Professional Documents
Culture Documents
Breman - 2001 - The Ears of The Hippopotamus - Manifestations - Determinants and Estimates of The Malaria Burden
Uploaded by
xxongh1Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Breman - 2001 - The Ears of The Hippopotamus - Manifestations - Determinants and Estimates of The Malaria Burden
Uploaded by
xxongh1Copyright:
Available Formats
Am. J. Trop. Med. Hyg., 64(1, 2)S, 2001, pp.
111
Copyright 2001 by The American Society of Tropical Medicine and Hygiene
THE EARS OF THE HIPPOPOTAMUS: MANIFESTATIONS, DETERMINANTS, AND
ESTIMATES OF THE MALARIA BURDEN
JOEL G. BREMAN
Fogarty International Center, National Institutes of Health, Bethesda, Maryland
Abstract. Malarious patients experience asymptomatic parasitemia; acute febrile illness (with cerebral damage,
anemia, respiratory distress, hypoglycemia); chronic debilitation (anemia, malnutrition, nervous systemrelated sequelae); and complications of pregnancy (anemia, low birth weight, increased infant mortality). These manifestations
in patients, communities, and countries reflect intrinsic (human, parasite, mosquito) and extrinsic (environmental,
social, behavioral, political, and economic conditions as well as disease-control efforts) determinants. At a minimum,
between 700,000 and 2.7 million persons die yearly from malaria, over 75% of them African children. Between 400
and 900 million acute febrile episodes occur yearly in African children under 5 yr of age living in endemic areas.
Although about half of these children are parasitemic, all merit consideration of malaria-specific therapy, which is
becoming more problematic because of parasite resistance to drugs. These numbers will more than double over the
next 20 yr without effective control. Fewer than 20% of these febrile episodes and deaths come to the attention of
any formal health system. The relatively few ill patients who have any contact with the health services represent the
ears of the hippopotamus. Greatly intensified research activities and control of the intolerable burden of malaria
are mandatory if economic development is to accelerate in Africa. In particular, support should be targeted to understanding and preventing malaria-induced anemia, hypoglycemia, effects on pregnancy, and neurologic and developmental impairment. To decrease and stop transmission of this intolerable scourge, there is an urgent need for
malaria vaccines, newer drugs, and better vector control methods as well as the ability to improve current technologies
and use them more efficiently.
INTRODUCTION
MANIFESTATIONS OF MALARIA
The burden of malaria is a challenge to quantify because
infection may be asymptomatic in partially immune persons,
may manifest in acute catastrophic cerebral illness and death
or permanent neurologic sequelae, or may appear in gradations between these clinical extremes. Many febrile illnesses
in endemic areas mimic malaria, and confirmatory parasitologic diagnosis is not often available, reliable, or prompt,
particularly in rural zones. Parasitemic patients can have other illnesses, complicating matters even more. Most important, case detection and reporting are woefully incomplete
because of the poor state of surveillance in malarious countries. This situation, whereby very little disease is perceived
or managed by health systems in the tropics, is analogous to
a hippopotamus floating in deep water, with only the ears
showing; the largest and most dangerous part of the beast
rests below the water.
With the recent increased support for malaria research and
control worldwide, particularly in Africa, it is urgent that
there be more precise definition of malarias clinical, epidemiologic, and economic burden. A recent review has concluded once again that about 1 million deaths (range,
744,0001,300,000) from the direct effects of malaria occur
yearly in Africa, more than 75% of them in children.1 This
burden is determined by a wide variety of factors and is
expressed in several clinical and epidemiologic forms, many
of which are not usually considered in calculations of the
malaria toll. This article will give an overview of the manifestations, important determinants, and estimates of the burden that dominate thinking about malarias impact as we
attempt to understand, control, and prevent this scourge early
in the 21st century. It will preface a series of articles that
address specific expressions of the malaria burden, many of
which have been lamentably neglected.
Malaria is defined variably as acute febrile illness in endemic areas, with or without parasitemia, depending upon
local capability for parasitologic confirmation. Malaria infection can result in asymptomatic parasitemia; clinical malaria (febrile episodes, parasitemia); severe malaria (anemia,
neurologic syndromes); and mortality.2 The major manifestations of acute febrile illness, chronic effects, and pregnancy-related complications are shown in Figure 1.320 Acute
severe illness can lead to cerebral malaria, with a high case
fatality rate.36 Coma, severe anemia, and respiratory distress
are ominous for children with acute malaria. One perilous
but eminently treatable complication of malaria is hypoglycemia due to parasite metabolism in red blood cells (RBCs)
and hyperinsulinemia secondary to use of quinine;7,8 pregnant women with malaria have a high risk of hypoglycemia.
Even when patients get to a hospital, differing malaria treatment regimens result in different outcomes in the hospital
and after discharge.910 The debilitating acute and chronic
effects of anemia and neurologic, cognitive, and developmental impairment are not well quantified.1116 Particularly
devastating to development are the long-duration effects of
malaria, manifested in learning and behavioral disorders and
decreased capacity to work.14,15 The extent of the impact of
malaria on the pregnant woman and her fetus, notable during
the first and second pregnancies, have only recently been
appreciated.1720 In particular, low birth weight and subsequent increased infant and childhood mortality result from
an infected placenta.21,22 The economic devastation caused
by malaria reflects health care costs, lost workdays and
schooldays by patients and family members, and other direct
and indirect costs.2325 Retardation of the rate of long-term
national, regional, and continental economic growth as a
consequence of malaria has been appreciated only recently.26
Biologic, genetic, immunologic, and pathophysiologic
BREMAN
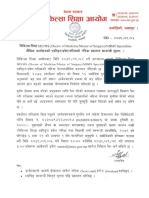
FIGURE 1.
Manifestations of the malaria burden.
mechanisms predisposing malarious patients to severe disease are beginning to be understood more completely. Tumor
necrosis factor, cytoadhesion of parasitized RBCs (particularly in cerebral vessels), nitric oxide, lactic acidosis, and
chondroitin sulfate A in the placenta are associated with adverse effects of malaria.27,28 The local epidemiologic profile
of malaria and other diseases is very important for diagnosing and quantifying accurately the cause of febrile illness.29
In areas with unstable malaria, the predictive values (positive
and negative) of fever will vary, depending upon season and
other prevalent diseases.3037 Hence, to manage patients
properly, particularly ill febrile children, it is necessary to
have a comprehensive understanding of the local pathology
and epidemiology.
DETERMINANTS OF THE MALARIA BURDEN
The manifestations of malaria in patients and the toll in
communities and countries reflect intrinsic and extrinsic determinants (Table 1). Of the intrinsic factors, host (human)
immunity, parasite species, anopheline longevity, and avidity
for humans have the greatest impact on the malaria burden.38
Among extrinsic factors, climate (mainly rainfall), economic
conditions (poverty), political commitment, and effectiveness of control and prevention efforts are the most important
determinants of malarias burden (Figure 2).
Host factors. Human populations exposed to malaria infection may vary in their susceptibility to infection and severity of illness. Sickle cell (AS) and other traits that alter
RBC structure limit parasite multiplication within RBCs.
The protection of populations by their genetic makeup is
termed balanced polymorphism, a concept strengthened by
the observation that the heterozygous (AS) trait is more
prevalent in African populations and may protect against
malaria, particularly cerebral malaria.39 The presence of the
Duffy blood factor on the surface of RBCs is required for
Plasmodium vivax to enter RBCs; because over 90% of sub-
Saharan Africans lack the Duffy factor, P. vivax is essentially absent from most of this area.40 Hereditary ovalocytosis, and thalassemia, glucose-6-phosphate dehydrogenase deficiency, spectrin, Lewis and Kid Is (a) red cell type
mutations in the gene for the red blood cell membrane protein and have also been associated with decreased susceptibility to severe malaria.41 A low frequency of the class I
major histocompatibility complex molecule HLA-B53 has
been associated with severe malaria in the Gambia, possibly
associated with immunity to liver stages of the parasite.42,43
Other innate factors, such as ICAM-1, the putative receptor
for infected RBCs binding to brain endothelium, and a polymorphism in the promoter region of tumor necrosis factor-
appear related to the frequency of severe disease.44,45 Although knowledge of host and parasite genetics has added
greatly to our understanding of susceptibility to malaria, the
use of genotype information for improved malaria treatments
and prevention remains a challenge for the future.
The immune status of the individual and population plays
the most important role in the clinical response to infection
and transmission. Maternally derived antibody offers limited
and short-duration protection to the newborn.46 In heavily
endemic areas, over 30% of children acquire parasites by 3
months of age.47 Researchers have identified humoral antibodies to sporozoites, intrahepatic parasites, merozoites, malaria toxins, parasite antigens on infected RBCs, intraerythrocytic parasites, and, within the mosquito, to parasite fertilization; cell-mediated immunity plays a role in the liver
and RBC invasion and parasite development.48 Even with
repeated infection, protective immunity is incomplete; individuals in malarious areas frequently have premunition, i.e.,
parasitemia and antibodies without symptoms, and this is age
dependent. There is recent evidence for a genetic basis for
antibody and cellular responses to malaria proteins.49,50 Identification of specific immunologic determinants of protection
will lead to development of the most promising vaccine candidates, including multistage vaccines.
THE MALARIA BURDEN
TABLE 1
Determinants of the malaria burden
Determinant
Genetic susceptibility
Sickle cell trait (AS), hereditary ovalocytosis
thalassemia, HbE, fetal Hb,
glucose-6-phosphate dehydrogenase deficiency, major
histocompatibility antigens
HLA-B53
Duffy blood factor
Effect
Limit parasite invasion/growth
in red blood cells (RBCs)
Protect against severe disease
Surface receptor needed for
Plasmodium vivax entry into
RBC
Immunologic status
Major histocompatibility antigen
ICAM-1
Absence on infected RBCs
limits T-cell recognition
Infected RBC receptor, binds
to brain endothelium, cerebral malaria
Tumor necrosis factor polymor- Linked to severe disease
phism
Nave mother
Susceptible newborn
Residence in area of no or un- Nave/incompletely protected
stable transmission
population
Residence in area of stable
Premunition, partial protection
transmission
Parasite
Plasmodium falciparum
P. vivax, Plasmodium ovale
Plasmodium malariae
Antigenic diversity
Resistance to drugs: P. falciparum (widespread); P. vivax
(reports from Asia, South
America)
Mosquito
Anopheles gambiae complex
High entomologic inoculation
rate
Resistance to insecticides
Environmental
Warm temperatures, high rainfall and humidity
Clear, still, sun-exposed water
collections
Engineering projects: dams,
roads
TABLE 1
Continued
Severe illness
Relapses
Nephrotic syndrome, recrudescence
New infections, not recrudescence
Inadequate patient management
and increased burden
Most efficient vector, widespread in Africa
Stable intense transmission and
severe disease in susceptibles
Transmission maintained and
increased burden
Determinant
Interventions
Policies, strategies and tactics
well-defined
Sufficient infrastructure
Good training, implementation
and evaluation
Drugs, insecticides and bed
nets available and effective
Adequate financing
Effect
Good program conception and
implementation
Ability to provide services
Ability to maintain effective
program
Services effective
Control and prevention
Parasite. Of the 4 species of plasmodia affecting humans,
Plasmodium falciparum, the most recently evolved species,
is the most virulent, for reasons incompletely understood.51
Although P. vivax, which can cause relapses months after
an infection, is widespread in Central and South America
and Asia, it causes substantial morbidity but fewer severe
complications; recently, low birth weight was reported with
placental infection by P. vivax,52,53 a well-established result
of P. falciparum infection.1720 Plasmodium malariae is associated with renal complications;54 if untreated, patients
may remain parasitemic and asymptomatic for years. Plasmodium ovale, also a relapsing species, is a rare ( 0.5%)
cause of infection; it is found principally in Africa. Evidence
is accruing that genetic diversity of parasites is frequent
within species, patients, and localities, probably because of
recombination and selection, and has an impact on clinical
presentation in various age groups and on malaria transmission.55,56 This may account for the lack of protective immunity and the frequent repeat infections and clinical episodes of malaria in persons, particularly young children, living in areas of intense and stable transmission, and it must
be considered in the development of vaccines.
The development of P. falciparum resistance to drugs over
the past 20 yr has been a major cause of poor malaria pro-
Increased mosquito longevity
Good vector breeding sites
New breeding sites, humanmade malaria
Education, social, behavioral, political, and economic
Illiteracy and poor knowledge
Uninformed, ineffective particiof disease cause, transmispation in control and prevension, and control
tion
Community participation
Necessary for proper prevention and control
Urbanization, economic oppor- Urban malaria
tunity
Natural disasters, civil and mil- Refugee movements to malariitary disruption
ous areas
Poverty
Inability to obtain and deploy
drugs, insecticides, bed nets,
and other measures
Political, economic commitReflects high priority, spirit of
ment
success
FIGURE 2.
Intrinsic and extrinsic factors linked to the malaria toll.
BREMAN
FIGURE 3.
Control of the malaria burden: current and future interventions.
gram performance and increasing burden; resistance to chloroquine is widespread, multidrug resistance is increasing,
and new strategies are being developed for their use.5760
Since 1980, following the demise of global malaria eradication, use of effective drugs to reduce mortality and morbidity has been the major strategy for malaria control, particularly in Africa.61 The increasing malaria burden reflects
the inadequacy of this current strategy, which may become
further compromised by the projected increasingly widespread use of sulfamethoxazole-trimethoprim as prophylaxis
for patients with human immunodeficiency virus and acquired immune deficiency syndrome.62 Resistance to sulfamethoxazole-trimethoprim may cross-react with a major antimalarial drug and vice versa.63 This would have ominous
implications, because sulfadoxine-pyrimethamine is becoming a cost-effective first-line therapy in eastern and southern
Africa.64
Mosquito. Although there are about 400 species of
Anopheles, only 60 of them transmit malaria under natural
conditions, and only 30 are of major importance.65 Of these,
the Anopheles gambiae complex and Anopheles funestus are
the most efficient vectors for P. falciparum transmission; the
highest rates of sporozoite development are in An. gambiae,
the species that is widespread throughout tropical Africa. Of
all factors related to malaria transmission, apart from host
immunity, the number (density), human-biting habits, and
longevity of anopheline mosquito vectors are the most important. Transmission is directly proportional to the density
of the vector, the square of the number of human bites per
day per mosquito, and the 10th power of the probability of
the mosquitos surviving for 1 d.38,65 Mosquito longevity is
particularly important, because the portion of the parasites
life cycle that takes place within the mosquitofrom gametocyte ingestion to subsequent inoculationcan take
from 8 to 30 d, depending on ambient temperature. In general, sporogony within the mosquito is not completed at temperatures below 1618C, and transmission does not occur.
The entomologic inoculation rate (EIR)the number of spo-
rozoite-positive mosquito bites per yearis the most common measure of malarial transmission; this varies from 1
in some parts of Latin America and Southeast Asia to 300
in parts of tropical Africa. The relation between level of
exposure (the EIR) and the incidence of severe malaria and
death remains controversial. A high EIR results in stable and
intense transmission, with young children the most vulnerable for severe illness. Higher EIRs are, in general, associated with increased frequency and density of parasitemia,
febrile episodes, anemia and cerebral malaria in heavily endemic areas.6669 The lower the EIR, the greater the number
of susceptible individuals who can develop severe infection
and illness.68,69
Because the health service delivery systems have been so
poor for malaria control and other diseases, vector control
has had limited success in heavily endemic countries, especially in Africa; indeed, outside of a few urban centers and
research projects, vector control has not been a major strategy, with the exception of a few areas in southern Africa.
There is increasing interest in attacking the mosquito both
with classical vector control technologies to prevent and
control epidemics and with insecticide-impregnated bed nets
and other materials for personal protection.7075 With the realization that the current drug-use strategy alone will have a
minimal impact on transmission and limited success in decreasing the malaria burden, newer vector-focused approaches are needed.
Environmental. Tropical areas with warm temperatures,
heavy rainfall, and high humidity are conducive to mosquito
breeding and longevity and parasite sporogony. An. gambiae
mosquitoes breed readily in large and small collections of
sun-exposed still water, such as exist throughout tropical Africa. Human engineering projects, e.g., construction of dams,
roads, and industrial and residential centers, can result in
disruption of the terrain, allowing increased mosquito breeding. Geographic areas where populations are susceptible to
epidemics are of particular importance; these zones are often
inundated by unseasonal rains, influxes of migrants and ref-
THE MALARIA BURDEN
FIGURE 4.
Estimated world and regional malaria cases, 19871999.
ugees, and breakdowns of malaria and other disease control
and prevention programs. Epidemics linked to rainfall, temperature, geography, and, above all, population susceptibility
and unresponsiveness to incipient epidemics will become
more frequent.7678 Recent mapping of malarious zones by
endemicity and epidemic risk can help prevent medically
catastrophic and disruptive malaria epidemics if realistic program objectives and indicators for action are established, periodic monitoring and supervision occur, and corrective steps
FIGURE 5.
are taken promptly when gaps are found.7982 The rapid trend
toward urbanization in developing countries will bring more
malaria to large cities and will expose susceptible populations to outbreaks.83 Measures to prevent malaria can be easier to implement and more cost-effective in urban and perurban areas than in rural zones.
Social, behavioral, political, and economic. Over the
past 100 yr there has been a decrease in malaria transmission
in northern countries, including those with tropical areas,
Estimated world and regional malaria deaths, 19521999.
BREMAN
FIGURE 6.
The Ears of the Hippopotamus where malaria patients are managed . . . and die.
following an improvement in education and in social and
economic conditions. The improvement of general hygiene
and public health included the filling in of swamps, elimination of open drainage ditches and other mosquito breeding
sites, screening of windows and doors, widespread use of
air conditioning, and availability of rapid diagnosis and
drugs for acute illness. Alleviation of poverty has been associated with a decrease in malaria endemicity. Economic
and educational gains, along with the ability to manufacture,
purchase, and deploy effectively DDT and other insecticides,
may have had the greatest impact on the malaria burden in
temperate zones.84,85 In some African countries, no associa-
tion was seen recently between socioeconomic status (SES)
and severe malaria, anemia, and reinfection.86,87 Here, the
SES may not reflect access to or use of malarial control or
prevention measures or may reflect the relative ineffectiveness of those employed. Knowledge of which malaria control strategies and interventions are most cost-effective is
needed because of the huge economic and medical toll of
malaria. Recent attention given to malaria by the presidents
of several African countries and by the leaders of northern
countries has been very gratifying and, one hopes, reflects
the political, financial, and other support for research and
operations that must continue to be forthcoming.88
FIGURE 7. Number and projected number of acute febrile episodes and malaria-associated febrile episodes in African children under 5 yr
of age living in endemic areas, 19952020.
THE MALARIA BURDEN
Interventions. The current malaria control and prevention
measures include personal protection, drug use, and vector
control strategies (Figure 3). The correct and timely application of these strategies can result in decreases in malariaspecific and overall mortality, but this is difficult to achieve
and sustain.61,8991 Experience in Sri Lanka during eradication
activities in the 1960s and 1970s showed that malaria can
resurge in epidemic form rapidly, even when transmission is
almost interrupted, if priorities change, field operations falter, and maintenance activities and resources are inadequate
or diverted.92
Because of the gaps in these strategies, difficulties in
mounting and maintaining effective operational activities,
and the peril of increasing parasite resistance to drugs and
insect resistance to insecticides, establishment of a sound
malaria research base, particularly in endemic countries, is
essential; the focus is now on developing 1 or more vaccines
against malaria and on developing genetically altered anophelines unable to complete the sporogonic cycle.48,93 Development of new prevention and control tools requires greatly
increasing the research and capacity of institutions in malarious areas and of partner institutions in the North.94 It is
expected that opportunities offered by, and collaboration between, the Multilateral Initiative on Malaria (MIM), the
Tropical Diseases Research and Training Program (TDR)/
World Health Organization (WHO), Wellcome Trust, Roll
Back Malaria/WHO, and other agencies, coupled with increasing private-sector interest and commitment, will accelerate new discoveries, their translation into interventions,
and their deployment operationally.
ESTIMATING THE BURDEN
Worldwide estimates of the number of patients with acute
febrile illness due to malaria have varied from 10 to 500
million annually.1,61,95101 These estimates are imprecise, misleading, and low because of inadequate diagnosis and incomplete reporting. Some authors have tried to approximate
the number of febrile patients who might be parasitemic, an
exercise that is difficult and has limited operational importance in malarious areas without diagnostic capacity. Others
have designated 5,00010,000 parasites/L or another
threshold level for a malaria diagnosis in partially immune
patients living in endemic areas, a criterion that has some
epidemiological but no clinical relevance. It is paradoxical
and regrettable that for many years Africa was not included
in WHO reporting of malaria morbidity and mortality because of poor surveillance and lack of parasitologic diagnosis, yet there is universal agreement that close to 90% of
cases globally occur in Africa (Figure 4), and virtually all
are caused by P. falciparum. Early estimations of African
malaria deaths were based on the autopsy study by BruceChwatt in Lagos, Nigeria;46 he concluded that approximately
1 million African children died from malaria each year. Recent, more precise estimations of malaria mortality have remained surprisingly close to this number, varying between
700,000 and 2.7 million, with well over 75% of deaths occurring in African children (Figure 5). It has not been appreciated that malaria-related anemia, hypoglycemia, respiratory distress, low birth weight, and other manifestations
are not usually included in defining the burden, and includ-
ing these may double the current estimates. Indeed, anemia
and low birth weight may contribute to 50% of the overall
malaria morbidity and mortality in children under 5 yr of
age in Africa.102,103 The acute and repeated effects of malaria
on the brain and their sequelae remain to be quantified fully.
International and bilateral organizations (including WHO,
the United Nations Childrens Fund [UNICEF], and the U.S.
Agency for International Development [USAID]) and public
health staff in malarious countries have advised that all febrile children under 5 yr of age in endemic areas be treated
for malaria. Home treatment is encouraged initially because
of the potential severe consequences of untreated illness, the
lack of precise diagnosis, and the relative inaccessibility of
secondary and tertiary health care facilities. Most febrile
persons do not come to the attention of the formal health
infrastructure.1,61,104106 The ears of the hippopotamus represent the fewer than 20% of patients who have any contact
with the formal health delivery service when they become
ill and die (Figure 6). The number of the most potentially
severe malaria episodes can be approximated using the number of young pediatric febrile episodes reported by parents
during field surveys in rural and urban endemic areas: these
vary generally from 4 to 9 per year in children under 5 yr
of age.61,106 Using this information, between 400 and 900
million febrile episodes would have occurred annually in
children less than 5 yr of age living in endemic areas in
Africa at the end of the 20th century; without effective interventions, by 2020 these numbers will have at least doubled (Figure 7). If 3060% of these children were parasitemic, as reported in some studies, about half would have true
malaria (200450 million annually).37,104,107 In many areas,
the parasitemia rate for children is higher, particularly during
and just after the rainy season. These numbers do not consider febrile episodes and malaria infections in older children
and adults in Africa and in endemic areas of the Americas
and Asia. These older groups in Africa have between 0.4
and 1 episode of malaria yearly and probably 2 or more
febrile episodes.1 Taking these older age groups and other
continents into consideration, it is highly likely that worldwide well over 2 billion febrile episodes resembling malaria
occur annually and that a substantial portion are parasitemic,
meriting effective treatment.
DISCUSSION
Malaria will be tamed only when its manifestations and
determinants are understood more completely where the
infection and disease have special epidemiologic and clinical profiles and when current and more efficacious control measures are applied more effectively. Study of the
intrinsic factorsin particular the genetic profiles of the
human host, parasite, and mosquito and their interrelationshipswill open new avenues for development of improved and new interventions. Relatively little can be
done now to enhance innate or acquired resistance to malaria, although more effective management of hospitalized
patients susceptible to severe or cerebral malaria might
occur by use of cytokines and, ultimately, vaccines. Parasites and mosquitoes are the main targets of current and
future interventions. Recent discoveries that plasmodial
infections are antigenically heterogeneous complicate at-
BREMAN
tempts to develop an effective blood-stage vaccine, but at
least 1 group has produced a multiantigenic construct.106
The geographic spread and intensity of multidrug-resistant
P. falciparum is ominous and mandates the development
of newer drugs and trials of drug combinations.60 Improved understanding of the genetic and biologic basis of
parasite resistance to antimalarial drugs is leading to newer diagnostic approaches.
An attack on the mosquitoby insecticide-impregnated
personal protection material (bed nets)is the main new
approach to malaria control, one that results in decreasing
overall mortality.75 This approach has the advantage of involving individuals, families, and communities in decision
making and implementation. Whether long-term use of
such materials will achieve the 50% decrease in malariarelated mortality and morbidity within 10 yrthe goal of
the WHO Roll Back Malariaremains to be seen.109111 Renewed effort in understanding Anopheles biology and ecology may lead to an original intervention that will prevent
parasite maturation in and transmission by the mosquito.
The recent sequencing of chromosome 2 of 1 isolate of
P. falciparum offers promise of increased understanding of
the function of specific genes within the parasite and sites
for newer drugs and vaccines;112114 of note is the recent
finding that a single gene in P. falciparum confers chloroquine resistance.114 Awaited with urgency is the development and field testing of the more effective antimalaria
drugs, vaccines, and vector control methods that will certainly follow these new discoveries. At the same time, more
effective and efficient health care delivery systems need to
be developed to uncover and treat more of the hippopotamus than is seen currently. Although falciparum malaria
certainly merits our full and immediate preoccupation, the
important burden of illness caused by P. vivax, as well as
the ill-defined effects of P. malariae and P. ovale, need
further attention, as does their control.115
To better confront and solve the considerable malaria research and operational challenges, an increased number of
well-trained and active scientists and institutions in the South
and North are joining the effort. The MIM is a coalition of
scientists and institutions in Africa and developed countries
that aims to strengthen and sustain through collaborative
research and training, the capability of malaria endemic
countries in Africa to carry out research required to develop
and improve tools for malaria control.116 To achieve the
needed critical mass of malariologists in Africa and elsewhere and to achieve mastery over malaria, the MIM, Roll
Back Malaria, and similar programs must be nurtured and
strengthened.
Acknowledgments: I thank Drs. Louis Miller, Robert Snow, and
Kenneth Bridbord for constructive comments; Mr. Sean Murphy and
Ms. Kathleen Deren-Bernocchi for review of morbidity and mortality data; and Ms. Melanie Rouse for manuscript assistance.
Authors address: Joel G. Breman, Fogarty International Center, National Institutes of Health, Building 31, Room B2C39, 31 Center
Drive, MSC 2220, Bethesda, MD 20892-2220, Telephone: 301-4961653, Fax: 301-402-0779 (e-mail: jbreman@nih.gov).
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
REFERENCES
1. Snow RW, Craig M, Deichmann U, Marsh K, 1999. Estimating
mortality, morbidity, and disability due to malaria among Af-
ricas non-pregnant population. Bull World Health Organ 77:
624640.
White NJ, Breman JG, 2001. Malaria and babesiosis caused
by red blood cell parasites. Braunwald E, Fauci AS, Kasper
DL, Hauser SL, Longo DL, Jameson JL, eds. Harrisons Principles of Internal Medicine. Fifteenth edition. New York: McGraw-Hill, 120313.
World Health Organization, 2000. Severe and complicated malaria. Trans R Soc Trop Med Hyg 94(suppl): 5190.
Molyneux ME, Taylor TE, Wirima JJ, Borgstein A, 1989. Clinical features and prognostic indicators in paediatric cerebral
malaria: a study of 131 comatose Malawian children. Q J Med
71: 441459.
Marsh K, Forster D, Wariuru C, Mwangi I, Winstanley M,
Marsh V, Newton C, Winstanley P, Warn P, Peshu N, Pasvol
G, Snow R, 1995. Indicators of life-threatening malaria in
African children. N Engl J Med 332: 13991404.
Waller D, Krishna S, Crawley J, Miller K, Nosten F, Chapman
D, ter Kuile OF, Craddock C, Berry C, Holloway PA, Brewster D, Greenwood BM, White NJ, 1995. Clinical features and
outcome of severe malaria in Gambian children. Clin Infect
Dis 21: 577587.
White NJ, Miller KD, Marsh K, Berry CD, Turner RC, Williamson DH, Brown J, 1987. Hypoglycemia in African children with severe malaria. Lancet 1: 708711.
Krishna S, Waller DW, ter Kuile F, Kwiatkowski D, Crawley
J, Craddock CF, Nosten F, Chapman D, Brewster D, Holloway
PA, White NJ, 1994. Lactic acidosis and hypoglycemia in
children with severe malaria: pathophysiological and prognostic significance. Trans R Soc Trop Med Hyg 88: 67.
Zucker J, Lackritz EM, Ruebush TK II, Hightower AW, Adungosi JE, Were JB, Metchok B, Patrick E, Campbell CC, 1996.
Childhood mortality during and after hospitalization in western Kenya: effect of malaria treatment regimens. Am J Trop
Med Hyg 55: 655660.
Lackritz EM, Campbell CC, Ruebush TK II, Hightower AW,
Wakube W, Steketee RW, Were JB, 1992. Effect of blood
transfusions on survival among children in a Kenyan hospital.
Lancet 340: 524528.
Slutsker L, Taylor TE, Wirima J, Steketee RW, 1994. In-hospital morbidity and mortality due to malaria due to malariaassociated severe anaemia in two areas of Malawi with different patterns of malaria infection. Trans R Soc Trop Med
Hyg 88: 548551.
Newton CR, Warn CR, Warn PA, Peshu N, Snow RW, Pasvol
G, Marsh K, 1997. Severe anaemia in children living in a
malaria endemic area of Kenya. Trop Med Int Health 2: 165
178.
Brewster DR, Kwiatkowski D, White NJ, 1990. Neurological
sequelae of cerebral malaria in children. Lancet 330: 1039
1043.
Van Hensbroek MB, Palmer A, Jaffar S, Schneider G, Kwiatkowski D, 1997. Residual neurologic sequelae after childhood
cerebral malaria. J Pediatr 131: 125129.
Verity C, Greenwood R, Golding J, 1998. Long-term intellectual and behavioral outcomes of children with febrile convulsions. N Engl J Med 338: 17231728.
Holding PA, Stevenson J, Peshu N, Marsh K, 1999. Cognitive
sequelae of severe malaria with impaired consciousness.
Trans R Soc Trop Med Hyg 93: 529534.
McGregor IA, Wilson ME, Billewicz WZ, 1983. Malaria infection of the placenta in the Gambia, West Africa: its incidence and relationship to still birth, birth weight and placental
weight. Trans R Soc Trop Med Hyg 77: 232244.
Brabin B, 1983. An analysis of malaria in pregnancy in Africa.
Bull World Health Organ 61: 10051016.
McCormick M, 1985. The contribution of low birth weight to
infant mortality and childhood morbidity. New Engl J Med
312: 8290.
Steketee R, Wirima JJ, Hightower AW, Slutsker L, Heymann
DL, Breman JG, 1996. The effect of malaria and malaria prevention in pregnancy on offspring birthweight, prematurity,
and intrauterine growth retardation in rural Malawi. Am J
Trop Med Hyg 55(suppl): 3341.
THE MALARIA BURDEN
21. Bloland P, Slutsker L, Steketee RW, Wirima JJ, Heymann DL,
Breman JG, 1996. Rates and risk factors for mortality during
the first two years of life in rural Malawi. Am J Trop Med
Hyg 55(suppl): 8286.
22. Slutsker L, Bloland P, Steketee RW, Wirima JJ, Heymann DL,
Breman JG, 1996. Infant and second-year mortality in rural
Malawi: causes and descriptive epidemiology. Am J Trop Med
Hyg 55(suppl): 7781.
23. Conly GN, 1975. The Impact of Malaria on Economic Development. A Case Study. Washington, DC: Pan American
Health Organization.
24. Mills A, 1991. The economics of malaria control. Targett GAT,
ed. Malaria: Waiting for the Vaccine. New York: John Wiley
and Sons, 141165.
25. Shephard DS, Ettling MB, Brinkmann V, Saurborn R, 1991.
The economic cost of malaria in Africa. Trop Med Parasitol
42: 199203.
26. Gallup JL, Sachs JD, 2001. The economic burden of malaria.
Am J Trop Med Hyg 64(suppl 1): 8496.
27. Kremsner PG, Winker S, Wilding E, Prada J, Bienzle U, Graninger W, Nussler AK, 1996. High levels of nitrogen oxides
are associated with severe disease and correlate with rapid
parasitological and clinical cure in Plasmodium falciparum
malaria. Trans R Soc Trop Med Hyg 90: 4447.
28. Fried M, Duffy PE, 1996. Adherence of Plasmodium falciparum to chondroitin sulfate A in the human placenta. Science
272: 1502.
29. Rougemont A, Breslow N, Brenner E, Moret AL, Doumbo O,
Dolo A, Soula G, Perrin L, 1991. Epidemiological basis for
clinical diagnosis of childhood malaria in endemic zone in
West Africa. Lancet 338: 12921295.
30. Gove S, Tamburlini G, Molyneux E, Whitesell P, Campbell H,
1999. Development and simplified guidelines for emergency
triage assessment and treatment in developing countries.
WHO integrated management of childhood illness (IMCI referral care project.) Arch Dis Child 81: 473477.
31. Zucker-Perkins BA, Zucker JR, Otieno J, Jafari HS, Paxton L,
Redd SC, Nahlen BL, Schwartz B, Oloo AJ, Olango C, Gove
S, Campbell CC, 1997. Evaluation of an algorithm for integrated management of childhood illness in an area of Kenya
with high malaria transmission. Bull World Health Organ
74(suppl): 3342.
32. Delfini LF, 1973. The relationship between body temperature
and malaria parasitemia in rural forest areas of western Nigeria. J Trop Med Hyg 76: 111114.
33. Trape JF, Peelman P, Morault-Peelman B, 1985. Criteria for
diagnosing clinical malaria among semi-immune populations
exposed to intense and perennial transmission. Trans R Soc
Trop Med Hyg 79: 435442.
34. Trape JF, Zoulani A, Quintet MC, 1987. Assessment of the
incidence and prevalence of clinical malaria in semi-immune
children exposed to intense and perennial transmission. Am J
Epidemiol 126: 193202.
35. Greenwood BM, Marsh K, Snow RW, 1991. Why do some
African children develop severe malaria? Parasitol Today:
277281.
36. Gbadegesin RA, Sodeine O, Adeyemo AA, Adewowo OG,
1997. Body temperature is a poor predictor of malaria parasitemia in children with acute diarrhea. Ann Trop Paediatrics
17: 8994.
37. Paluku KM, Breman JG, Moore M, Ngimbi NP, Sexton JD,
Roy J, Steketee RW, Weinman JM, Kalisa-Ruti, 1988. Response of children with Plasmodium falciparum to chloroquine and development of a national malaria treatment policy
in Zaire. Trans R Soc Trop Med Hyg 82: 353357.
38. Molineaux L, 1988. The epidemiology of human malaria as an
expression of its distribution including some implications for
its control. Wernsdorfer WH, McGregor IA, eds. Malaria,
Principles and Practice of Malariology. Vol 2. London: Churchill Livingston, 913998.
39. Allison AC, 1954. Protection afforded by sickle cell trait
against subtertian malaria infection. Br Med J: 290294.
40. Miller LH, Mason SJ, Clyde DF, McGinnis MH, 1976. The
resistance factor to Plasmodium vivax in blacks: the Duffy
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
blood group genotype, Fy-Fy. New Engl J Med 295: 302
304.
Luzzatto L, 1979. Genetics of red cells and susceptibility to
malaria. Blood 54: 961976.
Hill AVS, Allsopp CE, Kwiatkowski D, Anstey NM, Twumasi
P, Rowe PA, Bennett S, Brewster D, McMichael A, Greenwood BM, 1991. Common West African HLA antigens are
associated with protection from severe malaria. Nature 352:
595600.
Hill AVS, Elvin J, Willis AC, Aidoo M, Allsopp CE, Gotch
FM, Gao XM, Takiguchi M, Greenwood BM, Townsend AR,
McMichael AJ, Whittle HC, 1992. Molecular analysis of the
association of HLA-B53 and resistance to severe malaria. Nature 360: 434439.
Fernandez-Reyes D, Craig AG, Kyes SA, Peshu N, Snow RW,
Berendt AR, Marsh K, Newbold CI, 1997. A high-frequency
African coding polymorphism in the N-terminal domain of
ICAM-1 predisposing to cerebral malaria in Kenya. Human
Mol Genetics 6: 13571360.
McGuire W, Hill AVS, Allsopp CEM, Greenwood BM, Kwiatkowski D, 1994. Variation in the TNF promoter region associated with susceptibility to cerebral malaria. Nature 371:
508510.
Bruce-Chwatt LJ, 1952. Malaria in African infants and children in southern Nigeria. Ann Trop Med Parasitol 46: 173
200.
Slutsker L, Khoromana CI, Hightower AW, Machego A, Wirima JJ, Breman JG, Heymann DL, Steketee RW, 1996. Malaria infection in infancy in rural Malawi. Am J Trop Med
Hyg 55(suppl): 7176.
Hoffman SL, Miller LH, 1996. Perspectives on vaccine development. Hoffman SL, ed. Malaria Vaccine Development.
Washington, DC: American Society of Microbiology, 114.
Modiano D, Petrarca V, Sirima BS, Luoni G, Nebie I, Ciallot
DA, Esposito F, Coluzzi M, 1996. Different response to Plasmodium falciparum in West African sympatric ethnic groups.
Proc Natl Acad Sci USA 91: 24152419.
Hill AVS, 1992. Malaria resistance genes: a natural selection.
Trans R Soc Trop Med Hyg 86: 225226.
Gupta S, Hill AVS, Kwiatkowski D, Greenwood BM, Day KP,
1994. Parasite virulence and disease patterns in Plasmodium
falciparum malaria. Proc Natl Acad Sci USA 91: 37153719.
Singh N, Shukla MM, Sharma VP, 1997. Epidemiology of malaria in pregnancy in central India. Bull World Health Organ
77: 567572.
Nosten F, McGready R, Simpson JA, Thwai KL, Balkan S,
Cho T, Hkirijaroen L, Looareesuwan S, White NJ, 1999. Effects of Plasmodium vivax malaria in pregnancy. Lancet 354:
546549.
Hendrickse RG, Adeniyi A, Edington GM, Glasgow EF, White
RH, Houba V, 1972. Quartan malarial nephrotic syndrome.
Lancet 1: 11431149.
Gupta S, Trenholme K, Anderson RM, Day KP, 1994. Antigenic diversity and the transmission of dynamics of Plasmodium falciparum. Science 263: 961963.
Gupta S, Swinton J, Anderson RM, 1994. Theoretical studies
on the effect of genetic heterogeneity in the parasite population on the transmission dynamics of malaria. Proc R Soc
Lond B Biol Sci 256: 231238.
Onori E, 1984. The problem of Plasmodium falciparum drug
resistance in Africa south of the Sahara. Bull World Health
Organ 62(suppl): 5562.
Oliaro PL, Trigg PI, 1995. Status of antimalarial drugs under
development. Bull World Health Organ 75: 565571.
Trape JF, Pison G, Preziosi MP, Enel C, Desgrees du Lou A,
Delaunay V, Samb B, Largarde E, Molez JF, Simondon F,
1998. Impact of chloroquine resistance on malaria mortality.
Comptes rendus de lAcade mie des Sciences, Paris, Se ries III
321: 689697.
Newton P, White N, 1999. Malaria: new developments in treatment and prevention. Annu Rev Med 50: 1990.
Breman JG, Campbell CC, 1988. Combating severe malaria in
African children. Bull World Health Organ 66: 6170.
Kovacs JA, Masur H, 2000. Prophylaxis against opportunistic
10
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
BREMAN
infections in patients with human immunodeficiency virus.
New Engl J Med 342: 14161429.
Feikin DR, Dowell SR, Nwanyanwu OC, Klugman KP, Kazembe PN, Barat LM, Graf C, Bloland PB, Ziba C, Huebner
RE, Schwartz B, 2000. Increased carriage of trimethoprim/
sulfamethoxasole-resistant Streptococcus pneumoniae in Malawian children after treatment for malaria with sulfadoxinepyrimethamine. J Infect Dis 181: 15011505.
Bloland P, Ettling M, 1999. Making malaria-treatment policy
in the face of drug resistance. Ann Trop Med Parasitol 93:
523.
Bruce Chwatt LJ, 1985. Essential Malariology. Second edition.
New York: John Wiley and Sons.
Beier JC, Killeen GF, Githure JI, 1999. Short report: entomologic inoculation rates and Plasmodium falciparum malaria
prevalence in Africa. Am J Trop Med Hyg 61: 109113.
Bloland PB, Boriga DA, Ruebush TK, McCormick JB, Roberts
JM, Oloo AJ, Hawley W, Lal A, Nahlen B, Campbell CC,
1999. Longitudinal cohort study of the epidemiology of malaria infections in an area of intense malaria transmission II.
Descriptive epidemiology of malaria infection and disease
among children. Am J Trop Med Hyg 60: 641648.
Mbogo CN, Snow RW, Khamala CP, Kabiru WE, Ouma JH,
Githure JI, Marsh K, Beier JC, 1995. Relationships between
Plasmodium falciparum transmission by vector populations
and the incidence of severe disease at nine sites on the Kenyan coast. Am J Trop Med Hyg 52: 201206.
McElroy PD, Beier JC, Oster CN, Onyango FK, Oloo AJ, Lin
Y, Beadle C, Hoffman SL, 1997. Dose- and time-dependent
relations between infective Anopheles inoculation and outcomes of Plasmodium falciparum parasitemia among children
in western Kenya. Am J Epidemiol 145: 945956.
Lengeler C, Cattani JA, de Savigny D, eds, 1996. Net Gain:
New Method for Preventing Malaria Deaths. Geneva, Switzerland: Ottawa IDRC and Tropical Disease and Research
Program/World Health Organization.
Lengeler C, 1999. Insecticide treated bed nets and curtains for
preventing malaria (Cochrane Review). The Cochrane Library, Issue 4. Oxford: Update Software.
Binka FN, Kubaje A, Adjuik M, Williams LA, Lengeler C,
Maude GH, Armah GH, Kajihara B, Adiamah JH, Smith PG,
1996. Impact of permethrin impregnated bednets on child
mortality in Kassena-Nankana district, Ghana: a randomized
controlled trial. Trop Med Int Health 1: 147.
DAlessandro U, Olaleye BO, McGuire W, Langerock P, Bennett S, Aikins MK, Thomson MC, Cham MK, Cham BA,
Greenwood BM, 1995. Mortality and morbidity from malaria
in Gambian children after introduction of an impregnated bednet programme. Lancet 345: 479483.
Nevill CG, Some ES, Mungala VO, Muterri W, New L, Marsh
K, Lengeler C, Snow RW, 1996. Insecticide-treated bednets
reduce mortality and severe morbidity from malaria among
children on the Kenyan coast. Trop Med Int Health 1: 139
146.
Alonso P, Lindsay SW, Armstrong JRM, Conteh M, Hill AG,
David PH, Fegan G, de Drancisco A, Hall AJ, Shenton FC,
et al, 1991. The effect of insecticide-treated bed nets on mortality in Gambian children. Lancet 337: 14991502.
Fontaine RE, Najjar AE, Prince JS, 1961. The 1958 malaria
epidemic in Ethiopia. Am J Trop Med Hyg 10: 795803.
Lepers JP, Fontenille D, Rason MD, Chougnet C, Astagneau
P, Coulanges P, Deloron P, 1991. Transmission and epidemiology of newly transmitted falciparum malaria in the central
highland plateaux of Madagascar. Ann Trop Med Parasitol
85: 297304.
Conner SJ, Thomson MC, Molyneux DH, 1999. Forecasting
and prevention of epidemic malaria: new perspectives on an
old problem. Parassitologia 41: 439448.
Craig MH, Snow RW, Le Sueur D, 1999. African climatic
model of malaria transmission based on monthly rainfall and
temperature. Parasitol Today 15: 105111.
Snow RW, Craig MH, Deichmann U, LeSueur D, 1999. A
continental risk map for malaria mortality among African
children. Parasitol Today 15: 99104.
81. LeSueur D, 1996. Creating a preliminary malaria risk atlas in
Africa. Med Trop 56: 109111.
82. Bryce J, Rongou JB, Nguyen-Dinh P, Naimoli JF, Breman JG,
1994. Evaluation of national malaria control programmes in
Africa. Bull World Health Organ 72: 371381.
83. Trape JF, Quinet MC, Nzingoula S, Senga P, Tchichelle F, Carme B, Candito D, Mayanda H, Zoulani A, 1987. Malaria and
urbanization in Central Africa: the example of Brazzaville.
Part B: Pernicious attacks and mortality. Trans R Soc Trop
Med Hyg 81(suppl 2): 3442.
84. Andrewes J, Quimby GE, Langmuir AD, 1950. Malaria eradication in the United States. Am J Public Health 40: 1405
1411.
85. Bruce-Chwatt LJ, de Zulueta J, 1980. The Rise and Fall of
Malaria in Europe: A Historico-Epidemiologic Study. New
York: Oxford University Press.
86. Koram KA, Bennet S, Adiamah JH, Greenwood BM, 1995.
Socioeconomic determinants are not major risk factors for
severe malaria in Gambian children. Trans R Soc Trop Med
Hyg 89: 16031605.
87. Luckner D, Lell B, Greve B, Lehman LG, Schmidt-Ott RJ,
Matousek P, Herbich K, Schmid D, Mba R, Kremsner PG,
1998. No influence of socioeconomic factors on severe malarial anaemia, hyperparasitemia or reinfection. Trans R Soc
Trop Med Hyg 92: 478481.
88. Roll Back Malaria, The Abuja Declaration, Part III, April 25,
2000. 2000. Abuja, Nigeria.
89. Payne D, Grab B, Fontaine RE, Hempel JHG, 1976. Impact of
control measures on malaria transmission and general mortality. Bull World Health Organ 54: 369377.
90. Fontaine RE, Pull JH, Payne D, Pradhan GD, Joshi GB, Pearson JA, Thymakis MV, Camacho ME, 1978. Evaluation of
fenitrothion for the control of malaria. Bull World Health Organ 40: 771783.
91. Molineaux L, Gramiccia G, 1980. The Gharki Project: Research on the Epidemiology and Control of Malaria in the
Sudan Savanna of West Africa. Geneva, Switzerland: World
Health Organization.
92. Silva KT, 1994. Malaria eradication as a legacy of colonial
discourse: the case of Sri Lanka. Parassitologia 36: 149163.
93. Target GAT, ed, 1991. Waiting for the Vaccine. New York:
John Wiley and Sons, 1224.
94. Mons B, Klasen E, van Kessel R, Nchinda T, 1997. Partnerships between north and south crystallizes around malaria.
Science 279: 498499.
95. World Health Organization, 1996. WHO, 5864. Technical Report Series, No. 735, World Health Organization Expert Committee on Malaria, 18th report.
96. Sturchler D, 1989. How much malaria is there worldwide?
Parasitol Today 5: 3940.
97. World Health Organization, 1997. World malaria situation in
1994. Part I: Population at risk. Weekly Epidemiol Rec 72:
269274.
98. World Health Organization, 1997. World malaria situation in
1994. Part II: Population at risk. Weekly Epidemiol Rec 72:
277283.
99. World Health Organization, 1997. World malaria situation in
1994. Part III: Population at risk. Weekly Epidemiol Rec 72:
285290.
100. Molineux L, 1985. The impact of parasitic diseases and their
control, with an emphasis on malaria in Africa. Vallin J, Lopez A, eds. Health Policy, Social Policy and Mortality Prospects. Paris: Ordina Editions, 1344.
101. Murray CJL, Lopez AP, eds, 1996. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Geneva, Switzerland: World Health Organization and Boston: Harvard University Press.
102. Murphy SC, Breman JG, 2000. Gaps in the African childhood
malaria burden adding neurological sequelae, anemia, respiratory distress and complications of pregnancy to the calculus.
Am J Trop Med Hyg 64(suppl 1): 5767.
103. Steketee RW, Nahlen BL, Parise ME, Menendez C, 2000. The
THE MALARIA BURDEN
104.
105.
106.
107.
108.
109.
burden of malaria in pregnancy. Am J Trop Med Hyg
64(suppl 1): 2835.
Greenwood BM, Bradley AK, Greenwood AM, Byass P, Jammeh K, Marsh K, Tulloch, Oldfield FA, Hayes R, 1987. Mortality and morbidity from malaria among children in a rural
area of the Gambia, West Africa. Trans R Soc Trop Med Hyg
81: 478486.
Snow RW, Armstrong JR, Forster D, Winstanley WT, Marsh
VM, Newton CR, Wariuru C, Mwangi I, Winstanley PA,
Marsh K, 1992. Childhood deaths in Africa: uses and limitations of verbal autopsies. Lancet 340: 351355.
Dabis F, Breman JG, Roisin A, Haba F, 1989. Monitoring selective components of primary health care. Bull World Health
Organ 67: 675684.
Trape JF, Zoulani A, Quintet MC, 1987. Assessment of the
incidence and prevalence of clinical malaria in semi-immune
children exposed to intense and perennial transmission. Am J
Epidemiol 126: 193207.
Shi YP, Hasnain SE, Sacci JB, Holloway BP, Fujioka H, Kumar
N, Wohlhneter R, Hoffman SL, Collins WE, Lal AA, 1999.
Immunogenicity and in vitro protective efficacy of a recombinant multistage Plasmodium falciparum candidate vaccine.
Proc Natl Acad Sci USA 96: 16151620.
World Health Organization, 1999. The World Health Report
1999: Making a difference. Geneva, Switzerland: World
Health Organization.
11
110. Nabarro D, Taylor E, 1998. The Roll Back Malaria campaign. Science 280: 20672068.
111. Brundtland G, 1999. Reaching out for world health. Science
280: 2027.
112. Gardner MJ, Tettelin H, Carucci DH, Cummings LM, Smith
HO, Fraser CM, Venter JC, Hoffman SL, 1999. The malaria
genome sequencing project: complete sequence of Plasmodium falciparum chromosome 2. Parassitologia 41: 6975.
113. Shi Y, Das P, Holloway B, Udhayakumar V, Tongren JE, Candal F, Biswas S, Ahmad R, Hasnain SE, Lal AA, 2000. Development, expression, and murine testing of a multistage
Plasmodium falciparum malaria vaccine candidate. Vaccine
18: 29022914.
114. Fidock DA, Nomura T, Talley AK, Cooper RA, Dzekunov SM,
Ferdig MT, Ursos LMB, Sidhu ABS, Naude B, Deitsch KW,
Su X, Wootton JC, Roepe PD, Wellems TE, 2000. Mutations
in the Plasmodium falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol Cell 6: 861871.
115. Mendis K, Sina BJ, Marchesini P, Carter R, 2001. The neglected burden of Plasmodium vivax malaria. Am J Trop Med Hyg
64(suppl 1): 97106.
116. Davies CS, 1999. The Multilateral Initiative on Malaria: coordination and cooperation in international malaria research.
Parassitologia 41: 497500.
You might also like
- Choy Ecologies of ComparisonDocument22 pagesChoy Ecologies of Comparisonxxongh1No ratings yet
- Benezra DeStefano Gordon 2012 Anthropology of Microbes PDFDocument4 pagesBenezra DeStefano Gordon 2012 Anthropology of Microbes PDFxxongh1No ratings yet
- Becoming-Grizzly: Bodily Molecularity and The Animal That BecomesDocument30 pagesBecoming-Grizzly: Bodily Molecularity and The Animal That Becomesxxongh1No ratings yet
- DUNN-1965-On The Antiquity of MalariaDocument9 pagesDUNN-1965-On The Antiquity of Malariaxxongh1No ratings yet
- Embodiment - Holy PeopleDocument12 pagesEmbodiment - Holy Peoplexxongh1No ratings yet
- The Genesis of The Concepts of Habitus and of FieldDocument89 pagesThe Genesis of The Concepts of Habitus and of Fielddonaldo_scherl100% (3)
- Malaria: Civilization Versus DiseaseDocument1 pageMalaria: Civilization Versus Diseasexxongh1No ratings yet
- Malaria BednetsDocument14 pagesMalaria Bednetsxxongh1No ratings yet
- Setha Low 2003-Embodied SpacesDocument11 pagesSetha Low 2003-Embodied Spacesxxongh1No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Astm B19Document6 pagesAstm B19Davor IbarraNo ratings yet
- Shakespeare Sonnet EssayDocument3 pagesShakespeare Sonnet Essayapi-5058594660% (1)
- RFID Seminar AbstractDocument2 pagesRFID Seminar Abstractanushabhagawath80% (5)
- An Annotated Bibliography of Timothy LearyDocument312 pagesAn Annotated Bibliography of Timothy LearyGeetika CnNo ratings yet
- Impact of Pantawid Pamilyang Pilipino Program On EducationDocument10 pagesImpact of Pantawid Pamilyang Pilipino Program On EducationEllyssa Erika MabayagNo ratings yet
- Sources of Hindu LawDocument9 pagesSources of Hindu LawKrishnaKousikiNo ratings yet
- Subject Manual Tle 7-8Document11 pagesSubject Manual Tle 7-8Rhayan Dela Cruz DaquizNo ratings yet
- Technology Based Project: Special Track 1)Document14 pagesTechnology Based Project: Special Track 1)Kim ChiquilloNo ratings yet
- Evolution Army 3 R DadDocument341 pagesEvolution Army 3 R DadStanisław DisęNo ratings yet
- 16783Document51 pages16783uddinnadeemNo ratings yet
- Pg2022 ResultDocument86 pagesPg2022 ResultkapilNo ratings yet
- SweetenersDocument23 pagesSweetenersNur AfifahNo ratings yet
- Deep Hole Drilling Tools: BotekDocument32 pagesDeep Hole Drilling Tools: BotekDANIEL MANRIQUEZ FAVILANo ratings yet
- Phytotherapy On CancerDocument21 pagesPhytotherapy On CancerSiddhendu Bhattacharjee100% (1)
- QuexBook TutorialDocument14 pagesQuexBook TutorialJeffrey FarillasNo ratings yet
- Prevention of Waterborne DiseasesDocument2 pagesPrevention of Waterborne DiseasesRixin JamtshoNo ratings yet
- Perancangan Crushing Plant Batu Andesit Di PT Nurmuda Cahaya Desa Batujajar Timur Kecamatan Batujajar Kabupaten Bandung Barat Provinsi Jawa BaratDocument8 pagesPerancangan Crushing Plant Batu Andesit Di PT Nurmuda Cahaya Desa Batujajar Timur Kecamatan Batujajar Kabupaten Bandung Barat Provinsi Jawa BaratSutan AdityaNo ratings yet
- YIC Chapter 1 (2) MKTDocument63 pagesYIC Chapter 1 (2) MKTMebre WelduNo ratings yet
- Delusion in SocietyDocument2 pagesDelusion in SocietyGasimovskyNo ratings yet
- Teaching Profession - Educational PhilosophyDocument23 pagesTeaching Profession - Educational PhilosophyRon louise PereyraNo ratings yet
- Fast Track Design and Construction of Bridges in IndiaDocument10 pagesFast Track Design and Construction of Bridges in IndiaSa ReddiNo ratings yet
- PresentationDocument27 pagesPresentationMenuka WatankachhiNo ratings yet
- Hans Belting - The End of The History of Art (1982)Document126 pagesHans Belting - The End of The History of Art (1982)Ross Wolfe100% (7)
- Fire Protection in BuildingsDocument2 pagesFire Protection in BuildingsJames Carl AriesNo ratings yet
- UntitledDocument216 pagesUntitledMONICA SIERRA VICENTENo ratings yet
- Aleutia Solar Container ClassroomDocument67 pagesAleutia Solar Container ClassroomaleutiaNo ratings yet
- KsDocument5 pagesKsnurlatifahNo ratings yet
- The cardioprotective effect of astaxanthin against isoprenaline-induced myocardial injury in rats: involvement of TLR4/NF-κB signaling pathwayDocument7 pagesThe cardioprotective effect of astaxanthin against isoprenaline-induced myocardial injury in rats: involvement of TLR4/NF-κB signaling pathwayMennatallah AliNo ratings yet
- Lieh TzuDocument203 pagesLieh TzuBrent Cullen100% (2)
- 2022 WR Extended VersionDocument71 pages2022 WR Extended Versionpavankawade63No ratings yet