Professional Documents
Culture Documents
Step 3 Nephrology Part 1 of 3
Uploaded by
Bhavin ChoksiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Step 3 Nephrology Part 1 of 3
Uploaded by
Bhavin ChoksiCopyright:
Available Formats
USMLE Step 3 Video Review Course
Part 1 of 3
Nephrology
N. D. Agrawal, MD
Premier Review
USMLE Step 3 Video Review Course
Nephrology
Part 1 of 3
N .D. Agrawal, MD
Copyright 2009 by Premier Review, USMLE Step 3 Review Course. All rights reserved. No part of this material may be reported or
transmitted in any form or by any means without the permission of the Premier Review.
Care has been taken to confirm the accuracy of the information presented and to describe generally accepted practices. However, the
authors are not responsible for errors or omissions or any consequences from application of the information in this hand out and make
no warranty, express or implied, with respect to the contents of the material.
Copyright, Premier Review. Please DO NOT copy. Copying this material is violation of copyright law.
USMLE Step 3 Video Review Course
Part 1 of 3
Nephrology
N. D. Agrawal, MD
Urine Cast:
Tam Horsefall proteins are secreted by thick ascending loop and make Hyaline cast, it is a normal finding
Muddy brown granular cast- ATN
RBC cast, dysmorphic RBC- Glomerulonephritis
WBC, Granular cast- Interstitial nephritis, Acute Pyelonephritis
Oval or round fat droplets (In polarized light have maltese cross appearance)- Proteinuria
Waxy cast or Broad cast- Chronic kidney disease
Acute Renal Failure
Pre-Renal
Intra-Renal
Post Renal or Obstructive Uropathy
Post Renal
Elderly: mostly secondary to Prostate enlargement in male
Pelvic tumor, Ca cervix in female
Young adults- stone
Children- urethral valve, urethral stenosis, stenosis of vesico-ureteral junction
Post void residual>200ml- highly suspicious
Test of choice- Renal ultrasound- dilated bladder, ureter, calyceal system (hydronephrosis)
Ultrasound ve no obstruction
Ultrasound +ve look for the cause
If no obvious cause- do IVP, Retrograde pylography, Lasix renogram
Treatment: Lower tract obstruction- Foleys catheter
Upper tract obstruction- Ureteral stent or percutaneous nephrostomy
Once obstruction is relieved massive diuresis can occur- T/t- IVF 75cc/hr
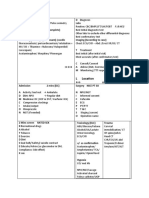
BUN/Creatinine
Urine sodium
FENa
Pre-Renal
>20:1
<10
<1
Renal
<20:1
>20
>1
Pre-Renal
Secondary to poor renal perfusion
Causes:
Dehydration
Peripheral vasodilatation eg. Sepsis
Low cardiac output
GI bleeding
Excess diuresis
T/t: IVF
Intra-Renal
Acute tubular necrosis (ATN)
Muddy Brown Cast
FENa >1%
Urine Na >20
Copyright, Premier Review. Please DO NOT copy. Copying this material is violation of copyright law.
USMLE Step 3 Video Review Course
Part 1 of 3
Nephrology
N. D. Agrawal, MD
Causes:
Ischemia- Dehydration, GI bleed-usually patients are oliguric
Toxin- Aminoglycoside, Ampho B, Radiocontrast, Myoglobinuria secondary to Rhabdomyolysis
Aminoglycoside and radio contrast cause non oliguric ARF
Contrast nephropathy typically begins immediately after the study, renal function starts recovering after 3-5
days
Aminoglycoside nephrotoxicity begins at least after 5 days of treatment
Prevention of contrast nephropathy Hydration, normal saline 75cc/hr 8-12 hr before and after the study.
Acetylcystein-600mg BID for 2 days in high risk patient eg. Pt. with diabetes, CHF, CRI
Rhabdomyolysis causing ARF
Cause:
Prolonged immobilization- Comatose patient or after prolonged surgery in one position e.g. elderly hip
fracture reduction.
Crush injury
Seizure
Patient struggling against restraints
Cocaine or other drug induced agitation
Extreme exertion
Neuroleptic Malignant syndrome
Labs: CPK, urine- blood+++, but microscopy- No RBC
Treatment: IVF, IV Sodium bicarbonate to alkalinize urine to solubilize myoglobin
Mannitol or forced diuresis
Tumor Lysis syndrome
Secondary to chemotherapy for malignancy, usually Burkitts lymphoma, Leukemia
ARF, hyperkalemia, Hyperphosphatemia, hypocalcemia, Uric acid
Treatment; Hemodialysis
Prevention: Allopurinol prior to chemotherapy, IVF+ sod.Bicarb to alkalinize urine which increases
solubility of uric acid
Acute interstitial nephritis
ARF + Fever + rash + arthralgia + Peripheral blood eosinophilia
Urine- WBC cast +ve, eosinophil +ve (Wrights stain)
Cause: Penicillin, Sulfonamide, NSAID (Including COX-2 inhibitors), Rifampin, Allopurinol, Indinavir, 5aminosalicylates, Proton Pump Inhibitors
Treatment: stop drug +Prednisone (can be prescribed)
Note: In NSAID induced acute interstitial nephritis typical features-Fever, rash, eosinophilia, eosinophiluria are
usually absent. Features like ARF, Increased WBC in urine, WBC cast and h/o use of NSAID should be there.
Papillary necrosis
Causes
Analgesic abuse
Diabetes
Sickle cell anemia
Obstructive uropathy
Copyright, Premier Review. Please DO NOT copy. Copying this material is violation of copyright law.
USMLE Step 3 Video Review Course
Part 1 of 3
Nephrology
N. D. Agrawal, MD
Labs: CT abdomen without contrast is study of choice
IVP-Ring shadow at papillary tip
Indication of hemodialysis
Hyperkalemia, metabolic acidosis (refractory to medical treatment)
Symptoms of uremia: abdominal pain, nausea, vomiting, anorexia, Asterixis, seizure, uremic pericarditis
Volume overload-Refractory to diuretics
Athero-embolic renal disease (Cholesterol emboli)
Another cause of ARF
Usually elderly patient with severe atherosclerosis went for angioplasty or angiography or vascular surgeryabout 3-4 weeks before (mostly subacute presentation)
ARF +cyanosis or gangrene in the toes, although peripheral pulses are intact + livedo reticularis
Lab finding hypocomplementemia, eosinophilia, urine eosinophil
If diagnosis in doubt- biopsy of skin lesion or kidney.
Treatment-supportive, no role of anticoagulation
Clot emboli causing Acute Renal Failure
Patient with history of A. Fibrillation comes with c/o acute onset of flank pain, nausea, vomiting and acute renal
failure
Confirm with Radioisotope Renogram (Study of choice) or Doppler ultrasound of renal arteries
Treatment: Heparin followed by coumadin
Glomerulonephritis
C/F: Hematuria, proteinuria, hypertension
Causes:
IgA nephropathy
Post - streptococcal GN
Wegener's granulomatosis
Good Pasture syndrome
Endocarditis
Lupus Nephritis
IgA nephropathy
History of upper respiratory tract infection, 1-2 days before presentation + Hematuria
Usually history of recurrent Hematuria following URI or exertion (after playing with children)
U/A- RBC + RBC cast or dysmorphic RBC + Protein
Other labs: in 50% Serum IgA increased, so normal IgA does not rule the diagnosis.
Normal complement level
To confirm renal biopsy
Treatment:
ACE inhibitor+ARB (Angiotensin II receptor blocker)
Fish Oil (Add if there is continued gradual deterioration despite ACE inhibitor/ARB)
Prednisone (Add if progressively active disease despite ACE inhibitor/ARB/Fish oil or severe disease to
begin with, like Nephrotic syndrome/ markedly proliferative disease on biopsy)
Copyright, Premier Review. Please DO NOT copy. Copying this material is violation of copyright law.
USMLE Step 3 Video Review Course
Part 1 of 3
Nephrology
N. D. Agrawal, MD
Post - streptococcal GN
History of URI 7-10 days before the presentation + Hematuria
Labs:
U/A- RBC + RBC cast or dysmorphic RBC + Protein
ASO titer
Low serum complement
Treatment:
Supportive
Almost 100% children will recover.
<5% adults will develop chronic renal failure
Wegener's granulomatosis
History of upper respiratory tract involvement (sinusitis or persistent rhinorrhea or bloody nasal discharge)
+ Lower respiratory tract symptoms (cough, shortness of breath, hemoptysis)
Chest X-ray- diffuse opacity or alveolar opacity or nodular lesion with cavity.
+ Hematuria, proteinuria
+ renal failure
+ cANCA +ve
U/A- RBC, RBC cast or dysmorphic RBC
Confirm with biopsy of nasopharyngeal lesion ( preferable)
If there is no nasopharyngeal lesiondo renal biopsy( shows crescentic necrotizing GN)
Treatment: Corticosteroid + Cyclophosphamide
Good Pasture syndrome
History of hemoptysis + Hematuria , proteinuria + renal failure
+anti-GBM antibody +ve
U/A- RBC, RBC cast or dysmorphic RBC
Treatment: Plasmapheresis +prednisone + Cyclophosphamide
Endocarditis
Presents with fever, peripheral signs of arterial emboli due to endocarditis.
C/O- flank pain, Hematuria
Labs: U/A- RBC, RBC cast
Hypocomplementemia
Renal failure
Lupus Nephritis:
Six types
Type I- Minimal mesangial
Type II- Mesangial proliferative
Type III- Focal proliferative
Type IV- Diffuse proliferative
Type V- Membranous
Type VI- Advance sclerosis
Prognosis is worst in Type IV.
Copyright, Premier Review. Please DO NOT copy. Copying this material is violation of copyright law.
USMLE Step 3 Video Review Course
Part 1 of 3
Nephrology
N. D. Agrawal, MD
Treatment:
Type I & II- No specific treatment, Just treat lupus
Type III If < 40% glomeruli involved, only Prednisone.
> 40% involved- Treat like Type IV.
Type IV Intravenous pulse Cyclophosphamide- Monthly X 6 dose.
Intravenous pulse Methylprednisone 1gm daily X 3 dose then monthly X 6 dose
Type V Non nephrotic proteinuria- only Prednisone
Nephrotic Proteinuria- Cyclosporine oral + Oral prednisone
Patients on Cyclophosphamide, should get:
Trimethoprim- Sulfamethoxazole Prophylaxis for PCP
IV hydration and MESNA- During infusion to prevent hemorrhagic cystitis and bladder cancer
Leuprolide (in women of child bearing age)- To prevent ovarian failure.
Patient on long term high dose steroid should get:
H2 Blocker or Proton Pump inhibitor- To prevent gastritis
Calcium and Vitamin D or Biphosphonate To prevent osteoporosis
Nystatin (Swish and swallow )- To prevent oropharyngeal candidiasis.
Nephrotic syndrome
C/F: Proteinuria >3.5gm/24h, Edema, Hypoalbuminemia, Hyperlipidemia
These pt. also have hypercoagulable state secondary to loss of anti-thrombin III in urine
Causes:
Renal:
Minimal Change Disease
Membranous Nephropathy
Focal segmental glomerular sclerosis
Systemic disease:
Systemic lupus Erythematosus
Diabetes
Amyloidosis
Minimal Change Disease
Most common cause of Nephrotic syndrome in children
Causes: Mostly idiopathic, Hodgkins disease, NSAID
Renal biopsy: on electron microscopy- fusion of epithelial foot processes are characteristic finding
Renal biopsy is a must in adults to diagnose minimal change disease but in children due to very high
prevalence empiric trial of corticosteroid is recommended and biopsy is done only in resistant cases
Treatment: Prednisone Relapse Again Prednisone
Frequent relapses: Cyclophosphamide
Membranous nephropathy
Most common cause of Nephrotic syndrome in adults
Causes: Idiopathic, Carcinoma, Hepatitis B, Hepatitis C, Systemic lupus erythematosus, Drugs-Gold,
Penicillamine, Captopril
Treatment: Prednisone
Copyright, Premier Review. Please DO NOT copy. Copying this material is violation of copyright law.
USMLE Step 3 Video Review Course
Part 1 of 3
Nephrology
N. D. Agrawal, MD
Focal Segmental Glomerular Sclerosis
Most common cause of Nephrotic syndrome in blacks, obese patients, IVDA, heroin abuse, HIV
Treatment: Prednisone
Mild proteinuria: May be Functional or Orthostatic
24 hour urine < 150mg / 24 hour is normal
Functional proteinuria: due to fever, stress, congestive heart failure or any other acute illness. If patient was
acutely sick at the time of urine collection, repeat the test after the acute event is over.
Orthostatic proteinuria: proteinuria at upright position, usually history of athlete with proteinuria. Take
morning spot sample of urine for protein and Creatinine or split urine collection of 16 hour (day time) and 8
hour (night)
CCS:
Patient with significant bilateral leg edema, facial swelling, may have anasarca
If has anasarca or crackels in lung field admit the patient and use IV furosemide otherwise manage as
outpatient with oral furosemide.
Labs: CBC, CHEM 8, PT/PTT, Liver function test, Lipid profile, Urine analysis, chest x-ray, EKG 12 lead
Order: Furosemide (oral if sending home, IV if admitting the patient)
Result: Urine analysis: Protein 3+, low albumin, increased cholesterol
Order: 24 hour urine for protein and creatinine, ANA, C3, C4, Hepatitis B Surface antigen, Hepatitis B
Surface antibody, Hepatitis C antibody, HIV, Renal ultrasound, start simvastatin, oral
Follow up results: Nephrotic range proteinuria
Order: Kidney biopsy
Result: Membranous Nephropathy
Order: PPD, Age appropriate cancer screening
Follow up results: Everything is normal:
Order: Prednisone, oral, continuous; Pantoprazole, oral; Nystatin, swish and swallow; Calcium, oral;
vitamin D, oral.
Copyright, Premier Review. Please DO NOT copy. Copying this material is violation of copyright law.
You might also like
- Hepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHepatorenal Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Uw Ccs Blog CasesDocument5 pagesUw Ccs Blog Cases808kailuaNo ratings yet
- CardiologyDocument8 pagesCardiologykhalidzubairiNo ratings yet
- Cephalosporins and FriendsDocument4 pagesCephalosporins and FriendsErika De JesusNo ratings yet
- Testicular Ultrasound Clinical Score NotesDocument15 pagesTesticular Ultrasound Clinical Score NotesrashmiajNo ratings yet
- AC(E) USMLE Step 2 Poisoning MnemonicsDocument5 pagesAC(E) USMLE Step 2 Poisoning MnemonicsMahmoud MohsenNo ratings yet
- Usmle Woreld MedicineDocument108 pagesUsmle Woreld MedicineSaeed HasanNo ratings yet
- Step 3 General Medicine Part 1 of 2Document10 pagesStep 3 General Medicine Part 1 of 2Bhavin ChoksiNo ratings yet
- Dr. Waqas Ayubian Notes For Step 3Document772 pagesDr. Waqas Ayubian Notes For Step 3Muhammad HammadNo ratings yet
- Renal Notes Step 2ckDocument34 pagesRenal Notes Step 2cksamreen100% (1)
- Cardiac and vascular disease treatment guideDocument9 pagesCardiac and vascular disease treatment guideDaanish100% (1)
- Words From The Wise-2017-Shelf2ck - CsDocument24 pagesWords From The Wise-2017-Shelf2ck - CsManoj SomagutaNo ratings yet
- Pediatrics - Allergy & Immunology TopicsDocument40 pagesPediatrics - Allergy & Immunology TopicspreethamNo ratings yet
- Mkasap Endocrinology NotesDocument6 pagesMkasap Endocrinology NotesUm HamoOdNo ratings yet
- Upper Gastrointestinal Endoscopy Is The Diagnostic Study of Choice When A Patient Presents With Acute Alkali Ingestion. 2Document2 pagesUpper Gastrointestinal Endoscopy Is The Diagnostic Study of Choice When A Patient Presents With Acute Alkali Ingestion. 2Mariam MohamedNo ratings yet
- My Step 3 228 Experience:: Materials UsedDocument2 pagesMy Step 3 228 Experience:: Materials UsedRicardoMelendez0% (1)
- Obgyn Step 3 Notes 140123143640 Phpapp02Document18 pagesObgyn Step 3 Notes 140123143640 Phpapp02anna grass100% (1)
- Arlete S Notes PDFDocument28 pagesArlete S Notes PDFjrabeNo ratings yet
- 2008 It e CritiqueDocument78 pages2008 It e Critiquerofi modiNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument96 pagesDr. Ali's Uworld Notes For Step 2 CKuyesNo ratings yet
- My Notes On Qbank QuestionsDocument10 pagesMy Notes On Qbank QuestionsRaffy GutmanNo ratings yet
- Case Files PedsDocument54 pagesCase Files PedsSam ZeezNo ratings yet
- Sports MedicineDocument32 pagesSports Medicinersimranjit100% (1)
- YFT IM Notes 1Document100 pagesYFT IM Notes 1AHMAD ALROWAILYNo ratings yet
- Nephrology PDFDocument38 pagesNephrology PDFOmar AyashNo ratings yet
- TiKi TaKa CK NEUROLOGYDocument24 pagesTiKi TaKa CK NEUROLOGYprofahmedNo ratings yet
- USMLE STEP 2 MCQsDocument1 pageUSMLE STEP 2 MCQsAhmad Waleed0% (2)
- Protozoal, bacterial and viral infections, cancer screening, cardiovascular disease and treatmentDocument20 pagesProtozoal, bacterial and viral infections, cancer screening, cardiovascular disease and treatmentHunter Ross100% (1)
- An Insight Into Step 3Document4 pagesAn Insight Into Step 3SpencerNo ratings yet
- Emergency Patient Care GuideDocument10 pagesEmergency Patient Care GuideRyan Turner100% (1)
- RX Beta Blocker Posioning: Recent Ingestion - Emesis, Bradycardia: Atropine - Isoproterenol - Glucagon - PaceDocument13 pagesRX Beta Blocker Posioning: Recent Ingestion - Emesis, Bradycardia: Atropine - Isoproterenol - Glucagon - PacepathoTM100% (2)
- L LocationDocument2 pagesL LocationZee MirzaNo ratings yet
- TiKi TaKa CK Preventive MedicineDocument3 pagesTiKi TaKa CK Preventive MedicinenonsNo ratings yet
- IM Shelf - AmbossDocument61 pagesIM Shelf - AmbossHaadi AliNo ratings yet
- Tiki Taka EndocrinoloyDocument17 pagesTiki Taka EndocrinoloykakuNo ratings yet
- Archer Usmle Step3 Ccs Workshop PDFDocument57 pagesArcher Usmle Step3 Ccs Workshop PDFSadia Ghani100% (1)
- UWorld Step3 CCS-1Document13 pagesUWorld Step3 CCS-1Sarah LCNo ratings yet
- 17 - Toronto Notes 2011 - NephrologyDocument92 pages17 - Toronto Notes 2011 - NephrologyKhairulsani Yusof100% (2)
- Step 2 CK NotesDocument76 pagesStep 2 CK Noteskeyurb100% (1)
- USMLE Step 2 Rapid Review - Flash Cards - 2Document92 pagesUSMLE Step 2 Rapid Review - Flash Cards - 2Mohammed FaragNo ratings yet
- International Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessFrom EverandInternational Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessRaghav GovindarajanNo ratings yet
- Objectives IMDocument104 pagesObjectives IMlaraNo ratings yet
- STIs, herpes screening, HPV vaccination, and prenatal careDocument26 pagesSTIs, herpes screening, HPV vaccination, and prenatal careAyodeji SotimehinNo ratings yet
- Satish Advani 271 CK ExperienceDocument10 pagesSatish Advani 271 CK ExperienceDileepa SuraweeraNo ratings yet
- Chronic Liver Disease PresentationDocument202 pagesChronic Liver Disease PresentationMohammadAbdurRahmanNo ratings yet
- Post-void residual volume and bladder scan interpretationDocument7 pagesPost-void residual volume and bladder scan interpretationyanks1120No ratings yet
- Top 10 Nephro Slides in Board ExamsDocument223 pagesTop 10 Nephro Slides in Board ExamsMirza Shaharyar Baig100% (2)
- 11th May MRCP RecallsDocument2,080 pages11th May MRCP Recallsgirlygirl10No ratings yet
- Routine Miracles: Personal Journeys of Patients and Doctors Discovering the Powers of Modern MedicineFrom EverandRoutine Miracles: Personal Journeys of Patients and Doctors Discovering the Powers of Modern MedicineRating: 3 out of 5 stars3/5 (1)
- Step 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionFrom EverandStep 3 Board-Ready USMLE Junkies 2nd Edition: The Must-Have USMLE Step 3 Review CompanionNo ratings yet
- N .D. Agrawal, MD: Infectious DiseasesDocument5 pagesN .D. Agrawal, MD: Infectious DiseasesBhavin ChoksiNo ratings yet
- Anti InfectiveProphylaxisinHeme OncDocument11 pagesAnti InfectiveProphylaxisinHeme OncBhavin ChoksiNo ratings yet
- Step 3 Medical GeneticsDocument7 pagesStep 3 Medical GeneticsBhavin ChoksiNo ratings yet
- Step 3 Human Development Part 1 of 1Document8 pagesStep 3 Human Development Part 1 of 1Bhavin ChoksiNo ratings yet
- Step 3 General Medicine Part 2 of 2Document15 pagesStep 3 General Medicine Part 2 of 2Bhavin ChoksiNo ratings yet
- Two and A Half Men - 4x06 - Apologies For The Frivolity - enDocument30 pagesTwo and A Half Men - 4x06 - Apologies For The Frivolity - enBhavin ChoksiNo ratings yet
- Step 3 General Medicine Part 1 of 2Document10 pagesStep 3 General Medicine Part 1 of 2Bhavin ChoksiNo ratings yet
- Usmle Essential BooksDocument3 pagesUsmle Essential BooksBhavin Choksi33% (3)
- Adverse Event Chloroquine 1Document8 pagesAdverse Event Chloroquine 1Ingrid KoutioNo ratings yet
- Kidney 360 2020 MicrohematuriaDocument7 pagesKidney 360 2020 MicrohematuriaRichardNo ratings yet
- NefIgArd TrialDocument12 pagesNefIgArd Trialfarah mujtabaNo ratings yet
- Nephritic SyndromeDocument10 pagesNephritic SyndromeRam AryalNo ratings yet
- Approach To Pateint With Edema Print VersionDocument14 pagesApproach To Pateint With Edema Print VersionmaybeNo ratings yet
- Pediatric Hematuria Guide: Causes, Evaluation and ManagementDocument40 pagesPediatric Hematuria Guide: Causes, Evaluation and ManagementAnoop ThoombayilNo ratings yet
- Understanding Glomerular Diseases: Nephritic vs Nephrotic SyndromesDocument127 pagesUnderstanding Glomerular Diseases: Nephritic vs Nephrotic SyndromesCoy NuñezNo ratings yet
- Proteinuria A Guide To Diagnosis and AssDocument7 pagesProteinuria A Guide To Diagnosis and AssMarcelliaNo ratings yet
- PlabDocument214 pagesPlabKarata SinghNo ratings yet
- An Update On The Pathogenesis and Treatment of IgADocument12 pagesAn Update On The Pathogenesis and Treatment of IgAYulius DonyNo ratings yet
- Pregnancy Induced Urinary Tract Changes Urinary Tract InfectionsDocument5 pagesPregnancy Induced Urinary Tract Changes Urinary Tract InfectionsDilausan B MolukNo ratings yet
- Model Poster MedicinaDocument1 pageModel Poster MedicinaGabriela BichirNo ratings yet
- Stine Helene Falsig Pedersen (Editor) - Reviews of Physiology, Biochemistry and Pharmacology. 177-Springer (2021)Document155 pagesStine Helene Falsig Pedersen (Editor) - Reviews of Physiology, Biochemistry and Pharmacology. 177-Springer (2021)shuvvro dhaNo ratings yet
- Pathology Board Exam QuestionsDocument9 pagesPathology Board Exam QuestionschristinejoanNo ratings yet
- KDIGO 2021 Glomerular Diseases GuidelineDocument276 pagesKDIGO 2021 Glomerular Diseases GuidelineAmbulatório Dieta Cetogênica HUBNo ratings yet
- NephroticDocument8 pagesNephroticsangheetaNo ratings yet
- Clinical Approach To RPRF PDFDocument6 pagesClinical Approach To RPRF PDFshankarNo ratings yet
- Diagnostic Algorithms in Renal Biopsy PDFDocument27 pagesDiagnostic Algorithms in Renal Biopsy PDFRajeev Pareek100% (1)
- Handbook of Urology Diagnosis and Therapy (3rd Ed.) - Lippincott Williams & WilkinsDocument556 pagesHandbook of Urology Diagnosis and Therapy (3rd Ed.) - Lippincott Williams & WilkinsdimasNo ratings yet
- New Insights in The Pathogenesis of Immunoglobulin A VasculitisDocument9 pagesNew Insights in The Pathogenesis of Immunoglobulin A VasculitisMikeyNo ratings yet
- Differential Diagnosis: Disease/Condition Differentiating Signs/Symptoms Differentiating TestsDocument2 pagesDifferential Diagnosis: Disease/Condition Differentiating Signs/Symptoms Differentiating TestsMuchsan SiregarNo ratings yet
- Chapter 21 - Urologic Aspects of Pediatric Nephrology - Campbell - Walsh-Wein UROLOGY 12thDocument19 pagesChapter 21 - Urologic Aspects of Pediatric Nephrology - Campbell - Walsh-Wein UROLOGY 12thkrisnaNo ratings yet
- ThePaleoApproach List of Autoimmune DiseasesDocument3 pagesThePaleoApproach List of Autoimmune DiseasesdevabakhtiNo ratings yet
- HematuriaDocument42 pagesHematuriaAhmad SobihNo ratings yet
- HEMATURIADocument9 pagesHEMATURIAAndreina AcevedoNo ratings yet
- Internal Medicine Mar 2022Document8 pagesInternal Medicine Mar 2022Sanielle Karla Garcia LorenzoNo ratings yet
- Renal Pathology Guide on Kidney Structure and FunctionDocument37 pagesRenal Pathology Guide on Kidney Structure and Functionapplesncore100% (1)
- Post Infectious Glomerulonephritis PDFDocument9 pagesPost Infectious Glomerulonephritis PDFilham fahrudinNo ratings yet
- Renal Module Anatomy and Physiology ReviewDocument71 pagesRenal Module Anatomy and Physiology ReviewFatima AbduljalilNo ratings yet
- Prof Djoko - Autoimmune Kidney Disease v2 ENGDocument35 pagesProf Djoko - Autoimmune Kidney Disease v2 ENGlaboratorium spektrumNo ratings yet