Professional Documents
Culture Documents
V22n02a14 PDF
Uploaded by
Samuel DuarteOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
V22n02a14 PDF
Uploaded by
Samuel DuarteCopyright:
Available Formats
166 Dent J (2011) 22(2): 166-170
Braz
J.H. Damante et al.
ISSN 0103-6440
Larva migrans in the Oral Mucosa:
Report of Two Cases
Jos Humberto DAMANTE1
Luiz Eduardo Montenegro CHINELLATO1
Fernando Toledo de OLIVEIRA1
Cleverson Teixeira SOARES2
Raul Negro FLEURY2
1Department
of Oral Medicine, Bauru Dental School, USP - University of So Paulo, Bauru, So Paulo, Brazil
2Departament of Pathology, Lauro de Souza Lima Institute, Bauru, SP, Brazil
Cutaneous Larva migrans is a very common disease in tropical regions. In the oral mucosa, the infection occurs in the same way as in
the skin, but it is rarer. This report describes two cases of Larva migrans in the oral mucosa. The first case was in a 27-year-old woman
who presented an erythematous plaque located on the buccal mucosa, extending to a posterior direction, following a linear pattern, to
other areas of the mouth. After incisional biopsy of the anterior-most portion of the lesion, morphological details obtained in multiple
examined sections suggested Necator or Ancylostoma braziliense larvae as the cause of infection. The second case was in a 35-yearold male who presented a fusiform erythematous plaque in the palatal mucosa. This area was removed and submitted to microscopic
examination under a presumptive diagnosis of parasite migratory stomatitis. The histological characteristics were suggestive of a
larva pathway. In both cases the lesion disappeared after biopsy and the patients were symptom-free.
Key Words: Larva migrans, oral parasite, subcutaneous oral lesion.
INTRODUCTION
Domesticated or wild animals have many parasites
whose infectious larvae are capable of completing their
life cycle only inside their natural host. When these larvae
infect a different host, including humans, they are usually
not able to grow properly. In these cases, the larvae may
migrate through the visceral or subcutaneous tissue,
causing lesions in the skin or mucosa (1). Therefore, the
term Larva migrans is used to describe the pathologies
caused by migration of larvae that usually do not infect
the human organism.
Visceral Larva migrans is rarer and normally
affects the liver in conjunction with pulmonary
infiltration. It is usually caused by a larva of the Toxocara
genus (2). On the other hand, cutaneous Larva migrans
is characterized by erythematous, pruriginous, and
serpiginous lesions that are similar to a sinuous snakelike trace (3). Cutaneous Larva migrans is a self-limited
disease because the larva cannot mature in the human
organism, dying after 4 weeks (4).
The etiological agents found with greater
frequency in these cutaneous infections are helminthes
belonging to the Cestode and Nematode classes,
especially Ancylostoma brasiliense and Ancylostoma
caninum. These parasites are commonly found in the
small intestine of dogs and cats (1).
These infections are more common in tropical
countries and in Central and South America (1-4).
Contamination usually occurs by direct contact of the
skin or mucosa with contaminated surfaces, especially
sand or vegetation, which are favored places for domestic
animals to deposit their feces (3). The most frequently
affected body parts are the feet, legs, buttocks, hands,
and forearms (4). Although these parasites also infect
mucosas, such as the oral mucosa, there are few reports
in the literature about these cases (1-4).
In order to address this gap in the literature, this
report describes two cases of Larva migrans found in
the oral mucosa.
Correspondence: Prof. Fernando Toledo de Oliveira, Departamento de Estomatologia, Faculdade de Odontologia de Bauru, USP, Alameda Dr. Octvio
Pinheiro Brisolla, 9-75, Vila Universitria, 17012-101 Bauru, SP, Brasil. Tel: +55-14-3235-8254. e-mail: fto@usp.br
Braz Dent J 22(2) 2011
Larva migrans in the mouth: report of cases
CASE REPORT
Case 1
A 27-year-old female from a rural area was
referred to our services by a dermatologist who requested
a biopsy. The patient complained of oral canker sores
that migrated in different directions in the mouth,
producing an itching sensation and leaving her with the
impression of a bug crawling in her mouth. When these
lesions reached the throat, the patient reported significant
discomfort, including dyspnea.
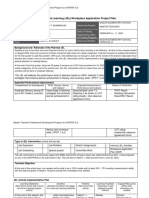
The lesion extended to a posterior direction in a
linear pattern, crossing the retromolar trigone and soft
palate, until it reached the anterior pillar of the opposite
side of the tonsils (Fig. 1A). The oral inspection revealed
an erythematous plaque located on the buccal mucosa,
next to the right side of the lip commissure (Fig. 1B).
Incisional biopsy of the anterior-most portion
of the lesion was performed (Fig. 1B) and showed the
following microscopic aspects: oral mucosa constituted
of stratified squamous epithelium with spongiosis,
intraepithelial vesicles, and exocitosis. Under the
epithelium, the lamina propria showed intense subacute
inflammatory reaction, edema, fissures surrounded
by hemorrhagic areas, mononuclear infiltrate, and
numerous eosinophils (Fig. 2A).
In other areas seen in transversal sections, an
intraepithelial tunnel containing a tubular-shape parasite
with narrow lumen, compatible with a helminth larva,
was identified (Fig. 2B, arrow). Morphologic details
obtained in multiple examined sections suggested
Necator or Ancylostoma braziliense larvae as the cause
of infection as opposed to larvae such as Toxocara canis,
Ascaris lumbricoides, and Strongiloides stercoralis.
All of these helminthes can lead to the Larva migrans
clinical manifestation, which was the final diagnosis in
this case. The lesion spontaneously disappeared 1 week
after biopsy.
Case 2
A 35-year-old male, non-smoker, working in a
rural area, was referred to our service for examination
of erythematous lesions in the oral mucosa. The
lesions had appeared 3 months before examination and
were recurrent and burning. The patients denied the
occurrence of any systemic alterations in his medical
history, mentioning only the occurrence of cutaneous
167
sandworms and a habit of chewing grass or wood chips.
Intraoral inspection revealed a linear lesion,
continuous throughout almost the entire oral area. The
lesion presented as a fusiform erythematous plaque that
initiated in the right area of the palatal mucosa, crossed
the palate to the left side, descended to the inferior
anterior alveolar mucosa, and ended in the buccal mucosa
on the right side (Fig. 3A,B).
In the buccal mucosa, in one of the extremities
of the larva pathway, there was an area that was larger,
more erythematous, more elevated, and mildly sensitive
to palpation. This 3-cmm-wide fusiform area was
removed and submitted to microscopic examination
under a presumptive diagnosis of parasite migratory
stomatitis.
The histological sections demonstrated an oral
mucosa fragment with mild epithelial hyperplasia. The
subjacent stroma presented intense edema, erythrocyte
overflow, and dilated vessels, as well as a mononuclear
infiltrate with a large number of polymorphonuclear
cells. The infiltrate affected the epithelium, leading to
spongiosis and the development of vesicles with serosity,
neutrophils, and eosinophils. Some areas had multiple
vesicles that formed a reticular pattern (Fig. 4A). The
subepithelial area presented abscesses amongst hyaline
material, with a tubular larva (Fig. 4B, arrow). The
histological characteristics were suggestive of a larva
pathway, with possible fragments of the parasite. The
lesion disappeared after incisional biopsy.
DISCUSSION
Cutaneous Larva migrans is a very common
disease in tropical regions (1-4). Animals, especially
dogs and cats, eliminate thousands of parasite eggs in
their feces. In ideal temperature and humidity conditions,
the eggs develop larvae. The larvae hatch and feed
on organic matter and microorganisms in the soil. In
approximately seven days, the larva reaches the infective
state. In dogs and cats, the larvae reach sexual maturity
within approximately 4 weeks. In the human body, the
larvae actively penetrate through the skin and migrate
through the subcutaneous area for weeks or months and
then eventually die (1).
Larva migrans in oral mucosa is rare (1-5), but
the infection occurs in the same way as in the skin, i.e.,
through direct contact with surfaces contaminated with
larvae. In the two reported cases, patients may have been
infected due to the lack of adequate hygiene of the hands
Braz Dent J 22(2) 2011
168
J.H. Damante et al.
and other body parts that could contact contaminated
dirt. The grass-chewing habit, which is common among
rural workers, is another contamination source, and it
was reported in Case 2. Capuano et al. (3) reported a
case of a patient from a rural area who had dogs and
cats in their backyard and who would eat fruits that had
fallen on the ground without washing them.
Jaeger et al. (2) reported another case in which
the infection probably occurred through direct contact
with surfaces contaminated with dog and cat feces. The
authors stated that the inoculation of the parasite might
have occurred because the patient, who was a fisherman,
used to hold fishing hooks between his lips, and these
objects had had contact with beach sand.
Regarding the clinical manifestation, the first
symptom is an erythematous papule at the larva
penetration site, which then evolves into a vesicle. Along
its migration route, the larva produces intense itching.
In older cutaneous lesions, crusts are formed, leaving a
dark line that later disappears (1,5).
The clinical manifestation is the same in oral
mucosa. In the case reported by Capuano et al. (3),
the lesions were originally composed of vesicles on
the palate and rapidly transformed into migratory
Figure 1. Clinical images of Case 1. A = Erythematous linear spot on the soft palate continuing as a linear erythematous plaque on the
buccal mucosa, on the right side; B = Detail of the anterior portion of the lesion. Emphasis on the hemorrhagic aspect.
Figure 2. Photomicrographs of Case 2. A = Oral mucosa with intense subacute inflammatory reaction, erythrocyte overflow, lymphocyte
predominance, and a large number of eosinophils. Presence of rounded eosinophilic structure compatible with parasite; B = Detail
indicating probable anterior extremity of the parasite, with tubular structure and narrow lumen.
Braz Dent J 22(2) 2011
Larva migrans in the mouth: report of cases
and pruriginous lesions in several areas of the mouth.
Although the larva can migrate a reasonable distance, it
is generally confined to a small territory. In some cases
(3,4), lesions are extensive, leaving a pathway in various
areas of the oral cavity, possibly due to more than one
infecting parasite.
In the human body, larvae are not able to maturate
and die between 4 and 8 weeks after infection. Therefore,
this is a self-limited disease. In some cases, there may
be hypersensitivity to the parasite, with the development
of urticaria and local edema (4). In addition, there may
be discomfort associated with the symptoms, such as
169
dyspnea when lesions reach the throat, as reported by
the patient in Case 1.
The diagnosis of Larva migrans is primarily
clinical, i.e., based on signs and symptoms. However,
because its presentation in the oral mucosa is rare,
incisional biopsy of the newest portion of the lesion is
recommended. This enables the parasite to be detected,
as in Case 1.
The larva belongs to the Cestode or Nematode
classes (4,6). The main etiological agents are
Ancylostoma brasiliense and Ancylostoma caninum,
which are parasites of the small intestine of dogs and
Figure 3. Clinical images of Case 2. A = Linear erythematous plaque crossing the palate; B = Anterior portion of the lesion affecting
the lip area and the buccal mucosa.
Figure 4. Photomicrographs of Case 2. A = Oral mucosa with epithelial hyperplasia; hemorrhagic areas and subepithelial inflammatory
infiltrate; and exocytosis. Suprabasal tubular structures (arrow). B = Detail showing eosinophilic-contour tunnel with fragment of
amorphous structure that is compatible with parts of the parasite (arrow). Emphasis on the mononuclear inflammatory infiltrate and
on the large number of eosinophils.
Braz Dent J 22(2) 2011
170
J.H. Damante et al.
cats. However, other parasites such as Ancylostoma
ceylonicum, Uncinaria stenocephala, Bubostomum
phebotomum, Gongylonema species, Anatrichosoma
cutaneum, Strongyloides stercoralis, and Necator
americanus can also cause the disease (4). In Case 1,
the morphologic characteristics of the parasite were
compatible with Necator americanus or Ancylostoma
brasiliense. Similar to the cases presented by other
authors (2,3), the histopathological examinations
did not allow us verifying the nature of the larva
with certainty, although some measurements and
morphologic characteristics matched the ones observed
for Ancylostoma larvae.
Although cutaneous Larva migrans is a selflimited disease because the larvae cannot mature and
dies within a few weeks, the majority of the authors
recommend treatment (1-4). The treatment may be
surgical, with either an excisional (4) or an incisional
biopsy, as performed in the two cases described in the
present report. Topic or systemic drug therapy is also an
option (1,4). In extensive cases with multiple lesions,
the systemic use of albendazole or thiabendazole is
recommended. In a previous oral Larva migrans case
(4), the lesion healed completely with systemic use of
thiabendazole (25 mg/kg twice a day for 5 days).
Finally, although oral Larva migrans is not
severe, it is a rare disease. Therefore, the reporting of
new cases is necessary so that lack of knowledge does
not compromise the diagnosis and treatment of patients.
RESUMO
Larva migrans cutnea uma doena muito comum em regies
tropicais. Na mucosa oral, a infeco ocorre da mesma forma
como na pele, mas raro. Este relato descreve dois casos de
Larva migrans na mucosa oral. O primeiro caso foi de uma
mulher de 27 anos de idade, que apresentou uma placa eritematosa
localizada na mucosa julgal, estendendo-se posteriormente, em
conformao linear, para outras reas da boca. Aps bipsia
incisional da poro mais anterior da leso, detalhes morfolgicos
obtidos em mltiplos cortes examinados sugeriram Necator ou
larvas de Ancylostoma braziliense como a causa da infeco.
O segundo caso foi de um homem de 35 anos de idade que
apresentou uma placa fusiformes eritematosas na mucosa palatina.
Esta rea foi removida e submetida a exame microscpico, com
diagnstico presuntivo de estomatite migratria por parasita.
As caractersticas histolgicas foram sugestivas de trajeto de
larva. Em ambos os casos a leso desapareceu aps a bipsia e
os pacientes estavam assintomticos.
REFERENCES
1. Andre J, Bernard M, Ledoux M, Achten G. Larva migrans of the
Braz Dent J 22(2) 2011
oral mucosa. Dermatologica 1988;176:296-298.
2. Jaeger RG, Arajo VC, Marcucci G, Arajo NS. Larva migrans in
the oral mucosa. J Oral Med 1987;42:246-247.
3. Capuano ACT, Sousa SCOM, Carvalhosa AA, Pinto Junior DS.
Larva migrans in the oral mucosa: Report of case. Quintessence
Int 2006;37:721-723.
4. Lopes MA, Zaia AA, Almeida OP, Scully C. Larva migrans that
affect the mouth. Oral Surg Oral Med Oral Pathol 1994;77:362367.
5. Hansen LS, Allard RHB. Encysted parasitic larvae in the mouth.
J Am Dent Assoc 1984;108:632-636.
6. Lambertucci JR, Rayes A, Serufo JC, Teixeira DM, GerspacherLara R, Nascimento E, et al.. Visceral Larva migrans and
tropical pyomyositis: A case report. Rev Inst Med Trop S Paulo
1998;40:383-385.
Accepted December 23, 2010
You might also like
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Conic SectionDocument58 pagesConic SectionNailah Sakinah100% (1)
- Modelling of Induction Motor PDFDocument42 pagesModelling of Induction Motor PDFsureshNo ratings yet
- Sengoku WakthroughDocument139 pagesSengoku WakthroughferdinanadNo ratings yet
- Al-Rimawi Et Al-2019-Clinical Oral Implants ResearchDocument7 pagesAl-Rimawi Et Al-2019-Clinical Oral Implants ResearchSohaib ShujaatNo ratings yet
- Muhammad v. Hall, 10th Cir. (2017)Document12 pagesMuhammad v. Hall, 10th Cir. (2017)Scribd Government DocsNo ratings yet
- Fractional GradingDocument7 pagesFractional Gradingapi-355619062No ratings yet
- Umair Mazher ThesisDocument44 pagesUmair Mazher Thesisumair_mazherNo ratings yet
- 14-15 TDP HandbookDocument28 pages14-15 TDP Handbookapi-266268398No ratings yet
- Module 2 - Content and Contextual Analysis of Selected Primary andDocument41 pagesModule 2 - Content and Contextual Analysis of Selected Primary andAngelica CaldeoNo ratings yet
- Intermediate Reading Comprehension Test 03Document5 pagesIntermediate Reading Comprehension Test 03MZNo ratings yet
- H-1 Nationalism in Europe NotesDocument5 pagesH-1 Nationalism in Europe Noteskanishk kumarNo ratings yet
- Mock Exam 2Document33 pagesMock Exam 2Althea Karmylle M. BonitaNo ratings yet
- BUMANGLAG - CLASS D - JEL PlanDocument3 pagesBUMANGLAG - CLASS D - JEL PlanMAUREEN BUMANGLAGNo ratings yet
- Endocrine Hypothyroidism HyperthyroidismDocument16 pagesEndocrine Hypothyroidism HyperthyroidismJeel MohtaNo ratings yet
- VDA ChinaDocument72 pagesVDA Chinatuananh1010No ratings yet
- 5 - Econ - Advanced Economic Theory (Eng)Document1 page5 - Econ - Advanced Economic Theory (Eng)David JackNo ratings yet
- INTRODUCTION Quali Observation ReportDocument2 pagesINTRODUCTION Quali Observation Reportmira hamzahNo ratings yet
- Simple Past Tense The Elves and The Shoemaker Short-Story-Learnenglishteam - ComDocument1 pageSimple Past Tense The Elves and The Shoemaker Short-Story-Learnenglishteam - ComgokagokaNo ratings yet
- DRR Module 4 Detailed Lesson PlanDocument8 pagesDRR Module 4 Detailed Lesson PlanFe Annalie Sacal100% (2)
- The Story of Babri MasjidDocument54 pagesThe Story of Babri MasjidKiran Penumala100% (1)
- Theo 5Document2 pagesTheo 5chingchongNo ratings yet
- Acute Care Handbook For Physical Therapists 5Th Edition Full ChapterDocument41 pagesAcute Care Handbook For Physical Therapists 5Th Edition Full Chaptergloria.goodwin463100% (20)
- Research Online Research OnlineDocument11 pagesResearch Online Research OnlineMunib HussainNo ratings yet
- Blind and Visually ImpairedDocument5 pagesBlind and Visually ImpairedPrem KumarNo ratings yet
- Media Planning SampleDocument37 pagesMedia Planning SampleHuzaifa Aman AzizNo ratings yet
- Web Search - One People's Public Trust 1776 UCCDocument28 pagesWeb Search - One People's Public Trust 1776 UCCVincent J. CataldiNo ratings yet
- Kung Fu MedicinesDocument9 pagesKung Fu MedicinesDavid HewittNo ratings yet
- 2 - RUBRIC PHY110 (For Student)Document3 pages2 - RUBRIC PHY110 (For Student)Puteri AaliyyaNo ratings yet
- The Meaning of Al FatihaDocument11 pagesThe Meaning of Al Fatihammhoward20No ratings yet
- Silvianita - LK 0.1 Modul 2 English For Personal CommunicationDocument3 pagesSilvianita - LK 0.1 Modul 2 English For Personal CommunicationSilvianita RetnaningtyasNo ratings yet