Professional Documents
Culture Documents
Fatal Leptopsirosis Case
Uploaded by
Fariz NurOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fatal Leptopsirosis Case
Uploaded by
Fariz NurCopyright:
Available Formats
Open Journal of Medical Microbiology, 2013, 3, 12-17
http://dx.doi.org/10.4236/ojmm.2013.31003 Published Online March 2013 (http://www.scirp.org/journal/ojmm)
Fatal Leptospirosis Case in Pediatric Patient:
Clinical Case
Laura I. Santiago Garca1, Citlalli Martnez Cruz1, Irma Zamudio Lugo2,
Beatriz Rivas Snchez3, Oscar Velasco Castrejn3, Joel Navarrete Espinosa1*
1
Coordination of Epidemiologic Surveillance, Unit of Public Health, IMSS, Mexico City, Mexico
Division of Hospital Epidemiologic, Childrens Hospital, CMN Century XXI, IMSS, Mexico City, Mexico
3
Clinic of Tropical Medicine, Unit of Experimental Medicine, School of Medicine, UNAM, Mexico
Email: *joel.navarrete@imss.gob.mx
Received December 6, 2012; revised January 11, 2013; accepted January 31, 2013
ABSTRACT
Introduction: Leptospirosis is a worldwide zoonosis. It is transmitted through the urine of infected animals. Currently,
there is an increase of reports in many countries. In humans, it presents an ample clinical spectrum, which goes from an
asymptomatic infection up to Weil syndrome, which is generally fatal. Clinical Case: A male, 6 years of age, who
started with onset fever and jaundice, handled in private means, diagnosed as viral hepatitis A and was referred to an
institutional hospital where hepatomegaly and splenomegaly were detected. His evolution was towards graveness and,
therefore, he was referred to a third level hospital with reactive Hepatitis diagnosis and to rule out lymphoma. On admission, he presented liver and kidney failure, as well as metabolic acidosis and pulmonary haemorrhage that led to
death 6 hours later. Confirmatory tests for hepatitis were negative; biopsies were taken post-mortem for Leptospira diagnosis, which were positive in liver and kidney. Conclusions: Leptospirosis is a disease that may be manifested in
multiple ways. It is important the understanding of this disease by the physician to improve the diagnosis and, for general population, to avoid exposure. The examination of the epidemiological history of the patient is essential.
Keywords: Leptospirosis; Fatal; Pediatric; Mxico
1. Introduction
Leptospirosis is considered a cosmopolitan zoonosis that
is present in both rural and urbanized areas, where environmental factors conjugate (weather, geographical area,
rivers, rain, etc.) and life styles (close relations with animals) promote their development [1]. Studies performed
by the International Society of Leptospirosis estimate
that each year around half million cases (severe cases) of
this disease are reported worldwide [2]. In Mexico, leptospirosis incidence is not exactly known because there is
not existing a specific surveillance system and only some
cases reported in some entities of the country are considered. However, studies performed in different populations with different techniques report prevalence that go
from 10% up to 63% in the affected population [3-6].
Leptospira is a fine bacterium, 6 to 20 m length,
flexible helical, with extremities as hooks, strictly aerobic, and extremely mobile; it may survive in water, alkaline soil, humid and warm environments. 250 serovares
are known, grouped into 24 serogroups. This bacterium
may remain for long periods in the renal tubules of ap*
Corresponding author.
Copyright 2013 SciRes.
parently healthy animals, being excreted in the urine for
many years, becoming asymptomatic carriers and favouring transmission from animal to animal or from animal to
human [1,2,7].
Humans are infected in a direct form (less frequent) by
the contact of urine and tissue from infected animals
through injured skin, especially feet or nasal and oral
mucosa, or conjunctiva, and an indirect form (epidemic
breakouts) through contact of stagnant water, dirt, or
food contaminated with Leptospira [1].
After an incubation period of 5 to 14 days, the infection may be asymptomatic or may be manifested in an
acute form, and/or become chronic. In its acute form,
symptoms may be undifferentiated or mild, or present a
serious condition known as Weil Syndrome, characterized by liver and kidney failure which commonly lead to
death [7]. The chronic form of the infection has been
known only since few years ago and it may present a
large diversity of clinical manifestations, affecting, in the
same way, different organs [8,9].
The lack of knowledge of the disease, its clinical behaviour and its transmission have conditioned the under
registration of the infection, and, even worse, determines
OJMM
L. I. S. GARCA ET AL.
an inadequate treatment, which redounds in the increase
of complications and lethality. This is especially true
when we consider child population and diseases such as
viral hepatitis, which presents an initial clinical frame
very similar to acute leptospirosis [10,11].
The case of a pediatric patient who sought attention
presenting a symptoms characterized by fever, jaundice,
and hepatitis, who presented a torpid evolution that after
seven days led to his death is presented. The purpose of
the divulging of this information is to better the diagnosis
and treatment of patients seeking medical attention due
to these causes.
2. Clinical Case
A 6-year-old male, living in the city of Queretaro, Queretaro, Mexico, from a medium socio-economic stratum.
2.1. Family Background
Father, 63 years of age, with a post-degree, writer;
mother, 31 years of age, finished high school, housewife.
Both parents apparently healthy and living in free union.
He has three siblings, 4, 3, and 1 year of age, apparently
healthy.
2.2. Pediatric-Clinical Background
He was a first-time, high risk pregnancy product; with
miscarriage threat in the fourth month. The product was
obtained by eutocic delivery at 39 weeks gestation,
weighing 2250 g, 47 cm height, and 8/9 Apgar. He was
breast-fed for 6 months, and then combined with formula
until one year and a half of age, being weaned at 4
months of age. At the age of four months he was hospitalized due to a rotavirus infection. Immunization schedule was complete for his age. Blood type A (-).
2.3. Current Condition
Clinical condition starts on 29/05/2011 with general malaise.
On 01/06/2012 he presents fever higher to 39C without schedule predominance, bilateral cervical lymph
adenopathy, approximately 1 cm, hard consistency and
painful on palpation, he also presented abdominal pain.
At that time he was managed with antipyretic (nimesulide) without an apparent improvement.
Two days later conjunctival jaundice, dark urine, and
acolia appear, so he is taken to a private doctor who
gives a diagnosis of viral hepatitis A and asks for laboratory tests which demonstrate alteration in liver function
(Table 1) and turn positive to antibody-anti-hepatitis A:
IgM and IgG (private laboratory). That same day it is
decided to take him to a second-level institutional hospital in the city of Quertaro, where he is admitted with
Copyright 2013 SciRes.
13
diagnoses of moderate dehydration, viral hepatitis in
study to rule out bicytopenia and lymphoma. On admission, he presented Kramer IV jaundice, bilateral cervical
lymphadenopathy 3 2 cm, mobile and tender to palpation, abdomen with hepatomegaly 3 cm, and mild splenomegaly.
During his hospital stay, platelet units were transfused,
as well as freshly frozen plasma. The abdominal ultrasound performed 4/06/2011 showed moderate hepatomegaly and splenomegaly; the performed serology performed in the hospital against hepatitis A, B, C, and Core
was negative, as well as other studies performed for
rubella, CMV (Cytomegalovirus), toxoplasmosis, coxsackie, Epstein Barr, herpes, and ECHO (enteric cytopathic human virus)
Due to the fast evolution towards graveness, on 5/06/
2011 he was transferred to a third-level hospital in Mexico City, where he was admitted to the ICU (Intensive
Care Unit).
On physical examination, hyperemic pharynx with
greenish postnasal discharge was found, plus submandibular lymphadenopath of approximately 1 cm, fixed to
plans and painful on palpation, the abdomen was soft,
depressible, with decreased peristalisis, and hemapatology and splenomegaly of 3 cm bellow the costal margin.
He required tracheal intubation and central venous catheter.
Six hours after admission in the service, he presented
metabolic acidosis episodes, pulmonary hemorrhage
bleeding visible through the cannula, thus increasing the
ventilation cycles. Chest X-rays presented effacement of
the cost right diaphragmatic angle, suggesting pleural
effusion.
On 06/06/2011 he presented torpid evolution with a
decrease in blood pressure, unresponsive to vasopressors
(dopamine), so he was handled with catecholamines
(adrenaline), showing minimum response. Neurologically, the patient was at that time under barbiturateinduced coma. Hours later, heavy bleeding occurred via
nasogastric tube and irreversible cardiac arrest occurred,
leading to the childs death.
Due to the fact that the tests performed for hepatitis
and other possible agents were negative, post-mortem
samples were taken for the diagnosis of leptospirosis,
which were processed in the laboratory of the Laboratorio de la Clnica de Medicina Tropical from the
Unidad de Medicina Experimental at the Medicine
Faculty from the Universidad Nacional Autnoma de
Mxico. Leptospira search was performed with silver
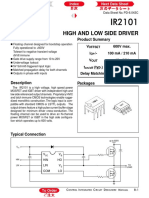
staining of biopsies by Warthin Starry stain, which resulted positive in liver (Figures 1 and 2) and kidney
(Figures 3 and 4), and negative in lymph node. In addition, diagnosis tests were performed to the patients
siblings, which also yielded positive results.
OJMM
L. I. S. GARCA ET AL.
14
Table 1. Laboratory tests performed to the patient according to the attending place.
Particular
2nd Level Hospital
3rd Level Hospital
Date
1.06.2011
2.06.2011
3.06.2011
5.06.2011
6.06.2011
Days of Evolution
Day 3
Day 4
Day 5
Day 7
Day 8
11.3
10.6
CBC
Hemoglobin
14
13.9
12.10
Hematocrit
41
40.4
33.40
Leucocytes
1000
920
1670
Lymphocytes
67
44.8
33
Neutrophiles
42.1
57.70
Eosinophils
0.1
0.2
2.240
19.000
Platelets
30
2200
3000
38.5
59.4
46.7
4.520
30.000
59.000
96
73
111
13
MCV
Blood Chemistry
75
Glucose
Urea
147
65
84
Creatinine
Uric Acid
12.6
Cholesterol
85
82
Triglycerides
304
365
Bilirrubinas
Total Bilirubin
10.5
10.9
14.45
16.95
Direct Bilirubin
8.1
9.7
10.97
12.24
Indirect Bilirubin
2.4
2.5
3.98
4.71
Liver Function Tests
ALT
1145
1408
3010
2410
2106
AST
2571
4154
7550
11460
9976
LDH
3781
1211
Phosphoquinase
161
193
120
98
Alkaline Phosphatase
Serum Electorlytes
Calcium
7.6
6.5
6.5
Sodium
127
133
136
Potasium
5.20
4.90
4.4
Chlorine
100
98
99
Phosphorus
4.4
6.6
Magnesium
Hepatitis Serology
Antibodies
IgM
Positive
IgG
Negative
Copyright 2013 SciRes.
Negative
OJMM
L. I. S. GARCA ET AL.
Figure 1. Leptospira in liver cut.
15
Figure 4. Leptospira in kidney cut.
3. Discussion
Figure 2. Leptospira in liver cut.
Figure 3. Leptospira in kidney cut.
Copyright 2013 SciRes.
In the last decades, leptosirosis has become quite important for it has been recognized that the disease may turn
acute, self-limited, or fatal, presenting a pulmonary hemorrhage or turn into chronic, being able of manifestation
in multiple ways [8,9,12]
Even more, the knowledge of its transmission mechanism has allowed recognizing that the infection is not any
more a professional disease, and it is now known that the
exposure may be from the contact with infected domestic
animals (dogs, cows, pigs) and wild fauna (rats), as well
as with water pollutes with urine of these animals, especially when recreation activities, such as swimming, are
performed or as a consequence of secondary flooding
due to heavy rains; another mechanism that has been
described is bad hygiene habits, such as the intake of
canned food without cleaning it first [13-15].
In this sense, it is more often heard of cases initially
diagnosed with several different diseases, and only after
several studies they were then diagnosed as leptospirosis [10,16]. These facts would be unimportant if the disease were self-limited and innocuous; however, leptospirosis is an infection that entails a high risk of death if
it is not timely diagnosed and treated.
Not knowing the disease and its clinical behaviour, as
well as the factors that condition it, causes the doctor not
to think in this possible diagnosis first, which worsens
when the evolution of the disease is fast and non-specific,
as in the present case in which the patient died before
reaching a diagnosis.
From a medical and epidemiologic point of view, if it
is true that an under registration of the infection is suspected, it is also true that leptospirosis may behave in
multiple ways and may be mixed up with many diseases
(Table 2), which translates in a handicap for the doctor
OJMM
L. I. S. GARCA ET AL.
16
when performing the diagnosis, implying a risk for the
evolution of the patient.
According to the above, the epidemiologic research of
these patients may be of great help to diagnose the disease correctly. In the reported case, there were data that
should have been key for the diagnosis of the disease,
among them, knowing the antecedent of being in contact
with water in a swimming pool that did not met the necessary hygiene conditions previous to the initial clinical
manifestation, as well as living closely with three dogs;
these data were important, especially when the confirmatory studies for infectious Hepatitis performed in the
hospital turned out negative and there was no previous
antecedent of contact with similar cases that could lead to
an outbreak of this viral infection. In this sense, the study
of this disease is important to establish which factors
determine an individual to get sick. It is noteworthy that
in this case, only one of the three infected brothers
suffered a severe condition, which could be related,
among other factors, to the individuals immune mechanisms.
All this highlights the importance of the spreading of
this information to lead the medical doctor towards this
diagnosis and in this way offer a better expectation to the
patient. Never the less, it is not to think in this infection
early, it is necessary the implementation of laboratory
tests that allow us identify on time the bacterium to be
able to treat the patient correctly, especially with clinical
data and laboratory parameter do not make evident great
differences that aid in the diagnosis (Table 3). According
to all the above, it is not redundant to mention the need to
start the use of antibiotics in the first days of evolution of
this infection to avoid its evolution towards graveness,
justifying their use at the mere suspicion of the infection.
Table 2. Differential leptospirosis diagnosis.
Acute Leptospirosis
Chronic Leptospirosis
Influenza
Dengue and hemorrhagic dengue
Hantavirus infections, including hantavirus pulmonary syndrome or other respiratory distress syndromes
Yellow fever and other viral hemorrhagic fevers
Rickettsioses
Borreliosis
Malaria
Typhoid and other enteric fevers
Viral hepatitis
Fever of unknown origin (FUO)
Toxoplasmosis.
Uveitis
Iridiociclitis
CNS alterations
Myelo-proliferative
Table 3. Comparison of laboratory parameters, normal values, hepatites A and patient with leptospirosis.
Laboratory Studies
Reference
Hepatitis A
Pacient
Liver Function
Direct Bilirrubin
0.0 - 0.456 mg/dL
5 - 6 mg/dL
>25 mg/dL (cholestatic hepatitis)
12.24 mg/dL
Transaminase Alanine Transferase
1 - 30 mU/ml
5 - 10 times the normal value
3010 mU/ml
Alkaline Phosphatase
190 - 490 mU/ml
>3 times the normal range
491mU/ml
CBC
Leucocytes
4000 - 11,000 mm
Incremento
16,700 mm3
Limphocytes
35% - 45%
Incremento
38.5 %
Neutrophiles
40% - 50%
Incremento
46.7%
Hemoglobine
10 - 14
14
s/d
Hematocrite
35 - 45
s/d
41
Plateletes
200,000 - 300,000
s/d*
19,000 - 59,000
No data.
Copyright 2013 SciRes.
OJMM
L. I. S. GARCA ET AL.
Leptospirosis is an ailment that is originated by the
close relation with domestic infected animals or water
contaminated with their urine; thus, exposure and infection rate of our population could be very high, which
implies the intentional search for the infection in all those
patients with fever and hepatitis-like data, hemorrhages,
acute kidney failure, which do not fall in a specific diagnosis.
Education and promotion are important for the general
populations health to avoid these risks factor that could
be fatal. In the same way, the magnitude and importance
of this disease justifies thinking in reinforcing a formal
epidemiological surveillance for leptospirosis in Mexico,
to really measure its magnitude and offer the necessary
elements in taking decision in prevention and zoonosis
control.
REFERENCES
[1]
[2]
[3]
[4]
A. R. Bharti, J. E. Nally, J. N. Ricaldi, M. A. Matthias, M.
M. Diaz, M. A. Lovett, et al., Leptospirosis: A Zoonotic
Disease of Global Importance, Lancet Infectious Diseases, Vol. 3, No. 12, 2003, pp. 757-771.
doi:10.1016/S1473-3099(03)00830-2
R. A. Hartskeerl, International Leptospirosis Society:
Objetives and Achievements, Revista Cubana de Medicina Tropical, Vol. 57, No. 1, 2005, pp. 7-10.
I. A. Vado-Sols, M. A. Crdenas-Marrufo, H. LaviadaMolina, F. Vargas-Puerto, J. E. B. Jimnez-Delgadillo y
Zavala-Velzquez, Estudio de Casos Clnicos e Incidencia de Leptospirosis Humana en el Estado de Yucatn,
Mxico Durante el Periodo de 1998-2000, Revista
Biomdica, Vol. 13, No. 3, 2002, pp. 157-164.
C. B. Leal-Castellanos, R. Garca-Surez, E. GonzlezFigueroa, J. L. Fuentes-Allen and J. Escobedo-De la Pea
Risk Factors and the Prevalence of Leptospirosis Infection in a Rural Community of Chiapas, Mxico,
Epidemiol Infect, Vol. 131, No. 3, 2003, pp. 1149-1156.
doi:10.1017/S0950268803001201
[5]
N. E. Joel, M. M. Maribel, R. S. Beatriz and V. C. Oscar,
Leptospirosis Prevalence in a Population of Yucatan,
Mexico, Journal of Pathogens, Vol. 2011, 2011, Article
ID: 408604.
[6]
G. Varela and V. J. Zavala, Estudio Serolgico de la
Leptospirosis en la Repblica Mexicana, Revista del
Instituto de Salubridad y Enfermedades Tropicales, Vol.
21, 1961, pp. 49-52.
Copyright 2013 SciRes.
17
[7]
P. N. Levett, Leptospirosis, In: Mandell, Douglas and
Bennetts, Eds, Principles and Practice of Infectious Diseases, 6th Edition, Elsevier, Churchill Livingstone, 2005,
pp. 2789-2795.
[8]
O. Velasco-Castrejn, B. Rivas-Snchez and H. H. RiveraReyes, Leptospirosis Humana Crnica, In: J. NarroRobles, O. Rivero-Serrano and J. J. Lpez Brcena, Eds.,
Diagnstico y Tratamiento en la Prctica Mdica, 2nd
Edition, Manual Moderno, Mxico, 2006, pp. 641-650.
[9]
C. O. Velasco, S. B. Rivas, J. Espinoza, J. Jimnez and E.
Ruiz, Enfermedades Simuladas y Acompaantes de Leptospirosis, Revista Cubana de Medicina Tropical, Vol.
57, No. 1, 2005, pp. 75-76
[10] M. S. Hernndez, G. R. Menndez, O. M. Torres, J. L. M.
Alonso and J. M. A. Snchez, Leptospirosis en Nios de
una Provincia Cubana, Revista Mexicana de Pediatra,
Vol. 73, No. 1, 2006, pp. 14-17.
[11] S. J. Prez, O. J. Colin, S. A. Caballero and E. A. Cuellar,
Seropositividad a Leptospiras de Pacientes Sospechosos
de Hepatitis Viral Negativos a Marcadores Serolgicos,
Revista Cubana de Medicina Tropical, Vol. 57, No. 1,
2005, pp. 57-58.
[12] R. T. Trevejo, P. J. G. Rigau, D. A. Ashford, E. M. McClure, G. C. Jarquin, J. J. Amador, et al., Epidemic Leptospirosis Associated with Pulmonary Hemorrhage-Nicaragua 1995, The Journal of Infectious Diseases, Vol.
178, No. 5, 1998, pp. 1457-1463. doi:10.1086/314424
[13] C. Manuel, T. Rafael, B. Lourdes, G. Dana, G. Martha
and V. J. M. Brote de, Leptospirosis Asociado a la
Natacin en una Fuente de Agua Subterrnea en Una
Zona Costera, Lima-Per, Revista Peruana de Medicina
Experimental y Salud Pblica, Vol. 26, No. 4, 2009, pp.
441-448.
[14] J. Pradutkanchana, S. Pradutkanchana, M. Kemapanmanus,
N. Wuthipum and Silpapajakul, The Etiology of Acute
Pirexia of Unknown Origin in Children after a Flood,
The Southeast Asian Journal of Tropical Medicine and
Public Health, Vol. 34, No. 1, 2003, pp. 175-178.
[15] E. J. Sanders, J. G. Rigau-Perez, H. L. Smits, C. C. Deseda, V. A. Vorndam, T. Aye, et al.. Increase of Leptospirosis in Dengue Negative Patients after a Hurricane in
Puerto Rico in 1966, The American Journal of Tropical
Medicine and Hygiene, Vol. 61, No. 3, 1999, pp. 399404.
[16] O. Velasco-Castrejn, B. Rivas-Snchez, E. Gutirrez, L.
Chvez, P. Duarte, S. Chavarra, et al., Leptospira Simulador o Causante de Leucemia? Revista Cubana de Medicina Tropical, Vol. 57, No. 1, 2005, pp. 17-24.
OJMM
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Templist Scroll by :dr. Lawiy-Zodok (C) (R) TMDocument144 pagesThe Templist Scroll by :dr. Lawiy-Zodok (C) (R) TM:Lawiy-Zodok:Shamu:-El100% (5)
- Abdomen - FRCEM SuccessDocument275 pagesAbdomen - FRCEM SuccessAbin ThomasNo ratings yet
- Internal Audit ChecklistDocument18 pagesInternal Audit ChecklistAkhilesh Kumar75% (4)
- Respiratory Tract InfectionDocument13 pagesRespiratory Tract InfectionFariz NurNo ratings yet
- Antinuclear Antibodies: When To Test and How To Interpret FindingsDocument4 pagesAntinuclear Antibodies: When To Test and How To Interpret FindingsFariz NurNo ratings yet
- 2015 AHA Guidelines Highlights EnglishDocument36 pages2015 AHA Guidelines Highlights EnglishshiloinNo ratings yet
- (Kasus-Endokrin) (2016!11!10) A Management of Type 2 Diabetes Mellitus and Hyperglycemic Hyperosmolar State in A Patient With Pulmonary Tuberculosis (Ismayadi)Document11 pages(Kasus-Endokrin) (2016!11!10) A Management of Type 2 Diabetes Mellitus and Hyperglycemic Hyperosmolar State in A Patient With Pulmonary Tuberculosis (Ismayadi)Fariz NurNo ratings yet
- Guidelines For The Prevention, Care And... Ic Hepatitis B PDFDocument16 pagesGuidelines For The Prevention, Care And... Ic Hepatitis B PDFFariz NurNo ratings yet
- Frailty, John E. MorleyDocument11 pagesFrailty, John E. MorleyFariz NurNo ratings yet
- Ana TestDocument4 pagesAna TestFariz NurNo ratings yet
- Pathophysiology of AKI BasileDocument99 pagesPathophysiology of AKI BasileFariz NurNo ratings yet
- Activation of The Coagulation Cascade in Patients With LeptospirosisDocument7 pagesActivation of The Coagulation Cascade in Patients With LeptospirosisFariz NurNo ratings yet
- En Wikipedia Org Wiki Absolute Neutrophil CountDocument5 pagesEn Wikipedia Org Wiki Absolute Neutrophil CountFariz NurNo ratings yet
- En Wikipedia Org Wiki Absolute Neutrophil CountDocument5 pagesEn Wikipedia Org Wiki Absolute Neutrophil CountFariz NurNo ratings yet
- Respiratory Tract InfectionDocument13 pagesRespiratory Tract InfectionFariz NurNo ratings yet
- Di, Siadh, CSWDocument17 pagesDi, Siadh, CSWVanitha Ratha KrishnanNo ratings yet
- Di, Siadh, CSWDocument17 pagesDi, Siadh, CSWVanitha Ratha KrishnanNo ratings yet
- Ethionamide-Induced Hypothyroidism in ChildrenDocument3 pagesEthionamide-Induced Hypothyroidism in ChildrenFariz NurNo ratings yet
- Ethionamide-Induced Hypothyroidism in ChildrenDocument3 pagesEthionamide-Induced Hypothyroidism in ChildrenFariz NurNo ratings yet
- Neutrophil GranulocyteDocument16 pagesNeutrophil GranulocyteFariz NurNo ratings yet
- Ptre HT and MortalitasDocument15 pagesPtre HT and MortalitasFariz NurNo ratings yet
- Insiden RematologiDocument11 pagesInsiden RematologiFariz NurNo ratings yet
- H.pylori Dan CA GasterDocument32 pagesH.pylori Dan CA GasterFariz NurNo ratings yet
- Steroid Lupus NefritisDocument3 pagesSteroid Lupus NefritisFariz NurNo ratings yet
- Understanding The Epidemiology SleDocument12 pagesUnderstanding The Epidemiology SleFariz NurNo ratings yet
- Ajg 1998292 ADocument9 pagesAjg 1998292 AFariz NurNo ratings yet
- Bacterial factors and host immune responses in H pylori infectionDocument5 pagesBacterial factors and host immune responses in H pylori infectionFariz NurNo ratings yet
- Death Fariz 2-1-14Document5 pagesDeath Fariz 2-1-14Fariz NurNo ratings yet
- Helicobacter Pylori Eradication: Changes in Gastric Acid Secretion Assayed by Endoscopic Gastrin Test Before and AfterDocument7 pagesHelicobacter Pylori Eradication: Changes in Gastric Acid Secretion Assayed by Endoscopic Gastrin Test Before and AfterFariz NurNo ratings yet
- Factors Associated With ParadoxicalDocument11 pagesFactors Associated With ParadoxicalFariz NurNo ratings yet
- Hyperbaric Oxygen Therapy: ReferenceDocument5 pagesHyperbaric Oxygen Therapy: ReferenceFariz NurNo ratings yet
- Hyperbaric Oxygen Therapy: ReferenceDocument5 pagesHyperbaric Oxygen Therapy: ReferenceFariz NurNo ratings yet
- Garlic Benefits - Can Garlic Lower Your Cholesterol?Document4 pagesGarlic Benefits - Can Garlic Lower Your Cholesterol?Jipson VargheseNo ratings yet
- 1989 GMC Light Duty Truck Fuel and Emissions Including Driveability PDFDocument274 pages1989 GMC Light Duty Truck Fuel and Emissions Including Driveability PDFRobert Klitzing100% (1)
- AI Model Sentiment AnalysisDocument6 pagesAI Model Sentiment AnalysisNeeraja RanjithNo ratings yet
- B. Pharmacy 2nd Year Subjects Syllabus PDF B Pharm Second Year 3 4 Semester PDF DOWNLOADDocument25 pagesB. Pharmacy 2nd Year Subjects Syllabus PDF B Pharm Second Year 3 4 Semester PDF DOWNLOADarshad alamNo ratings yet
- Datasheet PDFDocument6 pagesDatasheet PDFAhmed ElShoraNo ratings yet
- Parts of ShipDocument6 pagesParts of ShipJaime RodriguesNo ratings yet
- Coleman Product PageDocument10 pagesColeman Product Pagecarlozz_96No ratings yet
- Young Women's Sexuality in Perrault and CarterDocument4 pagesYoung Women's Sexuality in Perrault and CarterOuki MilestoneNo ratings yet
- EP - EngineDocument4 pagesEP - EngineAkhmad HasimNo ratings yet
- CAT Ground Engaging ToolsDocument35 pagesCAT Ground Engaging ToolsJimmy Nuñez VarasNo ratings yet
- Gas Natural Aplicacion Industria y OtrosDocument319 pagesGas Natural Aplicacion Industria y OtrosLuis Eduardo LuceroNo ratings yet
- Monster of The Week Tome of Mysteries PlaybooksDocument10 pagesMonster of The Week Tome of Mysteries PlaybooksHyperLanceite XNo ratings yet
- Features Integration of Differential Binomial: DX BX A X P N MDocument4 pagesFeatures Integration of Differential Binomial: DX BX A X P N Mابو سامرNo ratings yet
- Guidance Notes Blow Out PreventerDocument6 pagesGuidance Notes Blow Out PreventerasadqhseNo ratings yet
- Gautam Samhita CHP 1 CHP 2 CHP 3 ColorDocument22 pagesGautam Samhita CHP 1 CHP 2 CHP 3 ColorSaptarishisAstrology100% (1)
- Current Relays Under Current CSG140Document2 pagesCurrent Relays Under Current CSG140Abdul BasitNo ratings yet
- Is.4162.1.1985 Graduated PipettesDocument23 pagesIs.4162.1.1985 Graduated PipettesBala MuruNo ratings yet
- Chap 2 Debussy - LifejacketsDocument7 pagesChap 2 Debussy - LifejacketsMc LiviuNo ratings yet
- Cost Analysis and Financial Projections for Gerbera Cultivation ProjectDocument26 pagesCost Analysis and Financial Projections for Gerbera Cultivation ProjectshroffhardikNo ratings yet
- Discuss The Challenges For Firms To Operate in The Hard-Boiled Confectionery Market in India?Document4 pagesDiscuss The Challenges For Firms To Operate in The Hard-Boiled Confectionery Market in India?harryNo ratings yet
- Telco XPOL MIMO Industrial Class Solid Dish AntennaDocument4 pagesTelco XPOL MIMO Industrial Class Solid Dish AntennaOmar PerezNo ratings yet
- What Is DSP BuilderDocument3 pagesWhat Is DSP BuilderĐỗ ToànNo ratings yet
- The Art of Now: Six Steps To Living in The MomentDocument5 pagesThe Art of Now: Six Steps To Living in The MomentGiovanni AlloccaNo ratings yet
- Magnetic Pick UpsDocument4 pagesMagnetic Pick UpslunikmirNo ratings yet
- PC3 The Sea PeopleDocument100 pagesPC3 The Sea PeoplePJ100% (4)
- Pioneer XC-L11Document52 pagesPioneer XC-L11adriangtamas1983No ratings yet
- CP 343-1Document23 pagesCP 343-1Yahya AdamNo ratings yet