacteria. Recommended dosages by the
manufacturer are 400 mg orally twice daily for 10 days to treat bronchitis
and 200 mg orally twice daily for 10 days to treat uncomplicated skin and
soft tissue infections. The manufacturer suggests not using higher than 200
mg twice daily with moderate renal insuciency, such as a creatinine
clearance less than 40 mL/L. In severe renal disease, a creatinine clearance
less than 10 mL/L, no more than 200 mg once daily, is recommended.
Cefditorens spectrum of activity covers a broad array of gram-positive
and gram-negative organisms, but notably lacks activity against Pseudomonas aeruginosa and many atypical pathogens implicated in pneumonia, such
608
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
as Mycoplasma, Chlamydia, and Legionella spp One in vitro study compared
cefditoren with the other third-generation cephalosporins cefotaxime and
ceftazidime, and cexime (no longer available in the United States) against
multiple organisms. Findings indicated equal activity with other thirdgeneration cephalosporins against Enterobacteriaceae, Haemophilus, and
Moraxella spp. Of note, cefditoren seemed to be the most active agent
against methicillin-sensitive staphylococci, but had no activity against
methicillin-resistant strains (methicillin-resistant S aureus), P aeruginosa,
or enterococci [24]. The three most common bacterial causes of communityacquired respiratory tract infections include S pneumoniae, Haemophilus
inuenzae, and Moraxella catarrhalis. Although advent of a vaccine against
H inuenzae type b has led to decreasing numbers of infections from this
organism, the rise of pneumococci with decreased susceptibility to penicillin,
other b-lactams, and other nonb-lactam agents continues to be a problem
[25]. In vitro data comparing cefditoren with other commonly used oral
cephalosporins for respiratory tract infections, such as cefdinir, cefuroxime,
cefprozil, cefpodoxime, and cexime, show some increased activity. Cefditoren had the lowest MICs for pneumococci with an MIC50 of less than or
equal to 0.016 mg/L and an MIC90 of 0.03 mg/L for penicillin-susceptible
strains, whereas penicillin-resistant MICs were at 0.5 and 2 mg/L, respectively. Cefpodoxime, the next most active of the oral cephalosporins,
gave corresponding values of less than or equal to 0.03 and less than or
equal to 0.03 mg/L for penicillin-susceptible pneumococci and 2 and 4 mg/L
for resistant strains [26]. Multiple other studies of in vitro ecacy conrm
that cefditoren is highly potent and bactericidal toward penicillin-susceptible and many penicillin-resistant pneumococci, groups A and B streptococci, b-lactamasenegative and b-lactamasepositive H inuenzae, and
b-lactamasepositive M catarrhalis. Highly resistant S pneumoniae, however, are resistant to ceftidoren. In addition, it seems to have activity against
Escherichia coli and methicillin-sensitive staphylococci. Ceftidoren has
activity against many organisms that typically cause respiratory tract and
cutaneous-related infections.
In vivo data come from trials of patients with pharyngitis, acute
exacerbations of chronic bronchitis, uncomplicated skin and soft tissue
infections, acute maxillary sinusitis, and community-acquired pneumonia.
The small studies regarding streptococcal pharyngitis found it to be of at
least equal ecacy and as well tolerated as penicillin VK [27]. Two recent
trials compared cefditoren with cefpodoxime and amoxicillin-clavulanate
for the treatment of community-acquired pneumonia in ambulatory settings
[28,29]. Both studies found cefditoren to be no dierent statistically in
treatment compared with the other agents. Doses of 200 mg twice daily
versus 400 mg twice daily seemed to be equally eective and well-tolerated.
Two trials have emerged comparing cefditoren with cefuroxime and
clarithromycin for the treatment of acute exacerbations of chronic bronchitis [30,31]. Again, cefditoren seemed to be of equal ecacy and as well
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
609
tolerated. In the one published trial for skin and soft tissue infections,
cefditoren was comparable with cefuroxime and cefadroxil for cure rate and
tolerability, including documented S aureus and Streptococcus pyogenes
infections [32].
These clinical trials and other unpublished data indicate that cefditoren
pivoxil is, overall, a well-tolerated medication with an acceptable safety
prole. The most common adverse events were gastrointestinal, with up to
14% of patients suering from diarrhea and up to 6% with nausea. The
diarrhea was higher in comparison with the other agents on average, and
was the most frequent cause of discontinuation of therapy by the patients.
Other common side eects were considered mild and seemed equally
common among the comparing agents. These included headache in 2%,
abdominal pain in 2%, vaginal candidiasis in up to 6%, and dyspepsia in up
to 2% [2631].
The in vitro data for cefditoren show promise for a number of pathogens,
most notably penicillin-resistant pneumococci and other respiratory pathogens with b-lactamase activity, such as H inuenzae and M catarrhalis.
Cefditoren notably lacks activity toward Pseudomonas, and is not indicated
in settings where it may be of concern. The in vivo data are somewhat
limited for cefditoren, however, and point toward equal ecacy with other
oral third-generation cephalosporins, but it has yet to be proved more
ecacious. It has not been studied in pregnant women and has been
assigned to category B by the FDA. Sucient studies are also lacking for the
treatment of children, and it is currently not approved for children under
age 12. Other possible indications may be using cefditoren pivoxil as an oral
step-down therapy in patients after intravenous courses of cefotaxime or
ceftriaxone.
Ceftidoren does not seem to have any unique aspects to separate it from
other oral third-generation cephalosporins. It is, however, the most active of
the oral cephalosporins against S pneumoniae.
High-dose amoxicillin-clavulanate
The combination of the b-lactam antibiotic amoxicillin with the blactamase inhibitor clavulanate is a well-established and commonly used
antimicrobial combination for the treatment of a broad array of infections
in both adults and children. Its safety and ecacy have been detailed in
numerous studies and reviews [3337]. Amoxicillin is a semisynthetic
analogue of ampicillin, and is derived from the basic penicillin nucleus, 6aminopenicillanic acid. Clavulanate is an acid produced from the fermentation of Streptomyces clavuligerus, which is structurally related to
penicillins, but has little antibacterial activity; it inactivates various blactamases produced by many pathogens [38]. In response to the recent
emergence of penicillin-resistant pneumococci, formulations containing
610
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
increased amounts of amoxicillin relative to the clavulanate component have
been made. Because the pneumococcal resistance is not b-lactamase
mediated, the clavulanic acid does not enhance sensitivity to these strains.
The clavulanic acid dosage is not raised in the dierent formulations to
avoid increased gastrointestinal side eects without any benet.
Both amoxicillin and clavulanate are well-absorbed from the gastrointestinal tract, and do not seem to be aected by the concentration of gastric acid
[39]. One study did nd reduced absorption when the medication was taken in
relation to a high-fat meal; however, other studies have found no particular
correlation with co-administration of food. The high-dose formulation seems
to be better absorbed when given at the beginning of a standard meal (24.9 g
of fat) [40]. Once administered, the peak plasma concentration typically
occurs in approximately 1 hour. The half-life of both amoxicillin and
clavulanate is also about 1 hour [39]. Peak plasma concentration using the
standard formulation is approximately 11 to 12 mg/L for amoxicillin and 2.2
mg/L for clavulanate. The high-dose formulation has a peak amoxicillin
concentration closer to 17 mg/L [41]. Amoxicillin seems to be excreted in the
urine largely unchanged, whereas clavulanate is more extensively metabolized by the body before being excreted also by the urinary tract [42].
Probenecid increases serum levels of amoxicillin but not clavulanate, because
clavulanate is excreted by glomerular ltration, whereas amoxicillin is mainly
excreted by tubular secretion [43].
Amoxicillin-clavulanate has been shown to be eective in the treatment
of otitis media, sinusitis, bronchitis, urinary tract infections, and skin and
soft tissue infections [44]. The addition of clavulanate enhanced the activity
against b-lactamaseproducing strains including S aureus; H inuenzae; M
catarrhalis; E coli; and some Klebsiella, Proteus, and Bacteroides species [45].
It has shown little to no ecacy for methicillin-resistant strains of S aureus,
and Pseudomonas, Serratia, Enterobacter, and Citrobacter species. Its
decreasing ecacy against emerging penicillin-resistant S pneumoniae has
resulted in a clinical dilemma for the treatment of many respiratory tract
infections, including sinusitis and otitis, where S pneumoniae is such
a prominent pathogen.
In 1999, a consensus group published a report regarding amoxicillin and
the treatment of acute otitis media [46]. Historically, S pneumoniae has been
considered the most important pathogen of this disease, causing close to
50% of cases, and with the emergence of drug-resistant pneumococcus and
increasing numbers of treatment failures, a review was undertaken by the
Drug Resistant Streptococcus pneumoniae Therapeutic Working Group,
convened by the Centers for Disease Control and Prevention in 1996. The
incidence of penicillin resistance among pneumococci was reported to be
34% of isolates according to one multistate laboratory survey at the time
[47]. The presence of resistant pneumococci was noted to be substantially
higher in children, especially those in day care and in those who had recently
received antibiotics [48].
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
611
Amoxicillin not only has a long record of safety and ecacy in treating
acute otitis media, but had previously demonstrated longest time above the
MIC90 against drug-resistant pneumococcus compared with many other
orally available agents [49]. Studies showed, however, that standard doses of
the drug (4045 mg/kg/d) achieved middle ear uid concentrations of 1 to 6
mg/L, a level that some considered ineectual in a proportion of cases [46].
Higher-dose therapy in the form of amoxicillin-clavulanate, 90 and 6.4 mg/
kg/d, divided for twice a day administration, achieved middle ear amoxicillin levels of 3 to 8 mg/L at 3 hours after the rst dose [50]. In vitro
pharmacokinetic modeling indicates that such levels should be sucient to
eliminate some penicillin-nonsusceptible strains of pneumococci [51].
Appropriate candidates for high-dose therapy (amoxicillin, 8090 mg/kg/d)
were patients who were considered to be at highest risk for infections with
drug-resistant S pneumoniae, such as patients with day care exposure,
previous antibimicrobial use in the last 3 months, and those 2 years old or
younger [46].
The Centers for Disease Control and Prevention panels recommendation
for its use led to a large, open-label, multicenter study for the treatment of
acute otitis media in children and infants [52]. A total of 521 patients were
enrolled between the ages of 3 and 48 months, with a mean age of 18.6
months, and treated with amoxicillin-clavulanate, 90 and 6.4 mg/kg/d in two
divided doses for 10 days. Baseline tympanocentesis was performed on all
children with intact tympanic membranes. Cultures of discharge were
obtained with swabs from perforated membranes. One or more pathogens
were isolated in 355 of the enrollees (68%). Pathogens included S pneumoniae, H inuenzae, M catarrhalis, and S pyogenes. H inuenzae was the most
commonly isolated (N = 197), 37% of which tested positive for blactamase. S pneumoniae was the second most commonly isolated organism
(N = 159), 55% of which were considered penicillin-susceptible, 18% were
penicillin-intermediate, and 28% were penicillin-resistant. M catarrhalis was
the third most commonly isolated pathogen (N = 30), all of which were blactamase positive. Repeat tympanocentesis was performed at days 4 to 6
irrespective of the ndings on original sample collection in three of the
centers. In 22 of the centers, repeat tympanocentesis was performed only if S
pneumoniae was recovered, and in any patient who experienced clinical
failure after day 4.
Follow-up cultures showed bacterial elimination from 96% of patients
undergoing repeat tympanocentesis. A previous study comparing normally
dosed amoxicillin with azithromycin for the treatment of acute otitis media
had shown an eradication rate of 83% [53]. Specically, 98% of any
S pneumoniae isolates, 94% of H inuenzae, and 100% of M catarrhalis were
eectively eradicated. The eradication for S pneumoniae with penicillin
resistance showing an MIC of less than or equal to 2 mg/L was greater than
95%. For even more resistant pneumococcus with an MIC of 4 mg/L, the
eradication rate was lower at 86%. Patients with penicillin-resistant
612
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
S pneumoniae were more likely to be younger and to have received
antibiotics within the last 3 months. Clinical cures or improvements were
achieved in 89% of evaluated patients at days 12 to 15.
Adverse events were noted in 14% of the patients who received at least
one dose of the medication (N = 71). The most commonly reported
associated eect was diaper rash (N = 21), followed by diarrhea
(N = 19), vomiting (N = 12), and other rash (N = 7). A total of 24 (5%)
of the patients had to be withdrawn from the study because of adverse
eects. In a previous trial, the safety and tolerability of high-dose
amoxicillin-clavulanate was examined in children for the treatment of acute
otitis media caused by drug-resistant S pneumoniae [54]. The incidence of
adverse events with twice daily administration of high-dose amoxicillinclavulanate was not signicantly dierent from that of conventional dosing.
The authors conducted a randomized, double-blind trial of 408 children
with acute otitis media. Diarrhea, dened as greater than or equal to three
watery stools per day or two watery stools per day for 2 consecutive days,
occurred in 11% of patients on high-dose formula and 8.8% on standard
dose regimens. Rates of vomiting were also similar between the two groups.
The new high-dose formulation of amoxicillin-clavulanate designed for
children is now indicated for recurrent or persistent acute otitis media
caused by S pneumoniae with penicillin MICs less than or equal to 2 mg/L.
Other b-lactamaseproducing pathogens, such as H inuenzae and M
catarrhalis, remain susceptible with this formulation. The new high-dose
formulation is not indicated or recommended, however, for highly penicillin-resistant strains (MICs greater than or equal to 4 mg/L). Children at risk
for infections with penicillin-resistant strains of S pneumoniae continue to be
those who have been exposed to antibiotics within the prior 3 months,
attend day care, or are 2 years of age or younger. Both the Sinus and Allergy
Health Partnership and American Thoracic Society recommend up to 3 g/
d of amoxicillin, plus or minus clavulanate, for adults in the treatment of
acute bacterial sinusitis and community-acquired pneumonia caused by S
pneumoniae with reduced susceptibility to penicillin [55,56]. The use of an
extended-time-release amoxicillin-clavulanic acid formulation (Augmentin
XR) may ease administration of higher doses, and has earned FDA
approval for both indications. Highly penicillin-resistant strains of S
pneumoniae (MICs greater than or equal to 4 mg/L) should not be treated
with amoxicillin or amoxicillin-clavulanic acid.
Cefepime
Cefepime is a parenterally administered fourth-generation cephalosporin
rst approved by the FDA in 1997. Cephalosporins are a broad group of
b-lactam antibiotics classied into generations, based loosely on their
spectrum of activity. Cefepime has been classied as a fourth-generation
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
613
cephalosporin, unique from the other three generations in its extended
spectrum of activity toward both gram-positive and gram-negative organisms and its stability toward b-lactamase hydrolysis [57]. The prototypic
cephalosporin is cephalosporin C, produced by the fungus Cephalosporium
acremonium. Various cephalosporins are derived from this one drug with
diering substitutions at two dierent side chains [58]. Cefepime is unique in
that it contains a positively charged quaternary ammonium group in
position C-3, creating a zwitterion that may enhance its ability to penetrate
the outer membranes of gram-negative bacteria. It also contains a 2aminothiazolylacetamido group in the side chain at the C-7 position, which
helps increase its resistance to degradation by various b-lactamases [57].
This group is not unique to cefepime, because the third-generation
cephalosporins, cefotaxime, ceftazidime, and ceftriaxone, also contain it.
In the seven-position side chain of cefepime, however, in place of the 2carboxy-2-propoxyimino group, there is an alkoxyimino substitution, which
is thought to grant cefepime-enhanced antistaphylococcal coverage [59].
Cefepime is administered in either intravenous or intramuscular preparations. The usual dose is 1 g every 12 hours, although it is often
administered in 2-g doses for severe infections, in smaller doses of 500 mg
in certain milder infections, and in doses of 250 to 500 mg in patients with
varying degrees of renal insuciency. Various trials have also administered
cefepime every 8 hours for serious infections. The pharmacokinetics of
cefepime seems to be linear, with peak serum concentrations of roughly 70
mg/L [60]. With a 2-g infusion, this approaches 150 mg/L [61]. When given
intramuscularly as a single dose, this level is one half to one third of the peak
IV level, although the bioavailability is unchanged at nearly 100% [62].
Interestingly, when compared with ceftriaxone intramuscular administration, cefepime seems to be better tolerated and less painful either with or
without lidocaine [63].
Once infused, cefepime distributes widely into most body tissues and uids
with a half-life of approximately 2 hours, independent of the dose [60].
Protein binding in human serum ranges from 15% to 20% [64]. Studies have
been conducted that measure cefepime levels in various body uids and
tissues, including bronchial mucosa, appendiceal tissue, and blister uid.
Average levels of 24.1 mg/kg, 4.8 mg/kg, and 30 to 35 mg/L were found,
respectively [6567]. In one study of infants and children aged 2 months to 15
years with either highly suspected or proved bacterial meningitis, cefepime
administered at 50 mg/kg resulted in cerebrospinal uid concentrations of 5.7
mg/L at 30 minutes after a single infusion and 3.3 mg/L after 8 hours [68].
Like most cephalosporins, cefepime is excreted by the kidneys. Eightyve percent appears unchanged in the urine, although the remainder is
metabolized by the body into N-methylpyrrolidine and the 7-epimer of
cefepime [69]. For patients with a creatinine clearance less than 60 mL/min,
the manufacturer recommends that the dose of cefepime be administered
every 24 hours, instead of the usual 12 hours. For patients with a clearance
614
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
less than 30 mL/min, the recommendation is that the dose be reduced by
half to 0.5 to 1 g every 24 hours depending on the severity of the infection.
With a creatinine clearance less than or equal to 10 mL/min, this should be
reduced again by half to 0.25 to 0.5 g every 24 hours [64].
As a b-lactam, cefepime targets cell wall synthesis by binding to PBPs in
the bacterial cell wall, thereby inhibiting peptidoglycan synthesis, and
ultimately leading to cell lysis. Cefepimes coverage is quite broad, with
activity against a large array of both gram-positive and gram-negative
pathogens. When compared with other cephalosporins, cefepimes coverage
toward gram-negative organisms is considered to be equivalent to that of
ceftazidime. For gram-positive bacteria, cefepime seems to be comparable
with that of cefotaxime, generally surpassing that of ceftazidime [70].
Methicillin-resistant S aureus, methicillin-resistant Staphylococcus epidermidis, Enterococcus spp, Clostridium dicile, and Listeria monocytogenes seem
to be resistant to cefepime [71,72]. Streptococci, including moderately
penicillin-resistant S pneumoniae, and methicillin-sensitive S aureus seem
to be susceptible to cefepime [71,73].
Cefepime is unique among the cephalosporins in its frequent resistance to
hydrolysis by many of the inducible b-lactamases produced by gramnegative bacteria [74]. It is also known to enter many bacterial cells more
quickly than other third-generation cephalosporins and has a high anity
for many PBPs, including PBP1 and PBP3 in E coli and P aeruginosa. Not
only does it have activity equal to or greater than ceftazidime or cefotaxime
against many common gram-negative pathogens, such as Klebsiella pneumoniae, E coli, Serratia marcescens, H inuenzae, and Proteus, Salmonella, and
Shigella species, but cefepime also exhibits activity against certain other
isolates that can be resistant to the third-generation cephalosporins [75].
Enterobacter and Citrobacter species, in particular, can remain susceptible
when resistance to the third-generation cephalosporins is seen. Cefepimes
activity against P aeruginosa seems to be similar to ceftazidime in many
studies. Cefepime has activity against occasional P aeruginosa isolates that
are ceftazidime resistant. Other highly resistant gram-negative rods, such as
Burkholderia cepacia and S maltophilia, can be variable in susceptibility to
cefepime, and resistance is seen in many strains. Bacteroides fragilis is
generally considered resistant, whereas Neisseria gonorrhoeae and Neisseria
meningitidis are highly susceptible to cefepime.
Cefepime is well-tolerated, and adverse events are uncommon and usually
mild. In comparison with ceftazidime, there was no statistically signicant
dierence in the types and rate of many side eects. The rate of adverse
events was 13.8% for cefepime versus 15.6% for ceftazidime in comparison
trials between the two drugs. Headache was the most commonly reported at
2.4%, followed by nausea and rash at 1.8% each. Unlike some other
cephalosporins, cefepime does not contain an N-methylthiotetrazole sidechain that has been known to cause elevated prothrombin times and
disulram-like reactions. Overall, there does not seem to be a relationship
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
615
between duration of therapy or underlying renal or hepatic dysfunction and
the frequency of adverse events. Rash, which is the most common reason for
discontinuing cefepime, does seem to be dose-related [76].
Cefepime is approved to treat uncomplicated and complicated urinary
tract infections, moderate to severe respiratory tract infections, and
uncomplicated skin and soft tissue structure infections. It has been shown
to be eective in intra-abdominal infections, gynecologic infections, febrile
neutropenia, and meningitis in pediatric patients as well. It has yet to be
thoroughly evaluated for treating meningitis in adults. Its value in treating
severe infections, with or without other agents, is well-established, particularly in hospital-acquired infections where resistant organisms may play
a larger role. For instance, P aeruginosa and Enterobacteriaceae may be
more prominent in these infections. It has been suggested that use of
cefepime over ceftazidime may help decrease the emergence of resistance
among Enterobacteriaceae. Compared with third-generation cephalosporins, cefepime is less likely to select for organisms producing high levels of
chromosomal-mediated b-lactamase. In addition, cefepime sometimes
retains activity against organisms, hyperproducing chromosomal b-lactamase that are ceftazidime resistant. Resistance can develop, however, while
on therapy with cefepime [77].
With now well-established clinical experience and characteristics that
make it unique among the other approved cephalosporins, cefepime seems
to have earned its designation as a fourth-generation cephalosporin. The use
of cefepime, however, ultimately depends on local resistance patterns and
pharmacoeconomics to determine its value.
Summary
The number of b-lactam antibiotics continues to grow and change,
largely in response to developing bacterial resistance. These include new
antibiotics and new formulations of old antibiotics. The b-lactams described
here are some of the most recently approved antibiotics in the United States.
These agents have novel features that should provide advantages over
previously available antibiotics in certain situations. The decision to use any
of these newer agents over other, older antibiotics, however, should be
determined on an individual basis after full clinical evaluation.
References
[1] Kohler J, Dorso K, Young K, et al. In vitro activities of the potent, broad-spectrum
carbapenem MK-0826 against broad-spectrum b-lactamase- and extended-spectrum blactamase-producing Klebsiella pneumoniae and Escherichia coli clinical isolates. Antimicrob Agents Chemother 1999;43:11706.
[2] Majumdar AK, Musson DG, Birk KL, et al. Pharmacokinetics of ertapenem in healthy
young volunteers. Antimicrob Agents Chemother 2002;46:350611.
616
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
[3] Legua P, Lema J, Moll J, et al. Safety and local tolerability of intramuscularly
administered ertapenem diluted in lidocaine: a prospective, randomized, double-blind
study versus intramuscular ceftriaxone. Clin Ther 2002;24:43444.
[4] Shah PM, Isaacs RD. Ertapenem, the rst of a new group of carbapenems. J Antimicrob
Chemother 2003;52:53842.
[5] Livermore DM, Carter MW, Bagel S, et al. In vitro activities of ertapenem (MK-0826)
against recent clinical bacteria collected in Europe and Australia. Antimicrob Agents
Chemother 2001;45:18607.
[6] Goldstein EJC, Citron DM, Merriam CV, et al. Comparative in vitro activities of
ertapenem (MK-0826) against 1,001 anaerobes isolated from human intra-abdominal
infections. Antimicrob Agents Chemother 2000;44:238994.
[7] Friedland IR, Isaacs R, Mixson LA, Motyl M, Woods GL. Use of surrogate antimicrobial
agents to predict susceptibility to ertapenem. Diagn Microbial Infect Dis 2002;43:614.
[8] Ortiz-Ruiz G, Caballero-Lopez J, Friedland IR, Woods GL, Carides A. The Protocol 018
Ertapenem Community-Acquired Pneumonia Study Group. A study evaluating the
ecacy, safety, and tolerability of ertapenem versus ceftriaxone for the treatment of
community-acquired pneumonia in adults. Clin Infect Dis 2002;34:107683.
[9] Vetter N, Cambronero-Hernandez E, Rohlf J, et al. A prospective, randomized, doubleblind multicenter comparison of parenteral ertapenem and ceftriaxone for treatment of
hospitalized adults with community-acquired pneumonia. Clin Ther 2002;24:177085.
[10] Tomera KM, Burdmann EA, Pamo Reyna OG, et al. Ertapenem versus ceftriaxone
followed by appropriate oral therapy for treatment of complicated urinary tract infections
in adults: results of a prospective, randomized, double-blind multicenter study. Antimicrob
Agents Chemother 2002;46:2895900.
[11] Jimenez-Cruz F, Jasovich A, Cajigas J, et al. A prospective, multicenter, randomized, doubleblind study comparing ertapenem and ceftriaxone followed by appropriate oral therapy for
treatment of complicated urinary tract infections in adults. Urology 2002;60:1622.
[12] Solomkin JS, Yellin AE, Rotstein OD, et al. Ertapenem versus piperacillin/tazobactam in
the treatment of complicated intra-abdominal infections. Ann Surg 2003;237:23545.
[13] Graham DR, Lucasti C, Malafaia O, et al. Ertapenem once daily versus piperacillintazobactam 4 times per day for treatment of complicated skin and skin-structure infections
in adults: results of a prospective, randomized, double-blind multicenter study. Clin Infect
Dis 2002;34:14608.
[14] Roy S, Higareda I, Angel-Muller E, et al. Ertapenem once a day versus piperacillintazobactam every 6 hours for treatment of acute pelvic infections: a prospective,
multicenter, randomized double-blind study. Infect Dis Obstet Gynecol 2003;11:111.
[15] Li JT, Hou F, Lu H, et al. Phase I clinical trial of cefditoren pivoxil (ME 1207):
pharmacokinetics in healthy volunteers. Drugs Exp Clin Res 1997;23:14550.
[16] Kuti JL, Quintiliani R. Cefditoren pivoxil. Formulary 2001;36:26575.
[17] Kneer J. Pharmacokinetic properties of new oral cephalosporins. Med Mal Infect 1992;22:
55664.
[18] Darkes MJM, Plosker GL. Cefditoren pivoxil. Drugs 2002;62:31936.
[19] Mayer M, Mulford D, Witt G. Eect of an H2 receptor antagonist or an antacid on the
pharmacokinetics of cefditoren [abstract]. In: Programs and abstracts of the 40th annual
interscience conference on antimicrobial agents and chemotherapy. Washington: American
Society for Microbiology: 2000. poster no. 313.
[20] TAP Pharmaceuticals. Spectracef (cefditoren) package insert. Lake Forest (IL): TAP
Pharmaceuticals; 2001.
[21] Brass EP, Mayer MD, Mulford DJ, et al. Impact on carnitine homeostasis of short-term
treatment with the pivalate prodrug cefditoren pivoxil. Clin Pharmacol Ther 2003;73:
33847.
[22] Mulford D, Mayer M, Witt G. Eect of renal impairment on the pharmacokinetics of
cefditoren [abstract]. In: Programs and abstracts of the 40th annual interscience conference
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
[23]
[24]
[25]
[26]
[27]
[28]
[29]
[30]
[31]
[32]
[33]
[34]
[35]
[36]
[37]
[38]
[39]
[40]
[41]
[42]
617
on antimicrobial agents and chemotherapy. Washington: American Society for Microbiology; 2000. poster no. 311.
Mayer M, Mulford D, Witt G. Eect of hepatic impairment on the pharmacokinetics of
cefditoren [abstract]. In: Programs and abstracts of the 41st annual interscience conference
on antimicrobial agents and chemotherapy. Washington: American Society for Microbiology; 2001. poster no. 312.
Chin NX, Zhang YX, Neu HC. In vitro activity of a new cephalosporin ME-1206
compared with other agents. Diagn Microbiol Infect Dis 1991;14:41724.
Jacobs MR, Bajaksouzian S, Zilles A, et al. Susceptibilities of Streptococcus pneumoniae
and Haemophilus inuenzae to 10 oral antimicrobial agents based on pharmacodynamic
parameters: 1997 USA surveillance study. Antimicrob Agents Chemother 1999;43:19018.
Clark CL, Nagai K, Dewasse BE, et al. Activity of cefditoren against respiratory
pathogens. J Antimicrob Chemother 2002;50:3341.
Kaplan EL, Tucker RM, Poling TL, et al. A multicenter comparison of cefditoren pivoxil
and penicillin VK. J Respir Dis 2001;22(Suppl 8):604.
van Zyl L, le Roux JG, LaFata JA, et al. Cefditoren pivoxil versus cefpodoxime proxetil
for community-acquired pneumonia: results of a multicenter, prospective, randomized,
double-blind study. Clin Ther 2002;24:184053.
Fogarty CM, Cyganowski M, Palo WA, et al. A comparison of cefditoren pivoxil and
amoxicillin/clavulanate for the treatment of community-acquired pneumonia: a multicenter, prospective, randomized, investigator-blinded, parallel-group study. Clin Ther 2002;
24:185470.
Henry DC, Poling TL, Bettis RB, et al. A double-blind, randomized study of cefditoren
versus cefuroxime for acute exacerbations of chronic bronchitis (AECB). J Respir Dis
2001;22(Suppl 8):6974.
Ramirez JA, Tucker RM, Bettis RB, et al. Treating acute exacerbations of chronic
bronchitis. J Respir Dis 2001;22(Suppl 8):7580.
Bucko AD, Hunt BJ, Kidd SL, et al. Randomized, double-blind, multicenter comparison
of oral cefditoren 200 or 400mg bid with either cefuroxime 250 mg bid or cefadroxil 500 mg
bid for the treatment of uncomplicated skin and skin-structure infections. Clin Ther 2002;
24:113447.
Brogden RN, Carmine A, Heel RC, et al. Amoxycillin/clavulanic acid: a review of its
antibacterial activity, pharmacokinetics and therapeutic use. Drugs 1981;22:33762.
Weber DJ, Tolko-Rubin NE, Rubin RH. Amoxicillin and potassium clavulanate: an
antibiotic combination: mechanism of action, pharmacokinetics, antimicrobial spectrum,
clinical ecacy and adverse eects. Pharmacotherapy 1984;4:12236.
Stein GE, Gurwith MJ. Amoxicillin-potassium clavulanate, a b-lactamase-resistant
antibiotic combination. Clin Pharm 1984;3:5919.
Smith BR, LeFrock JL. Amoxicillin-potassium clavulanate: a novel b-lactamase inhibitor.
Drug Intell Clin Pharm 1985;19:41520.
Todd PA, Beneld P. Amoxicillin/clavulanic acid: an update of its antibacterial activity,
pharmacokinetic properties and therapeutic use. Drugs 1990;39:264307.
Neu HC, Fu KP. Clavulanic acid, a novel inhibitor of b-lactamases. Antimicrob Agents
Chemother 1984;14:6505.
Jackson D, Cooper DL, Horton R, et al. Augmentin: absorption, excretion and
pharmacokinetic studies in man. Postgrad Med 1984;76:5170.
GlaxoSmithKline. Augmentin XR (amoxicillin-clavulanate) package insert. Research
Triangle Park (NC): GlaxoSmithKline; 2003.
Kaye C, Allen A, Perry S, et al. The clinical pharmacokinetics of a new pharmacokinetically enhanced formulation of amoxicillin/clavulanate. Clin Ther 2001;23:57884.
Adam D, De Visser I, Koeppe P. Pharmacokinetics of amoxicillin and clavulanic
acid administered alone and in combination. Antimicrob Agents Chemother 1982;22:
3537.
618
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
[43] Staniforth DH, Jackson D, Clark HL, et al. Amoxycillin/clavulanic acid: the eect of
probenecid. J Antimicrob Chemother 1983;12:2735.
[44] Amoxicillin-clavulanic acid (Augmentin). Med Lett Drugs Ther 1984;26:99100.
[45] Fuchs PC, Barry AL, Thornsberry C, et al. In vitro evaluation of Augmentin by both
microdilution and disk diusion susceptibility testing: regression analysis, tentative interpretive criteria, and quality control limits. Antimicrob Agents Chemother 1983;24:318.
[46] Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance
in an era of pneumococcal resistance: report from the Drug-Resistant S. pneumoniae
Therapeutic Working Group. Pediatr Infect Dis J 1999;18:19.
[47] Thornsberry C, Ogilvie P, Kahn J, Mauriz Y. Surveillance of antimicrobial resistance in
Streptococcus pneumoniae, Haemophilus inuenzae, and Moraxella catarrhalis in the United
States in 1996-1997 respiratory season. Diagn Microbiol Infect Dis 1997;29:24957.
[48] Dowell SF, Schwartz B. Resistant pneumococci: protecting patients through judicious use
of antibiotics. Am Fam Physician 1997;55:164754.
[49] Craig WA, Andes D. Pharmacokinetics and pharmacodynamics of antibiotics in otitis
media. Pediatr Infect Dis J 1996;15:2559.
[50] Seikel K, Shelton S, McCracken GH. Middle ear uid concentrations of amoxicillin after
large dosages in children with acute otitis media. Pediatr Infect Dis J 1997;16:7101.
[51] Lister PD, Pong A, Chartrand SA, Sanders CC. Rationale behind high-dose amoxicillin
therapy for acute otitis media due to penicillin-nonsusceptible pneumococci: support from
in vitro pharmacodynamic studies. Antimicrob Agents Chemother 1997;41:192632.
[52] Dagan R, Hoberman A, Johnson C, et al. Bacteriologic and clinical ecacy of high dose
amoxicillin/clavulanate in children with acute otitis media. Pediatr Infect Dis J 2001;20:
82937.
[53] Dagan R, Johnson CE, McLinn S, et al. Bacteriologic and clinical ecacy of amoxicillin/
clavulanate vs. azithromycin in acute otitis media. Pediatr Infect Dis J 2000;19:95104.
[54] Botteneld GW, Burch DJ, Hedrick JA, et al. Safety and tolerability of a new formulation
(90 mg/kg/day divided every 12h) of amoxicillin/clavulanate (Augmentin) in the empiric
treatment of pediatric acute otitis media caused by drug-resistant Streptococcus pneumoniae. Pediatr Infect Dis J 1998;17:9638.
[55] Sinus and Allergy Health Partnership. Antimicrobial treatment guidelines for acute
bacterial rhinosinusitis. Otolaryngol Head Neck Surg 2000;123:S132.
[56] American Thoracic Society. Guidelines for the management of adults with communityacquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and
prevention. Am J Respir Crit Care Med 2001;163:173054.
[57] Sanders CC. Cefepime: the next generation? Clin Infect Dis 1993;17:36979.
[58] Marshall WF, Blair JE. The cephalosporins. Mayo Clin Proc 1999;74:10795.
[59] Naito T, Aburaki S, Kamachi H, et al. Synthesis and structure activity relationships of
a new series of cephalosporins, BMY-28142 and related compounds. J Antibiot (Tokyo)
1986;39:1092107.
[60] Barbhaiya RH, Forgue ST, Gleason CR, et al. Pharmacokinetics of cefepime after single
and multiple intravenous administrations in healthy subjects. Antimicrob Agents Chemother 1992;36:5527.
[61] Barbhaiya RH, Forgue ST, Gleason CR, et al. Safety, tolerance, and pharmacokinetic
evaluation of cefepime after administration of single intravenous doses. Antimicrob Agents
Chemother 1990;34:111822.
[62] Barbhaiya RH, Knupp CA, Tenney J, et al. Safety, tolerance, and pharmacokinetics of
cefepime administered intramuscularly to healthy subjects. J Clin Pharmacol 1990;30:
90010.
[63] Gubbelmans HL, Materman EC, Maesen FP. Cefepime versus ceftriaxone: a tolerance
study by intramuscular injection. Drug Ther Res 1990;15:1246.
[64] Bristol-Myers Squibb. Maxipime (cefepime) package insert. Princeton, NJ: Bristol-Myers
Squibb; 1996.
S.I. Martin, K.M. Kaye / Infect Dis Clin N Am 18 (2004) 603619
619
[65] Chadha D, Wise R, Baldwin DR, et al. Cefepime concentrations in bronchial mucosa and
serum after a single 2 gram intravenous dose. J Antimicrob Chemother 1990;25:95963.
[66] Okamoto MP, Chin A, Gill MA, et al. Analysis of cefepime tissue penetration into human
appendix. Pharmacotherapy 1991;11:3538.
[67] Kalman D, Barriere SL, Johnson BL. Pharmacokinetic disposition and bactericidal
activities of cefepime, ceftazidime, and cefoperazone in serum and blister uid. Antimicrob
Agents Chemother 1991;36:4537.
[68] Saez-Llorens X, Castano E, Garcia R, et al. Prospective randomised comparison of
cefepime and cefotaxime for treatment of bacterial meningitis in infants and children.
Antimicrob Agents Chemother 1995;39:93740.
[69] Barbhaiya RH, Knupp CA, Forgue ST, et al. Disposition of the cephalosporin cefepime in
normal and renally impaired subjects. Diagn Metab Dispos 1991;19:6873.
[70] Wynd MA, Paladino JA. Cefepime: a fourth generation parenteral cephalosporin. Ann
Pharmacother 1996;30:141424.
[71] Kessler RE, Bies M, Buck RE, et al. Comparison of a new cephalosporin, BMY-28142,
with other broad spectrum beta-lactam antibiotics. Antimicrob Agents Chemother 1985;
27:20716.
[72] Rolston KV, Alvarez ME, Hsu KC, et al. In vitro activity of cefpirome (HR-810), WIN49375, BMY-28142, and other antibiotics against nosocomially important isolates from
cancer patients. J Antimicrob Chemother 1986;17:4537.
[73] Conrad DA, Scribner RK, Weber AH, Marks MI. In vitro activity of BMY-28142 against
pediatric pathogens, including isolates from cystic brosis sputum. Antimicrob Agents
Chemother 1985;28:5863.
[74] Sanders WE Jr, Tenney JH, Kessler RE. Ecacy of cefepime in the treatment of infections
due to multiply resistant Enterobacter species. Clin Infect Dis 1996;23:45461.
[75] Kessler RE, Fung-Tomc J. Susceptibility of recent bacterial isolates from the cefepime
clinical trials in the United States. Am J Med 1993;95:107.
[76] Neu HC. Safety of cefepime: a new extended-spectrum cephalosporin antibiotic. Am J
Med 1993;95:6774.
[77] Acar J. Rapid emergence of resistance to cefepime during treatment. Clin Infect Dis 1998;
26:14846.
You might also like
- SCCCDocument8 pagesSCCCYampold Estheben ChusiNo ratings yet
- CMAR 52217 Regorafenib For The Treatment of Metastatic Colorectal Cance 030414Document11 pagesCMAR 52217 Regorafenib For The Treatment of Metastatic Colorectal Cance 030414Yampold Estheben ChusiNo ratings yet
- Goal-Directed Resuscitation For Patients With Early Septic ShockDocument11 pagesGoal-Directed Resuscitation For Patients With Early Septic ShockYampold Estheben ChusiNo ratings yet
- Goal-Directed Resuscitation For Patients With Early Septic ShockDocument11 pagesGoal-Directed Resuscitation For Patients With Early Septic ShockYampold Estheben ChusiNo ratings yet
- OtitisDocument4 pagesOtitisNegroNo ratings yet
- JNC 8Document14 pagesJNC 8amiwahyuniNo ratings yet
- Preclinical and Clinical Overview of Terpenes in The Treatment of UrolithiasisDocument5 pagesPreclinical and Clinical Overview of Terpenes in The Treatment of UrolithiasisYampold Estheben ChusiNo ratings yet
- Guia 2008 Sobreviviendo A La Sepsis INGLESDocument44 pagesGuia 2008 Sobreviviendo A La Sepsis INGLESVlady78No ratings yet
- Decolonization SamrDocument7 pagesDecolonization SamrYampold Estheben ChusiNo ratings yet
- Lower Respiratory Tract Infections: Prevention Using VaccinesDocument19 pagesLower Respiratory Tract Infections: Prevention Using VaccinesYampold Estheben ChusiNo ratings yet
- FN 2011 IdsaDocument38 pagesFN 2011 IdsaNuttawath UngwichanpunyaNo ratings yet
- Antibiotics For Gram+ Bacterial Infections...Document18 pagesAntibiotics For Gram+ Bacterial Infections...Yampold Estheben ChusiNo ratings yet
- Diabetic Foot InfectionsDocument7 pagesDiabetic Foot InfectionsYampold Estheben ChusiNo ratings yet
- Staphylococcus Aureus Bacteremia and EndocarditisDocument23 pagesStaphylococcus Aureus Bacteremia and EndocarditisYampold Estheben ChusiNo ratings yet
- Fungalarthritis and OsteomyelitisDocument21 pagesFungalarthritis and OsteomyelitisYampold Estheben ChusiNo ratings yet
- Current Best Practices and Guidelines-Indications For Surgical Intervention in Infective EndocarditisDocument23 pagesCurrent Best Practices and Guidelines-Indications For Surgical Intervention in Infective EndocarditisYampold Estheben ChusiNo ratings yet
- Pathogenesis of Streptococcal and Staphylococcal EndocarditisDocument22 pagesPathogenesis of Streptococcal and Staphylococcal EndocarditisYampold Estheben ChusiNo ratings yet
- Infective Endocarditis PrefaceDocument5 pagesInfective Endocarditis PrefaceYampold Estheben ChusiNo ratings yet
- Topical Antibacterial AgentsDocument17 pagesTopical Antibacterial AgentsYampold Estheben ChusiNo ratings yet
- Diagno 3Document16 pagesDiagno 3Yampold Estheben ChusiNo ratings yet
- Tropical and Temperate PyomyositisDocument9 pagesTropical and Temperate PyomyositisYampold Estheben ChusiNo ratings yet
- Update On Musculoskeletal Infections: PrefaceDocument2 pagesUpdate On Musculoskeletal Infections: PrefaceYampold Estheben ChusiNo ratings yet
- Prosthetic Joint InfectionsDocument30 pagesProsthetic Joint InfectionsYampold Estheben ChusiNo ratings yet
- Fungalarthritis and OsteomyelitisDocument21 pagesFungalarthritis and OsteomyelitisYampold Estheben ChusiNo ratings yet
- The Newer FluoroquinolonesDocument26 pagesThe Newer FluoroquinolonesYampold Estheben ChusiNo ratings yet
- Current Best Practices and Guidelines-Indications For Surgical Intervention in Infective EndocarditisDocument23 pagesCurrent Best Practices and Guidelines-Indications For Surgical Intervention in Infective EndocarditisYampold Estheben ChusiNo ratings yet
- Use of Antibacterial Agents in Renal FailureDocument29 pagesUse of Antibacterial Agents in Renal FailureYampold Estheben ChusiNo ratings yet
- Staphylococcus Aureus Bacteremia and EndocarditisDocument23 pagesStaphylococcus Aureus Bacteremia and EndocarditisYampold Estheben ChusiNo ratings yet
- Infections of Intracardiac Devices PDFDocument29 pagesInfections of Intracardiac Devices PDFYampold Estheben ChusiNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Antibiotic TableDocument5 pagesAntibiotic TableLiana Et Murat KalabalikNo ratings yet
- Saldo Penerimaan & Pengeluaran07 - Maret - 2021Document34 pagesSaldo Penerimaan & Pengeluaran07 - Maret - 2021Desi Yuliana HarahapNo ratings yet
- Medicine Price List MPL Acute and Chronic November 2020Document123 pagesMedicine Price List MPL Acute and Chronic November 2020karar hussainNo ratings yet
- No Kode Obat Nama Obat SAT Saldo Awal Barang Masuk Barang Keluar Sisa Barang (HMS) QYT RP (HB) QYT RP (HB) QYT RP (HB) QYTDocument32 pagesNo Kode Obat Nama Obat SAT Saldo Awal Barang Masuk Barang Keluar Sisa Barang (HMS) QYT RP (HB) QYT RP (HB) QYT RP (HB) QYTfarmasirshbNo ratings yet
- 2017 (Laporan Pelayanan Rawat Jalan Dr. Ida Ayu Anom Margareni)Document11 pages2017 (Laporan Pelayanan Rawat Jalan Dr. Ida Ayu Anom Margareni)Anggi RiyaniNo ratings yet
- ReportViewer Aspx PDFDocument2 pagesReportViewer Aspx PDFAmir ZamanNo ratings yet
- PDF Glee ProductsDocument1 pagePDF Glee ProductsSaurabh BishtNo ratings yet
- Antimicrobial AgentDocument46 pagesAntimicrobial Agentسامر الرفاعيNo ratings yet
- Ertapenem Review of New CarbapenemDocument17 pagesErtapenem Review of New CarbapenemFra1312No ratings yet
- Pharmacology - Mechanism of Action of All Drugs - +Document4 pagesPharmacology - Mechanism of Action of All Drugs - +Sahal ShaikhNo ratings yet
- Komposisi Dosis Nama Obat: AntibiotikaDocument12 pagesKomposisi Dosis Nama Obat: Antibiotikahilman fauzanNo ratings yet
- Micro 1 - Antibiotics TableDocument4 pagesMicro 1 - Antibiotics TableVenice RamosNo ratings yet
- Pricelist 17 November 2020Document21 pagesPricelist 17 November 2020Diana Nurrah AshariNo ratings yet
- Veltri Drug Cards - Quiz 1Document1 pageVeltri Drug Cards - Quiz 1starobinNo ratings yet
- Antibiotice PDFDocument1 pageAntibiotice PDFAlex Alex0% (2)
- Dosis Antbiotik by Dr. RidhaDocument5 pagesDosis Antbiotik by Dr. RidhaaliNo ratings yet
- MicrobialsDocument5 pagesMicrobialsMARIEMIL FOLLOSONo ratings yet
- Summary For Antibiotic For USMLE Exam - USMLE MaterialsDocument6 pagesSummary For Antibiotic For USMLE Exam - USMLE MaterialsAshik ThapaNo ratings yet
- Nama Antibiotik Regimen Dosis Dosis Per-Hari Rute No Kode PasienDocument10 pagesNama Antibiotik Regimen Dosis Dosis Per-Hari Rute No Kode PasienAri AnggaraNo ratings yet
- CephalosporinsrinDocument25 pagesCephalosporinsrinIsrar Qureshi100% (1)
- Anti Infective TherapyDocument78 pagesAnti Infective TherapyMax LocoNo ratings yet
- Cep Halo Sporin SDocument9 pagesCep Halo Sporin SJasper VictoriaNo ratings yet
- Tabel Activitate AntibioticeDocument1 pageTabel Activitate Antibioticebo6danbo6danNo ratings yet
- List 14 07 21Document93 pagesList 14 07 21Herowati WidjajaNo ratings yet
- Stok BernoDocument6 pagesStok BernoYulius RobinsonNo ratings yet
- PT - Permata Delta Agung: Halaman: (All)Document35 pagesPT - Permata Delta Agung: Halaman: (All)abdul husainNo ratings yet
- Synchro Pharmaceuticals: Price ListDocument1 pageSynchro Pharmaceuticals: Price ListRana TayyabNo ratings yet
- AntibiotikkDocument2 pagesAntibiotikkResa ElitaNo ratings yet
- 21 Cephalosp 2015 Mandell Douglas and Bennett S Principles and PracticeDocument20 pages21 Cephalosp 2015 Mandell Douglas and Bennett S Principles and PracticeHelen DyNo ratings yet
- Medication Card Case.2Document6 pagesMedication Card Case.2Jemina Rafanan RacadioNo ratings yet