Professional Documents
Culture Documents
Vascular Disturbances (Module C) Cerebrovascular Accident (Cva)
Uploaded by
RosmaryOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vascular Disturbances (Module C) Cerebrovascular Accident (Cva)
Uploaded by
RosmaryCopyright:
Available Formats
VASCULAR DISTURBANCES (MODULE C) Blanket on hip – promote normal gait
Knees and thigh should not be flexed – venous return
CEREBROVASCULAR ACCIDENT (CVA) Unilateral neglect – move affected part with unaffected part
-stroke; brain attack; counterpart of MI
- interruption of blood supply to the brain, causing temporary or 1 MOTOR DEFICITS
loss of movements, thoughts, speech or sensation. Ataxia – ambulation devices; provide safety
Dysarthria – gestures; ample time to respond
Predisposing factors: Psychological – emotional support
Hereditary ( familial predisposition) Dysphagia – chew properly and on unaffected side
Age ( increase age – increase risk) – 55 y.o. - Sit upright when eating or out of bed
Gender - NGT
- Tuck chin to chest – swallowing; prev. aspiration
Types:
>Large Artery Thrombotic stroke 2 VERBAL DEFICITS
>Small Penetrating Artery thrombosis Aphasia – loss/ineffective speech
- lacunar stroke; most common 3 types:
>Cardiogenic Embolic stroke >Sensory/Receptive/Wernicke’s/Fluent
- assoc. with atrial fibrillation >Motor/Expressive/Broca’s/Non-Fluent
>Cryptogenic stroke >Global
- no known cause
>Other causes: migraine, drug use, coagulopathies Interventions:
Use simple sentences
Precipitating factors: Encourage gestures and pictures
HPN, DM, Smoking, Atrial fibrillation, obesity, hyperlipidemia, Alternative means
increase alcohol consumption, stressful lifestyle Talk slowly and clearly
Ample time to respond
Atherosclerotic plaque Enc. to repeat alphabet sound esp on broca’s
Be consistent and repeat if necessary
*Thrombotic – slow, progressive ( LAT and SMA)
Embolic – sudden 3 VISUAL DEFICITS
**Homonymous Hemianopsia
HEMORRHAGIC STROKE Left Homonymous Hemianopsia
Precipitating factor : Right Homonymous Hemianopsia
Uncontrolled HPN
Arteriovenous malformation – rupture of vessel >Approach on unaffected side
Intracranial aneurysm – bleeding (rupture) >Provide safety
Intracranial neoplasm >Allow to scan room
Onset: sudden, rapid
**Aplopia – consistent placing of things in same place
Manifestations: >Explain location
>motor deficits – dysarthria; hemiparesis/plegia; ataxia(staggering,
unsteady gait) **Horner’s Syndrome – paralysis of sympathetic nerve
>”frozen” shoulder - Ptosis / sinking of eyeballs
>Subluxation of shoulder - Constriction of pupils
>Painful shoulder – hand dystrophy
- Tearing
>Addduction of arm with internal rotation. Flexion of elbow, wrist
>Explain location of things
and fingers
>Proper lighting
>External rotation of leg at hip joint, flexion at knee and plantar
flexion and supination of ankle.
4 SENSORY DEFICITS
>shortened heel cord
**Paresthesia – numbness/tingling sensation of affected
>speech difficulties and visual disturbances
extremities.
>Don’t use affected areas as dominant limb.
Interventions: >ROM – affected area.
>pillow below the axilla (side-lying position)
>free palm – relieve pressure 5 EMOTIONAL DEFICITS
For flaccid paralysis: ~depression ~mood swings
>”dorsal wrist splint” – spastic upper extreme. ~hostility ~loss of self-control
> passive ROM – affected ~anger ~decrease tolerance to stimuli
Active ROM – unaffected ~fear
4-5x daily >Encourage verbalization of feelings
>turn to sides q 2h >Participate in group activities
>15-30mins in prone
>less amount of time in affected area – decreased sensation
DX TESTS:
o Carotid Ultrasound
Pillow on head
o CT Scan Congenital conditions
o Cerebral Angiography Trauma
o PET Scan Infection
o MRI Inflammation
o ECG Increase turbulence in a section of a vessel
HPN
MANAGEMENT Smoking
MED: Pathophysio:
Goal : To allow brain to recover from initial insult Vasospasm - > ischemia
To restore cerebral blood flow Subarachnoid hemorrhage - > blood in CSF
To provide complications and tissue damage.
S/S: N/V – increased ICP
1. Maintain patent airway Visual disturbances
2. Reperfusion and hemodilution with volume expanders. COMPLI : Hydrocephalus
3. Thrombolytic therapy Cerebral Vasospasm
4. Antihypertensive therapy Seizures
5. Diuretic therapy Rebleeding in 1st 7-14days
6. Calcium channel blockers
7. Anticoagulant therapy DX TESTS:
8. Stool softeners o Lumbar Tap – presence of blood in subarachnoid space;
except for increase ICP
SURG: Craniotomy o Angiography – definitive exam
o Skull X-rays
>>Nuchal Rigidity – sign of altered cerebral tissue perfusion o CT-Scan
o Hunt-Hess Scale -bleeding
TRANSIENT ISCHEMIC ATTACK
“Silent Stroke” – can go unnoticed TX:
>lasts 5-20 mins MED:
>temporary disruption of blood supply >Antifibrinolytic agent – Epsilon Aminocaproic acid
>mini-stroke – copies s/s of stroke >Increase ICP – Dexamethasone
>warning stroke >Prophylactic anticonvulsant
DX TESTS: SURG:
o Auscultation of Carotid Artery Balloon Therapy
o CT Scan – Rule out stroke Gamma knife
o Transesophageal Echocardiography (TEEC)
NG:
MGT: Prevent occurrence of stroke Glasgow Coma Scale
Monitoring changes in ICP
>TIA caused by Atrial Fibrillation Monitor for focal neurologic deficits
-> Anticoagulant Therapy
>Exercise 10 mins everyday.
>Determine risk factors
SURG : Carotid Endarterectomy
Cerebral Angioplasty
INTRACRANIAL ANEURYSM
>a thin-walled outpouching or dilation of an artery of the brain
>develop usually at Circle of Willis and Internal Carotid Artery
>> Berry
Saccular – saccular outpouching
Fusiform - outpouching of vessel
Dissecting – intimal layer
>Usually aymptomatic until
-- compress surrounding tissue or cranial nerve
-- rupture and cause the classical symptoms of subarachnoid
hemorrhage
ETIOLOGY:
Atherosclerosis MYELOMALACIA
Genetics >softening or infarction of spinal cord from spinal artery occlusion
>poor prognosis
>little or no return of normal fxn Vascular malformation
>”transverse myelitis” Bleeding d/o
MANIF: MANIF:
INITIAL : Areflexia >immediately happens after spinal injury; depends on size of
Flaccid limbs hemorrhage
Motor paralysis >motor deficits
Sensory loss below level of lesion
Paralysis of bladder and bowel sphincters DX TESTS:
X-Ray
TX: Spinal Angiograph
>Symptomatic care of probs rxlting from cord lesion Spinal CT-Scans
>Tx of ds that caused vascular lesion MRI
NG: TX:
>Provide pain relief >Immediate surgery to relieve cord compression
>Maintain body fxns >Ligating the feeding vessels
>Preventing complications of immobility >Excising the entire malformation
>Intensive rehab for 12-48 hrs after onset of manifestations
NG:
>Provide pain relief
>Maintain body fxn
>Prevent compli of immobility
>Intensive rehab 12-14hrs pc onset of manif
HEMATOMYELIA
>hemorrhage into substance of spinal cord
Cause : Trauma
You might also like
- Neurorehabilitation 1: Stroke, TBI, MS, PD, GBS, and ALS ExaminationDocument439 pagesNeurorehabilitation 1: Stroke, TBI, MS, PD, GBS, and ALS ExaminationDuncan D'AmicoNo ratings yet
- Understanding Coma and StrokeDocument83 pagesUnderstanding Coma and StrokeNia AishiteruNo ratings yet
- Care of Clients With Life Threatening Conditions, Acutely Ill/Multi-Organ Problems, High Acuity, and Emergency SituationDocument75 pagesCare of Clients With Life Threatening Conditions, Acutely Ill/Multi-Organ Problems, High Acuity, and Emergency SituationleonielainecolbornNo ratings yet
- Neurology - Weakness PatternsDocument2 pagesNeurology - Weakness PatternsAnisah AliNo ratings yet
- MS - NeuroDocument10 pagesMS - Neuroknowamai567No ratings yet
- SPINAL CORD AND RADICULAR SYNDROMESDocument44 pagesSPINAL CORD AND RADICULAR SYNDROMESChairul AmriNo ratings yet
- StrokeDocument27 pagesStrokeJASON KO CHIA SHENGNo ratings yet
- Health Assess - Chapter 23 Key TermsDocument3 pagesHealth Assess - Chapter 23 Key TermsAllison Doubek GibsonNo ratings yet
- Neurological HX TakingDocument3 pagesNeurological HX Takingbloo tomartoNo ratings yet
- Umnl Vs LMNLDocument5 pagesUmnl Vs LMNLBell GatesNo ratings yet
- Approach To Seizures in ChildrenDocument12 pagesApproach To Seizures in ChildrenShamen KohNo ratings yet
- Cerebrovascular Accident or Stroke: By: Thalia Nicole SanchezDocument19 pagesCerebrovascular Accident or Stroke: By: Thalia Nicole SanchezMaesy LorenaNo ratings yet
- Localising CNS LesionsDocument3 pagesLocalising CNS LesionsDeeWallyNo ratings yet
- Hacks Final FormattedDocument183 pagesHacks Final Formattedbhoj RAJNo ratings yet
- NCP NeuroDocument20 pagesNCP NeuroNica Gaborne Navarro100% (3)
- Cerebro Vascular AccidentDocument82 pagesCerebro Vascular AccidentJayvee Novenario Casaljay100% (1)
- The Nervous SystemDocument24 pagesThe Nervous SystemKiara GovenderNo ratings yet
- Paediatric PEDocument2 pagesPaediatric PEAzizi RafieNo ratings yet
- CHAPTER 36Document3 pagesCHAPTER 36Samantha QuintoNo ratings yet
- PDF Cns - StrokeDocument42 pagesPDF Cns - Strokemdrnh6shbmNo ratings yet
- General Anesthesia Guide for VeterinariansDocument18 pagesGeneral Anesthesia Guide for VeterinariansMr. AlphaNo ratings yet
- Case Study CvaDocument6 pagesCase Study Cvajing_elizabethNo ratings yet
- Neurological Assessment For CVADocument8 pagesNeurological Assessment For CVAKristine Alejandro100% (1)
- Impaired pupillary reaction to light assessmentDocument7 pagesImpaired pupillary reaction to light assessmentDaintyGarcia100% (1)
- 7.1 Altered PerceptionDocument129 pages7.1 Altered PerceptionAlexander Blanche PajelaNo ratings yet
- NBME CMS Forms NotesDocument4 pagesNBME CMS Forms NotesJack Guccione100% (7)
- Steven Angelo E. Cruz, PTRPDocument130 pagesSteven Angelo E. Cruz, PTRPJoeNo ratings yet
- Ischemic Stroke: The Normal Blood Supply To The Brain Is DisruptedDocument5 pagesIschemic Stroke: The Normal Blood Supply To The Brain Is DisruptedMelchora Lea Castro SorianoNo ratings yet
- Iicp 1Document5 pagesIicp 1Melodia Turqueza GandezaNo ratings yet
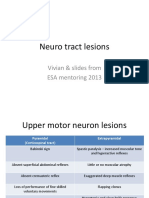
- Neuro tract lesions guide for UMN, LMN deficitsDocument16 pagesNeuro tract lesions guide for UMN, LMN deficitsসোমনাথ মহাপাত্রNo ratings yet
- Osce: Internal Medicine 1. JVP Measurement: © FAAS 3A, 2018Document11 pagesOsce: Internal Medicine 1. JVP Measurement: © FAAS 3A, 2018PatNo ratings yet
- Localisation in NeurologyDocument19 pagesLocalisation in NeurologyArnav GuptaNo ratings yet
- Neurology LocalizationDocument6 pagesNeurology LocalizationPramod ThapaNo ratings yet
- Localisation in NeurologyDocument19 pagesLocalisation in NeurologyArnav GuptaNo ratings yet
- FINALSDocument30 pagesFINALSMiden AlbanoNo ratings yet
- GuillainDocument4 pagesGuillainanime listNo ratings yet
- Disorders of The Spinal Cord: Refer Above Refer AboveDocument2 pagesDisorders of The Spinal Cord: Refer Above Refer AbovePaolo PunzalanNo ratings yet
- Seizure Disorder Types: Partial - Local Onset May or May Not Impair Consciousness SimpleDocument4 pagesSeizure Disorder Types: Partial - Local Onset May or May Not Impair Consciousness Simpleampogison08No ratings yet
- Cauda-Conus SyndromesDocument28 pagesCauda-Conus Syndromessruthimeena6891No ratings yet
- Neurology Self Directed Learning Target1Document7 pagesNeurology Self Directed Learning Target1turpificatusNo ratings yet
- In The Name of God, Most Gracious, Most MercifulDocument48 pagesIn The Name of God, Most Gracious, Most MercifulMohammad Sadiq AzamNo ratings yet
- Stroke SindromDocument13 pagesStroke SindromEvi Andriani LestariNo ratings yet
- Res 113Document197 pagesRes 113Belinda ELISHANo ratings yet
- REHABILITASI MEDIK PADA PENDERITA STROKEDocument55 pagesREHABILITASI MEDIK PADA PENDERITA STROKEKrisma susantiNo ratings yet
- StrokeDocument4 pagesStrokeMostafa SaadawyNo ratings yet
- Thyroid Gland Signs and Symptoms GuideDocument13 pagesThyroid Gland Signs and Symptoms GuidekylieverNo ratings yet
- Cranial Nerve Functions and Lesion SymptomsDocument4 pagesCranial Nerve Functions and Lesion SymptomsBloom DhillonNo ratings yet
- Neurological Examination: ObserveDocument9 pagesNeurological Examination: ObserveTom MallinsonNo ratings yet
- Common Cases in Neurological ExaminationDocument7 pagesCommon Cases in Neurological ExaminationSamuel Ravi ChoudhuryNo ratings yet
- EMS QUALITY NEWSLETTER ISSUE 4 HIGHLIGHTS ATYPICAL STROKE SYMPTOMSDocument2 pagesEMS QUALITY NEWSLETTER ISSUE 4 HIGHLIGHTS ATYPICAL STROKE SYMPTOMSScott TopiolNo ratings yet
- Acute Focal Neurological SignsDocument27 pagesAcute Focal Neurological SignsKayman SpartanNo ratings yet
- Demyelinating DiseasesDocument2 pagesDemyelinating DiseasesRosmaryNo ratings yet
- Stroke CVDDocument9 pagesStroke CVDangel.senido0198No ratings yet
- Askep StrokeDocument39 pagesAskep StrokeDeviana EnjelinaNo ratings yet
- Critical Limb Ischaemia Causes, Symptoms, and TreatmentsDocument2 pagesCritical Limb Ischaemia Causes, Symptoms, and Treatmentsdragtoss2No ratings yet
- Umnl & LMNLDocument13 pagesUmnl & LMNLTammy BoudNo ratings yet
- Neurological Examination SummaryDocument90 pagesNeurological Examination SummaryAlida Taranu TernströmNo ratings yet
- The Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaFrom EverandThe Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaNo ratings yet
- ResearchDocument6 pagesResearchRosmaryNo ratings yet
- Understanding Normal Laboratory ValuesDocument2 pagesUnderstanding Normal Laboratory ValuesRosmary0% (1)
- JurisprudenceDocument4 pagesJurisprudenceRosmaryNo ratings yet
- Nursing JurisprudenceDocument1 pageNursing JurisprudenceRosmaryNo ratings yet
- Nursing JurisprudenceDocument1 pageNursing JurisprudenceRosmaryNo ratings yet
- JURIS2Document1 pageJURIS2RosmaryNo ratings yet
- Introduction To Nursing ResearchDocument4 pagesIntroduction To Nursing ResearchRosmaryNo ratings yet
- English (Sequence)Document1 pageEnglish (Sequence)RosmaryNo ratings yet
- Discharge Care and RehabilitationDocument1 pageDischarge Care and RehabilitationRosmaryNo ratings yet
- Perception and Coordination Module ADocument3 pagesPerception and Coordination Module ARosmary100% (1)
- Inflammatory DiseasesDocument2 pagesInflammatory DiseasesRosmaryNo ratings yet
- RLE 6 and 7Document11 pagesRLE 6 and 7RosmaryNo ratings yet
- Demyelinating DiseasesDocument2 pagesDemyelinating DiseasesRosmaryNo ratings yet
- Degenerative DiseasesDocument1 pageDegenerative DiseasesRosmaryNo ratings yet
- Jose Protacio Rizal y MercadoDocument2 pagesJose Protacio Rizal y MercadoRosmaryNo ratings yet
- Pol Sci/word 1997 DocumentDocument13 pagesPol Sci/word 1997 DocumentRosmaryNo ratings yet
- Pol Sci/word 1997 DocumentDocument13 pagesPol Sci/word 1997 DocumentRosmaryNo ratings yet
- Second Law of EntrophyDocument22 pagesSecond Law of EntrophyMia Betia BalmacedaNo ratings yet
- GIS Arrester PDFDocument0 pagesGIS Arrester PDFMrC03No ratings yet
- School Quality Improvement System PowerpointDocument95 pagesSchool Quality Improvement System PowerpointLong Beach PostNo ratings yet
- Ramdump Memshare GPS 2019-04-01 09-39-17 PropsDocument11 pagesRamdump Memshare GPS 2019-04-01 09-39-17 PropsArdillaNo ratings yet
- BPO UNIT - 5 Types of Securities Mode of Creating Charge Bank Guarantees Basel NormsDocument61 pagesBPO UNIT - 5 Types of Securities Mode of Creating Charge Bank Guarantees Basel NormsDishank JohriNo ratings yet
- Lecture 1: Newton Forward and Backward Interpolation: M R Mishra May 9, 2022Document10 pagesLecture 1: Newton Forward and Backward Interpolation: M R Mishra May 9, 2022MANAS RANJAN MISHRANo ratings yet
- Individual Sports Prelim ExamDocument13 pagesIndividual Sports Prelim ExamTommy MarcelinoNo ratings yet
- Bandung Colonial City Revisited Diversity in Housing NeighborhoodDocument6 pagesBandung Colonial City Revisited Diversity in Housing NeighborhoodJimmy IllustratorNo ratings yet
- BMS Technical ManualDocument266 pagesBMS Technical Manualiago manziNo ratings yet
- Translation EquivalenceDocument6 pagesTranslation EquivalenceJamal Anwar TahaNo ratings yet
- Report Daftar Penerima Kuota Telkomsel Dan Indosat 2021 FSEIDocument26 pagesReport Daftar Penerima Kuota Telkomsel Dan Indosat 2021 FSEIHafizh ZuhdaNo ratings yet
- Driving Continuous Improvement by Developing and Leveraging Lean Key Performance IndicatorsDocument10 pagesDriving Continuous Improvement by Developing and Leveraging Lean Key Performance IndicatorskellendadNo ratings yet
- Unit 1 - Introduction To BankingDocument17 pagesUnit 1 - Introduction To Bankingc08No ratings yet
- Cold Forging Process TutorialDocument28 pagesCold Forging Process TutorialpanyamnrNo ratings yet
- 2007 Bomet District Paper 2Document16 pages2007 Bomet District Paper 2Ednah WambuiNo ratings yet
- Introduction To OpmDocument30 pagesIntroduction To OpmNaeem Ul HassanNo ratings yet
- 2019-10 Best Practices For Ovirt Backup and Recovery PDFDocument33 pages2019-10 Best Practices For Ovirt Backup and Recovery PDFAntonius SonyNo ratings yet
- Micropolar Fluid Flow Near The Stagnation On A Vertical Plate With Prescribed Wall Heat Flux in Presence of Magnetic FieldDocument8 pagesMicropolar Fluid Flow Near The Stagnation On A Vertical Plate With Prescribed Wall Heat Flux in Presence of Magnetic FieldIJBSS,ISSN:2319-2968No ratings yet
- Basf Masterseal 725hc TdsDocument2 pagesBasf Masterseal 725hc TdsshashiNo ratings yet
- Florence Walking Tour MapDocument14 pagesFlorence Walking Tour MapNguyễn Tấn QuangNo ratings yet
- Irctc Tour May 2023Document6 pagesIrctc Tour May 2023Mysa ChakrapaniNo ratings yet
- 2016 Mustang WiringDocument9 pages2016 Mustang WiringRuben TeixeiraNo ratings yet
- (Bio) Chemistry of Bacterial Leaching-Direct vs. Indirect BioleachingDocument17 pages(Bio) Chemistry of Bacterial Leaching-Direct vs. Indirect BioleachingKatherine Natalia Pino Arredondo100% (1)
- Electrosteel Castings Limited (ECL) - Technology That CaresDocument4 pagesElectrosteel Castings Limited (ECL) - Technology That CaresUjjawal PrakashNo ratings yet
- Fiera Foods - Production SupervisorDocument1 pageFiera Foods - Production SupervisorRutul PatelNo ratings yet
- DSE61xx Configuration Suite Software Manual PDFDocument60 pagesDSE61xx Configuration Suite Software Manual PDFluisNo ratings yet
- Distinguish Between Tax and FeeDocument2 pagesDistinguish Between Tax and FeeRishi Agarwal100% (1)
- SEO Design ExamplesDocument10 pagesSEO Design ExamplesAnonymous YDwBCtsNo ratings yet
- Numerical Methods: Jeffrey R. ChasnovDocument60 pagesNumerical Methods: Jeffrey R. Chasnov2120 sanika GaikwadNo ratings yet
- PREMIUM BINS, CARDS & STUFFDocument4 pagesPREMIUM BINS, CARDS & STUFFSubodh Ghule100% (1)