Professional Documents
Culture Documents
Case 4
Uploaded by
Maine AsuncionOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case 4
Uploaded by
Maine AsuncionCopyright:
Available Formats
Case 3 A 50 year old female presents at the OPD with symptoms of fatigue,
increased thirst & frequent urination. Her family history is significant for obesity,
diabetes & hypertension. Two of her 4 children had birthweights of over 9 pounds.
PE revealed a BMI of 34, blood pressure of 150/90 mm Hg and there was noted
weakness of both upper & lower extremities. Lab tests reveal a random blood sugar
of 260 mg/dL which was confirmed with a fasting plasma glucose of 193 mg/dL.
Guide Questions
1. What is your diagnosis? Describe the mechanism in the development of the
disease.
TYPE 2 DIABETES MELLITUS is a heterogeneous syndrome
characterized by abnormalities in carbohydrate and fat metabolism. The
causes of type 2 diabetes are multi-factorial and include both genetic and
environmental elements that affect beta-cell function and tissue (muscle,
liver, adipose tissue, pancreas) insulin sensitivity. It is characterized by an
insulin resistance combined with a relative deficiency in insulin secretion
leading to an unused supply of glucose in the blood (hyperglycemia) and its
toxicities.
2. What drug should be used as initial therapy? Describe its mechanism of
action and expected adverse reactions expected.
The standard therapy for diabetic patients is intensive glycemic control
and targeting near-normal glucose control associated with comprehensive
self-management. In pharmacologic treatment, however, Metformin is a firstline consideration. Metformin decreases hepatic glucose output through the
activation of AMP-activated protein kinase (AMPK) and, to a lesser extent,
sensitizes peripheral tissues to insulin. The most common toxic effects of
metformin are gastrointestinal (nausea, vomiting, abdominal discomfort and
diarrhea) which occur in 20% of patients. These are dose-related, tend to
occur at the onset of therapy, and are often transient.
Also, since there is a mild dysfunction of the beta-cells in the pancreas,
insulin therapy may also be a choice for these patients.
3. In case of clinical failure with the above drug, what drug can be used as
second agent. Describe their mechanisms of action and adverse reactions
expected. Which one is preferred? Why?
If metformin doesnt work, then possible second line treatments would
be Sulfonylureas (less expensive, with risk of hypoglycemia) or
Thiazolidenediones (more expensive, no risk of hypoglycemia).
Sulfonuylurea insulin secretagogues (e.g., glipizide [Glucotrol],
glimepiride [Amaryl]) and nonsulfonylurea insulin secretagogues (e.g.
nateglinide [Starlix]) increase insulin secretion by closing potassium channels
on the surface of pancreatic beta cells. Hypoglycemia can occur with any
insulin secretagogue. Sulfonylureas can cause weight gain; this effect is less
common with nonsulfonylurea secretagogues.
Thiazolidinediones increase insulin sensitivity in peripheral tissues and,
to a lesser extent, decrease hepatic glucose production. These agents will not
cause hypoglycemia when used as monotherapy. Thiazolidinediones (TZDs)
are agonists of peroxisome proliferator-activated receptor gamma (PPAR) and
primarily enhance sensitivity of muscle and fat, and mildly of the liver, to
exogenous and endogenous insulin. TZDs lower fasting and postprandial
blood glucose levels.
Thiazolidenediones would be a good choice since it can be taken only
once a day, however, studies suggest that these types of drugs increase the
risk of cardiovascular complications, especially to person with a
cardiovascular disease already so the decision would be up to the doctor
giving the medicine and the situation of the patient.
4. Describe possible third and fourth line therapy including mechanisms of
action and adverse reactions associated.
1. Alpha glucosidase inhibitors competitively block the enzyme alpha
glucosidase in the brush borders of the small intestine, which delays
absorption of carbohydrates (absorbed in the mid and distal portions of
the small intestine instead). They primarily target postprandial
hyperglycemia without causing hypoglycemia. GI complaints, such as
bloating, abdominal cramps, flatulence, and diarrhea are the main side
effects.
2. Incretin-based therapies can be used as injections (GLP-1 analogs) or as
pills (DPP-4 inhibitors). All incretin-based medications carry increased risk
of acute pancreatitis. Patients must be warned about this risk and be
advised to stop taking these medications and seek medical evaluation if
acute abdominal pain develops.
3. SGLT-2 inhibitors are the newest group of medications approved for
treatment of diabetes mellitus. SGLT-2 is a protein acting as sodiumglucose co-transporter in the kidneys proximal tubules whose main
function is reabsorption of the filtered glucose from the urine back into the
circulation. It is responsible for about 90% of total glucose reabsorption.
Inhibition of this protein leads to the excretion of the glucose in the urine
at much lower blood glucose level than normal. The most common side
effects of SGLT-inhibitors are vaginal yeast infections and urinary tract
infections. The greatest risk is seen in female patients and those men who
are uncircumcised. Polyuria is also seen.
You might also like
- Responsorial PsalmDocument1 pageResponsorial PsalmMaine AsuncionNo ratings yet
- PCAPDocument2 pagesPCAPMaine AsuncionNo ratings yet
- Vitamin D Deficiency Associated With Increased Incidence ofDocument8 pagesVitamin D Deficiency Associated With Increased Incidence ofMaine AsuncionNo ratings yet
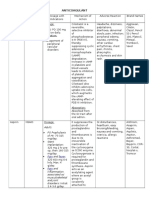
- Febuxostat: Drug Index Abela, Lorenzo 57M Drug Class Dose Mechanism of Action Wof/AdrDocument2 pagesFebuxostat: Drug Index Abela, Lorenzo 57M Drug Class Dose Mechanism of Action Wof/AdrMaine AsuncionNo ratings yet
- Ganong's Physiology Chapter 1-2 ReviewDocument2 pagesGanong's Physiology Chapter 1-2 ReviewMaine AsuncionNo ratings yet
- AnalgesicsDocument13 pagesAnalgesicsMaine Asuncion100% (1)
- Sing A New Song Responsorial Psalm Take and Receive Prayers For The Faithful The Lord'S Prayer Anima Christi One More GiftDocument1 pageSing A New Song Responsorial Psalm Take and Receive Prayers For The Faithful The Lord'S Prayer Anima Christi One More GiftMaine AsuncionNo ratings yet
- Oxaciline PDFDocument7 pagesOxaciline PDFamatoryfictionliteraNo ratings yet
- Febuxostat: Drug Index Abela, Lorenzo 57M Drug Class Dose Mechanism of Action Wof/AdrDocument2 pagesFebuxostat: Drug Index Abela, Lorenzo 57M Drug Class Dose Mechanism of Action Wof/AdrMaine AsuncionNo ratings yet
- Case 1 Pharma MdtermsDocument3 pagesCase 1 Pharma MdtermsMaine AsuncionNo ratings yet
- Saint Louis University - Hospital of The Sacred Heart Department of PediatricsDocument3 pagesSaint Louis University - Hospital of The Sacred Heart Department of PediatricsMaine AsuncionNo ratings yet
- AnticoagulantDocument15 pagesAnticoagulantMaine AsuncionNo ratings yet
- Normal Arterial Blood Gas ValuesDocument1 pageNormal Arterial Blood Gas ValuesMaine AsuncionNo ratings yet
- 543fe1010cf21227a11b97c2 PDFDocument30 pages543fe1010cf21227a11b97c2 PDFMaine AsuncionNo ratings yet
- 3 - Medicine 1 - Clinical Reasoning, Assessment, and Recording - Dr. Dominguez - August 18, 2014Document2 pages3 - Medicine 1 - Clinical Reasoning, Assessment, and Recording - Dr. Dominguez - August 18, 2014Maine AsuncionNo ratings yet
- Normal Arterial Blood Gas ValuesDocument1 pageNormal Arterial Blood Gas ValuesMaine AsuncionNo ratings yet
- Research EthicsDocument7 pagesResearch EthicsMaine AsuncionNo ratings yet
- Here Are The Steps of Maglalatik DanceDocument1 pageHere Are The Steps of Maglalatik DanceMaine AsuncionNo ratings yet
- Anatomy - Aug 14, 2013 - Dr. AbiogDocument4 pagesAnatomy - Aug 14, 2013 - Dr. AbiogMaine AsuncionNo ratings yet
- Varying Definitions of Online Communication ResearchDocument11 pagesVarying Definitions of Online Communication ResearchCalvin WirawanNo ratings yet
- Abg 2Document6 pagesAbg 2Maine AsuncionNo ratings yet
- Normal Arterial Blood Gas ValuesDocument1 pageNormal Arterial Blood Gas ValuesMaine AsuncionNo ratings yet
- Abg 2Document6 pagesAbg 2Maine AsuncionNo ratings yet
- Abg 2Document6 pagesAbg 2Maine AsuncionNo ratings yet
- Abg 2Document6 pagesAbg 2Maine AsuncionNo ratings yet
- Abg 2Document6 pagesAbg 2Maine AsuncionNo ratings yet
- Color Match Catyeri NGDocument1 pageColor Match Catyeri NGMaine AsuncionNo ratings yet
- Abg 2Document6 pagesAbg 2Maine AsuncionNo ratings yet
- Color Match Catyeri NGDocument1 pageColor Match Catyeri NGMaine AsuncionNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Prova CristinaDocument3 pagesProva CristinaRafael BatalhaNo ratings yet
- Electric Eels Use High-Voltage To Track Fast-MovinDocument6 pagesElectric Eels Use High-Voltage To Track Fast-MovinTatsumaki TornadoNo ratings yet
- Textbook of Veterinary Internal Medicine, 8th Edition-4693-4728 (1) - 1-18Document19 pagesTextbook of Veterinary Internal Medicine, 8th Edition-4693-4728 (1) - 1-18Kevin Andres Trujillo CastroNo ratings yet
- The Naming of The Cranial Nerves - A Historical ReviewDocument7 pagesThe Naming of The Cranial Nerves - A Historical ReviewAfnan SefffNo ratings yet
- Vietnamese Phonemic InventoryDocument2 pagesVietnamese Phonemic InventoryfroseboomNo ratings yet
- Modulation of Calmodulin Plasticity by The Effect of Macromolecular CrowdingDocument11 pagesModulation of Calmodulin Plasticity by The Effect of Macromolecular Crowdingsmileman_csNo ratings yet
- South African National Science Olympiad - Biology (2015) PDFDocument13 pagesSouth African National Science Olympiad - Biology (2015) PDFElevenPlus ParentsNo ratings yet
- Muscles, Cheat SheetDocument9 pagesMuscles, Cheat SheetIvan SkoricNo ratings yet
- 298830Document34 pages298830Mohamed belhasan100% (1)
- Benign Prostatic Hyperplasia (BPH)Document43 pagesBenign Prostatic Hyperplasia (BPH)dana3rfts100% (1)
- Pharmacology Lecture - 20 Antianginal DrugsDocument3 pagesPharmacology Lecture - 20 Antianginal DrugsChris QueiklinNo ratings yet
- Reflex ExercisesDocument43 pagesReflex ExercisesFlori100% (4)
- Isc Biology Class Xi DiagramsDocument2 pagesIsc Biology Class Xi DiagramsAbhimanyu SinhaNo ratings yet
- Brownies RecipeDocument2 pagesBrownies RecipeMrTakbaNo ratings yet
- Alzheimer's Disease and Memory Drugs PDFDocument97 pagesAlzheimer's Disease and Memory Drugs PDFbradbaderNo ratings yet
- Grade 10 12 Biology Revision Notes Transport in Plants and AnimalsDocument33 pagesGrade 10 12 Biology Revision Notes Transport in Plants and AnimalsMapalo ChirwaNo ratings yet
- TCM PDFDocument435 pagesTCM PDFalintuta2No ratings yet
- Asthma DiaryDocument3 pagesAsthma Diarybrian@coombsmd.comNo ratings yet
- Article Review MICR7002 FinalDocument8 pagesArticle Review MICR7002 FinalMiranda KeikuNo ratings yet
- QuestionDocument16 pagesQuestionellis garciaNo ratings yet
- Set1 - Final FRCA Viva Qs - June 2009 PDFDocument25 pagesSet1 - Final FRCA Viva Qs - June 2009 PDFAdham SalemNo ratings yet
- BiochemistryDocument38 pagesBiochemistryPrachiSinghNo ratings yet
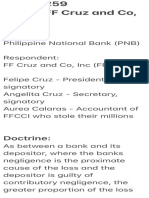
- GR 173259Document11 pagesGR 173259Anonymous wDganZNo ratings yet
- The Menstrual Cycle PDFDocument6 pagesThe Menstrual Cycle PDFPerry Sin100% (1)
- Biology Grade 11 Mock Exam Paper 1Document7 pagesBiology Grade 11 Mock Exam Paper 1Nicketa AndersonNo ratings yet
- Diseases and Immunity: Defence Against MicrobesDocument55 pagesDiseases and Immunity: Defence Against MicrobesIvan Prasetya100% (1)
- Santa Monica: Monday Tuesday Wednesday Thursday Friday Saturday SundayDocument2 pagesSanta Monica: Monday Tuesday Wednesday Thursday Friday Saturday SundayStephanie ThomasNo ratings yet
- Microbial GeneticsDocument14 pagesMicrobial GeneticshengkitanjungNo ratings yet
- Adcon FinalDocument63 pagesAdcon FinalHazel Mae SagorsorNo ratings yet
- ResearchDocument3 pagesResearchapi-380517264No ratings yet