Professional Documents
Culture Documents
Hiponatriemia
Uploaded by
Mihaela MocanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hiponatriemia
Uploaded by
Mihaela MocanCopyright:
Available Formats
Case Rep Nephrol Urol 2013;3:4650
DOI: 10.1159/000350910
Published online: April 19, 2013
2013 S. Karger AG, Basel
16645510/13/00310046$38.00/0
www.karger.com/cru
This is an Open Access article licensed under the terms of the Creative Commons AttributionNonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the
online version of the article only. Distribution for non-commercial purposes only.
Hyponatremia A Rare but Serious
Complication of Amiodarone: A Case
Report and Review of the Literature
Linh Phama
a
Andrea J. Shaera
Thomas Marnejona, b
Department of Medicine, St. Elizabeth Health Center, Youngstown, Ohio, and
Department of Medicine, Northeast Ohio Medical University, Rootstown, Ohio, USA
Key Words
Amiodarone Hyponatremia Syndrome of inappropriate antidiuretic hormone secretion
Side effect
Abstract
Introduction: Hyponatremia secondary to the syndrome of inappropriate antidiuretic
hormone secretion (SIADH) during amiodarone therapy is a rare but potentially lethal
adverse effect. We report a case of severe hyponatremia associated with amiodarone, and
discuss its clinical implications. Case Report: An 84-year-old Caucasian man with a past
medical history of hypertension and diabetes was admitted to the hospital with a non-ST
elevation myocardial infarction. He underwent coronary artery bypass graft and developed
atrial fibrillation on postoperative day 2. A loading dose of amiodarone followed by a
maintenance dose was started. The serum sodium level was 136 mmol/l at discharge and
subsequently decreased to 105 mmol/l 11 days later, at which time the patient represented
with altered mental status. The diagnosis of SIADH was made based on euvolemic hypoosmotic hyponatremia, lack of any other medication known to cause SIADH and urine that was
less than maximally dilute. The serum sodium increased gradually to 123 mmol/l after 36 h of
treatment with hypertonic saline, demeclocycline and fluid restriction. Conclusion: SIADHinduced hyponatremia associated with amiodarone occurs rarely. Since severe hyponatremia
is associated with significant neurological damage and mortality, clinicians should carefully
monitor serum sodium during amiodarone therapy.
Thomas Marnejon, DO
Department of Medicine, St. Elizabeth Health Center
1044 Belmont Avenue
Youngstown, OH 44504 (USA)
E-Mail thomas_marnejon@hmis.org
47
Case Rep Nephrol Urol 2013;3:4650
DOI: 10.1159/000350910
2013 S. Karger AG, Basel
www.karger.com/cru
Pham et al.: Hyponatremia A Rare but Serious Complication of Amiodarone: A Case
Report and Review of the Literature
Introduction
Amiodarone is an effective antiarrhythmic agent with well-known noncardiac toxicities
including pulmonary fibrosis, hypo- or hyperthyroidism, liver function abnormalities,
corneal deposits and photosensitivity. Hyponatremia secondary to the syndrome of
inappropriate antidiuretic hormone secretion (SIADH) during amiodarone therapy is a rare
but potentially lethal adverse effect of this drug. We describe the lowest reported serum
sodium level due to amiodarone therapy. We also review the previously reported cases of
SIADH-induced hyponatremia secondary to amiodarone and discuss salient clinical
implications.
Case Report
An 84-year-old Caucasian man with a past medical history of hypertension and diabetes
was admitted to the hospital with a non-ST elevation myocardial infarction. Urgent left heart
catheterization showed multivessel disease, and the patient subsequently underwent
coronary artery bypass graft. On postoperative day 2, the patient developed atrial fibrillation
with rapid ventricular response. He was started on intravenous amiodarone with a loading
dose of 150 mg, followed by a continuous infusion of 1 mg/min. After 24 h, intravenous
amiodarone was discontinued and switched to 400 mg orally every 8 h. The oral dose of
amiodarone was tapered over 7 days to 400 mg daily. The patients atrial fibrillation
converted to normal sinus rhythm after the loading dose of amiodarone. He was discharged
on postoperative day 7 on amiodarone 400 mg daily. At the time of discharge, his serum
sodium was 136 mmol/l.
The patient then presented to the emergency room 11 days later due to altered mental
status, weakness and loss of appetite. He was drowsy but arousable. Physical examination
revealed normal vital signs and euvolemic status. There was no orthostatic blood pressure
change. A neurological examination showed no focal deficit. Laboratory data revealed a
serum sodium level of 105 mmol/l. Renal and liver function tests were normal. Thyroid
stimulating hormone and cortisol levels were 0.7 IU/ml (normal range: 0.3505.000
IU/ml) and 16 g/dl (normal range: 3.0922.40 g/dl), respectively. Serum osmolality was
228 mOsm/kg and urine osmolality was 251 mOsm/kg. It was noted that the patient was on
furosemide 20 mg daily prior to his admission. Repeat testing after discontinuation of
furosemide revealed a serum osmolality of 256 mOsm/kg and a urine osmolality of 506
mOsm/kg. The fractioned excretion of sodium was greater than 1% and the urine sodium
was 124 mmol/l.
The diagnosis of SIADH was made based on euvolemic hypoosmotic hyponatremia, with
a urine osmolality greater than the serum osmolality, urine sodium level greater than 40
mmol/l, normal thyroid and adrenal function and the absence of other medications known
to cause SIADH. The patient was initially treated with hypertonic (3%) saline. His serum
sodium increased gradually to 117 and 123 mmol/l after 36 and 48 h of treatment,
respectively. Hypertonic saline was discontinued after 3 days, and demeclocycline was
added, together with fluid restriction. The patients mental status improved and his serum
sodium normalized after 10 days of treatment (fig. 1).
48
Case Rep Nephrol Urol 2013;3:4650
DOI: 10.1159/000350910
2013 S. Karger AG, Basel
www.karger.com/cru
Pham et al.: Hyponatremia A Rare but Serious Complication of Amiodarone: A Case
Report and Review of the Literature
Discussion
SIADH was first reported by Schwartz et al. in 1957 [1] in patients with bronchogenic
carcinoma and meningitis. In 1971, four cases of chlorpropamide-induced hyponatremia
were described by Weissman et al. [2]. Since then, a variety of drugs have been added to the
list of drugs that cause SIADH [3].
Amiodarone, a benzofuran derivative, was developed by a Belgian company (Labaz) in
1961 by the chemists Tondeur and Binon as an antianginal drug [4]. A few years later,
amiodarone was widely used as an antiarrhythmic drug in Europe and other countries. It
was not until the mid-1980s that amiodarone was approved by the FDA as a class III
antiarrhythmic agent in the United States. In 1996, the first case of amiodarone-induced
hyponatremia was reported [5]. Since then, a total of 10 cases of amiodarone-induced SIADH
have been published in the literature (table 1; [613]).
The mechanism of SIADH-induced hyponatremia secondary to amiodarone is unclear
[11]. It could possibly be due to the independent secretion of arginine vasopressin relative to
plasma osmolality, full suppression of secretion of this hormone or mutations of the
aquaretic (i.e. water channel regulating) vasopressin receptor [3]. Most medications cause
SIADH either by sensitizing the kidneys to antidiuretic hormone, by stimulating the release
of antidiuretic hormone or by both [14]. Of note, Shavit and Sherer [11] speculated that
amiodarone might induce SIADH by its channel-modulating properties on either renal or
neural tissues.
Among the 10 reported cases, the majority of patients were elderly men (8 out of 10)
with a median age of 69 years. Age and sex may be contributing factors to amiodaroneinduced SIADH. The elderly appear to be particularly at risk for drug-induced SIADH [14]. In
a study on 736 cases of selective serotonin re-uptake inhibitor-induced SIADH, 75% of
patients were over 65 years of age [15].
The duration of time from the initiation of amiodarone to the development of SIADH
varied from 3 days to 6 months in the reported cases. The onset of hyponatremia ranged
from day 3 to day 11 in patients who received loading doses of amiodarone. In contrast,
hyponatremia occurred at 14 days to 6 months in patients receiving maintenance doses. In 7
cases, the serum sodium level normalized within 714 days after discontinuation of
amiodarone and fluid restriction. It appears that amiodarone-induced SIADH is more
prevalent after a loading dose of the drug. However, because of the long half-life of
amiodarone, the cumulative effect on the development of SIADH remains undefined.
Acute, severe hyponatremia (serum sodium <125 mmol/l) has been associated with
serious sequelae, including confusion, hallucinations, seizures, coma and respiratory failure
leading to death [3]. The degree of hyponatremia in the majority of reported cases of
amiodarone-induced SIADH was 110120 mmol/l. In 2 cases, Paydas et al.s [10] and our
case, serum sodium levels were less than 110 mmol/l (107 and 105 mmol/l, respectively). It
is important to note that in hospitalized patients, the mortality was 28% in patients with
serum sodium <125 mmol/l and 50% in patients with serum sodium level <115 mmol/l
[16]. Therefore, amiodarone-induced SIADH is a rare but lethal adverse effect, which occurs
predominantly in elderly patients, who typically have multiple comorbidities, especially
cardiovascular diseases, for which the drug is used.
The only definitive treatment of SIADH is the elimination of its underlying cause [3, 14].
In all but 3 cases, amiodarone was discontinued and fluid restriction was instituted. In the
remaining cases, the dose was decreased. One patient required hemodialysis due to
decreasing serum sodium coupled with the development of altered mental status [12].
49
Case Rep Nephrol Urol 2013;3:4650
DOI: 10.1159/000350910
2013 S. Karger AG, Basel
www.karger.com/cru
Pham et al.: Hyponatremia A Rare but Serious Complication of Amiodarone: A Case
Report and Review of the Literature
To our knowledge, a total of 10 cases of amiodarone-induced SIADH have been reported
thus far in the literature. This adverse effect can occur as early as 3 days after receiving a
loading dose or as late as 6 months in patients on maintenance doses. Age and male sex
appear to be contributing factors. The severity of hyponatremia is directly correlated with
increased mortality in the hospitalized patient. Therefore, clinicians should be aware of this
important complication when treating patients with amiodarone.
References
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
Schwartz WB, Bennett W, Curelop S, Bartter FC: A syndrome of renal sodium loss and hyponatremia
probably resulting from inappropriate secretion of antidiuretic hormone. Am J Med 1957;23:529542.
Weissman PN, Shenkman L, Gregerman RI: Chlorpropamide hyponatremia: drug-induced inappropriate
antidiuretic-hormone activity. N Engl J Med 1971;284:6571.
Ellison DH, Berl T: Clinical practice. The syndrome of inappropriate antidiuresis. N Engl J Med
2007;356:20642072.
Deltour G, Binon F, Tondeur R, Goldenberg C, Henaux F, Sion R, Deray E, Charlier R: Studies in the
benzofuran series. VI. Coronary-dilating activity of alkylated and aminoalkylated derivatives of 3benzoylbenzofuran (in French). Arch Int Pharmacodyn Ther 1962;139:247254.
Munoz Ruiz AI, Calvo Elipe A, Guerrero Vega E, Gorgojo Martinez JJ, Vera Lopez E, Gilsanz Fernandez C:
Pancreatitis and inappropriate ADH secretion syndrome associated with amiodarone (in Spanish). An Med
Interna 1996;13:125126.
Aslam MK, Gnaim C, Kutnick J, Kowal RC, McGuire DK: Syndrome of inappropriate antidiuretic hormone
secretion induced by amiodarone therapy. Pacing Clin Electrophysiol 2004;27:831832.
Ikegami H, Shiga T, Tsushima T, Nirei T, Kasanuki H: Syndrome of inappropriate antidiuretic hormone
secretion (SIADH) induced by amiodarone: a report on two cases. J Cardiovasc Pharmacol Ther 2002;7:
2528.
Odeh M, Schiff E, Oliven A: Hyponatremia during therapy with amiodarone. Arch Intern Med
1999;159:25992600.
Patel GP, Kasiar JB: Syndrome of inappropriate antidiuretic hormone-induced hyponatremia associated
with amiodarone. Pharmacotherapy 2002;22:649651.
Paydas S, Araz F, Balal M: SIADH induced by amiodarone in a patient with heart failure. Int J Clin Pract
2008;62:337.
Shavit E, Sherer Y: Hyponatremia induced by amiodarone therapy. Isr Med Assoc J 2007;9:564565.
Singla S, Strobel AL, Deshmukh AJ, Paydak H: Amiodarone-related hyponatremia: rare but potentially lethal.
Am J Ther 2011, E-pub ahead of print.
Afshinnia F, Sheth N, Perlman R: Syndrome of inappropriate antidiuretic hormone in association with
amiodarone therapy: a case report and review of literature. Ren Fail 2011;33:456458.
Belton K, Thomas SH: Drug-induced syndrome of inappropriate antidiuretic hormone secretion. Postgrad
Med J 1999;75:509510.
Liu BA, Mittmann N, Knowles SR, Shear NH: Hyponatremia and the syndrome of inappropriate secretion of
antidiuretic hormone associated with the use of selective serotonin reuptake inhibitors: a review of
spontaneous reports. CMAJ 1996;155:519527.
Gill G, Huda B, Boyd A, Skagen K, Wile D, Watson I, van Heyningen C: Characteristics and mortality of severe
hyponatraemia a hospital-based study. Clin Endocrinol (Oxf) 2006;65:246249.
50
Case Rep Nephrol Urol 2013;3:4650
DOI: 10.1159/000350910
2013 S. Karger AG, Basel
www.karger.com/cru
Pham et al.: Hyponatremia A Rare but Serious Complication of Amiodarone: A Case
Report and Review of the Literature
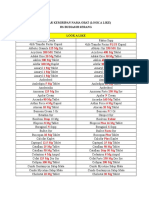
Table 1. Summary of the 10 cases of SIADH induced by amiodarone reported in the literature, including the
present case
First author
Age/
sex
Doses of amiodarone
Lowest
Time to
Treatment
sodium level develop
mmol/l
hyponatremia
Munoz Ruiz [5]
Odeh [8]
Patel [9]
Ikegami [7]
67/F
62/F
67/M
63/M
82/M
NA
300 mg qd
200 mg qd
800 mg qd
200 mg 7 days and 100 mg qd
110
120
117
119
121
4 months
6 months
3 months
7 days
15 days
Aslam [6]
Shavit [11]
Paydas [10]
Singla [12]
Afshinnia [13]
72/M
85/M
58/M
58/M
66/M
2 g qd
NA
NA
1,600 mg qd
IV 150 mg bolus then 900 mg
drip then 1,200 mg PO qd
84/M IV 150 mg bolus + drip, then PO
1,200 mg 7 days then 400 mg
qd
117
122
107
120
116
5 days
30 days
5 months
3 days
7 days
105
11 days
Pham et al. [this
report]
Day until serum
sodium level
normalized
D/C
Unknown
D/C
5 days
Fluid restriction + D/C
3 days
Decrease to 100 mg + fluid restriction 28 days
Continue 100 mg qd + fluid
14 days
restriction
Decrease dose to 200 mg qd
14 days
D/C
A few days
D/C
14 days
D/C and dialysis
D/C
16 days
D/C + 3% NaCl 3 days then fluid
restriction + demeclocycline
10 days
qd = Daily; NA = not available; D/C = amiodarone discontinued.
Fig. 1. Change in the serum sodium concentration with time. Note the serum sodium level nadir on day
17.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Videbeck Psychiatric NSG HandoutsDocument32 pagesVidebeck Psychiatric NSG Handoutskishor100% (4)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Pharmacology AbbreviationsDocument2 pagesPharmacology AbbreviationsChiisanaPlays LIFEAFTERNo ratings yet
- ER Diagram Case StudyDocument4 pagesER Diagram Case StudyRishikesh MahajanNo ratings yet
- CoatingDocument28 pagesCoatingVikrant Saluja0% (1)
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocument8 pagesPractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses Central100% (4)
- 15 Ruggeri2001Document1 page15 Ruggeri2001Mihaela MocanNo ratings yet
- 10 Bianchi2008Document4 pages10 Bianchi2008Mihaela MocanNo ratings yet
- Barbarawi 2019Document10 pagesBarbarawi 2019Mihaela MocanNo ratings yet
- Oral Anticoagulant Therapy-When Art Meets Science: Clinical MedicineDocument17 pagesOral Anticoagulant Therapy-When Art Meets Science: Clinical MedicineMihaela MocanNo ratings yet
- Hemochromatosis and HCCDocument4 pagesHemochromatosis and HCCMihaela MocanNo ratings yet
- Diagnosis and Management of Hyponatremia in Acute Illness PDFDocument13 pagesDiagnosis and Management of Hyponatremia in Acute Illness PDFMihaela MocanNo ratings yet
- Acosta 2003Document5 pagesAcosta 2003Mihaela MocanNo ratings yet
- Differentiating SIADH From Cerebral - Renal Salt Wasting - Failure of The Volume Approach and Need For A New Approach To HyponatremiaDocument9 pagesDifferentiating SIADH From Cerebral - Renal Salt Wasting - Failure of The Volume Approach and Need For A New Approach To HyponatremiaMihaela MocanNo ratings yet
- Eur Heart J 2007 Paulus 2539 50Document12 pagesEur Heart J 2007 Paulus 2539 50Mihaela MocanNo ratings yet
- A Case of Von Hippel Lindau Disease With ColorectalDocument6 pagesA Case of Von Hippel Lindau Disease With ColorectalMihaela MocanNo ratings yet
- Circ Arrhythm Electrophysiol 2014 Barana 861 8Document29 pagesCirc Arrhythm Electrophysiol 2014 Barana 861 8Mihaela MocanNo ratings yet
- Eur J Heart Fail 2008 Grewal 252 9Document8 pagesEur J Heart Fail 2008 Grewal 252 9Mihaela MocanNo ratings yet
- 2008 Guidelines For Device-Based Therapy of Cardiac Rhythm AbnormalitiesDocument2 pages2008 Guidelines For Device-Based Therapy of Cardiac Rhythm AbnormalitiesMihaela MocanNo ratings yet
- Missouri Counties Sue Drug Companies Over Opioid CrisisDocument274 pagesMissouri Counties Sue Drug Companies Over Opioid CrisisSam ClancyNo ratings yet
- Drug Related Problems: A Systemic Literature ReviewDocument7 pagesDrug Related Problems: A Systemic Literature ReviewBaru Chandrasekhar RaoNo ratings yet
- AspirinDocument15 pagesAspirinJuan PerezNo ratings yet
- Harga Beli Mersifarma Ekatalog 2019Document3 pagesHarga Beli Mersifarma Ekatalog 2019Jemmy GeraldzNo ratings yet
- BP IbadurrahmanDocument7 pagesBP Ibadurrahmanvani melianiNo ratings yet
- Siap Print Untuk SimulasiDocument3 pagesSiap Print Untuk SimulasiRossa patria NandaNo ratings yet
- TERIPARATIDE Dosage and Safety GuidelinesDocument1 pageTERIPARATIDE Dosage and Safety Guidelinessimpy989071No ratings yet
- UV GlibenclamideDocument6 pagesUV GlibenclamideGeraldi CoolNo ratings yet
- NarcoticsDocument8 pagesNarcoticsLudovico Fernandez PeRalta IIINo ratings yet
- Depo Medrol 80 MG - Google SearchDocument1 pageDepo Medrol 80 MG - Google SearchMohammad AamirNo ratings yet
- Total Knee Replacement Manual and Therapy/Rehab Protocol: Dr. Edward Kelly, MD, MBADocument12 pagesTotal Knee Replacement Manual and Therapy/Rehab Protocol: Dr. Edward Kelly, MD, MBAJasleen KaurNo ratings yet
- SVKM Information HandoutDocument2 pagesSVKM Information HandoutKshitij TrivediNo ratings yet
- Mike Feuer Opioids SuitDocument165 pagesMike Feuer Opioids SuitPaul GlickmanNo ratings yet
- ZoladexDocument2 pagesZoladexمحمد الزناتيNo ratings yet
- Pdrugs and P TreatmentDocument64 pagesPdrugs and P TreatmentWendz BouvierNo ratings yet
- List High AlertDocument11 pagesList High Alertputiasri85No ratings yet
- Obat Beta BlockerDocument3 pagesObat Beta BlockerLisa RosulliaNo ratings yet
- Paracetamol Biogesic Analgesic AntipyreticDocument8 pagesParacetamol Biogesic Analgesic AntipyreticGian Era100% (1)
- Formulation and Evaluation of Solid Dispersion For Anti Hypertensive DrugDocument12 pagesFormulation and Evaluation of Solid Dispersion For Anti Hypertensive DrugdadaNo ratings yet
- Journal Hemophilia 3Document7 pagesJournal Hemophilia 3Sastra SinagaNo ratings yet
- Chen 2018Document7 pagesChen 2018Victor MocioiuNo ratings yet
- The Delayed Dissolution of Paracetamol Products in The Canine Fed Stomach Can Be Predicted in Vitro But It Does Not Affect The Onset of Plasma LevelsDocument7 pagesThe Delayed Dissolution of Paracetamol Products in The Canine Fed Stomach Can Be Predicted in Vitro But It Does Not Affect The Onset of Plasma LevelsCendanaaNo ratings yet
- Price List of Zubit Life Care - A Pharma Company, Franchise in Pharma and PCD Pharma Company.Document6 pagesPrice List of Zubit Life Care - A Pharma Company, Franchise in Pharma and PCD Pharma Company.Zubit Life Care, PCD Pharma Company, PCD Pharma Franchise, Pharma Franchise CompanyNo ratings yet
- OkokosDocument3 pagesOkokoskaulauNo ratings yet
- Day Care Dental Anesthesia for Minor ProceduresDocument20 pagesDay Care Dental Anesthesia for Minor Proceduresramanrajesh83No ratings yet