Professional Documents
Culture Documents
Pancreatitis: (Alterations in Metabolic and Endocrine Functions)
Uploaded by
Jorie RocoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pancreatitis: (Alterations in Metabolic and Endocrine Functions)
Uploaded by
Jorie RocoCopyright:
Available Formats
[Alterations in Metabolic and Endocrine Functions]
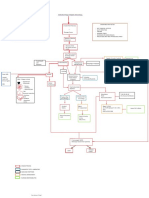
PANCREATITIS
Predisposing factors:
Precipitating factors:
- Alcohol abuse
- Drugs (antihypertensives, diuretics, antimicrobials,
immunosuppresives, oral contraceptives)
- Biliary obstruction
- Hypercalcemia
- Hypertriglyceridemia
- Abdominal trauma
- Tumors
- Ischemia
- Genetic/ Family History
- Anatomical variants
Damage to pancreatic
cells
Elastase
Inflammation of the
parenchyma
Necrosis of blood vessels
and ductal fibers
Edema of the pancreas
and pancreatic duct
Hemorrhage
Activation of pancreatic
enzymes inside pancreas
Acute
Pancreatitis
Phospholipase A
Autodigestion of the
pancreas
Fat necrosis
Cell membrane
Further inflammation
of pancreas
Lipase
Fat Necrosis
Obstruction to the flow
of pancreatic enzyme
Chronic
Pancreatitis
Kalikrein
Edema
Vascular permeability
Smooth muscle contraction
Vasodilation
Hypoperfusion
Peripancreatic exudation or pancreatic ductal
leakage
Necrosis
Pseudocyst
Invasion of bacteria
Infected necrotic pancreas or abscess
Compresses nearby organs
Constant pain or deep ache in the
abdomen which felt in the back
Realease of toxic metabolites into peritoneal space
Ruptured due to trauma to the sac
Realease of toxic metabolites into blood
Hemorrhage
Death
SOURCES:
Shock
Pulmonary Insufficiency
Acute renal failure
Dissemenated Intravascular
Coagulation
Hypovolemia
Fisher, T. & Raton, B. (2015, March 16). MedlinePlus: Pancreatic Pseudocyst. Retrieved March 20, 2015, from
http://www.nlm.nih.gov/medlineplus/ency/article/000272.htm.
Freedman, S. (2013, October). The Merck Manual: Acute Pancreatitis. Retrieved March 2015, from
[Alterations in Metabolic and Endocrine Functions]
http://www.merckmanuals.com/professional/gastrointestinal_disorders/pancreatitis/acute_pancreatitis.html.
Gardner, T. (2014, December 8). Medscape: Acute Pancreatitis. Retrieved March 2015, from
http://emedicine.medscape.com/article/181364-overview.
Pancreatitis. (2015). In Encyclopdia Britannica. Retrieved from http://www.britannica.com/EBchecked/topic/441022/pancreatitis.
PANCREATITIS
Pancreatitis is a disease in which the pancreas becomes inflamed. Pancreatic damage happens
when the digestive enzymes are activated before they are released into the small intestine and begin
attacking the pancreas.[1]
There are two forms of pancreatitis: acute and chronic.
Acute pancreatitis.
Acute pancreatitis is a sudden inflammation that lasts for a short time. It may range from mild
discomfort to a severe, life-threatening illness. Most people with acute pancreatitis recover completely
after getting the right treatment. In severe cases, acute pancreatitis can result in bleeding into the gland,
serious tissue damage, infection, and cyst formation. Severe pancreatitis can also harm other vital organs
such as the heart, lungs, and kidneys.[2]
Chronic pancreatitis.
Chronic pancreatitis is long-lasting inflammation of the pancreas. It most often happens after an
episode of acute pancreatitis. Heavy alcohol drinking is another big cause. Damage to the pancreas from
heavy alcohol use may not cause symptoms for many years, but then the person may suddenly develop
severe pancreatitis symptoms.[3]
ETIOLOGY
Acute pancreatitis has many causes, such as alcohol abuse, cholelithiasis, abdominal trauma,
virus infection, drugs, and metabolic factors. The mechanisms by which these conditions trigger
pancreatic inflammation have not been identified.[4]
Acute pancreatitis is thought to result from inappropriate intrapancreatic activation of proteases,
which causes autodigestion of the pancreas. Exactly how this occurs is unknown.
[5]
It is thought that
alcohol-induced pancreatitis may include a physiochemical alteration of protein that results in plugs that
Pancreatitis. (2015). In Encyclopdia Britannica. Retrieved from http://www.britannica.com/EBchecked/topic/441022/pancreatitis..
Freedman, S. (2013, October). The Merck Manual: Acute Pancreatitis. Retrieved March 2015, from
http://www.merckmanuals.com/professional/gastrointestinal_disorders/pancreatitis/acute_pancreatitis.html.
Lewis, S. and et.al. Medical Surgical Nursing: Assessment and Management of Clinical Problems. Singapore: Mosby Elsevier Inc. .
[Alterations in Metabolic and Endocrine Functions]
(2008).
4
Gardner, T. (2014, December 8). Medscape: Acute Pancreatitis. Retrieved March 2015, from
http://emedicine.medscape.com/article/181364-overview.
block the small pancreatic ductules. Biliary pancreatitis occurs when edema or an obstruction blocks
the ampulla of Vater, resulting in reflux of bile into pancreatic ducts or direct injury to the acinar cells.
Other causes include the following:
Hyperlipidemia, which may occur secondary to nephritis, castration, or exogenous estrogen
administration, or as hereditary hyperlipidemia
Hypercalcemia arising as a result of hyperparathyroidism
Cholecystitis and cholelithiasis
Familial cases with no definite mechanism defined
Pancreatic tumor
Pancreatic trauma or pancreatic duct obstruction, such as penetrating or blunt external trauma,
intraoperative manipulation, or ampullar manipulation, and pancreatic ductal overdistention during
endoscopic retrograde cholangiopancreatography (ERCP)
Pancreatic ischemia during episodes of hypotensive shock, cardiopulmonary bypass, visceral
atheroembolism, or vasculitis
Drugs; although azathioprine and estrogens have been directly linked with the disease, many
other drugs are believed to have an association (e.g., antibiotics, anticonvulsants, thiazide diuretics,
sulfonamides, valproic acid)
Other general causes, such as pancreatic duct obstruction, obesity, duodenal obstruction, viral
infection (e.g., mumps), carcinoma, scorpion venom, ERCP, peritoneal dialysis, and factors still to
be determined.[1]
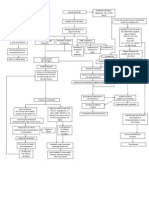
PATHOPHYSIOLOGY
Pancreatitis occurs when digestive enzymes produced in your pancreas become activated while
inside the pancreas, causing damage to the organ.[2]
During normal digestion, the inactivated pancreatic enzymes move through ducts in your pancreas
and travel to the small intestine, where the enzymes become activated and help with digestion.[3]
Pancreatitis. (2015). In Encyclopdia Britannica. Retrieved from http://www.britannica.com/EBchecked/topic/441022/pancreatitis.
[Alterations in Metabolic and Endocrine Functions]
2
Udan, J. (2002). Medical Surgical: Concepts and Clinical Application (First Edition). Philippines: Guiani Prints House.
Ibid
In pancreatitis, the enzymes become activated while still in the pancreas. This causes the pancreas to
undergo the process of inflammation. It is thought that alcohol increases the production of digestive
enzymes in the pancreas and/or increases the sensitivity to the hormone cholecystokinin (CKK). CCK
stimulates the production of pancreatic enzymes. Other and most common pathologic mechanism is
autodigestion of the pancreas that may lead to further damage to thepancreas. One possible cause is the
reflux of the bile acids into the pancreatic ducts through an open or distended sphincter of Oddi. This
causes the enzymes to irritate the cells of your pancreas, causing inflammation and the signs and
symptoms associated with pancreatitis.[1]
Regardless of the etiology, pancreatic enzymes (including trypsin, phospholipase A2, and elastase)
become activated within the gland itself. The enzymes can damage tissue and activate the complement
system and the inflammatory cascade, producing cytokines. This process causes inflammation, edema,
and sometimes necrosis. In mild pancreatitis, inflammation is confined to the pancreas. In severe
pancreatitis, there is significant inflammation, with necrosis and hemorrhage of the gland and a systemic
inflammatory response. After 5 to 7 days, necrotic pancreatic tissue may become infected by enteric
bacteria.[2]
Activated enzymes and cytokines that enter the peritoneal cavity cause a chemical burn and third
spacing of fluid; those that enter the systemic circulation cause a systemic inflammatory response that
can result in acute respiratory distress syndrome and renal failure. The systemic effects are mainly the
result of increased capillary permeability and decreased vascular tone, which result from the released
cytokines and chemokines. Phospholipase A2 is thought to injure alveolar membranes of the lungs.[3]
In about 40% of patients, collections of enzyme-rich pancreatic fluid and tissue debris form in and
around the pancreas. In about half, the collections resolve spontaneously. In others, the collections
become infected or form pseudocysts. Pseudocysts have a fibrous capsule without an epithelial lining.
Pseudocysts may hemorrhage, rupture, or become infected.[4]
Pancreatitis. (2015). In Encyclopdia Britannica. Retrieved from http://www.britannica.com/EBchecked/topic/441022/pancreatitis..
Freedman, S. (2013, October). The Merck Manual: Acute Pancreatitis. Retrieved March 2015, from
http://www.merckmanuals.com/professional/gastrointestinal_disorders/pancreatitis/acute_pancreatitis.html.
Gardner, T. (2014, December 8). Medscape: Acute Pancreatitis. Retrieved March 2015, from
http://emedicine.medscape.com/article/181364-overview.
[Alterations in Metabolic and Endocrine Functions]
4
Fisher, T. & Raton, B. (2015, March 16). MedlinePlus: Pancreatic Pseudocyst. Retrieved March 20, 2015, from
http://www.nlm.nih.gov/medlineplus/ency/article/000272.htm.
With repeated bouts of acute pancreatitis, damage to the pancreas can occur and lead to chronic
pancreatitis. Scar tissue may form in the pancreas, causing loss of function. A poorly functioning
pancreas can cause digestion problems and diabetes.[1]
CLINICAL MANIFESTATION
Signs and symptoms of pancreatitis may vary, depending on which type you experience.
Acute pancreatitis signs and symptoms include:
Upper abdominal pain
Abdominal pain that radiates to your back Abdominal pain that feels worse after eating
Nausea
Vomiting
Tenderness when touching the abdomen
Chronic pancreatitis signs and symptoms include:
Upper abdominal pain
Losing weight without trying
Oily, smelly stools (steatorrhea)
The following uncommon physical findings are associated with severe necrotizing pancreatitis:
Cullen sign (bluish discoloration around the umbilicus resulting from hemoperitoneum)
Grey-Turner sign (reddish-brown discoloration along the flanks resulting from retroperitoneal
blood dissecting along tissue planes); more commonly patients may have a ruddy erythema in the
flanks secondary to extravasated pancreatic exudate.
Erythematous skin nodules, usually no longer than 1 cm and typically located on extensor skin
surfaces; polyarthritis.[2]
Complications
Pancreatitis can cause serious complications, including:
Infection. Acute pancreatitis can make your pancreas vulnerable to bacteria and infection.
Pancreatic infections are serious and require intensive treatment, such as surgery to remove the
infected tissue. [3]
Pseudocyst. Acute pancreatitis can cause fluid and debris to collect in cyst-like pockets in your
pancreas. A large pseudocyst that ruptures can cause complications such as internal bleeding and
infection.[4]
Gardner, T. (2015, April 1). Medscape: Acute Pancreatitis. Retrieved April 15, 2015, from http://emedicine.medscape.com/article/181364-
[Alterations in Metabolic and Endocrine Functions]
overview.
2
Ibid
Ibid
Fisher, T. & Raton, B. (2015, March 16). MedlinePlus: Pancreatic Pseudocyst. Retrieved March 20, 2015, from
http://www.nlm.nih.gov/medlineplus/ency/article/000272.htm.
Breathing problems. Acute pancreatitis can cause chemical changes in your body that affect your
lung function, causing the level of oxygen in your blood to fall to dangerously low levels.[1]
Diabetes. Damage to insulin-producing cells in your pancreas from chronic pancreatitis can lead
to diabetes, a disease that affects the way your body uses blood sugar.[2]
Kidney failure. Acute pancreatitis may cause kidney failure, which can be treated with dialysis if
the kidney failure is severe and persistent.[3]
Malnutrition. Both acute and chronic pancreatitis can cause your pancreas to produce fewer of
the enzymes that are needed to break down and process nutrients from the food you eat. This can
lead to malnutrition, diarrhea and weight loss, even though you may be eating the same foods or the
same amount of food.[4]
Pancreatic cancer. Long-standing inflammation in your pancreas caused by chronic pancreatitis
is a risk factor for developing pancreatic cancer.[5]
Jaclyn Mae T. Alviola
MSN Student
Freedman, S. (2013, October). The Merck Manual: Acute Pancreatitis. Retrieved March 2015, from
http://www.merckmanuals.com/professional/gastrointestinal_disorders/pancreatitis/acute_pancreatitis.html.
[Alterations in Metabolic and Endocrine Functions]
2
Ibid
Ibid
Gardner, T. (2014, December 8). Medscape: Acute Pancreatitis. Retrieved March 2015, from
http://emedicine.medscape.com/article/181364-overview.
Ibid
You might also like
- PancreatitisDocument26 pagesPancreatitisJnah Macs100% (2)
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 2 Acute CholecystitisDocument21 pages2 Acute CholecystitisEtteh MaryNo ratings yet
- CHOLELITHIASISDocument46 pagesCHOLELITHIASIShttp_ugly88% (8)
- Cholelithiasis: - Other Names: - Gallbladder Attack - Biliary Colic - Gallstone Attack - Bile Calculus - Biliary CalculusDocument101 pagesCholelithiasis: - Other Names: - Gallbladder Attack - Biliary Colic - Gallstone Attack - Bile Calculus - Biliary CalculusYvonne100% (1)
- A Case Study On A Patient Diagnosed With UlcerDocument20 pagesA Case Study On A Patient Diagnosed With UlcerNevoj_Nygrin_3313No ratings yet
- Hiatal Hernia Pathophysiology - Schematic DiagramDocument1 pageHiatal Hernia Pathophysiology - Schematic DiagramTrixie Arabit100% (1)
- Pathophysiology of GastritisDocument2 pagesPathophysiology of GastritisFlorsean Mae Sala80% (5)
- Ugib Case StudyDocument30 pagesUgib Case StudyVenus Glaze Verzola80% (5)
- CHOLEDOCHOLITHIASISDocument38 pagesCHOLEDOCHOLITHIASISPrecious Cofreros100% (3)
- Tarlac State University College of Nursing case study on choledocholithiasisDocument53 pagesTarlac State University College of Nursing case study on choledocholithiasisCzarina ManinangNo ratings yet
- Pathophysiology: Cholecystitis Non Modifiable Factors Modifiable FactorsDocument4 pagesPathophysiology: Cholecystitis Non Modifiable Factors Modifiable FactorsYuyu Tulawie100% (1)
- Pathophysiology of BPH: Risk Factors, Symptoms & TreatmentDocument1 pagePathophysiology of BPH: Risk Factors, Symptoms & TreatmentKevin Jade Herrera0% (2)
- Pathophysiology of Intestinal ObstructionDocument3 pagesPathophysiology of Intestinal ObstructionJOvie Rectin100% (2)
- San Pablo Colleges Medical Center case presentation on cholelithiasisDocument43 pagesSan Pablo Colleges Medical Center case presentation on cholelithiasisMary Rose LinatocNo ratings yet
- Bowel Obstruction PathophysiologyDocument4 pagesBowel Obstruction PathophysiologyAya BolinasNo ratings yet
- Bladder Cancer Types, Symptoms, Tests & TreatmentDocument1 pageBladder Cancer Types, Symptoms, Tests & TreatmentCarmina AguilarNo ratings yet
- CHOLECYSTECTOMYDocument35 pagesCHOLECYSTECTOMYfaitheee100% (3)
- Acute PancreatitisDocument7 pagesAcute PancreatitisVytheeshwaran Vedagiri100% (9)
- CholelithiasisDocument5 pagesCholelithiasisrgflores1979100% (2)
- PancreatitisDocument12 pagesPancreatitisjhodane100% (4)
- NCP Anorexia NervosaDocument5 pagesNCP Anorexia NervosaJohn Ver Tolentino AdaoNo ratings yet
- Cholecystitis Case PresDocument103 pagesCholecystitis Case PresAnton LaurencianaNo ratings yet
- Hemorrhagic StrokeDocument12 pagesHemorrhagic StrokeManggara Surya DharmaNo ratings yet
- Acute PancreatitisDocument23 pagesAcute PancreatitisGel Torres Galvez50% (2)
- Care Study OsteomyelitisDocument23 pagesCare Study OsteomyelitisJake Pitos100% (1)
- Pathophysiology CholecystitisDocument4 pagesPathophysiology CholecystitiskikaycutieNo ratings yet
- Liver Cirrhosis: A Case Study OnDocument31 pagesLiver Cirrhosis: A Case Study OnCharmaine del RosarioNo ratings yet
- A Case Study On CholedocholithiasisDocument81 pagesA Case Study On Choledocholithiasischristelle6cadiente67% (9)
- CHOLANGITISDocument1 pageCHOLANGITISKirk Torregosa PañaresNo ratings yet
- CholelithiasisDocument37 pagesCholelithiasisbaby padzNo ratings yet
- Open CholecystectomyDocument15 pagesOpen CholecystectomyjimdioNo ratings yet
- Obstructive UropathyDocument47 pagesObstructive UropathyChristine Karen Ang Suarez100% (3)
- CP On Calculous CholelithiasisDocument102 pagesCP On Calculous Cholelithiasiskathy100% (3)
- Colorectal CancerDocument8 pagesColorectal Cancerjorgeacct100% (3)
- NCP LeukemiaDocument2 pagesNCP LeukemiaNichole Audrey Saavedra0% (1)
- Colon Cancer Case StudyDocument18 pagesColon Cancer Case Studyapi-271062060100% (2)
- Appendicitis (History & Examination)Document6 pagesAppendicitis (History & Examination)Doctor Saleem Rehman75% (4)
- CHOLECYSTITISDocument13 pagesCHOLECYSTITISdolly joy100% (1)
- Nursing Process of A Client With CholelithiasisDocument21 pagesNursing Process of A Client With Cholelithiasisapi-3822508100% (6)
- CholelithiasisDocument3 pagesCholelithiasisMIlanSagittarius0% (1)
- Pathophysiology of Acute PancreatitisDocument1 pagePathophysiology of Acute PancreatitisHarvin FrancoNo ratings yet
- CROHNSDocument2 pagesCROHNSAlvin Germo Pasuquin100% (1)
- PathophysiologyDocument4 pagesPathophysiologyAngelou Joefred Congreso100% (1)
- Obstructive JaundiceDocument54 pagesObstructive JaundiceJenine Ezra M. Conol50% (2)
- Urinary Tract InfectionDocument10 pagesUrinary Tract InfectionasokumrNo ratings yet
- Colon Cancer: Causes, Symptoms, Stages & TreatmentDocument17 pagesColon Cancer: Causes, Symptoms, Stages & TreatmentYaska MusaNo ratings yet
- Dka Patho DiagramDocument1 pageDka Patho DiagramGrae TaclobNo ratings yet
- Nursing Upper Gi BleedingDocument23 pagesNursing Upper Gi BleedingLord Pozak Miller100% (3)
- Gastric Cancer: Calag, Prescilla Tavas, Charme FayeDocument20 pagesGastric Cancer: Calag, Prescilla Tavas, Charme FayeDareRaymond0% (1)
- Calculous CholecystitisDocument137 pagesCalculous Cholecystitisrremonde100% (5)
- Anatomy, Diagnosis, and Treatment of Common Bile Duct StonesDocument3 pagesAnatomy, Diagnosis, and Treatment of Common Bile Duct StonesPao AcelajadoNo ratings yet
- Pathophysiology of DMDocument4 pagesPathophysiology of DMNicole Louise N. VillanuevaNo ratings yet
- Case Study MastectomyDocument26 pagesCase Study MastectomyIcheAnne Nilay100% (2)
- Pathophysiology of Prostate CancerDocument1 pagePathophysiology of Prostate CancerArnzz Agbulos100% (1)
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Nu'man AS DaudDocument23 pagesNu'man AS DaudHidayat BazeherNo ratings yet
- Acute PancreatitisDocument39 pagesAcute PancreatitisGloria KikiNo ratings yet
- PancreasDocument12 pagesPancreasAli KhanNo ratings yet
- Anatomic Changes, Infiltration FibrosisDocument23 pagesAnatomic Changes, Infiltration FibrosisAgus YohanesNo ratings yet
- Case Study ProposalDocument4 pagesCase Study ProposalJorie RocoNo ratings yet
- Critical Thinking PointersDocument40 pagesCritical Thinking PointersJorie RocoNo ratings yet
- BioethicsDocument31 pagesBioethicsJorie RocoNo ratings yet
- Cover Page Nursing ManualDocument1 pageCover Page Nursing ManualJorie RocoNo ratings yet
- Nursing TheoriesDocument51 pagesNursing TheoriesJorie RocoNo ratings yet
- Transpersonal CaringDocument46 pagesTranspersonal CaringJorie Roco100% (1)
- Chapter 1Document5 pagesChapter 1Jorie RocoNo ratings yet
- Approval Sheet SampleDocument1 pageApproval Sheet SampleJorie RocoNo ratings yet
- Hypos TestingDocument192 pagesHypos TestingJorie RocoNo ratings yet
- Kinds of Data PresentationDocument18 pagesKinds of Data PresentationJorie RocoNo ratings yet
- Jean Watson's Theory of Transpersonal CaringDocument24 pagesJean Watson's Theory of Transpersonal CaringJorie RocoNo ratings yet
- Measures of LocationDocument9 pagesMeasures of LocationJorie RocoNo ratings yet
- Overview of SpssDocument49 pagesOverview of SpssJorie RocoNo ratings yet
- Table of ContentsDocument2 pagesTable of ContentsJorie RocoNo ratings yet
- Measures of SkewnessDocument15 pagesMeasures of SkewnessJorie Roco100% (1)
- Kinds of Data PresentationDocument18 pagesKinds of Data PresentationJorie RocoNo ratings yet
- StaffingDocument50 pagesStaffingPradeep PandaNo ratings yet
- Cholecystitis: (Alterations in Metabolic and Endocrine Functions)Document4 pagesCholecystitis: (Alterations in Metabolic and Endocrine Functions)Jorie RocoNo ratings yet
- Advanced Statistics ReviewDocument21 pagesAdvanced Statistics ReviewJorie RocoNo ratings yet
- Summary StatisticsDocument28 pagesSummary StatisticsJorie RocoNo ratings yet
- The Teacher's Role and ResponsibilitiesDocument7 pagesThe Teacher's Role and ResponsibilitiesJorie RocoNo ratings yet
- SurveyDocument38 pagesSurveyJorie RocoNo ratings yet
- J1 Lecture 1 A Stimulus To DefineDocument6 pagesJ1 Lecture 1 A Stimulus To DefineJorie RocoNo ratings yet
- Measures of LocationDocument9 pagesMeasures of LocationJorie RocoNo ratings yet
- Survey Hema OncoDocument1 pageSurvey Hema OncoJorie RocoNo ratings yet
- Nursing Administration PowepointDocument27 pagesNursing Administration PowepointJorie RocoNo ratings yet
- Objectives For Hospital ExperienceDocument5 pagesObjectives For Hospital ExperienceJorie RocoNo ratings yet
- Saint Paul University Dumaguete Graduate School: Master of Science in NursingDocument5 pagesSaint Paul University Dumaguete Graduate School: Master of Science in NursingJorie RocoNo ratings yet
- Liver Cirrhosis: (Alterations in Metabolic and Endocrine Functions)Document8 pagesLiver Cirrhosis: (Alterations in Metabolic and Endocrine Functions)Jorie RocoNo ratings yet
- The Endocrine System Evy SulistyoningrumDocument100 pagesThe Endocrine System Evy SulistyoningrumPiko CandyNo ratings yet
- Renal MCQ 2021Document27 pagesRenal MCQ 2021Shahriar Ahmed Sujoy100% (2)
- Photo SkinDocument13 pagesPhoto SkinChan JianweiNo ratings yet
- UNIT 1 THE DIGESTIVE SYSTEM Def PDFDocument3 pagesUNIT 1 THE DIGESTIVE SYSTEM Def PDFDNo ratings yet
- Electrolyte and Acid Base DisordersDocument46 pagesElectrolyte and Acid Base DisordersMia ValdesNo ratings yet
- Digestive System Overview - Functions, Parts & ProcessesDocument17 pagesDigestive System Overview - Functions, Parts & ProcessesDexter DelcarmenNo ratings yet
- The Four Basic TissuesDocument38 pagesThe Four Basic TissuesAurha Akmal GinarisNo ratings yet
- Siadh - Patho, Signs, Causes, TreatmentDocument1 pageSiadh - Patho, Signs, Causes, TreatmentVishalNo ratings yet
- Drug Ekskretion - PPTX EditDocument29 pagesDrug Ekskretion - PPTX Editapoteker mudaNo ratings yet
- J Neurol Neurosurg Psychiatry-2010-Ffytche-1280-7Document9 pagesJ Neurol Neurosurg Psychiatry-2010-Ffytche-1280-7Juliana RestrepoNo ratings yet
- Geria ReviewerDocument2 pagesGeria ReviewerbillyktoubattsNo ratings yet
- 10.4 Homeostasis-1Document10 pages10.4 Homeostasis-1صالح ابراهيمNo ratings yet
- MRSM Biology Notes TransportDocument16 pagesMRSM Biology Notes TransportAhmad Hafize100% (2)
- Dexamethasone Suppression TestDocument2 pagesDexamethasone Suppression Testjbeans92No ratings yet
- Fastigial and Cerebellum and PDFDocument2 pagesFastigial and Cerebellum and PDFRobertNo ratings yet
- Case Study Nephrotic SyndromeDocument26 pagesCase Study Nephrotic SyndromeDimpal Choudhary0% (2)
- Chronic Kidney Disease LIFA FixxxDocument19 pagesChronic Kidney Disease LIFA FixxxMuzdalifa MohamadNo ratings yet
- Animal Nutrition DigestionDocument26 pagesAnimal Nutrition Digestionabdulrehman mughalNo ratings yet
- Neuro 1Document11 pagesNeuro 1Soundararajan RajagopalanNo ratings yet
- Heart Failure: Applied Medicine BY: Dr. Kinza IftikharDocument17 pagesHeart Failure: Applied Medicine BY: Dr. Kinza IftikharsabaamjadNo ratings yet
- SP1ES EGRA Class Reading Profile Grade 2Document2 pagesSP1ES EGRA Class Reading Profile Grade 2Camille Langit DelacruzNo ratings yet
- Lecture 10 PlasticityDocument36 pagesLecture 10 PlasticityDrGasnasNo ratings yet
- Patient Identification and Examination ReportDocument11 pagesPatient Identification and Examination Reportanimesh pandaNo ratings yet
- Act Sheet 1 4th Quarter Science 8Document3 pagesAct Sheet 1 4th Quarter Science 8Joseph Gabriel Genuino CruzNo ratings yet
- Diabetes Melitus 2 DkaDocument104 pagesDiabetes Melitus 2 DkaLaiza Fatima LacsonNo ratings yet
- Hepatocellular Carcinoma and Other Hepatic MassesDocument59 pagesHepatocellular Carcinoma and Other Hepatic MassesIsaac MwangiNo ratings yet
- Figure 1: Cracker LabDocument4 pagesFigure 1: Cracker Labapi-296590771No ratings yet
- VCE Biology Unit 3 Summaries - Immune SystemDocument7 pagesVCE Biology Unit 3 Summaries - Immune SystemDJTofiNo ratings yet
- ENGLISHDocument5 pagesENGLISHArmida SisonNo ratings yet
- HormonesDocument2 pagesHormonesmaxwell amponsahNo ratings yet