Professional Documents
Culture Documents
Phototherapy For Atopic Dermatitis
Uploaded by
Kadek Widhiana UtamiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Phototherapy For Atopic Dermatitis
Uploaded by
Kadek Widhiana UtamiCopyright:
Available Formats
Clinical dermatology X Review article
Phototherapy for atopic dermatitis
J. Krutmann
Clinical and Experimental Photodermatology, Department of Dermatology, University of Duesseldorf, Germany
Summary
The beneficial effects of ultraviolet (UV) radiation on atopic dermatitis has been
appreciated for many years. While broadband UVB and psoralen UVA have been the
mainstay of phototherapy for some time, the past 5 years have seen the introduction of
phototherapeutic modalities, including UVA-1 and 311nm UVB. The best modality and
mode of usage is dependent on the type of atopic dermatitis, severity and body site. T
lymphocytes play an important role in disease pathogenesis and UV radiation has
profound effects on skin and systemic immune responses.
g and presents clinically as
Concept linked
phototherapy for
atopic dermatitis
Introduction
It has been appreciated for decades that ultraviolet (UV)
radiation may be beneficial for patients with atopicAtopic dermatitis represents
dermatitis. In 1929, the German dermatologist Buschkea T-cell mediated immune
stated that the effect of sea climate on atopic dermatitisresponse directed against
4
allergens.
was `simply surprising', and in the 1940s, Lomhold and inhalant
which
are
Norrlind concluded that most patients with atopic Cytokines,
dermatitis improved during the summer season. Nexmanproduced by in situ helper T
in 1948 was the first to assess systematically the cells present in lesional skin
beneficial effects of phototherapy in atopic dermatitis of patients with atopic
patients, which in his study were exposed to radiation dermatitis, are responsible
from a carbon arc lamp. Modern fluorescent lamps with for the generation and
defined emission spectra for phototherapy of atopic maintenance of skin lesions
dermatitis have been used continuously from the end of in atopic dermatitis patients.
the 1970s until today. During the last 5 years, several newIt has been learned that the
1
phototherapeutic modalities including UVA-1 therapy andquality of the cytokine profile
2
expressed in a patient's skin
311 nm UVB therapy have been introduced. As adepends critically on the
consequence, dermatologists may now select 2 from a stage of this disease. The
diversified spectrum of distinct phototherapeuticpathogenesis
of
atopic
modalities 2 the phototherapy of choice for their particular eczema is best described by
patient. This choice has to be reflected upon thea two-phase model, in which
background of recent pathogenetic concepts.
an initiation phase, which
represents
a
Th2-like
inflammatory response and
which develops without
clinically appar-ent skin
Correspondence: J. Krutmann, Clinical and Experimental Photodermatology,
lesions, is switched into a
University of Duesseldorf, Moorenstrasse 5, D-40225 Duesseldorf, Germany.
second, eczematous phase,
Tel.: 149 211 811 7627. Fax: 149 211 811 8830.
which is dominated by the
E-mail: krutmann@rz.uni-duesseldorf.de
Th1-like cytokine interferon-
552
q 2000 Blackwell Science Ltd X Clinical
and Experimental Dermatology, 25, 552558
eczema.
Based on this twophase model it is now
possible to discriminate
therapeutic
strategies,
directed at the initiation
phase of atopic dermatitis
(and thus in a more
general sense may be
regarded as prophylactic)
from those therapies which
are
directed
at
the
eczematous phase of this
disease,
and
which
provide symptomatic relief
by
down-regulating
interferon-g expression in
lesional
atopic
skin.
Treatments targeted at the
initiation phase of atopic
dermatitis
are
not
available
and
current
phototherapy of atopic
dermatitis as conducted in
daily practice is identical
with
a
symptomatic
treatment
approach
targeted
at
the
eczematous
phase.
Symptomatic phototherapy
needs
Phototherapy for atopic dermatitis X J. Krutmann
Table 1 Phototherapy for atopic dermatitis.
Indication
Modality
Comment
Mode of action
Acute, severe
High-dose UVA-1,
PUVA
Extracorporeal photopheresis
Monotherapy, alternative to
glucocorticosteroids
Symptomatic, antieczematous
Chronic, moderate
311 nm UVB,
UVA/UVB
Low-dose UVA-1
Broad-band UVB
Broad-band UVA
Combination therapy, to save
glucocorticosteroids
Symptomatic, antieczematous, maintenance
therapy
exacerbation
dermatitis.
importantly, cessation of
to be differentiated further into very potent photother-apeutic PUVA
therapy
was
modalities, which are used as a monotherapy for short associated
with
the
periods of time to treat effectively patients with acute, severe occurrence
of
rebound
ecxacerbation of atopic dermatitis, and less effective forms of phenomena in a high
phototherapy, which are successfully used as combination percentage of patients if
regimens over longer periods of time to treat patients with photochemotherapy was not
5
chronic forms of atopic dermatitis. The distinction between combined with systemic
chronic moderate disease and acute severe disease is glucocorticosteroids, or if
arbitrary and in a given clinical situation may not always be as maintenance therapy was
clear as stated above. In order to emphasize the significant not continued for longer
qualitative differences in photo(chemo)therapy regi-mens time intervals extending
used for acute, severe vs. moderate forms of atopic over several years. Longdermatitis, however, this distinction will be made throughout term use of PUVA is of
particular concern in view of
this chapter for didactic reasons.
the relatively young age of
patients
with
atopic
Photo(chemo)therapy for acute, severe atopic dermatitis
and
recent
dermatitis
reports indicate that longPUVA
may
be
In general, symptomatic phototherapy of acute, severe term
associated
with
an
exacerbation of atopic dermatitis may be achieved with
increased
risk
of
developing
systemic PUVA therapy, extracorporeal photochecancer
including
motherapy, and, most importantly, UVA-1 phototherapy skin
possibly
malignant
(Table 1).
9
Systemic photochemotherapy (PUVA) combines the oral melanoma.
Further
administration of psoralens with UVA radiation (henceforth disadvantages result from
referred to by the acronym PUVA; psoralen plus UVAprolonged photosen-sitivity
radiation). Since its introduction into derma-tological requiring
protection
by
phototherapy some 35 years ago, PUVA has been found to sunglasses
to
prevent
be highly effective for the treatment of a variety of skin cataract formation, and the
68
diseases including atopic dermatitis.
Although there is nooccurrence of systemic
doubt that PUVA therapy may be used successfully not onlyside-effects such as nausea
a
relatively
high
for moderate, but also severe and even erythrodermic forms in
of atopic dermatitis, it has to be realized that PUVA therapy of percentage of patients (up
58
this disease is associated with significant disadvantages. to 20%). PUVA therapy is
As com-pared with PUVA therapy of psoriasis, the actual thus of limited use for the
number of treatments required for clearance of atopictreatment of patients with
atopic dermatitis and does
dermatitis was found to be relatively high. Even more
not represent an equivalent
alternative
to
glucocorticosteroids or UVA1
therapy
in
the
management of severe
of
atopic
Evidence
exists
that
extracorporeal
photopheresis may be of
benefit for the management
of patients with severe
atopic
dermatitis.
Extracorporeal
photopheresis consists of
the passage of freshly
drawn blood that contains
photoactivable psoralen (8methoxypsoralen) through
an
extracorporeal
UVA
10
exposure system.
It is
assumed that UVA radiation
activates the pharmacologically
inactive
8methoxypsoralen
which
then is thought to affect the
lymphoyctes
within
the
blood
preparation,
and
subsequently
these
`modulated'
lym-phocytes
are reinfused into the
patient.
Extracorporeal
photopheresis has been
used with some success in
the treatment of patients
with
Sezary
syndrome.
There are also some
indications that it might be
used for the treatment of
several
immunologically
based skin dis-eases such
as graft vs. host disease.
Prinz et al. were the first to
use
extracorporeal
photochemotherapy
success-fully for patients
11
with atopic dermatitis.
They reported three patients
with severe atopic dermatitis
with a
q 2000 Blackwell
and Experimental Dermatology, 25, 552558
Science Ltd X Clinical
553
Phototherapy for atopic dermatitis X J. Krutmann
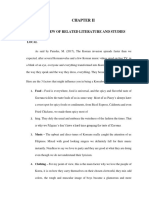
Figure 1 A patient with previously intractable atopic dermatitis before (a) and after (b) extracorporeal photochemotherapy (10 treatment
cycles).
exposed once per day to a
life-long history of atopic dermatitis. Because their disease single dose of 130 J/cm 2
had finally become resistant to conventional therapies, UVA-1 (high-dose UVA-1
extracorporeal photopheresis was started in thesetherapy) for 15 consecutive
patients at 4-week intervals and was found to induce
2
days.
The
therapeutic
clinical improvement of skin lesions associated with a
effectiveness
of
UVA-1
reduction in serum levels of total IgE. Extra-corporeal
therapy was compared to
photochemotherapy was not used as a monotherapeutic
that of a conventional
approach, but was combined with the external use of
UVA/UVB therapy by using
topical prednicarbat which, by itself, was insufficient to
both
modalities
as
a
control disease activity in these patients. These studies
monotherapy:
that
is
have been confirmed in an independent study in which
additional treatment was
three patients with previously intractable atopic dermatitis
restricted in both groups to
were subjected to extracorporeal photochemotherapy in a
12
the
use
of
emollients.
monother-apeutic design. All patients showed prompt Therapeutic effectiveness
improve-ment which was dependent on the frequency ofwas assessed by means of
treatment cycles (Fig. 1). When extracorporeal photo- an
established
clinical
chemotherapy was given twice monthly, a rapid decrease scoring
system
that
in the overall skin score and in serum levels of eosinophil consisted of both a severity
cationic protein and total IgE was observed. Uponand a topographical score,
extension of treatment-free intervals from 2 to 4 weeks, and by monitoring serum
however, these beneficial effects were rapidly lost, butlevels of eosinophil cationic
could be reachieved by use of the 2-weeks treatmentprotein. Serum levels of
schedule. In aggregate these studies suggest thateosinophil cationic protein
extracorporeal photopheresis is effective for the treatmenthad
been
identified
of patients with atopic dermatitis, but controlledpreviously
as
sensitive
randomized studies with a larger number of patients are parameters, which reflect
required to confirm these preliminary observations. Also, disease activity in atopic
this modality is expensive and time consuming anddermatitis, and therefore
therefore its use should be limited to atopic dermatitis were used as objective
patients in which other modalities have proven to be parameters to evaluate the
therapeutic effectiveness of
ineffective.
UVA-1 irradiation. AssessThe therapeutic effectiveness of UVA-1 irradiation in thement of clinical scores
management of patients with atopic dermatitis was first demonstrated that UVA-1
assessed in a pilot study, in which patients with acute, therapy was efficient in
promptly
inducing
an
severe exacerbation of atopic dermatitis were
improve-ment in clinical
symptoms of patients with
atopic dermatitis, and that in
comparison
with
conventional
UVA/UVB
therapy,
significant
differences in favour of
UVA-1
therapy
were
observed after six and 15
2
exposures
(Fig.
2).
Similarly, elevated serum
levels of eosinophil cationic
protein in patients with
atopic
dermatitis
were
decreased significantly by
UVA-1
therapy,
but
remained
essentially
unaltered
in
patients
undergoing
UVA/UVB
therapy. These preliminary
but
promising
results
indicated
that
UVA-1
therapy may represent a
novel
phototherapeutic
modality, which could be
used as a monotherapeutic
approach to treat patients
with
acute,
severe
exacerbation
of
atopic
dermatitis.
Within
the
following
years,
these
original observations have
been
confirmed
by
numerous
uncontrolled,
open, and sometimes even
not
comparative
studies.
1315
However, the pilot
study failed to provide a
direct comparison of
UVA-1 therapy with the
gold standard in the
management of patients
with acute, severe
554
q 2000
Blackwell Science Ltd X Experimental Dermatology, 25, 552558
Clinical and
Phototherapy for atopic dermatitis X J. Krutmann
Figure 2 A patient with severe, acute exacerbation of atopic dermatitis before (a) and after (b) UVA-1 phototherapy (10 130 J/cm ).
corroborated by laboratory
assessments, in which
exacerbation of atopic dermatitis 2 that is the topical useserum levels of eosinophil
of glucocorticosteroids. In a subsequent multicentre trial, a
cationic protein as well as
total of 53 patients were randomly assigned to
peripheral
blood
2
either UVA-1 therapy (once daily 130 J/cm , total eosinophilia
were
10 days) or conventional UVA/UVB therapy [once compared before and after
daily minimal erythema dose (MED)-dependent, total 10 therapy between the three
days] or topical treatment with fluocortolone (once daily,treatment groups
and
16
10 days). To this day, this study is the only one to found to be significantly
provide a multicentric evaluation of the efficacy of UVA-1 decreased after UVA-1
therapy in a controlled randomized fashion. It wasand steroid, but not after
observed that after 10 treatments, patients in all three UVA/UVB therapy. UVA-1
groups had improved, but the decrease in total clinical therapy may thus be used
scores and thus clinical improvement was significantlyas an alternative to
greater in patients receiving glucocorticos-teroid or UVA-1glucocorticoster-oids
to
therapy, as compared with UVA/UVB therapy. Under these treat
severe
atopic
conditions, UVA-1 therapy, as compared with dermatitis.
glucocorticosteroid treatment, was significantly better at UVA-1 therapy may not
day 10 of therapy in reducing the total clinical score. be performed in atopic
These clinical observations were
dermatitis
patients
with
UVA-1-sensitive
dermatitis
or
photodermatoses such as
polymorphic light eruption. It
is necessary to exclude
these diseases prior to
initiation of UVA-1 therapy.
This can be accomplished
easily by photoprovocation
testing. No side-effects have
been observed although the
potential carcinogenic risk is
5
a
theoretical
concern.
Exposure of hairless, albino
Skh-hr1 mice to UVA-1
radiation has been shown to
induce
squamous
cell
carcinoma.
The
actual
contribution
of
UVA-1
radiation to the development
of malignant
atopic
q 2000 Blackwell
and Experimental Dermatology, 25, 552558
Science Ltd X Clinical
555
Phototherapy for atopic dermatitis X J. Krutmann
low-dose UVA-1 therapy are used in mild and moderate
melanoma in humans is currently under debate and at this
point cannot be excluded. Until more is known about UVA-1
therapy, its use should be limited to periods of severe,
acute exacerbation and in general, one treatment cycle
should not exceed 1015 continuously applied exposures
and should not be repeated more than once a year. Under
no circumstances should UVA-1 photother-apy be used for
children (age , 18 years) with atopic dermatitis. In order to
assess potential long-term side-effects of UVA-1
photherapy in a systematic manner, in Europe a
prospective longitudinal study has been started to monitor
patients treated with UVA-1 phototherapy for the
development of skin cancer and photoaging.
There is an ongoing debate whether the therapeutic
effectiveness of UVA-1 therapy is dose dependent. Similar
2
to a high-dose regimen with 130 J/cm , a medium UVA-1
13
dosage schedule seems to be superior to UVA/UVB. A
direct comparison between a low-dose vs. a high-dose
UVA-1 regimen has been performed recently by Simon et
al. (J. C. Simon et al. personal communication). In this
2
open study, a high-dose protocol (130 J/cm ) was superior
2
to a medium-dose regimen (50 J/cm ), which was more
2
efficient than a low-dose schedule (20 J/cm ). The latter
observation is consistent with previous reports that suggest
2
that a medium-dose regimen (50 J/cm ) is superior to a
2 14
low-dose regimen (20 J/cm ).
In addition UVA/UVB
therapy was reported to be superior to a low-dose regimen
2 17
(20 J/cm ). It thus appears that a low-dose regimen does
not offer any advantage over conventional phototherapeutic
modalities. This is in contrast with medium-and high-dose
UVA-1 photother-apy. To achieve an optimal therapeutic
response, how-ever, a high-dose regimen might be
necessary.
Substantial progress has been made in understanding
the photoimmunological mechanisms responsible for the
therapeutic effectiveness of UVA-1 therapy in atopic
18
dermatitis. From these studies it appears that UVA-1
therapy is capable of down-regulating in situ expression of
interferon-g in lesional skin of patients with atopic
dermatitis. Down-regulation of interferon-g expression in
atopic eczema is the consequence of direct effects of UVA1 radiation on Th1 cells present within the dermal infiltrate.
UVA-1 phototherapy induces apoptosis in skin-infiltrating T
cells and thereby causes a gradual reduction of the
inflammatory infiltrate and a con-comitant improvement of
patients' skin disease.
Photo(chemo)therapy for chronic, moderate
atopic dermatitis
Broad-band UVB therapy, combined UVA/UVB therapy,
311 nm UVB therapy, broad-band UVA therapy or
atopic eczema, but are not effective in patients with
3,17,1923
acute severe exacerbation of their disease.
These forms of UV phototherapy are usually not
used as monotherapeutic approaches but are rather
used in combination with topical glucocorticosteroids
to reduce the need for corticosteroid application.
Recent studies indicate that combinations of UVB
irradiation with UVA irradiation 2 UVA/UVB therapy 2 are superior to conventional broad-band UVB,
conventional UVA and low-dose UVA-1 therapy in the
17,22
management of chronic, moderate atopic dermatitis.
In
two paired comparison studies, Jekler and Larko have
shown UVB therapy to be superior to placebo and UVB in
high doses (0.8 MED) to be equipotent to UVB in moderate
17,21
doses (0.4 MED).
The same authors, by using a
clinical scoring system, demonstrated in a paired
comparison study statistically significant differences in
favour of UVA/UVB therapy, as compared with broad-band
22
UVB therapy.
In this trial, patients were allowed to
continue use of topical glucocorticosteroids, and, in
addition, were irradiated three times per week for a
maximum of 8 weeks in a UVB MED-dependent manner.
These careful observations further prove the concept that
UVA/UVB therapy is superior to UVB therapy in the
management of patients with atopic dermatitis.
Patients most frequent complaint about phototherapy
for atopic dermatitis relates to worsening of itch and
induction of sweating by heat, which may be associated
with UV, in particular UVA therapy. In a recent study,
George et al. have therefore incorporated air-condition3
ing into a 311 nm UVB irradiation unit. By using 50 100
W-W TL 01 lamps equipped with reflectors, a UVB
2
output of 5 mW/cm was achieved which resulted in
maximum treatment times of less than 10 min. In this
well-designed study, steroid use by patients with
moderate, chronic atopic dermatitis was monitored 12
weeks prior to phototherapy, during 12 weeks of
phototherapy, and followed for 24 weeks after cessation
of phototherapy. Start of 311 nm UVB therapy not only
decreased the total clinical score, but also substantially
reduced the use of potent steroids. These beneficial
effects were still present in the majority of patients 6
months after cessation of phototherapy.
These studies indicate that 311 nm UVB therapy may
represent the phototherapeutic modality of choice to
induce long-term improvement in patients with atopic
dermatitis. They have recently been confirmed by an
independent report which suggested that no special
cooling system is required in order to achieve the
excellent therapeutic effects reported by George et al.
20
In our hands, 311 nm UVB therapy has been found
556
q 2000 Blackwell Science Ltd X Clinical and Experimental
Dermatology, 25, 552558
to be ideal for following UVA-1 therapy: UVA-1 is
used in the initial phase of treatment to manage
5
acute, severe exacerbations of atopic dermatitis and
is then replaced by 311 nm UVB therapy, which is an
effective (and presumably safe) means of
maintenance therapy. Because its presumed safety,
19
it has also been advocated to be used for children.
Photo(chemo)therapy for chronic vesicular
hand and feet eczema
Vesicular eczema of palms and soles is a common
manifestation of atopic dermatitis which often runs a
chronic course. Since clinical symptoms are limited to
defined areas of the skin, whole body UV irradiation is
inappropriate. The recent development of cream-PUVA
therapy offers the possibility to treat single, defined skin
areas such as palms and soles without exposing nonlesional skin to UV radiation. In addition, partial body
UVA-1 irradiation has been proposed for this indication.
For cream-PUVA a water-in-oil ointment containing
0.0006% 8-methoxypsoralen is applied to the skin area to
24
be treated 1 h prior to UVA irradiation.
Optimal
phototoxicity is given 13 h after cream application and
then rapidly falls. In a first report, cream-PUVA therapy was
found to be extremely beneficial for patients with chronic
hand and feet eczema. After an average of 40 treatments,
complete remission was observed in nine out of 10
24
patients. There is also evidence that cream-PUVA is
superior to bath PUVA for this indication. This might be
because the repetitive use of cream-PUVA, in contrast with
bath PUVA, does not cause dryness of eczematous skin. In
addition cream-PUVA, as compared with bath PUVA, is
easier, cheaper and safer to perform.
In a recent study, palms and backs of 12 patients with
chronic dyshidrotic eczema were exposed to local UVA2 25
1 phototherapy at a single dose of 40 J/cm . Local
UVA-1 phototherapy was given as a monotherapy. After
15 treatments, there was a gradual improvement in 10
out of 12 patients. There was no relapse over a 3-month
follow-up period. It has been suggested that the latter
might be an advantage which local UVA-1 phototherapy
might offer in comparison with local PUVA therapy.
Controlled, comparative studies to prove this point,
however, are currently not available.
Phototherapy for atopic dermatitis X J. Krutmann
Schopf E. High-dose UVA1 therapy in the treatment of
patients with atopic dermatitis. J Am Acad Dermatol
1992; 26: 22530.
13
George SA, Bilsland DJ, Johnson BE, Fergusson J.
Narrow-band (TL01) UVB air-conditioned phototherapy for
chronic severe adult atopic dermatitis. Br J Dermatol 1993;
128:
4956.
14
Grewe M, Bruijnzeel-Koomen CAFM, Schopf E et
al. A role for Th1 and Th2 cells in the immunopathogenesis
of atopic dermatitis. Immunol Today 1998; 19: 35961.
15
Krutmann J. Therapeutic photomedicine:
Phototherapy. In: Freedberg IM, Eisen AZ, Wolff K et al.
eds. Fitzpatrick's Dermatology in General Medicine, 5th
edn. New York:
McGraw-Hill, 1999: 28709.
16
Atherton DJ, Carabott F, Glover MT, Hawk JM. The
role of psoralen photochemotherapy (PUVA) in the
treatment of severe atopic eczema in adolescents. Br J
Dermatol 1988;
118: 7915.
17
Binet O, Aron-Brunetiere C, Cuneo M, Cesaro M-J.
Photochimiotherapie par voie orale et dermatite atopique.
Ann Dermatol Venereol 1982; 109: 58990.
18
Morison WL, Parrish JA, Fitzpatrick TB. Oral
psoralen photochemotherapy of atopic eczema. Br J
Dermatol 1978;
98: 2530.
19
Stern RS et al. Malignant melanoma in patients
treated with psoriasis with methoxsalen (psoralen) and
ultraviolet
A radiation (PUVA). New Engl J Med 1997; 336: 10415.
10 Gasparro F, Edelson RL. Extracorporeal photochemo-therapy.
In: Krutmann J, Elmets CA, eds Photoimmunology. Oxford:
Blackwell Scientific, 1995: 23145.
11 Prinz B, Nachbar F, Plewig G. Treatment of severe
atopic dermatitis with extracorporeal photopheresis.
Arch Dermatol Res 1994; 287: 4852.
12 Richter H, Billmann-Eberwein C, Grewe M et al. Successful
monotherapy of severe and intractable atopic dermatitis by
photopheresis. J Am Aacd Dermatol 1998; 38: 5858.
13 Kobyletzki G, Pieck C, Hoffmann K, Freitag M, Altmeyer
References
1 Jekler J. Phototherapy of atopic dermatitis with ultraviolet
radiation. Dissertation, University of Goteborg, 1992.
2 Krutmann J, Czech W, Diepgen T, Niedner R, Kapp A,
P. Medium-dose UVA1 cold-light phototherapy in the
treat-ment of severe atopic dermatitis. J Am Acad
Dermatol 1999; 41: 9317.
14 Kowalzick L, Kleinhenz A, Weichenthal M, Ring J. Low
dose versus medium dose UVA-1 treatment in severe
atopic dermatitis. Acta Derm Venereol (Stockh) 1995;
75: 435.
15 Meffert H, Sonnichsen N, Herzog M, Hutschenreuther A.
UVA-1 cold light therapy of severe atopic dermatitis.
Dermatol Monatsschr 1992; 78: 2916.
16 Krutmann J, Diepgen TL, Luger TA et al. High-dose UVA1
therapy for atopic dermatitis: Results of a multicenter trial.
J Am Acad Dermatol 1998; 38: 58993.
17 Jekler J, Larko O. Phototherapy for atopic dermatitis with
ultraviolet A (UVA), low-dose UVB and combined UVA and
UVB. two paired comparison studies. Photodermatol
Photo-immunol Photomed 1991; 8: 1516.
18 Morita A, Werfel T, Stege H et al. Evidence that singlet
oxygen-induced human T-helper cell apoptosis is the basic
q 2000 Blackwell Science Ltd
552558
Clinical and Experimental Dermatology, 25,
557
Phototherapy for atopic dermatitis X J. Krutmann
mechanism of ultraviolet-A radiation phototherapy. J
Exp Med 1997; 186: 17638.
19 Collins P, Ferguson J. Narrowband (TLO1) UVB
aircondi-tioned phototherapy for atopic eczema in
children. Br J Dermatol 1995; 133: 6534.
20 Hudson-Peacock MJ, Diffey BL, Farr PM. Narrowband UVB phototherapy for severe atopic dermatitis.
Br J Dermatol 1996; 135: 332.
phototherapy for atopic dermatitis. J Am Acad
Dermatol 1990; 22: 4953.
23 Midelfart
K, Stenvold S-E, Volden G. Combined UVB
and
UVA phototherapy
of
atopic
eczema.
Dermatologica 1985; 171: 958.
24 Stege H, Berneburg M, Ruzicka T, Krutmann J. CreamPUVA-Photochemotherapy. Hautarzt 1997; 48: 8993.
25 Schmidt T, Abeck D, Boeck K, Mempel M, Ring J. UVA1
irradiation is effective in treatment of chronic vesicular
dyshidrotic hand eczema. Acta Derm Venereol (Stockh)
21 Jekler
J, Larko O. UVB phototherapy of atopic
eczema. Br J Dermatol 1988; 119: 697705.
1998; 78: 3189.
22 Jekler J, Larko O. Combined UV-A-UV-B versus UVB
558
q 2000 Blackwell Science Ltd X Clinical and Experimental
Dermatology, 25, 552558
You might also like
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- For Treatment of Atopic Eczema (Atopic Dermatitis) Part II. J Eur Acad Dermatol VenereolDocument1 pageFor Treatment of Atopic Eczema (Atopic Dermatitis) Part II. J Eur Acad Dermatol VenereolKadek Widhiana UtamiNo ratings yet
- Clinical Chemistry-2 (MLT 302) Liver Function and The Biliary Tract Lecture Three Dr. Essam H. AljiffriDocument18 pagesClinical Chemistry-2 (MLT 302) Liver Function and The Biliary Tract Lecture Three Dr. Essam H. AljiffriKadek Widhiana UtamiNo ratings yet
- 2230.2000.00700.X/Abstract Jsessionid 0B1A0C1A7 D1Fb8Ddb38333Aa98B9C3F1.F03T04? Deniedaccesscustomisedmessage &userisauthenticat Ed FalseDocument1 page2230.2000.00700.X/Abstract Jsessionid 0B1A0C1A7 D1Fb8Ddb38333Aa98B9C3F1.F03T04? Deniedaccesscustomisedmessage &userisauthenticat Ed FalseKadek Widhiana UtamiNo ratings yet
- Congres of Dermatology Paris July 2002. p:7-9. 2003Document1 pageCongres of Dermatology Paris July 2002. p:7-9. 2003Kadek Widhiana UtamiNo ratings yet
- Morpot BilliDocument12 pagesMorpot BilliKadek Widhiana UtamiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Data Analytics IntroductionDocument9 pagesData Analytics IntroductionsumitNo ratings yet
- IED Copy of Reading-Report-and-Learning-Diary-Revised-20190220 - 27th-Anniv-Revised-Form.Document3 pagesIED Copy of Reading-Report-and-Learning-Diary-Revised-20190220 - 27th-Anniv-Revised-Form.Noxian TelicNo ratings yet
- Car Design TutorialDocument61 pagesCar Design TutorialNastase Costel100% (15)
- Choral Music Hits PDFDocument9 pagesChoral Music Hits PDFstefano bettineschiNo ratings yet
- A044 2019 20 Readiness Review Template For EAC 3-12-2018 FinalDocument25 pagesA044 2019 20 Readiness Review Template For EAC 3-12-2018 FinalMohamed AbdelSalamNo ratings yet
- Slow LearnerDocument33 pagesSlow LearnerMuhammad Khairul Nizam100% (1)
- O-Ring UKDocument12 pagesO-Ring UKAan Sarkasi AmdNo ratings yet
- Thermodynamics QsDocument3 pagesThermodynamics QsT Hari PrasadNo ratings yet
- Exercises Problem 2 Lesson 4Document2 pagesExercises Problem 2 Lesson 4Marianne DevillenaNo ratings yet
- 1993 Book Non ThermalPlasmaTechniquesFor 2Document422 pages1993 Book Non ThermalPlasmaTechniquesFor 2denizinak100% (1)
- Capstone Project MarketingDocument9 pagesCapstone Project MarketingKawalpreet SinghNo ratings yet
- X Ray DiffractionDocument12 pagesX Ray DiffractionSiddraKhalidNo ratings yet
- Emu ManualDocument86 pagesEmu ManualMiguel GutierrezNo ratings yet
- Business Plan PDFDocument86 pagesBusiness Plan PDFNicholas SalisNo ratings yet
- "Some of Us May Never Die," by Kathleen SteinDocument5 pages"Some of Us May Never Die," by Kathleen SteinMark PlusNo ratings yet
- Ajax UlerDocument19 pagesAjax UlernsbNo ratings yet
- Final Coaching - FundaDocument3 pagesFinal Coaching - FundaenzoNo ratings yet
- MIS Downloads Requirement Specification Document Example 2Document14 pagesMIS Downloads Requirement Specification Document Example 2Rajashree PatilNo ratings yet
- Jurnal Kacang Hijau Dan MaduDocument7 pagesJurnal Kacang Hijau Dan Madusri margiatiNo ratings yet
- Rudolf DreikursDocument17 pagesRudolf DreikursKatrina Cassandra0% (1)
- Istambul TurciaDocument2 pagesIstambul Turciaantoneacsabin06No ratings yet
- Unit 2 Installation and Configuration of AndroidDocument23 pagesUnit 2 Installation and Configuration of AndroidAtharv KadamNo ratings yet
- ISC HydroCom ComparisonDocument22 pagesISC HydroCom Comparisonrahilshah100No ratings yet
- TestingDocument116 pagesTestingAkarsh LNo ratings yet
- Revenge, Hypnotism, and Oedipus in OldboyDocument13 pagesRevenge, Hypnotism, and Oedipus in OldboyAdrián PiqueroNo ratings yet
- Charles Stanley - Let Go and Let GODDocument50 pagesCharles Stanley - Let Go and Let GODTheAgapeIncNo ratings yet
- Chapter II Sample ThesisDocument13 pagesChapter II Sample ThesisAllen Bradley OngNo ratings yet
- Understanding Advertising and Consumer Behaviour: Pankaj KumarDocument7 pagesUnderstanding Advertising and Consumer Behaviour: Pankaj KumarAlfredo ValeraNo ratings yet
- Test Report: LaboratoryDocument5 pagesTest Report: LaboratorybethNo ratings yet
- From The Explorer's DaughterDocument2 pagesFrom The Explorer's DaughterMisho DragnevNo ratings yet