Professional Documents
Culture Documents
A Physicist's Role in Patient Healthcare
Uploaded by
BobCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Physicist's Role in Patient Healthcare
Uploaded by
BobCopyright:
Available Formats
The Scientist Training Programme (STP)
Jodie Schultz, Stephen Milner
STP Trainees, Medical Physics, Mount Vernon Hospital, Northwood, Middlesex.
What is the STP?
Radiotherapy Patient Pathway
The Scientist Training Programme (STP) is a post-graduate training
scheme for those wishing to become registered clinical scientists.
The course takes three years to complete, combining academic
elements with work-based learning, and continuous assessment.
Academic learning A masters degree in Medical Physics &
Engineering is completed within the 3 years.
Work based learning An online portfolio is created as evidence of
being competent in the areas required of a Medical Physicist.
Trainees spend the first year of the course rotating through four
different specialisms: radiotherapy, imaging with ionising
radiation, radiation safety, and imaging with non-ionising
radiation. This gives the trainee a chance to see and to learn the
basics of the areas in which medical physicists can be involved.
A patient who is diagnosed with cancer may be referred for
radiotherapy.
Radiotherapy makes use of ionising radiation emitted from a
Linac or other source to precisely treat cancer while sparing the
healthy surrounding tissue.
Images of the tumour site are taken using a CT, MRI or PET
scanner to provide anatomical information in 3D. This is then
used to plan the patients treatment.
Radiotherapy Planning
After the first year the trainee will choose one of these subject
areas to specialise in, and they will spend the remainder of the
course working within their chosen subject area. The trainee will
be placed into a hospital or training centre that has the facilities to
provide a complete training experience for them and will decide if
the trainee is competent in the required skills.
Radiotherapy treatments are planned on computers by
physicists and radiographers using specialised software.
The computer software is used to simulate how the radiation
source will operate around the patient during treatment using
their CT scan, allowing the planner to choose where a radiation
dose will be delivered.
A planning CT slice
of a breast with
dose lines visible
At the end of the three years, trainees will be assessed from the
evidence portfolio of competencies they have built up, and a set
of Objective Structured Final Assessments (OSFAs).
If all of these elements have been successfully completed by the
trainee, then they are eligible to apply for national registration as
a healthcare professional.
Quality Assurance
Medical Physics Specialties
Radiotherapy is a treatment, often used to treat cancer, which uses
ionising radiation to target and destroy cancerous cells. During a
short placement in radiotherapy, a trainee will be involved in the
planning of a radiotherapy treatment, as well as the maintenance
and QA of the equipment used for radiotherapy.
Imaging with Ionisation Radiation uses ionising
radiation to view and diagnose medical conditions.
This may be done in the form of diagnostic x-rays or
CT scans. In nuclear medicine, patients are injected
with a radioactive pharmaceutical that targets the
area of interest to make it viewable. A physicists role in this is
crucial due to their expert knowledge of ionising radiation.
Radiation Safety is concerned with all areas of
medicine that use radiation, and is responsible for
the safe use of radiation. This is done through
ensuring that legislation such as IRR99 and IR(ME)R
2000 is being followed, as well as ensuring that
equipment is performing as expected through QA.
Imaging with Non-ionising Radiation includes using ultrasound,
lasers and MRI to view and diagnose medical conditions. Nonionising radiation is not governed by the same legislation as
ionising radiation, and presents different hazards to the patient and
the operator. Physicists must understand these hazards, and must
also understand the equipment and how it works in order to be
able to maintain it and ensure it is performing and being used
optimally.
Quality Assurance (QA) is performed by physicists to ensure
that all the equipment and software in the department is
working as expected.
This includes regularly checking the Linacs themselves, as well
as the treatment planning software.
Several advanced treatment techniques require a physicist to
QA a treatment plan by delivering it on the linac to a special
detector to ensure the plan has transferred to the machine
correctly and is deliverable by the machine.
Finally the Linac and the plan are
ready for the patient to begin their
treatment.
A Varian TrueBeam Linac used to
administer radiotherapy treatments
Scan this link with your phone to view a video on
the physicists role in radiotherapy:
References: NHSCS Website - http://www.nshcs.org.uk/
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Laporan Lplpo Juni 2023Document72 pagesLaporan Lplpo Juni 2023Elvira PidoNo ratings yet
- Kyle Garafolo Resume 2018 Copy - No Contact InfoDocument2 pagesKyle Garafolo Resume 2018 Copy - No Contact Infoapi-425716959No ratings yet
- Handbook - Classification of Medical DevicesDocument46 pagesHandbook - Classification of Medical DevicesRicha RohillaNo ratings yet
- Harga Retail-AgustusDocument7 pagesHarga Retail-AgustusMedia FarmasiNo ratings yet
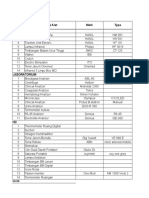
- Nama Alat Merk Type Rehab Medik: Daftar Alat Kalibrasi Rsi At-TinDocument14 pagesNama Alat Merk Type Rehab Medik: Daftar Alat Kalibrasi Rsi At-Tineka febriNo ratings yet
- Ascento Dental Line Catalog Implanturi Alpha Dent GermaniaDocument82 pagesAscento Dental Line Catalog Implanturi Alpha Dent GermaniaGabriela IconaruNo ratings yet
- Basic Components of Radiography Imaging EquipmentDocument24 pagesBasic Components of Radiography Imaging EquipmentEdgardo CayananNo ratings yet
- Comparison Chart: Computed Tomography (CT) ScannersDocument1 pageComparison Chart: Computed Tomography (CT) ScannersRooffNo ratings yet
- Formulir RL5 Halaman 1: Data Peralatan Medik Rumah Sakit ) TAHUN 2010Document7 pagesFormulir RL5 Halaman 1: Data Peralatan Medik Rumah Sakit ) TAHUN 2010putu tiraNo ratings yet
- GE Healthcare: Confirmation of Authorized DistributorshipDocument1 pageGE Healthcare: Confirmation of Authorized DistributorshipAsabila SafilaNo ratings yet
- QuestionDocument3 pagesQuestionSatish PaswanNo ratings yet
- Daftar Obat & Alkes Stok Ruangan IGD: No Nama Obat & Cairan Jumlah NoDocument4 pagesDaftar Obat & Alkes Stok Ruangan IGD: No Nama Obat & Cairan Jumlah Noadyat89No ratings yet
- Otto-Leibinger Dental Instruments CatalogDocument51 pagesOtto-Leibinger Dental Instruments CatalogpuspaNo ratings yet
- Logiq P Series: Make It Easy. Make It Your OwnDocument2 pagesLogiq P Series: Make It Easy. Make It Your OwnNam LeNo ratings yet
- Laparoscopy 2021Document23 pagesLaparoscopy 2021Аташ КочкоровNo ratings yet
- Medigroup Proposal For ICU BedsDocument13 pagesMedigroup Proposal For ICU Bedsmohyeb padamshiNo ratings yet
- Radiography imaging technique using X-raysDocument52 pagesRadiography imaging technique using X-raysPraveen PrasadNo ratings yet
- OPG Machine Manufacturer Offers Dental and Medical Imaging EquipmentDocument6 pagesOPG Machine Manufacturer Offers Dental and Medical Imaging EquipmentVikas MehtaNo ratings yet
- Bulanan Hal-1 IGD LT-1Document192 pagesBulanan Hal-1 IGD LT-1Riio Ibn AmrNo ratings yet
- Mri Scan Sir Ganga Ram Hospital DelhiDocument7 pagesMri Scan Sir Ganga Ram Hospital DelhiAmit SinghNo ratings yet
- The Emergency Trolley: Perhimpunan Dokter Ahli Emergensi IndonesiaDocument30 pagesThe Emergency Trolley: Perhimpunan Dokter Ahli Emergensi IndonesiaAhmad Syamsul ThelionAremaNo ratings yet
- Equipments of Advanced Modalities 1. Mammography System:: 7. Recent Advances in Imaging SystemsDocument1 pageEquipments of Advanced Modalities 1. Mammography System:: 7. Recent Advances in Imaging SystemsProfessor's Tech AcademyNo ratings yet
- Surgical $ Lab 2018 Price ListDocument171 pagesSurgical $ Lab 2018 Price ListDaniel MaikoNo ratings yet
- KENAIKAN HARGA OBAT PER 1 OKTOBER 2015Document2 pagesKENAIKAN HARGA OBAT PER 1 OKTOBER 2015Juon Vairzya AnggraeniNo ratings yet
- VINNO-M86 BrochureDocument6 pagesVINNO-M86 BrochureMedis MEDISNo ratings yet
- Expediente Sanitario Nombre Producto Registro Sanitario Vencimiento Modalidad Estado Registro ObservacionesDocument4 pagesExpediente Sanitario Nombre Producto Registro Sanitario Vencimiento Modalidad Estado Registro ObservacionesFuneRales GaMezNo ratings yet
- Suction ProDocument1 pageSuction Progoodybag HunterNo ratings yet
- Collection of over 30 MRI books and guidesDocument2 pagesCollection of over 30 MRI books and guidesAnto Oi100% (1)
- IV Infusion ProcedureDocument6 pagesIV Infusion ProcedureAnonymous B0c72x2No ratings yet
- Product CatalogDocument2 pagesProduct CatalogIon CirnovNo ratings yet