Professional Documents
Culture Documents
Approach To A Child With Fever
Uploaded by
vikoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Approach To A Child With Fever
Uploaded by
vikoCopyright:
Available Formats
Viral fevers: viral hepatitis, enteroviral,
chicken pox, measles, mumps
Infective endocarditis
Abscess
Approach to a child with fever at the
Kanti Childrens Hospital OPD in
children of more than 2 months
It is the Commonest symptom for which
parents bring their children to Kanti
Childrens Hospital. It should be carefully
reviewed because often there are
no
localizing signs, managed with different
modalities of treatment and often present
late with modified pathology. It is necessary
to have good clinical approach to reach the
cause of fever and avoid unnecessary use
of antibiotics or diagnostic tools. It is
essential to differentiate fever under two
heading: fever for less than three days and
fever for more than three days for the OPD
management.
Fever of less than three days
Malaria. Kalazar
UTI
Approach to Fever - In a brief history, it is
essential to ask for (do not ask those
questions for which you cans see e.g. ear
discharge, rash etc)
1. Duration of fever
Family members or at
hostel having similar illness
Associated symptoms:
vomiting, diarrhea, cough,
convulsion, urinary problem.
Treatment given
2. Travel to other places
3. History of immunization
Causes - Common causes of fever in
different age groups are as follows:
Quick Examination: (It is mandatory to
examine a child with minimum clothes)
2 months to 1 yr
A. The following signs must be carefully
looked for:
Respiratory infection nasopharyngitis,
pneumonia, tonsillitis, otitis media
Viral fevers - influenza, measles, hepatitis,
chicken-pox,
mumps,
herpangina
GI infection- dysentery, diarrhea
Occult sepsis
Skin infection -abscess, pyodermas
Urinary Tract Infection
Malaria, Kalazar
Dehydration fever.
1yr to 5 yr
Respiratory infection
GI infection - Typhoid, diarrhea
1.Look of the child - sick looking, toxic,
playful
2.Resp. rate, cyanosis, icterus,
lymphadenopathy, petechiae, purpuric
spots, dehydration, sweating, red weeping
eyes, blisters, generalized or local
tenderness , salivation, swellings, wounds.
Swollen, tender joints.
3. Throat and ear: tonsils, ulcer over palate
and gum, ear discharge and drum
4. Abdomen: hepatomegaly, splenomegaly,
tenderness (right hypochondria appendicitis)
5. Meningism or bulging fontanalle, neck
stiffness
6. Chest: murmurs, ronchi, creps, reduced
air entry.
Which patients needs admission?
Children with suspected meningitis (include
first convulsion with fever even the child
does not have meningeal signs) moderate to
severe dehydration, subcostal indrawing,
suspected of occult sepsis, bacterial
endocarditis,
purpura, large abscess,
severe pallor, severe malnutrition, GI
bleeding, respiratory distress, on oral
antibiotic for 5 days and the child looks toxic
with high fever.
Which patients could be discharged from
OPD?
Most of the patients who does not have the
severe signs could be followed up from
OPD. Children with fever on their first visit
may not have localizing signs within three
days of onset of fever. Fever is not an
indication to write antibiotics. Antibiotic can
only be prescribed if site of infection is
known. These children are prescribed with
antipyretics and discharged with good
counseling.
What to do in the next follow-up?
Look for the localizing signs. If signs are
present treatment and investigations are
done accordingly. If no localizing signs are
seen following investigations are asked for:
It is common practice to ask for a battery of
investigations, which should be avoided
unless - fever is for prolonged time and not
responding to routine treatment
- chronic fevers which relapse frequently
Common investigations to be asked for are
1. Total and Differential WBC count , ESR.
2. Blood culture, Urine culture
UTI is
strongly suspected (pus cells are moderate
to high/HPF).
3. X-ray chest - if signs of pneumonia,
empyema, pleural effusion or primary
complex, or no localizing signs
4. Liver function tests
5. Mantaux tests.
Clinical approach to a child with fever
A good clinical history and a thorough
physical examination should form the basis
of making a provisional diagnosis.
Laboratory tests should only be supportive
and not an alternative to clinical diagnosis.
A. History
1. Age: Fever in infants < 2 months of age
should be considered as evidence of serious
bacterial infection until proven otherwise.
2. Duration of fever : Fever lasting for more
than 4-7 days is rarely due to self limiting
viral illness and needs investigation. Fever
lasting for more than 2 weeks indicates
serious underlying problem and needs
thorough investigation.
3. Chills and rigors: both are non specific
and suggest no definite etiology. Similarly
sweating and night sweats are non specific
in children.
4. Pattern of fever : The wide use of the
antipyretics modifies the natural pattern of
fever. It is not necessary to find out the type
of temperature (continuous, remittent or
intermittent) in the OPD setting. Nausea
may indicate hepatic disease. Persistence of
headache and vomiting may indicate
meningitis.
5. Progress of fever: Fever due to viral
infection peaks over a day or two and
gradually declines in 3-4 days. Bacterial
fever worsens if left untreated. Malarial fever
develops suddenly and declines swiftly.
6. Accompanying symptoms: specific
symptoms help in localising the site of
infection such as cough/cold in respiratory
illness, diarrhea/vomiting in GI infection,
dysuria in UTI, drowsiness or convulsions in
meningitis. Non specific symptoms include
bodyache, headache, anorexia, vomiting
and irritability. Many children react with fever
by these symptoms. These usually
disappear with the reduction of fever.
Persistence of anorexia, headache and
vomiting is seen in infective hepatitis,
tubercular meningitis or UTI.
7. Contact with similar diseases:
Knowledge of the epidemiology of a
prevailing illness helps in suspecting the
illness.
8. Past history of similar illness:
Recurrent viral infections are common in
children especially in the first year of school.
Children between 2 months to 5 years of
age are also susceptible to recurrent viral
infections. Malaria may often recur, as the
therapy is merely suppressive.
9. Drugs used in the treatment and its
response
The inter febrile state helps in the evaluation
of the probable cause of fever. Patterns of
fever have limited value in predicting the
etiology of fever. Therapeutic response to an
antibiotic is very difficulty to assess
accurately. Natural remission of a viral fever
may be interpreted as response to an
antibiotic. Typically, fever due to bacterial
infection responds to antibiotic in 2-3 days.
Typhoid fever takes longer duration to
normalize.
10. Immunization: Vaccine preventable
diseases are rare in immunized children.
Clinical manifestations of the disease are
often modified in immunized children.
e) Severe pallor
f) Abdominal guarding / rigidity
2. General examination:
i) General appearance: Toxic/ill look
indicates serious illness. Irritability or
discomfort may either be due to pain or
respiratory distress. A comfortable child
indicates that a benign illness is likely.
ii) Body temperature: Must be quickly
judged by merely touching the skin over the
central and peripheral parts of the body.
Differential
body
temperature:
warm
chest/abdomen and cool periphery-indicates
severe illness.
iii) Pulse rate: With every degree
Fahrenheit rise in the fever, pulse rate goes
up by 10 beats/min. Disproportionate
increase in the pulse rate may suggest early
sepsis or primary cardiac disease.
iv) Respiratory rate : Normal ratio of pulse
and respiration in health is 4:1. The ratio is
increased in primary cardiac disease and
decreased in respiratory pathology.
v) Skin rash
vi) Lymphadenopathy
vii) ENT examination (often forgotten)
3. Systemic examination
B. Physical examination:
i. Respiratory system
1. Assess seriousness:
ii. Central nervous system
Presence of the following signs suggests the
possibility of serious underlying diseases:
iii. Cardiovascular system
a) Respiratory distress
iv. Abdomen
b) Drowsiness / meningeal signs
c) Signs of impending shock
d) Purpuric spots
Good clinical history and thorough
physical examination form the first
step in the management of fever in
children.
Inter febrile clinical state without
antibiotic is the best predictor of
fever etiology.
Beware of warning signs that may
suggest serious underlying illness in
a febrile child.
C. Clinical approach to fever in relation to
the duration of the fever:
See Algorithm I-A : Fever of 1-3 days
I.Therapeutic trial in undiagnosed fever:
In case of failure to diagnose inspite of
rational approach, the following may be
considered:
Trial with chloroquine (considering
epidemiology)
Trials with antibiotics, choice based
on the presumptive diagnosis. Trial
with broad spectrum antibiotics
should not be considered without
relevant investigations to rule out
serious infections such as UTI,
Meningitis, Typhoid or Pneumonia.
If the response to the first antibiotic
is poor, another drug may be tried.
If two drugs have failed, it is logical
to reconsider the diagnosis rather
than change the antibiotic.
Do not try empirical treatment for
tuberculosis
except
in
lifethreatening
situations,
wherein
treatment must be completed for full
conventional period, unless another
cause for fever is found out during
the trial period.
Steroids should never be used for
undiagnosed fever.
III. Change of specific antibiotic in fever:
Do not prescribe an antibiotic
without presumptive diagnosis.
Routine investigations must be
carried out to support the diagnosis.
As clinical diagnosis of Bacterial
infection in OPD is rarely possible
within the first 2-3 days of fever,
(except in case of Tonsillitis or otitis)
In confirmed diagnosis, change of
therapy is rarely necessary.
Improvement is anticipated over
varying period of time in different
drug
sensitive,
uncomplicated
infections.
E.g. in malaria fever is under control in 2
days In respiratory infections 3-4 days In
tuberculosis fever may continue for 1-2
weeks. In typhoid the fever begins to decline
by 4th day of antibiotic therapy. The culture
sensitivity reports for salmonella typhi from
Kanti Childrens Hospital Laboratory shows
nearly more than 80% are sensitive to cotrimoxazole.
II. Empirical choice of antibiotic in fever:
prescribing
antibiotic
is
not
recommended during this period.
If antibiotic is justified then, for most
community
infections,
oral
amoxycillin, or cotrimoxazole is
sufficient (first line drugs).
Injectable antibiotics are almost
never needed in OPD practice.
Newer
antibiotics
are
not
recommended
for
routine
community acquired infections.
In case of therapeutic failure check
drug dosage, compliance, presence
of any complications and the
correctness of the diagnosis.
In case the diagnosis is reasonably
confirmed
again,
appropriate
change of antibiotic is necessary
based on the knowledge of
prevalence of drug resistance
pattern,
unless
specific
bacteriological diagnosis and drug
sensitivity pattern is available for
choice of an antibiotic.
Therapeutic failure even after the
second trial of antibiotic demands
reconsideration of diagnosis.
IV. Clinical approach to partially treated
fever:
In such conditions the clinical picture might
have been modified by prior therapy. If
etiologic evidence is based on reasonable
evidence, dosage & compliance of drug is
checked. In case of suspected drug
resistance, change of therapy is justified. If
the disease has never been diagnosed and
the therapy is empirical, failure of response
may be due to wrong diagnosis. It is best to
continue
empirical
therapy
while
investigations are repeated to arrive at the
right diagnosis.
V. Interpretation of laboratory tests in
partially treated fever:
Lab tests need to be repeated in
patients who continue to be febrile
even after few days of therapy
Some tests may be modified by
therapy.
E.g.
WBC
counts,
peripheral smear for malarial
parasites, urinalysis and bacterial
culture.
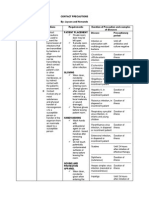
Algorithm for fever (less than three days)
Persistence of high ESR inspite of
treatment suggests uncontrolled
active disease. So is persistent
eosinopenia, hence change in
therapy may be indicated.
Change from neutrophilic response
to
lymphocytic
response
in
peripheral
smear
indicates
recovering bacterial infection, hence
to continue the same antibiotic.
Improving laboratory tests with no
clinical response should alert the
physician to the possibility of
complications.
Clinical improvement with persistent
abnormal tests warrants close
observation without change in the
antibiotic.
Fever of 1-3 days duration
No
Specific localizing
signs and
symptoms
Signs organ specific
part of system involved
Tonsillitis,
pharyngitis, UTI
Probble bacterial
aetiology
Specific antibiotic
therapy
No localizing
signs/symptoms
Assess seriousness
Meningeal signs
Respiratory distress
Purpura
Surgical abdomen
Septic shock
Yes:
Hospitalize
Multiple organs or part of the
System involved
URTI, LRTI, respiratory tract
with GI system involvement
Probably viral aetiology
Symptomatic
therapy
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Heart SoundDocument29 pagesHeart Sounddianpratiwirahim100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Pediatric History and Physical Exam GuideDocument7 pagesPediatric History and Physical Exam GuideIndunil AnuruddhikaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Medical AbbreviationsDocument2 pagesMedical AbbreviationsAdrian Jun ChuNo ratings yet
- Nursing Care Plan for Postpartum PainDocument2 pagesNursing Care Plan for Postpartum PainJoseph Nawen Sindiong100% (1)
- C Post Concussion ChecklistDocument1 pageC Post Concussion Checklistalston96No ratings yet
- Genetic Disorders SourcebookDocument748 pagesGenetic Disorders Sourcebookpaconscribd100% (1)
- APPROACH TO MANAGING JOINT PAINDocument44 pagesAPPROACH TO MANAGING JOINT PAINKavya Anoop100% (1)
- AphasiaDocument71 pagesAphasiaVarun B RenukappaNo ratings yet
- AHA Vs ERC GuidelinesDocument39 pagesAHA Vs ERC GuidelinesYoel Harianto100% (2)
- Pediatric H&P Assessment and PlanDocument10 pagesPediatric H&P Assessment and PlanmaddythedocNo ratings yet
- Febrile InfantDocument5 pagesFebrile InfantvikoNo ratings yet
- FeverDocument33 pagesFeverNikki KyriacouNo ratings yet
- NICE Fever GuideDocument38 pagesNICE Fever Guidedante_chungaNo ratings yet
- Cards Resp 2Document4 pagesCards Resp 2vikoNo ratings yet
- Graduate SOAP NOTE TEMPLATEDocument7 pagesGraduate SOAP NOTE TEMPLATEMiley MunozNo ratings yet
- PSA and Psoriasis Exam ChecklistDocument2 pagesPSA and Psoriasis Exam ChecklistChaken ManiyanNo ratings yet
- Contact PrecautionsDocument2 pagesContact PrecautionsCristina L. JaysonNo ratings yet
- Medical Biology 3Document42 pagesMedical Biology 3Malik MohamedNo ratings yet
- NVBSP Form15Document6 pagesNVBSP Form15Rhodz Caballes RefuerzoNo ratings yet
- L01 Obs. - History - Dr.a.rahim 2021 2022Document5 pagesL01 Obs. - History - Dr.a.rahim 2021 2022salmaNo ratings yet
- Renal Exam Class TestDocument8 pagesRenal Exam Class Test1fleetingNo ratings yet
- Substance-Related Disorders: Ms. Jocelyn Alcera Nazario, RN MANDocument149 pagesSubstance-Related Disorders: Ms. Jocelyn Alcera Nazario, RN MAN102680No ratings yet
- StudentsDocument756 pagesStudentsxxx xNo ratings yet
- Three Cases of Chronic Suppurative Otitis Media (CSOM) Caused by Kerstersia Gyiorum and A Review of The LiteratureDocument6 pagesThree Cases of Chronic Suppurative Otitis Media (CSOM) Caused by Kerstersia Gyiorum and A Review of The LiteraturealdaNo ratings yet
- Jerome Cauthen V3 PCDocument4 pagesJerome Cauthen V3 PCSammy ChegeNo ratings yet
- Prelim ProgrammeDocument7 pagesPrelim Programmeasalizwa ludlalaNo ratings yet
- PDF Tablet Lepas LambatDocument13 pagesPDF Tablet Lepas Lambatannisya bubblesNo ratings yet
- Tay-Sachs Disease I. What Is Tay-Sachs Disease?Document2 pagesTay-Sachs Disease I. What Is Tay-Sachs Disease?DBA MurialdoNo ratings yet
- VAERS Report Details Deaths and Adverse Events Following COVID VaccinesDocument234 pagesVAERS Report Details Deaths and Adverse Events Following COVID VaccinesbeneNo ratings yet
- Crohn's Disease Case Study: Matt SimsDocument14 pagesCrohn's Disease Case Study: Matt SimsKipchirchir AbednegoNo ratings yet
- Bipolar Affective Disorder: Captain DR Yujal Man Singh Neuropsychiatrist, Shree Birendra HospitalDocument15 pagesBipolar Affective Disorder: Captain DR Yujal Man Singh Neuropsychiatrist, Shree Birendra HospitalYujal Man SinghNo ratings yet
- Case Presentation-Nasopharyngeal CarcinomaDocument18 pagesCase Presentation-Nasopharyngeal Carcinomatehkie04100% (3)
- Dbs VnsDocument22 pagesDbs Vnswen tvaleNo ratings yet
- Horner Syndrome: DescriptionDocument3 pagesHorner Syndrome: DescriptionMeike WinataNo ratings yet
- IDSA Molnupiravir GuidelineDocument10 pagesIDSA Molnupiravir GuidelineJaz ButuyanNo ratings yet
- A Laser Peripheral Iridotomy Would Most Likely Relieve AngleDocument2 pagesA Laser Peripheral Iridotomy Would Most Likely Relieve AngleGlaucoma UnhasNo ratings yet