Professional Documents
Culture Documents
Soberhea Dermatis
Uploaded by
Risma PertiwiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Soberhea Dermatis
Uploaded by
Risma PertiwiCopyright:
Available Formats
ASIAN PACIFIC JOURNAL OF ALLERGY AND IMMUNOLOGY (2005) 23: 101-105
Malassezia furfur in Infantile Seborrheic
Dermatitis
Siriwan Wananukul1, Ariya Chindamporn2, Poomjit Yumyourn2, Sunchai Payungporn3,
Chanchuree Samathi1 and Yong Poovorawan3
SUMMARY Our objective was to study both incidence and various strains of Malassezia in infantile seborrheic
dermatitis (ISD). Sixty infants between 2 weeks and 2 years old with clinical diagnosis of ISD at the Department of
Pediatrics, King Chulalongkorn Memorial Hospital from May 2002 to April 2003 were recruited. Malassezia spp.
were isolated from cultured skin samples of the patients, genomic DNA was extracted and the ITS1 rDNA region
was amplified. The PCR product was examined by agarose gel electrophoresis and DNA sequences were determined. The ITS1 sequences were also subjected to phylogenetic analysis and species identification. ISD is most
commonly found in infants below the age of 2 months (64%), followed by those between 2 and 4 months (28%) old.
Cultures yielded yeast-like colonies in 15 specimens. PCR yielded 200-bp products (Candida) in 3 patients and
300-bp products (Malassezia furfur) in 12 patients (18%). Sugar fermentation using API 20C aux performed on the
three 200-bp PCR products yielded Candida species. M. furfur was the only Malassezia recovered from skin scrapings
of children with ISD.
Various studies have been performed on the
role of Malassezia and seborrheic dermatitis in infants and adults.1-6 Malassezia is found in many skin
diseases such as psoriasis, atopic dermatitis, tinea
versicolor, pityrosorum folliculitis as well as in
healthy infants.6,7 Malassezia species may be associated with catheteracquired sepsis, fungemia and
pulmonary infection in neonates8-12 and also in cancer patients.13-14
The genus Malassezia can now be divided
into seven species.15 Cell-mediated immunity to M.
furfur has been shown to be different in patients with
seborrheic dermatitis and pityriasis versicolor.16
Malassezia can induce cytokine production by
keratinocytes17,18 with differences in this ability
among the various Malassezia yeasts.19 Six different
species of Malassezia were recovered from different
dermatosis cases and different anatomical sites.20
The objective of this study was to investigate
both incidence and species of Malassezia in infantile
seborrheic dermatitis (ISD) based on the internal
transcribed spacer 1 region (ITS1) of the ribosomal
DNA (rDNA) sequence. ITS1 is located between
18S and 5.8S rDNA and has proven useful for species identification and strain typing of Malassezia
spp.19
1
From the Department of Pediatrics, Department of Microbiology
3
and Viral Hepatitis Research Unit, Faculty of Medicine, Chulalongkorn University, Bangkok, 10330 Thailand
Correspondence: Yong Poovorawan
E-mail address: Yong.P@chula.ac.th
102
WANANUKUL, ET AL.
MATERIALS AND METHODS
Study population
All infants diagnosed with ISD without prior
treatment, aged between 2 weeks and 24 months
were recruited into this study between May 2002 and
April 2003. The study protocol was approved by the
Ethics Committee of the Faculty of Medicine, Chulalongkorn University. Parents were informed regarding the objective of the study and their written
consents were obtained before specimen collection.
Malassezia isolation and DNA extraction
We scraped ISD skin lesions for scaling and
subsequently adhered slides coated with Saboraud
dextrose agar (SDA) as transport medium to the skin
lesions.
The transport medium was transferred to
SDA overlaid with olive oil and incubated at room
temperature for 4 weeks. DNA was extracted from a
fraction of a colony suspended in 100 l lysis buffer
(200mM Tris-HCl, pH 8.0; SDS 0.5% w/v, 250 mM
NaCl, 25 mM EDTA). After mixing by vortex for 5
seconds, the sample was incubated at 100C for 15
minutes. Then 100 l of 3.0 M sodium acetate were
added, mixed, incubated at -20C for 10 minutes and
centrifuged at 6,060 x g for 5 minutes. The supernatant was extracted once with phenol:chloroform:
isoamyl alcohol (25:24:1, v:v:v) and once more with
chloroform. DNA was precipitated in 40 l 3.0 M
sodium acetate, 4 l glycogen and 800 l absolute
ethanol at -70C for 30 minutes. The resulting DNA
pellet was washed in 1 ml 70% ethanol and centrifuged at 13,700 x g for 15 minutes. Finally, the pellet
was dried and resuspended in 50 l sterile water.
Amplification of ITS1
The ITS1 region was amplified in a Mastercycler personal (Eppendorf, Hamburg, Germany)
using the primer sequences previously described.18
The forward primer was 18SF1: 5-AGGTTTCCGTAGGTGAACCT-3; and the reverse primer was
58SR1: 5-TTCGCTGCGTTCTTCATCGA-3. Each
PCR reaction mixture contained 2.5 l 10x reaction
buffer (Finnzymes, Finland), 10.0 M each of dATP,
dCTP, dGTP and dTTP (Promega, Madison, WI),
2.5 U Taq polymerase (Finnzymes, Finland), 0.5 M
of each primer and 1.0 l DNA template solution.
PCR was performed under the following conditions:
after an initial 5-minute denaturation step at 94C,
35 cycles of amplification were performed, each including 1 minute denaturation at 94C, 15 seconds
annealing at 60C and 30 seconds extension at 72C,
followed by a final 10-minute extension at 72C.
Each amplified DNA sample (10 l) was added to
loading buffer (4 l) and run on a 2.0% agarose gel
with ethidium bromide on preparation (FMC Bioproducts, Rockland, ME) at 100 V for 60 minutes.
The sizes of DNA products were visualized under
UV transillumination.
ITS1 direct sequencing and phylogenetic analysis
For automated DNA sequencing, the PCR
products of interest were excised from the gel and
purified using the Gel Extraction Kit (Perfectprep
Gel Cleanup, Eppendorf, Hamburg, Germany) according to the manufacturers specifications. The purified PCR products were subjected to direct sequencing using a DNA Sequencing Kit (Applied
Biosystems, CA) and primer 18SF1 in a Perkin
Elmer 310 Sequencer (Perkin-Elmer, Boston) according to the manufacturers instructions. Species
identification was determined by BLAST analysis.
ITS1 sequences obtained from this study were submitted to the Genbank database (www.ncbi.nlm.nih.
gov) and multiple aligned with reference sequences
of Malassezia standard strains (M. globosa;
AB019344, M. restricta; AB019340, M. slooffiae;
AB019348, M. sympodialis; AB019345, M. parchydermatis; AB019339, M. obtusa; AB019336 and M.
fufur; AB019329) using the CLUSTAL X program
(version 1.8). The TREEVIEW program (version 1.5)
was run for phylogenetic tree construction. The sample sequences appearing on the same node as the reference sequences were classified as belonging to the
same species.
RESULTS
Among the 60 infants diagnosed with ISD,
31 were male and 29 female with the majority below
2 months of age (62%), followed by 2-4 months
(28%), 4-6 months (5%), 6-12 months (2%) and 1224 months (3%). The most common site of affliction
was the scalp. Most patients displayed lesions on
102
MALASSEZIA IN INFANTILE SEBORRHEIC DERMATITIS
103
more than one site (Table 1). Cultures of 15 samples
yielded yeast-like colonies. One of those 15 samples
was from a patient with tinea versicolor. PCR was
performed and yielded products of 200 bp in 3 patients and of 300 bp in 12 patients. The PCR products were stained with ethidium bromide and visualized by UV transillumination (Fig. 1).
Cultures obtained from seborrheic dermatitis
in adult patients produced M. sympodialis, M. globosa, M. furfur and M. slooffia, with more than one
Malassezia species recovered at different anatomical
sites from both lesions and non-lesions.20 Nakabayashi et al.22 found that with seborrheic dermatitis in
adults, M. furfur (35%) and M. globosa (22%) were
isolated from facial skin lesions at significantly
higher rates than from normal subjects, in whom M.
globosa (22%), M. sympodialis (10%) and M. furfur
(3%) prevailed.
ITS1 DNA sequences were aligned using the
Clustal X computer program. The 300-bp product
matched the Malassezia furfur sequence (Accession
No. AY880912-AY880923) and the 200-bp product
the Candida sequence. (Accession No. AY880924AY880926). The phylogenetic tree was constructed
based on the ITS1 sequence data of Malassezia spp.
(Fig. 2). In 3 patients with a PCR product sizes of
200 bp, sugar fermentation using API 20C aux
yielded Candida species.
There are still various difficulties pertaining
to research on Malassezia and ISD. Both culture me-
DISCUSSION
Malassezia were found in many skin diseases as well as in healthy infants.6,10 RuizMaldonado et al.21 reported growth of M. furfur in
53% of healthy infants between 1 and 24 months old
and Bergbrant et al.7 reported it in 87% of healthy
children between 2 months and 15 years old with the
largest number of colonies found among children
aged between 2 and 23 months. The choice of culture
media is crucial to promote growth of Malassezia.
Tollesson et al.4 demonstrated that Malassezia failed
to grow in one particular medium (PDM; Pityrosporum Contact Plates; Biodisk AB, Solna, Sweden),
whereas it yielded positive cultures with 17 out of 20
specimens obtained from healthy children using a
different medium. (Max Lab Diagnostics HB, V.
Frolunda, Sweden).5
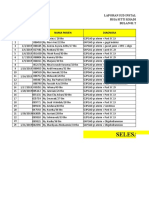
Fig. 1
Agarose gel electrophoresis of ITS1 amplified by 18SF1 and 58SR1 primer pair
yielding 200 bp (lane 1) and 300 bp (lanes
2 and 3) PCR products. Lane M, molecular
size marker. Lane P, positive control.
Lane N, negative control.
Table 1 Sites of affliction in 60 patients presented with infantile seborrheic dermatitis
1 Site
n = 27 (%)
2 Sites
n = 29 (%)
Scalp
16 (59)
20 (34)
4 (33.3)
Eyebrows
5 (19)
10 (17)
4 (33.3)
Post auricular
Site
3 Sites
n = 4 (%)
6 (22)
22 (37)
4 (33.3)
Cheek
4 (7)
Forehead
3 (5)
103
104
Fig. 2
WANANUKUL, ET AL.
Phylogenetic tree analysis of Malassezia spp. based on the ITS1 DNA sequences of 15 samples in this
study and 7 reference strains from the GenBank database. (S01: AY880924; S02: AY880912; S03:
AY880925; S04: AY880913; S05: AY880914; S06: AY880915; S07: AY880916; S08: AY880917; S09:
AY880918; S10: AY880919; S11: AY880920; S12: AY880926; S13: AY880921; S14: AY880922 and S15:
AY880923).
dia and the method of specimen collection certainly
affect the growth of Malassezia. The pathogenesis of
Malassezia is still controversial as it can induce cytokine production by keratinocytes,17,18 but can also
be found on non-lesion skin and even in healthy infants. There are conflicting results relating to its
growth subsequent to treatment in that there has been
some evidence of reduction23 which has been contradicted by other authors.4 Faergemann23 demonstrated a significantly reduced number of cultured
Pityrosporum orbeculare colonies in all groups
treated with miconazole-hydrocortisone, miconazole
and hydrocortisone, yet in the hydrocortisone group
it was still significantly higher than in other groups.
On the other hand, Tollesson et al.5 showed that the
number of M. furfur colonies did not significantly
change during the treatment and follow-up periods.
In our study, we found M. furfur in only
18% ISD lesions which is very low in comparison
with previous studies (70-90%).5,6 The low prevalence of Malassezia in this study may be due to different culture media, the specimen collection technique applying a contact plate, as well as the environment and methods of child rearing which in turn
can affect the growth of microorganisms. Therefore,
further studies especially targeting prevalence are required. Novel and effective methods pertaining to
both culture and culture media are imperative to
study the prevalence of Malassezia species and their
role in skin diseases.
ACKNOWLEDGMENTS
This work was supported in part by a grant
from Ratchadapiseksompotch Fund, Faculty of
Medicine, Chulalongkorn University, and the Thailand Research Fund, Senior Research Scholar. S.P. is
a Ph.D. student, supported by the Golden Jubilee
Ph.D. Program of the Thailand Research Fund. We
also would like to thank Venerable Dr. Mettanando
Bhikkhu of The Foundation of King Rama IX, the
great and Ms. Petra Hirsch for reviewing this manuscript.
REFERENCES
1. Faergemann J, Jones TC, Hettler O, Loria Y. Pityrosporum
ovale (Malassezia furfur) as the causative agents of seborrhoeic dermatitis: new treatment options. Br J Dermatol
1996; 134: 125.
2. Janniger CK. Infantile seborrheic dermatitis: an approach to
cradle cap. Cutis 1993; 51: 2335.
104
MALASSEZIA IN INFANTILE SEBORRHEIC DERMATITIS
105
3. Rajka G. Infantile seborrheic dermatitis. In: Harper J,
Orange A, Prose N, eds. Textbook of Pediatric Dermatology. Oxford, Blackwell Scientific 2000; pp. 255-9.
4. Ljubojevic S, Skerlev M, Lipozencic J, Basta-Juzbasic A.
The role of Malassezia furfur in dermatology. Clin Dermatol
2002; 20: 179-82.
5. Tollesson A, Frithz A, Stenlund K. Malassezia furfur in
infantile seborrheic dermatitis. Pediatr Dermatol 1997; 14:
423-5.
6. Broberg A, Faergemann J. Infantile seborrheic dermatitis
and Pityrosporum ovale. J Dermatol 1994; 21: 334-40.
7. Bergbrant IM, Brobug A. Pityrosporum ovale culture from
the forehead of healthy children. Acta Derm Venereol 1994;
74: 260-1.
8. Danker WM, Spector SA, Furer J, et al. Malassezia
fungemia in neonates and adults: complication of hyperalimentation. Rev Infect Dis 1987; 9: 743-53.
9. Larocco MA, Dorenbaum A, Robinson A, Pickering LK.
Recovery of Malassezia pachydermatis from eight infants in
a neonatal intensive care nursery: clinical and laboratory features. Pediatr Infect Dis J 1988; 7: 398-401.
10. Mickelsen PA, Viano-Paulson MC, Stevens DA, et al.
Clinical and microbiological features of infection with
Malassezia pachydermatis in high-risk infants. J Infect Dis
1988; 157: 1163-8.
11. Richet HM, McNeil MM, Edwards MC, et al. Cluster of
Malassezia furfur pulmonary infections in a neonatal intensive care unit. J Clin Microbiol 1989; 27: 1197-200.
12. Welbel SF, McNeil MM, Pramanik A, et al. Nosocomial
Malassezia pachydermatis bloodstream infections in a neonatal intensive care unit. Pediatr Infect Dis J 1994; 13: 1048.
13. Francis P, Walsh TJ. Approaches to management of fungal
infections in cancer patients. Oncol 1992; 6: 133-48.
14. Samonis G, Bafaloukas D. Fungal infections in cancer patients: an escalating problem. In Vivo 1992; 6: 133-48.
15. Gupta AK, Kohli Y, Li A, Faergemann J, Summerbell RC.
In vitro susceptibility of the seven Malassezia species to ketoconazole, voriconazole, itraconazole and terbinafine. Br J
Dermatol 2000; 142: 758-65.
16. Bergbrant IM, Andersson B, Faergemann J. Cell-mediated
immunity to Malassezia furfur in patients with seborrhoeic
dermatitis and pityriasis versicolor. Clin Expl Dermatol
1999; 24: 402-06.
17. Faergemann J, Bergbrant IM, Dohse M, Scott A, Westgate
G. Seborrhoeic dermatitis and Pityrosporum (Malassezia)
folliculitis: characterization of inflammatory cells and mediators in the skin by immunohistochemistry. Br J Dermatol
2001; 144: 549-56.
18. Watanabe S, Kano R, Sato H, Nakammura Y, Hasegawa A.
The effects of Malassezia yeasts on cytokine production by
human keratinocytes. J Invest Dermatol 2001;116: 769-73.
19. Makimura K, Tamira Y, Kudo M, Uchida K, Saito H. Species identification and strain typing of Malalassezia species
stock strains and clinical isolates base on the DNA sequences of nuclear ribosomal internal transcribed spacer 1
regions. Mycol Med 2000; 49: 29-35.
20. Gupta AK, Kohli Y, Summerbell C, Faergemann J. Quantitative culture of Malassezia species from different body sits
of individuals with or without dermatoses. Med Mycology
2001; 39: 243-51.
21. RuizMaldonado R, LopezMatinez R, Chavarria EP,
Castanon LR, Tamayo L. Pityrosporum ovale in infantile
seborrheic dermatitis. Pediatr Dermatol 1989; 6: 1620.
22. Nakabayashi A, Sei Y, Guiuol J. Identification of Malassezia
species isolated from patients with seborrheic dermatitis;
atopic dermatitis, pityriasis versicolor and normal subjects. J
Mycol Med 2000; 38: 337-41.
23. Faergemann J. Seborrheic dermatitis and Pityrosporum orbiculare: treatment of the seborrheic dermatitis of the scalp
with miconazone-hyerocortisone (Daktacort), miconazole
and hydrocortisone. Br J Dermatol 1986; 114: 695-700.
105
You might also like
- Lumpy Skin Disease: A Field Manual for VeterinariansFrom EverandLumpy Skin Disease: A Field Manual for VeterinariansNo ratings yet
- Development of An Enzyme-Linked Immunosorbant Assay (ELISA) For The Serodiagnosis of Canine Dermatophytosis Caused by Microsporum CanDocument6 pagesDevelopment of An Enzyme-Linked Immunosorbant Assay (ELISA) For The Serodiagnosis of Canine Dermatophytosis Caused by Microsporum CanjenNo ratings yet
- Epidermidis Carrying Biofilm Formation GenesDocument5 pagesEpidermidis Carrying Biofilm Formation GenesLini MaliqisnayantiNo ratings yet
- Roque Et Al., 2006. M. Audouninii M13.Document6 pagesRoque Et Al., 2006. M. Audouninii M13.leite321No ratings yet
- IJP 5 001paraDocument8 pagesIJP 5 001paraSetya AmaliaNo ratings yet
- Physical and Chemical Characterization of Avian ReovirusDocument9 pagesPhysical and Chemical Characterization of Avian ReovirusNariestaNo ratings yet
- Methicillin-Resistant StaphylococcusDocument5 pagesMethicillin-Resistant StaphylococcusAriane Barcellos Dos SantosNo ratings yet
- Colletotrichum Gloeosporioides From Mango Ataulfo: Morphological, Physiological, Genetic and Pathogenic AspectsDocument7 pagesColletotrichum Gloeosporioides From Mango Ataulfo: Morphological, Physiological, Genetic and Pathogenic AspectsresearchinbiologyNo ratings yet
- Dermatophyte Infections in CairoDocument5 pagesDermatophyte Infections in CaironevinNo ratings yet
- Resume Jurnal - InggrisDocument6 pagesResume Jurnal - InggrisMalikhatul WafiyahNo ratings yet
- EJHM Volume 77 Issue 6 Pages 5804-5816Document13 pagesEJHM Volume 77 Issue 6 Pages 5804-5816فردوس يسNo ratings yet
- Molecular Epidemiology Of: Fonsecaea SpeciesDocument6 pagesMolecular Epidemiology Of: Fonsecaea SpeciesJulie Yamile Fonseca ReyesNo ratings yet
- Nej M 199701163360302Document9 pagesNej M 199701163360302naim157No ratings yet
- Cridia SergipensisDocument19 pagesCridia SergipensisedugersNo ratings yet
- Investigation of Plant Extracts in Traditional Medicine - 2010 - Journal of EthDocument6 pagesInvestigation of Plant Extracts in Traditional Medicine - 2010 - Journal of EthAgnes ContarNo ratings yet
- Detection of Mycoplasma Contamination in Cell Cultures and Bovine SeraDocument7 pagesDetection of Mycoplasma Contamination in Cell Cultures and Bovine SeramaniiiiiiiiNo ratings yet
- Ijhs 10554+8363 8374Document12 pagesIjhs 10554+8363 8374radurere247No ratings yet
- Comparative Analysis of The Frequency, Distribution and Population SizesDocument7 pagesComparative Analysis of The Frequency, Distribution and Population SizesLarissa AlonsoNo ratings yet
- Isolation and Identification of Pathogenic Fungi From Diabetic Patients in DiyalaDocument9 pagesIsolation and Identification of Pathogenic Fungi From Diabetic Patients in DiyalaRaisya KeshaNo ratings yet
- Jof 03 00017Document10 pagesJof 03 00017Asterlita RyaneNo ratings yet
- Risk Factors For Otitis Media and Carriage of Multiple Strains of Haemophilus Influenzae and Streptococcus PneumoniaeDocument9 pagesRisk Factors For Otitis Media and Carriage of Multiple Strains of Haemophilus Influenzae and Streptococcus Pneumoniaeanggrenii SNo ratings yet
- International Journal of Health Sciences and ResearchDocument4 pagesInternational Journal of Health Sciences and ResearchCimol AgustinaNo ratings yet
- Incidence and Prevalence of Dermatophytosis in and Around Chennai, Tamilnadu, IndiaDocument6 pagesIncidence and Prevalence of Dermatophytosis in and Around Chennai, Tamilnadu, IndiaYanna RizkiaNo ratings yet
- Fungal Malassezia 2006Document9 pagesFungal Malassezia 2006DianaNo ratings yet
- Transmission and Persistence of Methicillin-Resistant Staphylococcus Aureus in Milk, Environment, and Workers in Dairy Cattle FarmsDocument6 pagesTransmission and Persistence of Methicillin-Resistant Staphylococcus Aureus in Milk, Environment, and Workers in Dairy Cattle Farmsadimas89No ratings yet
- PrimerDocument5 pagesPrimerrfsh rfshNo ratings yet
- Multiple-Antibiotic Resistance Mediated by Plasmids and Integrons in Uropathogenic Escherichia Coli and Klebsiella PneumoniaeDocument5 pagesMultiple-Antibiotic Resistance Mediated by Plasmids and Integrons in Uropathogenic Escherichia Coli and Klebsiella PneumoniaeProbioticsAnywhereNo ratings yet
- Detection of Toxoplasma Gondii by PCR and Quantitative PCR With High Specificty and Lower Limit of DetectionDocument7 pagesDetection of Toxoplasma Gondii by PCR and Quantitative PCR With High Specificty and Lower Limit of DetectionSholatya FurqonieNo ratings yet
- Antibiotic Resistance Profile of Staphylococci From Clinical Sources Recovered From InfantsDocument7 pagesAntibiotic Resistance Profile of Staphylococci From Clinical Sources Recovered From InfantsCornius TerranovaNo ratings yet
- Diagnosis of Breast Cancer Using Neural Network ApproachDocument8 pagesDiagnosis of Breast Cancer Using Neural Network ApproachNavneet YadavNo ratings yet
- Direct and Sensitive Detection of Trypanosoma Evansi by Polymerase Chain ReactionDocument9 pagesDirect and Sensitive Detection of Trypanosoma Evansi by Polymerase Chain ReactionFernando RamiroNo ratings yet
- Molecular Characterization of Fluconazole Resistant Candida Isolated From Pregnant Women in A Tertiary Healthcare InstitutionDocument7 pagesMolecular Characterization of Fluconazole Resistant Candida Isolated From Pregnant Women in A Tertiary Healthcare Institutionijmb333No ratings yet
- 143-Article Text-451-1-10-20230129Document9 pages143-Article Text-451-1-10-20230129radurere247No ratings yet
- Case Report: Severe Congenital Toxoplasmosis: A Case Report and Strain CharacterizationDocument4 pagesCase Report: Severe Congenital Toxoplasmosis: A Case Report and Strain CharacterizationNamanamanaNo ratings yet
- BBRC Vol 14 No 04 2021-36Document6 pagesBBRC Vol 14 No 04 2021-36Dr Sharique AliNo ratings yet
- Potential Development of Temephos Resistance in Aedes Aegypti Related To Its Mechanism and Susceptibility To Dengue VirusDocument6 pagesPotential Development of Temephos Resistance in Aedes Aegypti Related To Its Mechanism and Susceptibility To Dengue VirusMichael KevinNo ratings yet
- 35429-Article Text-126139-2-10-20180206Document5 pages35429-Article Text-126139-2-10-20180206Robertus RonnyNo ratings yet
- Adherence of Staphylococcus Intermedius To Canine Corneocytes in VitroDocument8 pagesAdherence of Staphylococcus Intermedius To Canine Corneocytes in VitrojenNo ratings yet
- Effects of Ribavirin and Hydroxyurea On Oral Infection of Aedes Aegypti (L.) With Dengue VirusDocument7 pagesEffects of Ribavirin and Hydroxyurea On Oral Infection of Aedes Aegypti (L.) With Dengue VirusRogério HitsugayaNo ratings yet
- 3.evaluation of DFM, Isolation - IJPBS-July 2012Document5 pages3.evaluation of DFM, Isolation - IJPBS-July 2012SHIVA JYOTHINo ratings yet
- Causes of Infectious Acute Diarrhea in Infants Treated at Pediatric ClinicDocument5 pagesCauses of Infectious Acute Diarrhea in Infants Treated at Pediatric ClinicBrenda KarinaNo ratings yet
- The Multistage Process of Carcinogenesis in Human Esophageal Epithelial Cells Induced by Human PapillomavirusDocument8 pagesThe Multistage Process of Carcinogenesis in Human Esophageal Epithelial Cells Induced by Human PapillomavirusIlma Kurnia SariNo ratings yet
- Toxoplasmose Latente EsplenomegaliaDocument11 pagesToxoplasmose Latente EsplenomegaliaWeverson LinharesNo ratings yet
- in Vitro Antiherpetic Activity of An Aqueous Extract From The Plant Phyllanthus OrbicularisDocument7 pagesin Vitro Antiherpetic Activity of An Aqueous Extract From The Plant Phyllanthus OrbicularisLednys Palomino ZambranoNo ratings yet
- The Investigation On The Distribution of Malassezia Yeasts On The Normal Korean Skin by 26S rDNA PCR-RFLPDocument9 pagesThe Investigation On The Distribution of Malassezia Yeasts On The Normal Korean Skin by 26S rDNA PCR-RFLPGerman GodinezNo ratings yet
- Jurnal HibridisasiDocument12 pagesJurnal HibridisasiNurfanida Natasya mNo ratings yet
- Identification of Infective Larva (L3) Proteins of Strongyloides Stercoralis by ImmunoblotDocument5 pagesIdentification of Infective Larva (L3) Proteins of Strongyloides Stercoralis by ImmunoblotMardhiyanti KhamidaNo ratings yet
- Comparative Methods For Demonstration: Study of Tissue Culture of Toxoplasma GondiiDocument4 pagesComparative Methods For Demonstration: Study of Tissue Culture of Toxoplasma GondiiSalim JufriNo ratings yet
- EpidemiologicalStudyofSomeCandidaalbicans PDFDocument7 pagesEpidemiologicalStudyofSomeCandidaalbicans PDFTerem TebautaNo ratings yet
- Neopetrosia ChaliniformisDocument5 pagesNeopetrosia ChaliniformisMuh. Ade ArtasastaNo ratings yet
- PDF 9Document7 pagesPDF 9Justy GuavaNo ratings yet
- Determining The Antibiotic Resistance Potential of The Indigenous Oral Microbiota of Humans Using A Metagenomic ApproachDocument6 pagesDetermining The Antibiotic Resistance Potential of The Indigenous Oral Microbiota of Humans Using A Metagenomic ApproachdiegovelizNo ratings yet
- 11733-Article Text-105903-1-10-20200629Document6 pages11733-Article Text-105903-1-10-20200629FERNANDO GOMEZ ORDOÑEZNo ratings yet
- Molecular Characterization of Extended-Spectrum BetaLactamase (ESBLs) Genes in Pseudomonas Aeruginosa From Pregnant Women Attending A Tertiary Health Care Centre in Makurdi, Central NigeriaDocument7 pagesMolecular Characterization of Extended-Spectrum BetaLactamase (ESBLs) Genes in Pseudomonas Aeruginosa From Pregnant Women Attending A Tertiary Health Care Centre in Makurdi, Central NigeriaJASH MATHEWNo ratings yet
- Hasanbeigi Et AlDocument4 pagesHasanbeigi Et AlAhmad BukhariNo ratings yet
- Development of A PCR Test To Differentiate Between Staphylococcus Aureus and Staphylococcus IntermediusDocument4 pagesDevelopment of A PCR Test To Differentiate Between Staphylococcus Aureus and Staphylococcus IntermediusFina RahmiNo ratings yet
- Use of Destained Cytology Slides For The Application of Routine PDFDocument9 pagesUse of Destained Cytology Slides For The Application of Routine PDFovejacaracolNo ratings yet
- Typhoidal Salmonaelle in Holy Familyred Crescent Medical College Hospital, Dhaka, BangladeshDocument4 pagesTyphoidal Salmonaelle in Holy Familyred Crescent Medical College Hospital, Dhaka, BangladeshTanveer KhanNo ratings yet
- Prepared By: Ken Robin A. Canada, RMT, Mls AscpiDocument35 pagesPrepared By: Ken Robin A. Canada, RMT, Mls AscpiKen Robin CanadaNo ratings yet
- 1 s2.0 0168170286900080 MainDocument13 pages1 s2.0 0168170286900080 MainfalmazanNo ratings yet
- Tcid 50Document10 pagesTcid 50Rohan Walking Tall100% (1)
- Best Supplements For ADHD and Focus Support For Kids - GNC IndiaDocument3 pagesBest Supplements For ADHD and Focus Support For Kids - GNC IndiaTrần Thị UyênNo ratings yet
- F17 Reflection 383 FN - 15 Nov 17Document7 pagesF17 Reflection 383 FN - 15 Nov 17jigsawNo ratings yet
- Nso AblaparotomyDocument3 pagesNso AblaparotomyAleeya SarajanNo ratings yet
- WRAS MarinasDocument4 pagesWRAS MarinasAdam ReesNo ratings yet
- Groupwork Proposal BSW 3705 June 2022Document17 pagesGroupwork Proposal BSW 3705 June 2022Mtshali Nthuseng100% (1)
- Laporan Iud 2019Document91 pagesLaporan Iud 2019Yuli AntiNo ratings yet
- Location: Capacity: Architect: Mr. Anil Yadav: Qutub Institutional Area 150 PatientsDocument18 pagesLocation: Capacity: Architect: Mr. Anil Yadav: Qutub Institutional Area 150 PatientsManishaDhimanNo ratings yet
- Zombie Brains PDFDocument1 pageZombie Brains PDFLorna GrayNo ratings yet
- Cases in Health Services Management Sixth Edition 6th Edition Ebook PDFDocument61 pagesCases in Health Services Management Sixth Edition 6th Edition Ebook PDFkelli.rechtzigel668100% (43)
- CircCircuit Protection in Health Care Facilitiesuit Protection in Health Care FacilitiesDocument43 pagesCircCircuit Protection in Health Care Facilitiesuit Protection in Health Care FacilitiesMenaNo ratings yet
- Assisting For Endotracheal IntubationDocument16 pagesAssisting For Endotracheal IntubationSREEDEVI T SURESH100% (1)
- Block-D FinalDocument47 pagesBlock-D FinalAnonymous 7IKdlmNo ratings yet
- An Electromyographical Analysis of Sumo and Conventional Style DeadliftsDocument8 pagesAn Electromyographical Analysis of Sumo and Conventional Style DeadliftsRafael EscamillaNo ratings yet
- LimpDocument7 pagesLimpRakesh DudiNo ratings yet
- APLS Scenario OSCE PDFDocument5 pagesAPLS Scenario OSCE PDFNikita JacobsNo ratings yet
- UFGS 09 97 13.17 Interior Coating of Steel Petroleum TanksDocument39 pagesUFGS 09 97 13.17 Interior Coating of Steel Petroleum TanksThomas M RiddleNo ratings yet
- Englishmelon Oet Writing Test 2Document2 pagesEnglishmelon Oet Writing Test 2Cam Achondo56% (27)
- Clothier-Wright2018 Article DysfunctionalVoidingTheImportaDocument14 pagesClothier-Wright2018 Article DysfunctionalVoidingTheImportaMarcello PinheiroNo ratings yet
- Nzmail 18821014Document26 pagesNzmail 18821014zeljkogrNo ratings yet
- Treatment and Prognosis of Febrile Seizures - UpToDateDocument14 pagesTreatment and Prognosis of Febrile Seizures - UpToDateDinointernosNo ratings yet
- 21.JMM Promotion and Management, Inc. vs. Court of AppealsDocument3 pages21.JMM Promotion and Management, Inc. vs. Court of AppealsnathNo ratings yet
- Mental HealthDocument14 pagesMental Healthapi-455779994100% (1)
- 5 Cover Letter Samples For Your Scientific ManuscriptDocument11 pages5 Cover Letter Samples For Your Scientific ManuscriptAlejandra J. Troncoso100% (2)
- Combat StressDocument94 pagesCombat StressClaudia Maria Ivan100% (1)
- 3 Colinet Dustsampling PDFDocument21 pages3 Colinet Dustsampling PDFom pandeyNo ratings yet
- SR.# Weight (KG) Height (FT) Age (Yrz) Others RecommendationsDocument2 pagesSR.# Weight (KG) Height (FT) Age (Yrz) Others RecommendationsshaniNo ratings yet
- HKS CannabisDocument21 pagesHKS CannabisRavioli Boo GaddamNo ratings yet
- Answers To Questions: Earl John E. CañoneroDocument2 pagesAnswers To Questions: Earl John E. CañoneroEarl CañoneroNo ratings yet
- Business Ethics and Corporate Social Responsibility: Analyze Complex Issues in CSR and Corporate GovernanceDocument6 pagesBusiness Ethics and Corporate Social Responsibility: Analyze Complex Issues in CSR and Corporate GovernanceDime PierrowNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (30)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (60)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainFrom EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainRating: 4 out of 5 stars4/5 (95)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)