Professional Documents
Culture Documents
Shah Et Al - Lam
Uploaded by
abob619Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Shah Et Al - Lam
Uploaded by
abob619Copyright:
Available Formats
JOURNAL OF CLINICAL MICROBIOLOGY, Aug. 2010, p.
29722974
0095-1137/10/$12.00 doi:10.1128/JCM.00363-10
Copyright 2010, American Society for Microbiology. All Rights Reserved.
Vol. 48, No. 8
Quantitative Analysis of a Urine-Based Assay for Detection of
Lipoarabinomannan in Patients with Tuberculosis
Maunank Shah,1 Neil A. Martinson,1,2 Richard E. Chaisson,1 Desmond J. Martin,3
Ebrahim Variava,4 and Susan E. Dorman1*
Johns Hopkins University School of Medicine, Baltimore, Maryland1; Perinatal HIV Research Unit, University of the Witwatersrand,
Soweto, South Africa2; Toga Laboratories, Johannesburg, South Africa, and Department of Medical Virology, University of
Pretoria, South Africa3; and Tshepong Hospital, Northwest Department of Health, Klerksdorp, South Africa4
Received 22 February 2010/Returned for modification 18 May 2010/Accepted 2 June 2010
Urinary lipoarabinomannan (LAM) detection is a promising approach for rapid diagnosis of active tuberculosis (TB). In microbiologically confirmed TB patients, quantitative LAM detection results increased progressively with bacillary burden and immunosuppression. Patients with disseminated TB and/or advanced HIV
are target populations for whom urine LAM detection may be particularly useful.
cohort study at three hospitals in South Africa to evaluate the
diagnostic accuracy of the urine LAM test. Hospitalized adult
TB suspects were enrolled after informed consent. Study-directed testing included sputum smear microscopy for acid-fast
bacilli (AFB), sputum mycobacterial culture, mycobacterial
blood cultures, HIV and CD4 testing, urine LAM testing using
the Clearview TB ELISA kit, and additional mycobacterial
cultures (e.g., from enlarged lymph nodes) when clinically indicated. Participants had a follow-up study visit at 2 months.
Participants with at least one positive AFB smear or mycobacterial culture positive for Mycobacterium tuberculosis were determined to have confirmed TB and were included in the
current analysis. Individuals with M. tuberculosis isolated from
a blood culture (mycobacteremia) were considered to have
disseminated disease. Pulmonary TB (PTB) was defined as the
presence of one or more sputa positive for AFB by microscopy
and/or positive for M. tuberculosis by culture. Localized extrapulmonary TB was defined as isolation of M. tuberculosis
from pleural culture or fine-needle aspiration of a lymph node
but not from other respiratory specimens or blood. Quantitative urine LAM test results were expressed as optical density
(OD) readings. The final sample OD was determined by subtracting the OD of the negative control from the sample reading, with a minimum value of 0 (i.e., a value of 0 was reported
if the OD of the negative control was greater than the OD of
the sample). An OD above 0.1 was considered positive per
manufacturer specifications. Multiple linear regression models
were used to determine predictors of higher quantitative urine
LAM test results. Wilcoxon rank sum and Kruskal-Wallis tests
were used to compare nonnormal continuous outcomes; chisquare (2) tests were used to compare categorical outcomes.
A P value of 0.05 was considered statistically significant, and
95% confidence intervals (95% CI) were used. Statistical calculations were performed using Stata 10.1 (StataCorp). This
study was approved by the institutional review boards of Johns
Hopkins University School of Medicine and the University of
Witwatersrand.
Full characteristics of the study population are published
elsewhere (16). Overall, 499 participants were enrolled, and
193 (39%) had confirmed TB (185 with positive cultures for M.
Effective control of tuberculosis (TB) is hindered by the lack
of rapid, accurate diagnostic modalities. Current tools have
serious limitations when applied to HIV-infected patients, and
clinical diagnosis can be challenging (2, 6, 8, 13). Sputum
smear microscopy is widely utilized to diagnose active TB but
has impaired sensitivity and detects less than half of HIV-TB
coinfection cases (2, 6, 8). Mycobacterial culture is the laboratory standard for diagnosis but is not widely available in
resource-constrained settings and can take weeks to determine
a positive result.
The detection of lipoarabinomannan (LAM), a 17.5-kDa
glycolipid component of the mycobacterial cell wall, is an attractive approach to diagnosing active TB (1, 7, 9, 15, 16).
LAM is released from metabolically active mycobacteria and is
detectable intact in urine (1, 7). The Clearview TB enzymelinked immunosorbent assay (ELISA) (urine LAM test; Inverness Medical Innovations, Waltham, MA) is a direct antigen sandwich immunoassay in a 96-well-plate format that
provides both quantitative and qualitative results. Our group
and others have recently reported on the qualitative diagnostic
accuracy of this urine LAM test (9, 10, 16). Urine LAM test
sensitivity, while imperfect, appears to be higher than that of
sputum smear microscopy, and the test performs with a high
positive predictive value in populations with high HIV and TB
prevalence (9, 12, 16). However, quantitative urine LAM test
results have not been studied fully. Quantitative analysis allows
a more complete understanding of test performance and may
offer insight into optimal test usage. Preclinical data and limited regression modeling from clinical studies have shown that
quantitative test results positively correlate with increasing bacillary burden (1, 16). We therefore examined the relationship
between quantitative urine LAM test results and TB characteristics among patients with culture-confirmed TB.
A full description of the study design has been published
previously (16). Briefly, we conducted a nested prospective
* Corresponding author. Mailing address: Johns Hopkins University
Center for Tuberculosis Research, CRB2, Room 1M-12, 1550 Orleans
Street, Baltimore, MD 21231. Phone: (410) 502-2717. Fax: (410) 9550740. E-mail: dsusan1@jhmi.edu.
Published ahead of print on 9 June 2010.
2972
VOL. 48, 2010
NOTES
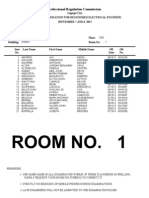
TABLE 1. Optical density by type of disease (determined by site)
among participants with confirmed TB
Type of disease (no. of
cases)
OD median
(IQR)
OD mean
(SD)
No. of cases with
positive urine
LAM test result
(% sensitivity,
95% CI)
Localized extrapulmonary
TB (5)a
Pulmonary TB only (145)b
Mycobacteremia only (18)c
Pulmonary TB with
mycobacteremia (25)
P value
0.01 (0.010.06)
0.09 (0.16)
1 (20, 172)
0.13 (0.020.70)
0.64 (0.141.43)
1.4 (0.432.8)
0.63 (0.97)
0.99 (1.02)
1.6 (1.1)
78 (54, 4562)
14 (78, 5294)
21 (84, 6496)
0.0001d
0.003f
Four of five participants had M. tuberculosis isolated from pleural cultures,
and 1 of 5 had M. tuberculosis isolated from a lymph node. The urine LAM test
was positive in the participant with M. tuberculosis isolated from the lymph node
but negative in the 4 participants with localized pleural TB.
b
M. tuberculosis in sputum but not blood.
c
M. tuberculosis in blood but not sputum.
d
Kruskal-Wallis test of equality between types of disease.
e
, analysis of variance (ANOVA) was not performed, due to nonnormal
distribution.
f
Chi-square (2) test comparing proportions of positive urine LAM test results
(sensitivities) between types of disease.
tuberculosis and 8 with positive AFB smears only); 6/193 (3%)
confirmed TB cases were on recent TB treatment (less than 2
months) at time of enrollment. Among the confirmed TB
cases, the median age was 34 years, 65% were female, and 87%
(167/193) had documented HIV infection, of which 9% (15/
167) were on antiretroviral therapy (ART) at the time of enrollment. TB manifestations ranged from localized to disseminated disease (Table 1). Localized extrapulmonary TB was
diagnosed in 5 cases (3%), PTB without mycobacteremia (M.
tuberculosis in sputum but not blood) in 145 cases (75%),
mycobacteremia without PTB (M. tuberculosis in blood but not
sputum) in 18 cases (9%), and combined PTB with mycobacteremia (M. tuberculosis in blood and sputum) in 25 cases
(13%). The overall LAM test sensitivity was 59% (95% CI, 52
to 66) in participants with confirmed TB, and the specificity
was 96% (95% CI, 91 to 99) among individuals without TB.
Among participants with confirmed TB, the range of quantitative LAM test results was 0 to 4.87 (median, 0.19; interquartile range [IQR], 0.03 to 1.3).
Among participants with confirmed TB, there was a significant difference in median OD for those with more localized
disease compared to those with disseminated disease (P
0.0001) (Table 1). The median OD increased progressively
from 0.01 (IQR, 0.01 to 0.06) to 0.13 (IQR, 0.02 to 0.70) to 0.64
(IQR, 0.14 to 1.43) to 1.4 (IQR, 0.43 to 2.8) in those with
localized extrapulmonary TB, PTB alone, mycobacteremia
without PTB, and combined PTB with mycobacteremia, respectively. Among 161 participants with sputum culture-positive PTB, those that were AFB smear positive had higher ODs
than those that were smear negative (median ODs of 0.33
versus 0.13, respectively; P 0.03) (Table 2). There was a
trend toward higher OD with increasing grades of smear positivity (median ODs of 0.13 [IQR, 0.02 to 0.62], 0.18 [IQR, 0.1
to 1.3], 0.26 [IQR, 0.03 to 2.8], and 0.38 [IQR, 0.048 to 1.8] for
smear-negative, smear-positive grade 1, smear-positive grade
2, and smear-positive grade 3 cases, respectively; P 0.18).
Among confirmed TB patients with HIV infection, the urine
LAM test OD increased with decreasing strata of CD4 count
2973
TABLE 2. Optical density by sputum AFB smear microscopy status
among participants with sputum culture-positive pulmonary TB
OD median
(IQR)
OD mean
(SD)
No. of cases with
positive urine
LAM test result
(% sensitivity,
95% CI)
Negative (88)
0.13 (0.020.62)a,b
0.60 (0.93)
47 (53, 0.420.64)
Positive
Any grade (73)
Grade 1 (13)
Grade 2 (15)
Grade 3 (45)
0.33 (0.0521.71)b
0.18 (0.11.3)a
0.26 (0.032.8)a
0.38 (0.0481.8)a
0.94 (1.15)
0.68 (0.89)
1.13 (1.3)
0.95 (1.18)
47 (64, 0.520.75)
10 (77, 0.460.94)
10 (67, 0.380.88)
27 (60, 0.440.74)
Sputum AFB
smear microscopy
status (no. of
cases)c
a
P 0.18 for comparison of AFB-negative, AFB 1, AFB 2, and AFB 3
results by the Kruskal-Wallis test.
b
P 0.03 for comparison of AFB-negative and AFB-positive results by the
Wilcoxon rank sum test.
c
Grading per WHO guidelines (http://wwwn.cdc.gov/dls/ila/documents/lstc2
.pdf).
(P 0.0001) (Table 3). The median OD increased progressively from 0.10 (IQR, 0.02 to 0.5) to 0.20 (IQR, 0.03 to 0.8) to
0.42 (IQR, 0.04 to 1.0) to 1.3 (IQR, 0.2 to 2.8) in those with
CD4 counts of 150, 101 to 150, 50 to 100, and 50, respectively (P 0.0001).
Multiple linear regression models were used to further explore factors associated with higher quantitative urine LAM
test results. Covariates included in the models were age, sex,
HIV status, mortality at 2 months, TB treatment, mycobacteremia, sputum smear positivity, fever, Karnofsky score, chest X
ray (CXR) cavitation, hypoxia, pulse, and CD4 strata. Adjusting for all other factors, individuals with mycobacteremia had
an average OD that was 0.64 OD units higher than that for
individuals with negative blood cultures (P 0.002); individuals with smear-positive pulmonary TB had an average OD
that was 0.33 OD units higher than that for individuals with
smear-negative pulmonary TB (P 0.05). Among HIV-infected patients, individuals with CD4 counts of 50 had an
average OD that was 1.05 OD units higher than that for individuals with CD4 counts of 150 (P 0.0001). No other
covariates were significantly associated with higher quantitative urine LAM test results.
Taken together, our findings show that quantitative urine
LAM test results correlate with degree of bacillary burden in
patients with microbiologically confirmed TB. Further, the absolute urine LAM test OD increased dramatically as immuno-
TABLE 3. Optical density by CD4 status among participants with
HIV infection and confirmed TB
CD4 count
(no. of cases)
OD median
(IQR)
OD mean
(SD)
No. of cases with
positive urine LAM
test results (%
sensitivity, 95% CI)
150 (63)
101150 (16)
50100 (28)
50 (60)
P value
0.10 (0.020.5)
0.2 (0.030.8)
0.42 (0.041.0)
1.3 (0.22.8)
0.0001a
0.42 (0.72)
0.65 (0.96)
0.72 (0.9)
1.4 (1.12)
b
32 (51, 0.380.64)
9 (56, 0.300.80)
20 (71, 0.510.87)
51 (85, 0.730.93)
0.00c
Kruskal-Wallis test of equality between CD4 strata.
, ANOVA was not performed, due to nonnormal distribution.
Chi-square (2) test comparing proportions of positive urine LAM test results (sensitivities) between CD4 strata.
b
c
2974
NOTES
J. CLIN. MICROBIOL.
suppression progressed among HIV-coinfected TB patients,
probably due to higher mycobacterial burden and greater likelihood of disseminated TB. Strikingly, the median quantitative
urine LAM test result was over 10-fold higher than the current
threshold for test positivity in those with CD4 counts less than
50 and 5-fold higher than this threshold in those with CD4
counts between 51 and 100. Usage of quantitative urine LAM
test results may thus offer additional clinical insight into the
degree of TB disease severity that cannot be gleaned from
qualitative results alone.
To date, studies of the qualitative accuracy of the urine
LAM test have yielded varied results. In heterogeneous populations with low HIV prevalence, the sensitivity has ranged
from 13 to 51% (3, 4, 10, 12, 14). Alternatively, sensitivity rises
among HIV-positive patients and could reach 67 to 85% in
those with low CD4 counts (9, 16). This quantitative analysis
provides evidence that urine LAM test performance may be
best in patients with disseminated TB disease and high mycobacterial disease burden. HIV-infected TB suspects with advanced immunosuppression, a group in which sputum microscopy is of low yield (5, 8, 11, 17), may be a target population for
whom the urine LAM test would be particularly useful. Of
note, the combination of LAM testing and sputum smear microscopy may have an additive benefit in this target group (16).
While the urine LAM test is unlikely to stand alone for definitive TB diagnostic testing, its usage is attractive as a rapid
diagnostic modality that complements smear microscopy for
HIV-prevalent, resource-constrained settings where mycobacterial culture is unavailable.
This work was funded in part by the Doris Duke Charitable
Foundation and the United Kingdom Government through a grant
from the Department for International Development (DFID). Additional support was provided by NIH grants AI48526, AI01637,
and T32AI007291-18.
Clearview TB ELISA kits were generously provided by Inverness
Medical Innovations, which had no role in the study design, implementation, or analysis, the manuscript writing, or the decision to submit a manuscript for publication.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
REFERENCES
1. Boehme, C., E. Molokova, F. Minja, S. Geis, T. Loscher, L. Maboko, V.
Koulchin, and M. Hoelscher. 2005. Detection of mycobacterial lipoarabinomannan with an antigen-capture ELISA in unprocessed urine of Tanzanian
17.
patients with suspected tuberculosis. Trans. R. Soc. Trop. Med. Hyg. 99:893
900.
Colebunders, R., and I. Bastian. 2000. A review of the diagnosis and treatment of smear-negative pulmonary tuberculosis. Int. J. Tuberc. Lung Dis.
4:97.
Daley, P., J. S. Michael, P. Hmar, A. Latha, P. Chordia, D. Mathai, K. R.
John, and M. Pai. 2009. Blinded evaluation of commercial urinary lipoarabinomannan for active tuberculosis: a pilot study. Int. J. Tuberc. Lung Dis.
13:989995.
Dheda, K., V. Davids, L. Lenders, T. Roberts, R. Meldau, D. Ling, L. Brunet,
R. van Zyl Smit, J. Peter, C. Green, M. Badri, L. Sechi, S. Sharma, M.
Hoelscher, R. Dawson, A. Whitelaw, J. Blackburn, M. Pai, and A. Zumla.
2010. Clinical utility of a commercial LAM-ELISA assay for TB diagnosis in
HIV-infected patients using urine and sputum samples. PLoS One 5:e9848.
El-Sadr, W. M., and S. J. Tsiouris. 2008. HIV-associated tuberculosis: diagnostic and treatment challenges. Semin. Respir. Crit. Care Med. 29:525531.
Getahun, H., M. Harrington, R. OBrien, and P. Nunn. 2007. Diagnosis of
smear-negative pulmonary tuberculosis in people with HIV infection or
AIDS in resource-constrained settings: informing urgent policy changes.
Lancet 369:2042.
Hamasur, B., J. Bruchfeld, M. Haile, A. Pawlowski, B. Bjorvatn, G. Kallenius, and S. B. Svenson. 2001. Rapid diagnosis of tuberculosis by detection
of mycobacterial lipoarabinomannan in urine. J. Microbiol. Methods 45:
4152.
Havlir, D. V., H. Getahun, I. Sanne, and P. Nunn. 2008. Opportunities and
challenges for HIV care in overlapping HIV and TB epidemics. JAMA
300:423.
Lawn, S. D., D. J. Edwards, K. Kranzer, M. Vogt, L. G. Bekker, and R. Wood.
2009. Urine lipoarabinomannan assay for tuberculosis screening before antiretroviral therapy diagnostic yield and association with immune reconstitution disease. AIDS 23:18751880.
Mutetwa, R., C. Boehme, M. Dimairo, T. Bandason, S. S. Munyati, D.
Mangwanya, S. Mungofa, A. E. Butterworth, P. R. Mason, and E. L. Corbett.
2009. Diagnostic accuracy of commercial urinary lipoarabinomannan detection in African tuberculosis suspects and patients. Int. J. Tuberc. Lung Dis.
13:12531259.
Perkins, M. D., and J. Cunningham. 2007. Facing the crisis: improving the
diagnosis of tuberculosis in the HIV era. J. Infect. Dis. 196(Suppl. 1):S15.
Peter, J., C. Green, M. Hoelscher, P. Mwaba, A. Zumla, and K. Dheda. 2010.
Urine for the diagnosis of tuberculosis: current approaches, clinical applicability, and new developments. Curr. Opin. Pulm. Med. 16:262270.
Reid, M. J., and N. S. Shah. 2009. Approaches to tuberculosis screening and
diagnosis in people with HIV in resource-limited settings. Lancet Infect. Dis.
9:173.
Reither, K., E. Saathoff, J. Jung, L. T. Minja, I. Kroidl, E. Saad, J. F.
Huggett, E. N. Ntinginya, L. Maganga, L. Maboko, and M. Hoelscher. 2009.
Low sensitivity of a urine LAM-ELISA in the diagnosis of pulmonary tuberculosis. BMC Infect. Dis. 9:141.
Sada, E., D. Aguilar, M. Torres, and T. Herrera. 1992. Detection of lipoarabinomannan as a diagnostic test for tuberculosis. J. Clin. Microbiol.
30:24152418.
Shah, M., E. Variava, C. B. Holmes, A. Coppin, J. E. Golub, J. McCallum,
M. Wong, B. Luke, D. J. Martin, R. E. Chaisson, S. E. Dorman, and N. A.
Martinson. 2009. Diagnostic accuracy of a urine lipoarabinomannan test for
tuberculosis in hospitalized patients in a high HIV prevalence setting. J.
Acquir. Immune Defic. Syndr. 52:145151.
Swaminathan, S., C. Padmapriyadarsini, and G. Narendran. 2010. HIVassociated tuberculosis: clinical update. Clin. Infect. Dis. 50:13771386.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pharmaceutical Sciences: Pharmacy PrepDocument238 pagesPharmaceutical Sciences: Pharmacy Prepabob619100% (1)
- BFD-180-570 DN65 GBDocument25 pagesBFD-180-570 DN65 GBalexander100% (3)
- BROCHURE Training Specialist On Medication Therapy Management April 2018Document2 pagesBROCHURE Training Specialist On Medication Therapy Management April 2018abob619No ratings yet
- Dialectical Behavior Therapy Webinar SlidesDocument49 pagesDialectical Behavior Therapy Webinar SlidesJanelle100% (1)
- Reference No. 072619Document2 pagesReference No. 072619abob619No ratings yet
- Key Drugs Mnemonics Study Tips Pebc Osce ResourcesDocument18 pagesKey Drugs Mnemonics Study Tips Pebc Osce Resourcesvishpinder sharma100% (1)
- Pharmacist Evaluating Examination Syllabus: The Pharmacy Examining Board of CanadaDocument74 pagesPharmacist Evaluating Examination Syllabus: The Pharmacy Examining Board of CanadapppNo ratings yet
- Tatay TagDocument2 pagesTatay Tagabob619No ratings yet
- LAM by AckharDocument12 pagesLAM by Ackharabob619No ratings yet
- Overview of Moral SituationDocument32 pagesOverview of Moral SituationMyzhel InumerableNo ratings yet
- LAM During TreatmentDocument11 pagesLAM During Treatmentabob619No ratings yet
- Results ULAMDocument9 pagesResults ULAMabob619No ratings yet
- LAM by AGHADocument7 pagesLAM by AGHAabob619No ratings yet
- LAM by LAWNDocument9 pagesLAM by LAWNabob619No ratings yet
- 06 Brakes PDFDocument6 pages06 Brakes PDFAKILI PSINo ratings yet
- Atg SPRL 01 PDFDocument25 pagesAtg SPRL 01 PDFMuhammad Faiez AfzaalNo ratings yet
- 24 - Al Nahda The Sheffeild Privat To International City, Greece K12 Dubai Bus Service TimetableDocument10 pages24 - Al Nahda The Sheffeild Privat To International City, Greece K12 Dubai Bus Service TimetableDubai Q&ANo ratings yet
- DuranDuran OrdinaryWorldDocument1 pageDuranDuran OrdinaryWorldEduardo LuzNo ratings yet
- Atcmorse PDFDocument50 pagesAtcmorse PDFdivyansh bansalNo ratings yet
- ED1021 - I/O Expander With UART Interface & Analog Inputs: PreliminaryDocument9 pagesED1021 - I/O Expander With UART Interface & Analog Inputs: PreliminaryMilan NovakovićNo ratings yet
- Atomic Rex A Kaiju Thriller (Matthew Dennion) (Z-Library)Document163 pagesAtomic Rex A Kaiju Thriller (Matthew Dennion) (Z-Library)Strictly Aviator Amritansh VermaNo ratings yet
- Safety Data Sheet: 1. IdentificationDocument7 pagesSafety Data Sheet: 1. IdentificationKhobeb MuslimNo ratings yet
- Trane 5 Ton HP Cond submittat4TWB3060-SUB-106 - 05.05 - 11012009Document2 pagesTrane 5 Ton HP Cond submittat4TWB3060-SUB-106 - 05.05 - 11012009nobleairNo ratings yet
- Mass, Weigth and Density IGCSEDocument6 pagesMass, Weigth and Density IGCSEsapiniNo ratings yet
- Woodcock 1987Document37 pagesWoodcock 1987Rodrigo MachadoNo ratings yet
- REE0913ra LegazpiDocument6 pagesREE0913ra LegazpiScoopBoyNo ratings yet
- Serial Interface RS485 (RS422) Configuration InstructionsDocument20 pagesSerial Interface RS485 (RS422) Configuration Instructionsyana sopian hidayatNo ratings yet
- 1.8 CarderoDocument29 pages1.8 CarderoRodrigo Flores MdzNo ratings yet
- A Report On External Analysis of Construction in NepalDocument13 pagesA Report On External Analysis of Construction in Nepalsubash upretiNo ratings yet
- Figure Eight Island Homeowners' Association, Inc. Case StudyDocument16 pagesFigure Eight Island Homeowners' Association, Inc. Case StudyYoong YingNo ratings yet
- Documentation ExamplesDocument5 pagesDocumentation ExamplesErika HarveryNo ratings yet
- I-R Nirvana IRN250-300H-2S Parts ManualDocument28 pagesI-R Nirvana IRN250-300H-2S Parts ManualMistysParts100% (4)
- Bruker d8 XRD TutoriallDocument16 pagesBruker d8 XRD TutoriallravarNo ratings yet
- Description Features: PT6964 LED Driver ICDocument15 pagesDescription Features: PT6964 LED Driver ICDhivya NNo ratings yet
- Hebrew and TamilDocument98 pagesHebrew and TamilSreshta JustinNo ratings yet
- Rajesh CVDocument3 pagesRajesh CVS R PramodNo ratings yet
- 4864.21 - Optics System 2Document39 pages4864.21 - Optics System 2Edgar Jose Aponte MartinezNo ratings yet
- Chapter 11Document10 pagesChapter 11NungkiwidyasNo ratings yet
- 2 2 1 A Productanalysis 2Document5 pages2 2 1 A Productanalysis 2api-308131962No ratings yet
- 21 Day Fasting & Prayer 2022Document29 pages21 Day Fasting & Prayer 2022StephenNo ratings yet
- Ancient CivilizationsDocument9 pagesAncient CivilizationsMarienne LaoNo ratings yet
- Installation Instructions: Harley-Davidson Softail Saddlebag Mount Bracket PART# 21946Document4 pagesInstallation Instructions: Harley-Davidson Softail Saddlebag Mount Bracket PART# 21946Justin StewartNo ratings yet
- HINO Dutro Fault Codes List PDFDocument4 pagesHINO Dutro Fault Codes List PDFANH LÊNo ratings yet