Professional Documents
Culture Documents
Student Prep - Basics of A SOAP Note-2
Uploaded by
lovefifteenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Student Prep - Basics of A SOAP Note-2
Uploaded by
lovefifteenCopyright:
Available Formats
ECM 3-4 Students: Preparation
Preparation for the Session: Basics of a SOAP note
Not to be confused: Full H&P vs. a SOAP note:
Usually on the first day that a patient is admitted to your medical team or when a new patient shows up in your
outpatient clinic, a full and complete History & Physical or H&P or an admit note is written, which includes a
detailed write-up of CC, HPI, past medical history, past surgical history, family history, allergies, etc. Starting on the
second day of admission or when seeing a patient you are familiar with, a SOAP note can be written, with the goal of
documenting any NEW information and an updated assessment & plan since the last visit with the patient.
Practically speaking, this means that a SOAP note can include only the new information elicited from the patient since
the last visit. However, important information already documented in the previous notes can be repeated for
improved communication, when it is appropriate for the situation and/or depending on the personal style.
Talking about personal style
The residents and attendings youll be working with will be the best resources for feedback on your SOAP notes. Ask
them at the very beginning for their expectations on notes from medical students. Often times, for the sake of
students learning, the format can be different than what you see the residents and attendings write for themselves.
The attendings may (and often do) use your SOAP notes as part of the evaluation for your overall rotation grade. And
since each clerkship may require different SOAP note elements, it is best to ask early for guidance. Just as a
reference, several samples of SOAP notes will be provided at the completion of this session.
What is a SOAP note?
SOAP stands for Subjective, Objective, Assessment, and Plan.
Subjective: This section is for information provided to you, often verbally, by others.
This is essentially the History portion of the History & Physical, which includes pretty much everything that the
patient or the family tells you. Obtain the patients history since the last visit by asking either How were things over
night? if you saw the patient yesterday or How were things since the last visit? if you havent seen the patient in a
while.
Other pertinent things that may be included in this section include reports from the nursing staff or other new
subjective information, such as new family history information or new information obtained from hospital records.
Objective: This section is for info you can verify yourself.
This includes the vitals, fluids in/out of the body, general appearance and physical exam, labs, imaging, and
medications/procedures/surgeries that your team has performed while under your care. A mnemonic that can be
used to remember the order in which this information is commonly presented is VIP LIMPS, which stands for Vitals,
I/Os, Physical exam, Lab, Imaging, Medications, Procedures, Surgeries.
Another thing not to be confused: Medications taken at home before admission or procedures done on the patient
before being on your team would belong to the subjective aka history portion of the admit H&P or your SOAP
note.
Developed by Richard Keyme MD, Class of 2013
ECM 3-4 Students: Preparation
The medications that are provided to the patient now and the procedures that you perform yourself are objective
aka directly observed and would belong in this section.
Assessment:
Consider this portion the executive summary of the SOAP note. A lot of information has been presented so far in this
latest SOAP note, as well as in the previous SOAP notes and the admit H&P. Try to synthesize all of the information
known about the patient, including a working diagnosis and a rationale for the diagnosis.
Plan:
As a M3 medical student, you should always practice proposing a plan for your patient, but also expect that it will
often require additional input from residents and attendings. This will improve with more experience within the field,
as well as experience throughout the third year. Even though you will often have incomplete or incorrect
assessment/plan portion of the SOAP notes, its just as important to practice synthesizing it yourself. Practice will
make it almost perfect.
As a medical student, it may be more important (and expected) to include the following components:
1. Your differential diagnosis (in ranked order of likelihood) with explanation
2. The current management for the problem
3. Your proposal for the next steps in management (diagnostic, therapeutic, patient education) with
explanation
*Note: Assessment/Plan can be combined for convenience or personal preference. And just like other parts of the
SOAP note, the exact format of this section can depend on the personal style and/or the situation. Two common
approaches to A/P are system based and problem based. Whichever system you decide to use, it is important as
a medical student to provide the differential diagnosis and provide an explanation justifying the differential. Just as a
reference, in internal medicine, system based approaches are more commonly used in the ICU setting and problem
based approaches are more commonly used in the general wards. Examples are provided during the session.
And lastly, please remember to sign your note and have it reviewed by a resident or an attending:
Your full name, MS3
Additional Reference in preparation for the session:
How to write short-hand lab results:
Chem 7:
CBC:
Basic Metabolic Panel (BMP): Refers to a Chem 7 + Calcium
Developed by Richard Keyme MD, Class of 2013
ECM 3-4 Students: Preparation
Comprehensive Metabolic Panel (CMP): BMP + Albumin, Total Protein, Alkaline Phosphatase, AST, ALT, Bilirubin
Not to be confused: Do not confuse Metabolic Panel with Lipid Panel. Lipid panel is the test ordered to measure
LDL, HDL, Triglycerides, Total cholesterol, VLDL, and cholesterol:HDL ratio.
*Side note: It may take some time, but it will be useful to know the normal values for all the components above (or at
least have a general idea of when a number is grossly abnormal). Even with all the computers and electronics easily
available, it will save a significant time in the long run to have this knowledge as early as possible.
Practice Questions: Please categorize the following statements as (S) for Subjective, (O) for Objective, (A) for
Assessment, and (P) for Plan.
Eg: S Patient reports 4 out of 10 abdominal pain.
1. ___ Todays hemoglobin is 8.0
2. ___ 24 year old male with no past medical history has a 6 out of 10 non-radiating sharp forearm pain with
movement after a fall with outstretched arm, but negative for fractures or displacement on x-ray. Given
absence of swelling, full ROM on exam, and negative imaging, likely not a fracture.
3. ___ Nurse reports that the patient did not eat anything for dinner.
4. ___ On exam, patient appears to be Not in Acute Distress (NAD) and breathing comfortably.
5. ___ Dressing appears clean, dry, and intact.
6. ___ Start the patient on subcutaneous heparin for DVT prophylaxis.
7. ___ CXR taken today was normal.
8. ___ Patient reports not having any bowel movement for the third day in a row.
9. ___ Will consult interventional radiology for a possible central line placement.
10. ___ Patient was taking 1 baby aspirin and multi-vitamin (MVI) per day at home.
11. ___ 70 year old female with no complaints here for an annual follow up. Normal vitals and physical exam.
Patient up to date with immunizations, colonoscopies, DEXA scan, mammogram, and all normal previous pap
smears. No other concerns at this time.
12. ___ Discontinue antibiotics today.
13. ___ Discussed the importance of smoking cessation today.
14. ___ Patient had a shortness of breath (SOB) over night, but no complaints this morning.
15. ___ Follow up in 4 weeks.
Developed by Richard Keyme MD, Class of 2013
ECM 3-4 Students: Preparation
ANSWER KEY
1. O Todays hemoglobin is 8.0
2. A
24 year old male with no past medical history has a 6 out of 10 non-radiating sharp forearm pain with
movement after a fall with outstretched arm, but negative for fractures or displacement on x-ray. Given
absence of swelling, full ROM on exam, and negative imaging, likely not a fracture.
3. S
Nurse reports that the patient did not eat anything for dinner.
4. O On exam, patient appears to be Not in Acute Distress (NAD) and breathing comfortably.
5. O Dressing appears clean, dry, and intact.
6. P
Start the patient on subcutaneous heparin for DVT prophylaxis.
7. O CXR taken today was normal.
8. S
Patient reports not having any bowel movement for the third day in a row.
9. P
Will consult interventional radiology for a possible central line placement.
10. S
Patient was taking 1 baby aspirin and multi-vitamin (MVI) per day at home.
11. A
70 year old female with no complaints here for an annual follow up. Normal vitals and physical exam.
Patient up to date with immunizations, colonoscopies, DEXA scan, mammogram, and all normal previous pap
smears. No other concerns at this time.
12. P
Discontinue antibiotics today.
13. P
Discussed the importance of smoking cessation today.
14. S
Patient had a shortness of breath (SOB) over night, but no complaints this morning.
15. P
Follow up in 4 weeks.
Developed by Richard Keyme MD, Class of 2013
You might also like
- SOAP Note AdviceDocument5 pagesSOAP Note AdviceNico AvellanaNo ratings yet
- Resident Survival GuideDocument104 pagesResident Survival Guidescalixto100% (1)
- Writing SOAP Notes NYCCDocument7 pagesWriting SOAP Notes NYCCmassagekevin100% (2)
- A Road Map For The Soap Note-2021-2022: Name: DobDocument3 pagesA Road Map For The Soap Note-2021-2022: Name: DobDat Phan100% (1)
- Pain Case - SOAP Note (2011)Document2 pagesPain Case - SOAP Note (2011)Alfie Lee100% (3)
- 11 - Dot Phrase Templates HMC ED June 2017 - Rev 9.6.17Document13 pages11 - Dot Phrase Templates HMC ED June 2017 - Rev 9.6.17M100% (1)
- Care Plan Handbook TemplateDocument34 pagesCare Plan Handbook TemplateBreanna Hopkins100% (1)
- Nurs 5018 - Soap Note Chronic IllnessDocument5 pagesNurs 5018 - Soap Note Chronic Illnessapi-308904543No ratings yet
- A. Subjective: 1. Progress NoteDocument3 pagesA. Subjective: 1. Progress NoteEvan100% (1)
- Daily Nursing AssessmentDocument2 pagesDaily Nursing Assessmentkiku_laiNo ratings yet
- Final Check Off Soap NoteDocument4 pagesFinal Check Off Soap Notesana100% (1)
- SOAP Notes Format in EMR: SOAP Stands For Subjective, Objective, Assessment, and PlanDocument2 pagesSOAP Notes Format in EMR: SOAP Stands For Subjective, Objective, Assessment, and PlanNick Jacob100% (7)
- Focused AssessmentDocument5 pagesFocused AssessmentPiyali SahaNo ratings yet
- SOAP Note DiabetesDocument16 pagesSOAP Note Diabetesmichael thorn92% (25)
- Cdiff Case SOAP NoteDocument1 pageCdiff Case SOAP Notetwomintomid0% (1)
- Patient History and Presentation SkillsDocument4 pagesPatient History and Presentation Skillsbnarnold100% (2)
- Physical Exam ChecklistDocument2 pagesPhysical Exam ChecklistRaisah Bint Abdullah100% (5)
- Soap Note 4 DominguezDocument5 pagesSoap Note 4 Dominguezapi-320062911100% (1)
- The Primary Care of Seizure Disorders: A Practical Guide to the Evaluation and Comprehensive Management of Seizure DisordersFrom EverandThe Primary Care of Seizure Disorders: A Practical Guide to the Evaluation and Comprehensive Management of Seizure DisordersNo ratings yet
- Soap Note Week 1 Sep7Document3 pagesSoap Note Week 1 Sep7dondavis77No ratings yet
- Primary Care Case: Sore ThroatDocument9 pagesPrimary Care Case: Sore Throatarunateja100% (2)
- Med H&P TemplateDocument2 pagesMed H&P TemplatehellayeahNo ratings yet
- H&P For ScriptDocument12 pagesH&P For ScriptAlina KievskyNo ratings yet
- Soap Note - Musculoskeletal and Nervous SystemsDocument2 pagesSoap Note - Musculoskeletal and Nervous SystemsSummer Keller88% (8)
- Soap NotesDocument1 pageSoap Notesjcfx2100% (1)
- Soap Note-Heidi Martinez PedsDocument6 pagesSoap Note-Heidi Martinez PedsHeidi Martinez100% (2)
- Soap Note 5.0Document4 pagesSoap Note 5.0Paulus IskandarNo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Final Practicum - Soap Note 3Document17 pagesFinal Practicum - Soap Note 3api-494643478100% (2)
- Contraception SOAP Note ReviewDocument7 pagesContraception SOAP Note ReviewAnnah AnnNo ratings yet
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Health HistoryDocument19 pagesHealth HistoryAngelene Caliva100% (1)
- Soap Note 3 DominguezDocument6 pagesSoap Note 3 Dominguezapi-320062911No ratings yet
- Powerchart Review Guide v2 1rpDocument6 pagesPowerchart Review Guide v2 1rpapi-224958119No ratings yet
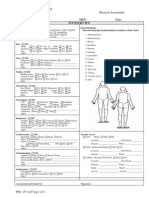
- 2510 - A-07 Nursing Physical AssessmentDocument1 page2510 - A-07 Nursing Physical AssessmentJenNo ratings yet
- Sample Soap NoteDocument12 pagesSample Soap NoteSedaka Donaldson0% (1)
- Nurs 5024 - Soap - Well AdultDocument6 pagesNurs 5024 - Soap - Well Adultapi-308904543100% (1)
- NU 665 Pediatric Gastrointestinal Case Study - Michelle - StewardDocument10 pagesNU 665 Pediatric Gastrointestinal Case Study - Michelle - StewardMichelle StewardNo ratings yet
- ClinicalSurvivalGuide 2012 2013Document62 pagesClinicalSurvivalGuide 2012 2013Zebram Zee100% (1)
- ITP - SOAP Note #1 (Cardiac)Document3 pagesITP - SOAP Note #1 (Cardiac)FrozenMan100% (1)
- Acute Cholecystitis ER AdmissionDocument6 pagesAcute Cholecystitis ER Admissionjessica100% (5)
- Internal Medicine Admission NoteDocument3 pagesInternal Medicine Admission NoteBui Hua Nhu TrongNo ratings yet
- NEONATAL NURSE PRACTITIONER: Passbooks Study GuideFrom EverandNEONATAL NURSE PRACTITIONER: Passbooks Study GuideNo ratings yet
- Intern Survival Guide 2012-2013Document23 pagesIntern Survival Guide 2012-2013alaa100% (1)
- Sample Soap NoteDocument7 pagesSample Soap Notesedaka260% (1)
- Final Product NUR 248 Care PlanDocument22 pagesFinal Product NUR 248 Care PlanJennifer AltenburgNo ratings yet
- Soap NotesDocument7 pagesSoap NotesCharles Ravan80% (5)
- Documentation for Skilled Nursing & Long-Term Care: A Guide for Occupational TherapistsFrom EverandDocumentation for Skilled Nursing & Long-Term Care: A Guide for Occupational TherapistsNo ratings yet
- SOAP PracticeDocument2 pagesSOAP PracticeAnna Madorskaya100% (2)
- Adult - Case StudyDocument14 pagesAdult - Case Studyapi-494643478100% (2)
- Head To Toe AssessmentDocument7 pagesHead To Toe AssessmentShine TorricerNo ratings yet
- Head To Toe Assessment Guide ToolDocument3 pagesHead To Toe Assessment Guide Toolkezia_lillyNo ratings yet
- Cardiac AssessmentDocument7 pagesCardiac AssessmentBryan Mae H. Degorio75% (4)
- Peds - Soap Note 5Document3 pagesPeds - Soap Note 5api-546259691No ratings yet
- SBAR TemplateDocument1 pageSBAR TemplateBella SmithNo ratings yet
- m6 Endocrine System - Lesson 1 HormonesDocument32 pagesm6 Endocrine System - Lesson 1 HormonesJunimar AggabaoNo ratings yet
- Bangkok, Thai Krung Thep, City, Capital, and Chief Port ofDocument17 pagesBangkok, Thai Krung Thep, City, Capital, and Chief Port ofBoracu BoracuNo ratings yet
- Junal ScreeningDocument9 pagesJunal ScreeningRama BayuNo ratings yet
- Barber 1961Document12 pagesBarber 1961mariavardehNo ratings yet
- POST ACTIVITY REPORT-MH Caravan-PalananDocument5 pagesPOST ACTIVITY REPORT-MH Caravan-PalananKeith Clarence BunaganNo ratings yet
- B Cells and T Follicular Helper Cells Mediate Response To Checkpoint Inhibitors in High Mutation Burden Mouse Models of Breast CancerDocument38 pagesB Cells and T Follicular Helper Cells Mediate Response To Checkpoint Inhibitors in High Mutation Burden Mouse Models of Breast CancerRoger FigueiredoNo ratings yet
- Assignment 1Document2 pagesAssignment 1Ayessa GomezNo ratings yet
- ICOIN2022 Program Book v8 20220112Document32 pagesICOIN2022 Program Book v8 20220112Vi VuVoNo ratings yet
- Concrete Cutter Procedure Rev.2Document9 pagesConcrete Cutter Procedure Rev.2Jennifer JavierNo ratings yet
- CocaineDocument2 pagesCocainecarlitog782No ratings yet
- Management of Infant with GastroschisisDocument2 pagesManagement of Infant with GastroschisisAnonymous 9wHscMNo ratings yet
- Jarvis 2017Document5 pagesJarvis 2017drelvNo ratings yet
- Empathy For Service: Benefits, Unintended Consequences, and Future Research AgendaDocument15 pagesEmpathy For Service: Benefits, Unintended Consequences, and Future Research AgendaBojana VulasNo ratings yet
- PriceList MOHDocument1,574 pagesPriceList MOHpharmacymuntasirNo ratings yet
- Introduction to OSH Standards and Enforcement in the PhilippinesDocument4 pagesIntroduction to OSH Standards and Enforcement in the Philippinesfatima ramosNo ratings yet
- Values Restoration Parreno Weeks 1&2Document3 pagesValues Restoration Parreno Weeks 1&2Shirley Robles ParrenoNo ratings yet
- BTech Major Project Design ConstraintsDocument2 pagesBTech Major Project Design ConstraintsgfgfghNo ratings yet
- Johnson Jerry Alan Chinese Medical Qigong Therapy Vol 5-261-280Document20 pagesJohnson Jerry Alan Chinese Medical Qigong Therapy Vol 5-261-280toanbauNo ratings yet
- Finite Element Analysis of Occlusal Splint Therapy in Patients With BruxismDocument9 pagesFinite Element Analysis of Occlusal Splint Therapy in Patients With Bruxismwirda yunita darwisNo ratings yet
- Effect of Therapeutic Exercises On Pregnancy-Related Low Back Pain and Pelvic Girdle Pain: Secondary Analysis of A Randomized Controlled TrialDocument7 pagesEffect of Therapeutic Exercises On Pregnancy-Related Low Back Pain and Pelvic Girdle Pain: Secondary Analysis of A Randomized Controlled TrialSUCIUNo ratings yet
- Social Cognitive TheoryDocument33 pagesSocial Cognitive TheoryNurse and Holistic CareNo ratings yet
- Thesis Topics in GynecologyDocument5 pagesThesis Topics in Gynecologyxdkankjbf100% (2)
- Sas of DR Mohan C. RegmiDocument2 pagesSas of DR Mohan C. Regmisrijan consultancyNo ratings yet
- Library Essay in EnglishDocument4 pagesLibrary Essay in Englishbopajagenal2100% (2)
- Toxic Responses To The LiverDocument18 pagesToxic Responses To The LiversaiibelievesNo ratings yet
- Assessment of Knowledge Sharing For Prevention of Hepatitis Viral Infection Among Students of Higher Institutions of Kebbi State, NigeriaDocument9 pagesAssessment of Knowledge Sharing For Prevention of Hepatitis Viral Infection Among Students of Higher Institutions of Kebbi State, NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- TuberculosisDocument12 pagesTuberculosisanon ymousNo ratings yet
- Blind Suctioning For BeginnersDocument7 pagesBlind Suctioning For BeginnersMark HammerschmidtNo ratings yet
- Safety Data Sheet: Dyestone Printgen XA-301Document4 pagesSafety Data Sheet: Dyestone Printgen XA-301unisourcceeNo ratings yet
- Monitor Mediana Lucon m30Document150 pagesMonitor Mediana Lucon m30lgflousaNo ratings yet