Professional Documents
Culture Documents
Genetic Immunodeficiency Diseases
Uploaded by
Annisa Chaerani BurhanuddinCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Genetic Immunodeficiency Diseases
Uploaded by
Annisa Chaerani BurhanuddinCopyright:
Available Formats
Chapter 143
Genetic
Immunodeficiency
Diseases
Ramsay L. Fuleihan & Amy S. Paller
ANTIBODY DEFICIENCY
DISORDERS
Agammaglobulinemia
ETIOLOGY AND PATHOGENESIS.
The underlying defect in agammaglobulinemia is
failure of maturation of a pre-B cell into an immature B cell; early B-cell precursors are found in the
bone marrow in normal numbers. The causative
genes, including BTK, participate in B-cell receptor
signaling and are essential for B-cell maturation.
Cell-mediated immunity is normal. More than 500
different mutations in BTK have been reported, and
no single mutation is detected in more than 3% of
the patients.4 Carrier detection in XLA is possible by
analyzing the patterns of X-chromosome inactivation, with selective inactivation of the abnormal X
chromosome in B lymphocytes from female carriers
or by intracellular staining and flow cytometry for
BTK in monocytes.
Common Variable
Immunodeficiency
EPIDEMIOLOGY.
The disease prevalence of common variable immunodeficiency (CVI) is estimated at 1 in 25,000
and affects males and females equally.7,8 The onset
of symptoms occurs at any age, with male patients
presenting earlier than female patients; the mean
age of onset of symptoms is 23 and 28 years, and
mean age of diagnosis of 29 and 33 years, respectively.9 A minimum age of 4 years is used to exclude
patients with other primary immunodeficiency
diseases.10 Most cases are sporadic, but at least 10%
are familial with a predominance of autosomal
dominant over autosomal recessive inheritance.
ETIOLOGY AND PATHOGENESIS.
Identified genetic defects underlying CVI result in
abnormalities in transmembrane activator, calcium
modulator, and cyclophilin ligand interactor (TACI),
inducible costimulator (ICOS), B-cell activation
factor of the tumor necrosis factor (TNF) family
receptor (BAFF-R), and CD19. Each of these is critical for B-lymphocyte activation and differentiation.
Altogether, mutations in these genes account for
approximately 10% to 20% of patients, with defects
in TACI being the most common.7 The majority of
defects are yet to be discovered.
LABORATORY FINDINGS.
Failure in B-cell differentiation and resultant impaired secretion of immunoglobulins (Ig) leads to
reduction in serum IgG and IgA and/or IgM by two
standard deviations or more below the mean. The
numbers of circulating B lymphocytes are usually
normal but may be decreased or absent. Cellular
immunity may be impaired.16 Approximately onehalf of patients have T-cell dysfunction,17 with the
incidence increasing with advancing age. Some
patients have a decreased absolute number of circulating CD4+ T cells and a normal number of CD8+
T cells.18 The diagnosis of CVI requires the exclusion
of known genetic causes of other immunodeficiency diseases and a 2-year period free of lymphoma.8
PROGNOSIS, CLINICAL COURSE, AND
TREATMENT
Ig replacement is standard treatment for CVI. Prophylactic antibiotics should be initiated in patients
who continue to have infections despite Ig therapy.19 Patients with granulomatous inflammation
have a worse prognosis.20 The mean age of death
for females is 45.5 years and for males 40 years. The
majority of patients die from either lymphoma or
chronic sinopulmonary infections.9
SELECTIVE IMMUNOGLOBULIN
DISORDERS
Immunoglobulin A Deficiency
IgA deficiency is often sporadic, but both autosomal recessive and autosomal dominant forms of
inheritance have been described. Susceptibility to
IgA has been linked to the HLA-DQ/DR locus and
Copyright McGraw-Hill Companies, Inc. All rights reserved.
220 Chapter 143: Genetic Immunodeficiency Diseases
an extended major histocompatibility complex
(MHC) haplotype (HLA-B8, SC01, DR3) is found
with increased frequency in both IgA deficiency
and CVI.9,15,21 Mutations in the TNF receptor family
member TACI are also found in patients with IgA deficiency, accounting for about 5% of patients. B cells
from individuals with TACI mutations do not produce IgG and IgA in response to the TACI ligand, reflecting impaired isotype switching.7 IgA deficiency
occurs in approximately 1 in 600 persons, and most
of those affected are healthy. However, affected
individuals tend to have an increased incidence of
upper respiratory tract infections (especially viral),
allergies, atopic dermatitis, chronic gastroenteritis,
and autoimmune disorders with circulating autoimmune antibodies.22 Individuals prone to infection
should be screened for functional defects. Patients
with no detectable IgA who have the capacity to
synthesize specific antibodies may develop IgE,
anti-IgA antibodies with infusion of blood products
that contain IgA,23 and risk transfusion reactions
with subsequent blood product infusions including
IVIG. However, the incidence of anti-IgA reactions
in IVIG administration is rare and life-saving blood
product infusions should not be withheld in an
IgA-deficient patient, especially if it is the patients
first infusion.
Immunoglobulin M Deficiency
IgM deficiency is associated with an increased risk
of pneumococcal and neisserial infections, warts,
and eczema. The pathogenesis of selective IgM deficiency is not known.
CELLULAR DEFICIENCIES
X-Linked Lymphoproliferative
Disease (Duncan Disease)
EPIDEMIOLOGY.
The incidence of X-linked lymphoproliferative disease (XLP) is 1 in 3 million males.24
PATHOGENESIS.
XLP disease results from mutations in SH2D1A,25
which encodes an adapter protein, signaling lymphocytic activation molecule (SLAM)-associated
protein (SAP), critical to intracellular signaling pathways.26 SAP is expressed in T cells, natural killer (NK)
cells, and NKT cells. Patients have no NKT cells in
the periphery and defective SAP-mediated activation of their NK and CD8+ T cells.27
CLINICAL FINDINGS.
XLP is characterized by fulminant infectious mononucleosis, dysgammaglobulinemia, and lymphoproliferative disorders.26 Patients are also at risk for
the development of autoimmune disorders. These
clinical manifestations usually develop following
EpsteinBarr virus (EBV) infection in boys who have
previously had normal immunologic responses.
With EBV infection, however, patients respond
abnormally to the antigen and fail to develop EBVspecific serologic responses.
Infectious mononucleosis, the most common
clinical manifestation, affects 60% of patients and
median age at onset is 3 years.26 Clinical signs
include fever, pharyngitis, rash, lymphadenopathy,
and hepatosplenomegaly. A progressive hypogammaglobulinemia is seen in 30% of patients before or
after EBV infection; the median age of onset of hypogammaglobulinemia is 79 years.24,28 All patients
with infectious mononucleosis and most patients
with dysgammaglobulinemia have evidence of EBV
infection. In contrast, the development of lymphomas can occur in XLP patients with no evidence of
detectable EBV infection.29 Malignant lymphomas
and nonmalignant lymphoproliferative disorders,
including lymphomatoid granulomatosis, granulomatosis with polyangiitis (Wegeners), and necrotizing vasculitis, affect 20% to 30% of patients.28 The
majority of malignant tumors are of B-cell origin.
PROGNOSIS, CLINICAL COURSE, AND
TREATMENT.
XLP is a fatal disease and 70% of patients die by the
age of 10 years.27 The median survival after development of primary EBV infection and fulminant
mononucleosis is 12 months.24 Most patients die
from severe hepatitis, liver necrosis, and hepatic
failure. Patients with isolated hypogammaglobulinemia treated with Ig replacement have a better
prognosis than those who develop fulminant infectious mononucleosis or lymphoma.26
Chronic Mucocutaneous
Candidiasis
ETIOLOGY AND PATHOGENESIS.
The clinical features of CMC may be seen in a variety of immunologic disorders, all characterized by
ineffective defense mechanisms against Candida. In
general, the patients with greater severity and an
earlier onset of cutaneous candidal infections have
more severe immunologic alterations. CMC patients
Copyright McGraw-Hill Companies, Inc. All rights reserved.
Chapter 143:
have shown general dysregulation of interleukin 12
(IL-12), IL-6, and interferon- (IFN-) production,30 as
well as autoantibodies to IL-17 and IL-2231 resulting
in an inability to mount a cell-mediated response
to clear candidal organisms. Chronic infections
result in production of high levels of inflammatory cytokines (IL-6) followed by anti-inflammatory
cytokines (IL-10) that further reduce the production
of T helper 1 (Th1)-inducing cytokines via a positive
feedback loop.30
Humoral immunity appears normal in most
patients and 25% to 35% of patients with CMC
have no demonstrable immunologic defects. Many
patients with CMC have associated APECED syndrome,32 owing to mutations in the autoimmune
regulator (AIRE) gene which maps to 21q22.3 and
encodes a DNA transcription factor.33 Mice that are
deficient in AIRE do not delete organ-specific T cells
in the thymus, thus promoting the development of
autoimmune disease.34 The reason for susceptibility
to mucocutaneous candidal infections is unclear,
but may be related to the decreased Th17 and
Th1 immune responses.31 APECED must be distinguished from immune dysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) syndrome, an
X-linked recessive disorder in which the abnormal
development of regulatory T cells results from
mutations in the FOXP3 gene. Patients with IPEX
syndrome show atopic or psoriasiform dermatitis,
nail dystrophy, autoimmune endocrinopathies
(overlapping with those seen in APECED syndrome),
and autoimmune skin conditions such as alopecia
universalis.35,36
DiGeorge Syndrome
EPIDEMIOLOGY.
The incidence of DiGeorge syndrome (DGS) is 1 in
4,000 live births39 Ninety percent of the cases are
associated with a deletion in chromosome 22qll.l.
ETIOLOGY AND PATHOGENESIS.
DGS (congenital thymic aplasia) is a member of
a group of disorders that result from deletion of
chromosome 22q11 (CATCH 22/DGS/velocardiofacial syndrome).40 The disorder results from developmental defects of the third and fourth pharyngeal
pouches due to haploinsufficiency of Tbx1, a t-box
transcription factor.41 Five percent to 10% of patients do not have this deletion; some have deletion
of chromosome 10 and others have no identifiable
gene defect.42 All patients have T cell defects, but
patients with partial DGS have only mild T cell
Genetic Immunodeficiency Diseases 221
abnormalities, showing an increase in T cell numbers from birth to age 2 that subsequently do not
decrease with time.43 Patients with complete DGS
(complete lack of thymus and T cell percentage less
than 1 to 2) have SCID with B cell immunodeficiency as well, presumably due to the lack of T cell help
for B cells. These patients do not recover functional
T-cells throughout early infancy. Complete DGS
occurs in less than 1% of cases.44 It is often found
in conjunction with 22q11 hemizygosity,45,46 the
CHARGE association,47,48 or diabetic embryopathy.49
CLINICAL FINDINGS.
The thymic shadow is absent or reduced at birth.
Infants often have neonatal tetany with hypocalcemia due to the aplastic parathyroid glands. The
cardiac anomalies are most commonly truncus
arteriosus, septal defects, and abnormal aortic arch
vessels. Characteristic facial features of DGS include
a short philtrum, low-set malformed ears, and
hypertelorism.
Many patients have recurrent mucocutaneous
candidal infections as neonates, as well as increased
susceptibility to viral infections, Pneumocystis
jiroveci, and other fungal infections. Graft-versushost disease (GVHD) may develop in infants given
nonirradiated blood products. A small percentage
of patients have complete athymia and about onethird of them develop an eczematous dermatitis
with lymphadenopathy driven by oligoclonal T cells,
known as atypical complete DiGeorge anomaly.
There is an overall increase of malignancy in DGS,
particularly hepatoblastoma; in a cohort of patients
under the age of 14, the overall risk of malignancy
was 900 per 100,000, whereas the overall risk of
malignancy in children under 14 years is 3.4 per
100,000.50
PROGNOSIS, CLINICAL COURSE, AND
TREATMENT.
Patients with complete DGS usually die within
the first 2 years of life.51 In rare cases, transplant of
HLA-matched bone marrow or peripheral blood
mononuclear cells restores T-cell function.52 Postnatal thymus transplant can restore T-cell function in
patients with complete DGS.44,53
Copyright McGraw-Hill Companies, Inc. All rights reserved.
222 Chapter 143: Genetic Immunodeficiency Diseases
CARTILAGEHAIR HYPOPLASIA
SYNDROME
Epidemiology
Cartilagehair hypoplasia (CHH) syndrome is an
autosomal recessive disorder that is most common
in Amish and Finnish individuals.54 There is a 4:1
femalemale ratio.55
ETIOLOGY AND PATHOGENESIS.
The disorder results from mutations in RMRP, the
RNA component of a ribonucleoprotein endoribonuclease.56 RNase MRP cleaves RNA primers
responsible for DNA replication in mitochondria
and in the nucleolus processes pre-rRNA. CHH has
been mapped to 9p13.57 Forty different mutations
have been described, most commonly 70A>G.
Mutations alter ribosomal processing, leading to
altered cytokine signaling and cell cycle progression in terminally differentiating lymphocytes and
chondrocytes.58 Most patients have defective cellmediated immunity, and patients may be particularly susceptible to severe disseminated varicella.55
Fifty-seven percent of patients have a decreased
CD4+ cell count with a decreased total count of T
lymphocytes and a subnormal CD4+/CD8+ ratio.55
A subset of patients, particularly those of Finnish
origin, also has defective humoral immunity; 35% of
patients have a deficiency of IgA or IgG subclasses
or a combination.55
CLINICAL FINDINGS.
Patients have fine, sparse, hypopigmented hair
(eFig. 143-5.1), and metaphyseal dysostosis that
results in short-limbed dwarfism. Patients may have
soft, doughy skin with degenerated elastic tissue.
Chronic oral fungal or viral infections as well as
recurrent upper respiratory infections, otitis media,
and pneumonias are related to defective cellular
and humoral immunity. Associated pleiotropic
features include Hirschsprung disease, deficient
erythrogenesis, and an increased risk of malignancies,59 particularly non-Hodgkin lymphoma and
basal cell carcinomas. There is a marked variation in
the clinical phenotype of patients with RMRP mutations including severe immunodeficiency without
any other features.60
PROGNOSIS, CLINICAL COURSE, AND
TREATMENT.
Supportive therapy with appropriate antibiotic
treatment is indicated. Bone marrow transplantation, although rarely performed, has fully corrected
the immune deficiency but has no influence on the
course of the chondroplasia or elastic tissue. A DNA
marker-based analysis provides a useful method for
prenatal diagnosis.
COMBINED ANTIBODY AND
T-CELL DEFICIENCY
Hyperimmunoglobulin M
Syndrome
EPIDEMIOLOGY.
The disorder usually occurs in males, with X-linked
inheritance in approximately 70% of affected individuals.61 Incidence is approximately 1 in 1 million
live births.62 An X-linked recessive form caused by
mutations in CD40 ligand (CD154) gene and three
autosomal recessive forms caused by mutations
in CD40 or downstream signaling pathway components [activation-induced cytidine deaminase
(AICD) and uracil-N-glycosylase (UNG)] have been
described.63
PATHOGENESIS.
Hyper-IgM syndrome is caused by a defect of B-cell
differentiation secondary to a failure of TB cell
interaction via CD40 ligand-CD40 pathway.62,63 Mature B cells expressing IgM and IgD on their surface
develop normally but fail to undergo T cell (CD40
ligand)-dependent Ig isotype switching to produce
IgG, IgA, or IgE antibodies. Some patients have detectable IgA levels in their serum, which is thought
to occur in a CD40 ligand-independent manner. Ig
isotype switching is a mechanism by which the
immune system produces antibodies with different
effector function while retaining variable region
(antigen) specificity (see Chapter 10).
Normally, isotype switching in B cells requires a
contact-dependent signal from T cells delivered by
CD40 ligand on activated T cells to CD40, a glycoprotein on the surface of B cells. Most patients with
hyper-IgM syndrome have a mutation in the gene
that encodes CD40 ligand, located on the X chromosome. T cells from patients with the syndrome
cannot synthesize CD40 ligand, or in some cases a
Copyright McGraw-Hill Companies, Inc. All rights reserved.
Chapter 143:
nonfunctional ligand is produced. B cells respond
to antigen and produce specific antibodies; however, they are restricted to the IgM isotype, and there
is no memory response. Patients with CD40 ligand
deficiency may have defective antigen-induced
T-cell proliferation64 and defective T-cell effector
function.65,Elevations of IgM in the face of immunodeficiency have also been described in some
patients with hypohidrotic ectodermal dysplasia
due to defects in the gene encoding nuclear factor
B essential modulator (NEMO), also an X-linked
recessive disease (see Ectodermal Dysplasia with
Immunodeficiency).6668
In contrast to X-linked agammaglobulinemia,
female carriers of the hyper-IgM syndrome due to
mutations in CD40 ligand have random inactivation
of the X chromosome in T lymphocytes because
CD40 ligand is not required for the normal development of T lymphocytes. Female carriers, in general,
do not show clinical manifestations. However, a
female carrier who was noted to have 95% of her
T cells expressing the mutant X chromosome had
recurrent infections of the upper and lower respiratory tract69 and another carrier had gastric lymphoma.70
CLINICAL FINDINGS.
More than one-half of patients develop symptoms
of immunodeficiency and are diagnosed before
age 1 year. Nearly all patients have symptoms by
4 years of age.62 Most notable are respiratory tract
infections, seen in 81% of patients,62 dermatitis, an
increased incidence and severity of warts, and oral
ulcerations, sometimes in association with neutropenia.71,72 Cellulitis and subcutaneous abscesses
are seen in 13% of patients.62 Recurrent diarrhea,
central nervous system (CNS) infections, and sepsis
are also common. Patients with X-linked hyper-IgM
(CD40 ligand defects) and autosomal recessive
defects in CD40 have a T cell immunodeficiency in
addition to the antibody deficiency and are prone
to opportunistic infections, including P. jiroveci.63
These patients have small lymph nodes without
germinal centers. In contrast, patients with hyperIgM syndrome caused by mutations in AICD or UNG
have lymphoid hyperplasia, but do not appear to
be susceptible to opportunistic infections because
the defect only affects B cells and CD40-dependent
costimulation of T cells by antigen-presenting
cells is not affected. Hyper-IgM patients have an
Genetic Immunodeficiency Diseases 223
increased frequency of autoimmune disorders, especially of the hematopoietic system. Uncontrolled
proliferation of IgM-producing plasma cells often
occurs during the second decade of life, at times
resulting in potentially fatal, massive infiltration
of the GI tract, liver, and gallbladder. Patients with
hyper-IgM syndrome also have an increased risk of
cancer involving the GI tract. The sera of patients
with hyper-IgM syndrome have very low amounts
of IgG, IgA, and IgE. Although levels of IgM and IgD
may be normal or high, high levels of IgM are actually found in fewer than one-third of patients.62
PROGNOSIS, CLINICAL COURSE, AND
TREATMENT.
The leading causes of death are pneumonia,
encephalitis, and malignancy. The condition is
treated prophylactically with Ig replacement and
P. jiroveci prophylaxis; neutropenia may respond to
granulocyte-macrophage colony-stimulating factor.
Few patients survive beyond the third decade.62
Allogeneic bone marrow transplantation can correct the immunodeficiency even if liver disease is
present.73,74
Severe Combined
Immunodeficiency
EPIDEMIOLOGY.
Severe combined immunodeficiency (SCID)
includes a group of heterogeneous disorders
characterized by similar clinical manifestations and
immunologic deficiencies of both humoral and cellmediated immunity.8688 The overall incidence of
SCID is 1 in 75,000 births.89 The mode of inheritance
is either X-linked or autosomal recessive.
PATHOGENESIS.
All patients with SCID share most clinical features
and have abnormalities of both cell-mediated
and humoral immunity, although the extent of
deficiency is variable. The underlying basis of SCID
is the absence of T cells or the absence of T cell
function. B cells and NK cells may or may not be
present and SCID can be categorized based on the
presence or absence of all three types of lymphocytes. The underlying genetic defect (Table 143-4)
also correlates with the cellular phenotype. Ninetyfive percent of SCID cases have an identified gene
defect.90 SCID with absence of all three cell types
Copyright McGraw-Hill Companies, Inc. All rights reserved.
224 Chapter 143: Genetic Immunodeficiency Diseases
usually results from reticular dysgenesis or from
the accumulation of toxic metabolites in patients
with mutations in the gene for the purine-degradation enzyme adenosine deaminase (ADA, 16%
of patients) or purine nucleoside phosphorylase
(PNP).91 X-linked SCID affects approximately 46%
of patients, and is characterized by the absence of
T cells and NK cells. B cells are present in normal or
slightly reduced numbers. The genetic defect is a
mutation in the gene encoding the c chain of the
IL-2 receptor, which is also shared with five other
interleukin receptors, including the interleukin 7
receptor (IL-7R) and IL-15R, which are required for
T cell and NK cell development, respectively. Janus
kinase 3 is a signaling molecule downstream of
the c chain and is mutated in autosomal recessive
SCID with a similar cellular phenotype as X-linked
SCID. In contrast, mutations in the gene encoding
interleukin 7 receptor chain (IL-7R) only affects
T cell development and patients with this form of
SCID have no T cells but have normal numbers of B
cells and NK cells.92 Genetic defects that affect the
recombination of antigen receptors on T cells and
B cells including gene defects in recombination-activating gene 1 or 2 (RAG1 or RAG2) or Artemis gene
result in SCID with no T cells or B cells but normal
numbers of NK cells.89
Mutations in the genes that encode the CD3
and CD3 chains of the T-cell antigen receptor/
CD3 complex account for less than 1% of cases.89
Mutations in the gene for CD45 (phosphatase that
regulates immune cell signaling),92 LIG4 (ligase required for DNA repair),93 and CD8A (which enables
differentiation of memory CD8+ cells)94 also cause
SCID. These molecular defects all result in total or
selective lymphopenia. Additional defects fail to
completely block T-cell differentiation but the resultant T cells are functionally impaired. These include
ZAP-70 deficiency,95 CD3 chain deficiency,96 MHC
class II deficiency and MHC class I deficiency/transporter for antigen presentation (TAP) deficiency.
The human homolog of the nude mouse with total
alopecia and nail dystrophy has been linked to
mutations in WHN (winged helix nude) (see Table
143-4).97
Clinical Findings
The subtype of SCID is generally determined by
flow cytometry for the presence or absence of T
cells, B cells, NK cells, and other specific cell surface
markers, and confirmed by DNA analysis for known
gene defects. All subtypes have absent or low T-cell
number and function, and total lymphocyte counts
are usually <1,500 to 2,000 cells (normal is >3,000).
With maternal engraftment, T lymphocyte counts
may be close to normal. The number of B cells and
NK cells differs depending on the genetic defect
(see Table 143-4). ADA and PNP enzyme activity in
leukocytes can be measured to confirm ADA- or
PNP-deficient SCID.
In families with a previously affected sibling of
a known phenotype, prenatal detection of SCID
is possible by DNA analysis (if the gene defect is
known), by fluorescence-activated cell sorting
of fetal blood with monoclonal antibodies, or by
analysis of enzyme levels in cultured amniocytes.
Carrier mothers of boys with X-linked SCID may be
detected by the selective inactivation of the abnormal X chromosome in T cells.
PROGNOSIS, CLINICAL COURSE, AND
TREATMENT.
Affected children with most forms of SCID rarely
survive beyond 1 year of age without transplantation. The definitive treatment of choice for SCID
is a hematopoietic stem cell transplant from
HLA-identical or haploidentical T-cell-depleted
bone marrow.105 Removal of postthymic cells from
parental marrow may diminish the risk of GVHD
in patients with SCID without an HLA-identical
donor. Bone marrow transplants done before the
age of 3 months have a 95% survival rate, whereas
after 3 months of age, the survival rate decreases
to 75%,106 emphasizing the importance of early
diagnosis. Hematopoietic stem cell transplant may
not result in complete immune reconstitution in regards to B-cell function and many patients remain
dependent on Ig replacement and prophylactic
antibiotics. Some patients develop waning T-cell
numbers years after transplant. In utero transfer
of haploidentical CD34 cells and retroviral gene
therapy105 have been successful for patients with
c- and ADA-deficient forms of SCID. The success of
gene therapy has been tempered by the development of leukemia in three patients who received
retroviral gene therapy for c SCID. Gene therapy
is currently restricted to patients who are unlikely
to survive allogenic transplantation or who have
already undergone standard transplantation but
do not have satisfactory T-cell immunity.105 Patients
with IL-2 deficiency have been treated with IL-2
injections. Enzyme replacement therapy with polyethylene glycol modified bovine ADA, administered
Copyright McGraw-Hill Companies, Inc. All rights reserved.
Chapter 143:
subcutaneously 12 times weekly, has resulted in
clinical and immunologic improvement in patients
with ADA deficiency. Gene therapy is also being
used for the treatment of ADA-deficient SCID.107
Ataxia-Telangiectasia
ETIOLOGY AND PATHOGENESIS.
AT results from mutations in ataxia-telangiectasia
mutated (ATM), which encodes a phosphatidylinositol 3-kinase-like serine/threonine protein kinase
that plays a central role in activating apoptotic and
cell cycle responses to DNA damage.124 More than
400 different ATM mutations have been identified in patients with AT. The MRE11-RAD50-NBS1
(MRN) complex senses DNA breaks and recruits
and activates ATM.125 The autophosphorylated ATM
monomers then phosphorylate and thus activate
several targets, among them p53, BRCA1, and NBS1
and MRE11 themselves, leading to cell cycle arrest
and facilitated DNA repair. The activation of ATM
occurs in response to external damage, such as
from ionizing radiation and radiomimetic agents
(bleomycin), and in physiologic DNA breaks, such
as during meiosis, telomere maintenance, and V(D)
J recombination in lymphocytes.124 These important roles of ATM explain the immunodeficiency,
premature aging, progressive neurologic deterioration, and sensitivity to ionizing radiation. Oxidative
stress related to ATM dysfunction has also been
implicated.
Mutations in the NBS1 and MRE11 genes, respectively, cause Nijmegen breakage syndrome (immunodeficiency with microcephaly, chromosomal
instability, and a cancer predisposition, but no
ataxia)126 and AT-like disorder (with neurologic
manifestations and radiosensitivity, but no telangiectasias).
DISORDERS OF PHAGOCYTOSIS
AND CELL KILLING
Leukocyte Adhesion Deficiencies
EPIDEMIOLOGY.
Three autosomal recessive disorders are grouped
under the term leukocyte adhesion deficiency (LAD)
that are characterized by the inability of neutrophils
to reach sites of infection.
Genetic Immunodeficiency Diseases 225
ETIOLOGY AND PATHOGENESIS.
The LADs are rare inherited disorders that affect the
ability of neutrophils to emigrate to sites of infection by disrupting one of several steps in the adhesion cascade.145 Adherence of leukocytes relates
in part to a group of cell surface glycoproteins (2
integrins) that share a common 95-kDa 2 subunit
(CD18) encoded on chromosome 21q22.3. This 2
subunit may be linked to three distinct chains to
form three different surface glycoproteins(1) the
iC3b receptor (CR3), (2) lymphocyte function-associated antigen 1, and (3) p150,95. A mutation in the
gene encoding CD18 leads to absent or deficient
surface glycoproteins in LAD1. As a result, neutrophil and monocyte chemotaxis and phagocytosis
are impaired. The first step in the adhesion cascade
involves rolling of leukocytes on vascular endothelium mediated by sialyl Lewis X (CD15s) and other
selectin ligands. LAD2 results from defects in fucose
metabolism and the absence of selectin ligands
on the surface of leukocytes. LAD3 is caused by a
defect in the regulation of the GTPase activating
protein Rap-1 resulting in defective activation of all
integrins (1,2,3-integrins).
CLINICAL FINDINGS.
Patients have frequent infections of the skin and
the respiratory and GI tracts, often caused by
S. aureus or Gram-negative enteric bacteria. The
skin infections are often precipitated by puncture
wounds or skin surface trauma and begin as small
erythematous or necrotic abscesses, progressing
to large ulcerative lesions that resemble pyoderma
gangrenosum, but the inflammatory response and
production of purulent material are impaired (eFig.
143-10.1). Histopathology often reveals complete
absence of tissue neutrophils. Poor wound healing
leads to paper-thin or dysplastic cutaneous scars.
Cellulitis of the face and perirectal area is common.
Gingivitis with periodontitis results in loss of teeth.
Delayed umbilical cord separation and omphalitis
are also characteristic features of LAD1.
Patients with LAD2 have less severe infections but
have developmental delay and the Bombay (hh)
erythrocyte phenotype. LAD3 is similar to LAD1 but
has an associated bleeding tendency.
LABORATORY ABNORMALITIES.
Laboratory examinations reveal a persistent leukocytosis, often out of proportion to the degree of
symptoms. Diagnosis is confirmed by showing the
reduction of glycoproteins or lack of upregulation
Copyright McGraw-Hill Companies, Inc. All rights reserved.
226 Chapter 143: Genetic Immunodeficiency Diseases
after stimulation with flow cytometry using monoclonal antibodies specific for the three subunits,
CD15s, and the common CD18 subunits.
PROGNOSIS, CLINICAL COURSE, AND
TREATMENT.
The severity of clinical involvement is proportional
to the degree of glycoprotein deficiency. Patients
with severe phenotypes (<1% of normal expression of CD18) present in the newborn period with
delayed umbilical cord separation and omphalitis.
Life-threatening severe bacterial or fungal infections occur with a mortality rate of more than 75%
before the age of 5 years.145 Patients with moderate
phenotype (1% to 30% of normal expression of
CD18) often have a milder course and are diagnosed later in life. More than one-half of these
patients die between the ages of 10 and 30 years.
Antimicrobial therapy is the mainstay of treatment.
Skin abscesses/ulcers often require debridement
and grafting. Bone marrow transplantation restores
leukocyte function and is recommended in patients
with the severe phenotype. Successful treatment
of LAD by allogeneic stem cell transplantation has
been reported.146 Gene therapy introducing the
normal CD18 subunit gene into affected hematopoietic stem cells has successfully restored CD18 expression. The ex vivo transfer of CD18 into affected
cells, followed by infusion of the transduced cells,
may represent another therapeutic approach.147
Oral fucose replacement has been helpful in some
patients with LAD2. Leukocyte adhesion molecules
are expressed on fetal leukocytes and make prenatal diagnosis possible by fetal blood sampling at
20-weeks gestation.
COMPLEMENT DEFICIENCY
DISORDERS
The complement system represents an enzymatic
reaction cascade that involves three major initial
pathways [(1) classicalC1, C4, C2; (2) lectin; and
(3) alternativeC3, factors B, D, H, and I, properdin]
and a shared terminal pathway (membrane attack
complexC5C9) (see Chapter 37). Complement
proteins regulate humoral and cellular immune
functions, and participate in the killing of bacterial
organisms. Abnormalities of the complement system tend to manifest as increased susceptibility to
bacterial organisms or autoimmune disorders.176,177
Epidemiology
The most common hereditary complement
disorder is C2 deficiency, which can result from a
defect in either protein synthesis (type 1) or secretion (type 2); 1% to 2% of the Caucasian population
is heterozygote178 and 0.005% are homozygote.179
The deficiency is usually caused by a 28-base pair
deletion in the C2 gene. Homozygous deficiencies
of C1q, C1r, C1s, and C4 (C4A or C4B) are rare, but
manifest with autoimmune disease more frequently
than homozygous C2 deficiency. The incidence of
SLE in patients with C1q, C4, and C1r is 93%, 75%,
and 57%, respectively; in contrast, SLE only occurs
in 10% with C2 deficiency (25% if homozygous).176
Total deficiency of mannan-binding lectin (MBL)
is the most common among homozygote states
(approximately 3%), although clinical penetrance
is low.180 In addition, approximately 0.01% of
individuals have a homozygous deficiency in the
MBL-associated serum protease, which is activated
by MBL binding to the surface carbohydrates
of bacteria and generates classical pathway C3
convertase via cleavage of C4 and C2. Excluding
deficiency of MBL, however, homozygote forms
of complement deficiency represent 0.03% of the
population. In general, heterozygotes produce sufficient complement to ensure function and remain
asymptomatic, so individuals who manifest complement disorders tend to be homozygotes. Hereditary
angioedema (HAE), on the other hand, manifests
in heterozygotes with deficiency or dysfunction of
the C1 inhibitor (C1 INH) (see Section Hereditary
Angioedema). Despite the rarity of homozygous
deficiency the incidence of complement deficiency
in patients with recurrent neisserial infection has
been found to be as high as 20%. In patients with
autoimmune disorders, such as SLE, the incidence
of C2 deficiency is approximately 7%178 and of MBL
deficiency is increased two- to threefold. Properdin
deficiency is the only X-linked complement deficiency and all known patients are male.
Etiology and Pathogenesis
Defects involving the early components of the
classical complement pathway (C1, C4, C2) manifest
with an increased incidence of autoimmune disorders, especially SLE (Table 143-9). The reason for the
increased incidence of autoimmune disorders and
particularly lupus in patients with complement deficiency is unclear. The genes that encode C4A, C4B,
Copyright McGraw-Hill Companies, Inc. All rights reserved.
Chapter 143:
C2, and factor B are localized to the MHC region
on chromosome 6; just as HLA types have been
linked to SLE (e.g., HLA A1, B8, DR3), gene alterations in this region may play a role in generation of
autoimmunity. One functional hypothesis links the
development of lupus with impaired clearance of
apoptotic cells of the skin and kidneys that present
autoantigens.181 Binding of C1q results in classical
pathway activation and facilitates the uptake of
apoptotic cells by phagocytes. C1q-deficient mice
show histological evidence of glomerulonephritis
characterized by apoptotic cell bodies and immune
deposits.182 In addition, cultured keratinocytes
undergoing UVB-induced apoptosis preferentially
display autoantigens such as Ro in plasma membrane blebs, which may lead to its presentation to T
cells and generation of autoantibodies; however, no
difference in the rate of clearance of sunburn cells
was found in C1q-deficient mice and chronic ultraviolet exposure did not result in the production of
autoantibodies or the development of glomerulonephritis.183 Decreased MBL-mediated clearance of
apoptotic cells may also explain the occurrence of
SLE in MBL deficiency. Complement components
are also important for handling immune complexes
and maintenance of B cell tolerance.183,184
The variety of recurrent infections associated
with complement deficiencies underscores the key
role of complement in bacterial clearance. Patients
with a deficiency of the early classical components,
especially C2, have a mildly increased susceptibility
to infections with encapsulated bacteria. Opsonization of bacteria and fungi may be ineffective in disorders of the classical pathway because of the slow,
inadequate formation of C3b. However, the development of infection is likely mitigated by the ability
of the lectin and alternative pathways to generate
C3, thus bypassing the early classical pathway (see
Chapter 37). C5 deficiencies result in impaired
generation of chemotactic factors, which may lead
to inadequate neutrophil function. Individuals with
C5 to C9 (membrane attack complex) deficiencies typically develop chronic recurrent neisserial
infections as teenagers, reflecting the role of the
terminal complement pathway in the destruction of
these organisms. Similarly, the effect of properdin
in stabilizing the alternative C3 convertase is critical
for killing of organisms because properdin deficiency leads to fulminant neisserial infections. Manifestations of complement deficiency may also result
from alterations in the regulators of the complement pathway that lead to uncontrolled activation
of the complement cascade (see Chapter 37).
Genetic Immunodeficiency Diseases 227
Clinical Features
Cutaneous and joint findings of lupus erythematosus (see Chapter 155) are the most common
autoimmune manifestation of deficiency of the
early complement components (see Table 143-9),
and often first show manifestations during childhood. Manifestations of deficiency of C2 are seen
most commonly, given its prevalence, but homozygous C1q deficiency is the strongest single genetic
risk factor for SLE identified to date. In general, the
lupus associated with C2 deficiency is milder than
that associated with deficiency of other classical
complement components (eFig. 143-14.1), which
have an earlier onset, and increased risk of associated glomerulonephritis. In addition to patients
who meet criteria for lupus erythematosus, undifferentiated connective tissue disease and vasculitis
are the most common autoimmune manifestations
in individuals with C2 deficiency. C2 deficiency has
also been found in patients with dermatomyositis, juvenile rheumatoid arthritis, atrophoderma,
HenochSchnlein purpura, cold urticaria, and
inflammatory bowel disease.
The most common feature of lupus in persons
with C2 deficiency is photosensitivity, and lesions
typical of subacute cutaneous lupus are seen more
often than those of acute cutaneous lupus (see eFig.
143-14.1) or discoid lupus. Oral ulcerations are present in approximately 50% of affected individuals,
and cicatricial alopecia may occur. In general, the
lesions may be more resistant than those of lupus
without complement deficiency, but noncutaneous
manifestations tend to be less severe. Arthralgias or
arthritis is seen in 80%, but renal disease tends to
be mild or occult. C2 deficiency and C4 deficiency
lupus are unlikely to be associated with elevated
antinuclear antibody titers or anti-DNA antibodies, but 75% of patients have detectable anti-Ro
antibodies.
Direct immunofluorescence may show deposition but is more likely to be negative than in lupus
unrelated to C2 deficiency. Leukopenia has been
described in 50% of affected individuals and rheumatoid factor in 40%. Although most individuals
with MBL deficiency show no clinical manifestations, deficiency of MBL or its associated serum
protease is also associated with an increased risk of
SLE, and MBL deficiency has been described with
dermatomyositis. In patients with SLE, having MBL
deficiency is associated with a higher risk of bacterial complications. The risk of SLE is also increased in
Copyright McGraw-Hill Companies, Inc. All rights reserved.
228 Chapter 143: Genetic Immunodeficiency Diseases
individuals with deficiencies in C3 or regulators of
the complement pathway, such as factor H or factor
I (C3b inactivator). Approximately 5% of individuals
with deficiency of the late complement components have evidence of immune complex or autoimmune disease, and these manifestations have not
been described with properdin deficiency.
zygous C2 deficiency,176 and has been described in
mannan-binding ligand deficiency and experimental C3 deficiency as well; the reason for the association is unclear.
The bacterial organisms that cause problems in
complement deficiency of classical components
are encapsulated bacteria, including Pneumococcus
and H. influenzae. Infections can be severe with an
onset during infancy and childhood.185,186 A recent
retrospective study of 40 patients with homozygous C2 deficiency over a mean of 39 years (range,
177 years) found that severe infection was the
predominant clinical manifestation176; 23 patients
had a history of septicemia or meningitis caused by
Pneumococcus, and in 12 the infections were recurrent. Nineteen patients had at least one episode of
pneumonia, with recurrence in 10 affected individuals.
In complement deficiencies other than HAE,
total hemolytic complement (CH50) is markedly
decreased (e.g., in C9 deficiency) or undetectable
(most complement deficiencies). The alternative
pathway lytic test (AP50) is less sensitive than the
CH50, but may be useful to screen for deficiencies
in the alternative pathway components. Levels of
specific complement components and MBL are
generally measured by enzyme-linked immunosorbent assay or radial immunodiffusion assays.177
Although usually absent with C2 deficiency itself,
anti-Ro antibodies are present in three-fourths of
patients with C2 deficiency who have SLE.
With deficiency of components of the membrane
attack complex or regulators of the alternative
pathway, particularly properdin deficiency, infections most commonly begin in teenage years and
are caused by neisserial organisms, particularly
meningococcus. Properdin deficiency is associated
with fulminant meningococcal disease that can
lead to death in up to 28% of patients and usually
manifests as a single episode, but the neisserial
disease with deficiency of the late complement
components tends to be recurrent and of lesser
severity, only occasionally leading to death.
Progressive partial lipodystrophy involving
the thoracic or cephalothoracic region has been
described with hereditary deficiency of C3.187
Although more commonly acquired, the condition
has been described in siblings, suggesting autosomal recessive inheritance; affected individuals may
show associated membranoproliferative glomerulonephritis, insulin resistance and an increased
incidence of autoimmune diseases. The Leiner
phenotype of generalized erythroderma, failure to
thrive, diarrhea, and increased infections has been
described with deficiency of C5 or deficiency or
dysfunction of C3. An atypical form of hemolytic
uremic syndrome that is not associated with diarrhea has been reported with heterozygous mutations in factor H and in the membrane cofactor
protein (MCP) CD46, a complement regulator.188
Atherosclerosis has recently been linked to homo-
Laboratory Abnormalities
Differential Diagnosis
Secondary decreases in complement levels may
be seen in patients with a variety of disorders,
most commonly in SLE and hypocomplementemic
vasculitis. Complement levels may also be reduced
by bacterial (particularly endocarditis) and viral
infections, hepatic disease, myeloma, malnutrition
including anorexia nervosa, and medications that
may cause a lupus-like syndrome (especially hydralazine, penicillamine, and procainamide). The Leiner
phenotype of erythroderma with failure to thrive,
originally described with complement abnormalities, has been described in patients with HIES, SCID,
and X-linked agammaglobulinemia.
Treatment
Traditional management of lupus erythematosus is appropriate for patients with complement
deficiency and should be chosen based on clinical
manifestations. Topical anti-inflammatory medications and sun protection may adequately treat
milder cases with cutaneous findings, but antimalarial medications, systemic corticosteroids, and
other immunosuppressive drugs may be required
for more severe cases; given the increased risk of
infections in patients with complement deficiency,
careful monitoring is critical. The use of plasma
transfusions to replace the deficient components
Copyright McGraw-Hill Companies, Inc. All rights reserved.
Chapter 143:
Genetic Immunodeficiency Diseases 229
may actually activate the cascade and accelerate
immune complex deposition. If fever or other signs
of infection occurs, cultures should be obtained
with a low threshold for administration of antibiotics. Accumulating evidence suggests the value
of immunization of the patient and household
contacts for Pneumococci, H. influenzae, and N.
meningitides. In individuals with deficiency of the
membrane attack complex who received meningococcal polysaccharide vaccine(s), antibody levels
against the meningococcal polysaccharides were
detectable within a month and remained elevated
for 3 years, concurrent with a significant decrease in
the risk of meningococcal disease during a 38-year
period of observation.189 Replacement therapy with
recombinant complement proteins may be available in the near future.
Copyright McGraw-Hill Companies, Inc. All rights reserved.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Child Psych and Dev - Prenatal and Postpartum Maternal Psychological Distress and Infant DevelopmentDocument32 pagesChild Psych and Dev - Prenatal and Postpartum Maternal Psychological Distress and Infant DevelopmentAnnisa Chaerani BurhanuddinNo ratings yet
- Management of Postpartum DepressionDocument12 pagesManagement of Postpartum DepressionAnnisa Chaerani BurhanuddinNo ratings yet
- Campbell-Walsh Urology, 10th Edition 2012Document1 pageCampbell-Walsh Urology, 10th Edition 2012Annisa Chaerani BurhanuddinNo ratings yet
- Perioperative Intravenous Fluid Therapy For Adults: Rob Mac Sweeney, Rachel Alexandra Mckendry, Amit BediDocument8 pagesPerioperative Intravenous Fluid Therapy For Adults: Rob Mac Sweeney, Rachel Alexandra Mckendry, Amit BediAnnisa Chaerani BurhanuddinNo ratings yet
- PBL Skenario 1: Anak Kurus: Blok Biomedik 2Document2 pagesPBL Skenario 1: Anak Kurus: Blok Biomedik 2Annisa Chaerani BurhanuddinNo ratings yet
- Epidural Analgesia - A Self-Directed Learning Module 3rdDocument41 pagesEpidural Analgesia - A Self-Directed Learning Module 3rdAnnisa Chaerani BurhanuddinNo ratings yet
- Conners Comprehensive Behavior Rating ScaleDocument28 pagesConners Comprehensive Behavior Rating ScaleAnnisa Chaerani Burhanuddin60% (5)
- PhototherapyDocument7 pagesPhototherapyAnnisa Chaerani BurhanuddinNo ratings yet
- CCC Adhd TestingDocument6 pagesCCC Adhd TestingAnnisa Chaerani Burhanuddin100% (1)
- PhotoprotectionDocument1 pagePhotoprotectionAnnisa Chaerani BurhanuddinNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- XXXXXX 121Document11 pagesXXXXXX 121AndriantkNo ratings yet
- Ventilator Graphics & Trouble-Shooting - EditedDocument64 pagesVentilator Graphics & Trouble-Shooting - EditedAbhishek SinghNo ratings yet
- Nursing Care of A Hospitalized ChildDocument17 pagesNursing Care of A Hospitalized ChildtinaNo ratings yet
- ShockDocument53 pagesShockHassan Ahmed100% (3)
- Vertical Root Fracture !Document42 pagesVertical Root Fracture !Dr Dithy kkNo ratings yet
- Diabetic Nephropathy BaruDocument24 pagesDiabetic Nephropathy BaruRobiyanti Nur Chalifah HattaNo ratings yet
- @MBS MedicalBooksStore 2020 CompressionDocument46 pages@MBS MedicalBooksStore 2020 CompressionTaufikNo ratings yet
- Complications of Insulin TherapyDocument16 pagesComplications of Insulin TherapyIngrid NicolasNo ratings yet
- Nur 601 - Literature Review Manuscript-Icd-10-Sunny Carrington-HahnDocument22 pagesNur 601 - Literature Review Manuscript-Icd-10-Sunny Carrington-Hahnapi-357138638No ratings yet
- Anatomy and Physiology - Dengue FeverDocument3 pagesAnatomy and Physiology - Dengue Feverhael yam62% (13)
- Worksheet 4, Ubaidillah, 3BDocument6 pagesWorksheet 4, Ubaidillah, 3BUbay SegaNo ratings yet
- Operative ProcedureDocument22 pagesOperative Procedurezianab aliNo ratings yet
- CH 14 Antepartum Nursing Assessment NotesDocument8 pagesCH 14 Antepartum Nursing Assessment NotesMary LowryNo ratings yet
- OS Pharmacy L III - IVDocument125 pagesOS Pharmacy L III - IVashagrie67% (3)
- Lesson Plan On Spina BifidaDocument24 pagesLesson Plan On Spina BifidaPriyaNo ratings yet
- Feeling GreatDocument243 pagesFeeling GreatSunny LamNo ratings yet
- On and Off Male Birth Control MethodsDocument2 pagesOn and Off Male Birth Control MethodsLeón L.PNo ratings yet
- Medication AdministrationDocument8 pagesMedication AdministrationMarku LeeNo ratings yet
- Nurse Shift PDFDocument11 pagesNurse Shift PDFWisnu YogaNo ratings yet
- Lipo LaserDocument13 pagesLipo LaserLuis A Gil Pantoja100% (1)
- APA Practice Guideline For The Treatment of Patients With Substance Use DisordersDocument276 pagesAPA Practice Guideline For The Treatment of Patients With Substance Use DisordersRaja Ahmad Rusdan MusyawirNo ratings yet
- Case Study 5 Dengue Fever CorrectedDocument13 pagesCase Study 5 Dengue Fever CorrectedyounggirldavidNo ratings yet
- Treating Canine Distemper VirusDocument23 pagesTreating Canine Distemper VirusJack HollandNo ratings yet
- Salmonella Typhi 2012Document60 pagesSalmonella Typhi 2012Mohd Syaiful Mohd ArisNo ratings yet
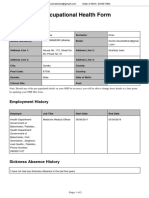
- Occupational Health Form: General DetailsDocument2 pagesOccupational Health Form: General DetailsKhushal khanNo ratings yet
- Lista Preturi Teste Genetice GendiaDocument227 pagesLista Preturi Teste Genetice GendiaMatei FloriNo ratings yet
- Aatru Medical Announces FDA Clearance and Commercial Launch of The NPSIMS™ - Negative Pressure Surgical Incision Management SystemDocument4 pagesAatru Medical Announces FDA Clearance and Commercial Launch of The NPSIMS™ - Negative Pressure Surgical Incision Management SystemPR.comNo ratings yet
- Probiotic Supplementation For Prevention of Atopic Dermatitis in Infants and Children: A Systematic Review and Meta AnalysisDocument11 pagesProbiotic Supplementation For Prevention of Atopic Dermatitis in Infants and Children: A Systematic Review and Meta AnalysisGrace Malinda LimopranotoNo ratings yet
- COVID-19 and Pregnancy: A Review of Clinical Characteristics, Obstetric Outcomes and Vertical TransmissionDocument20 pagesCOVID-19 and Pregnancy: A Review of Clinical Characteristics, Obstetric Outcomes and Vertical TransmissionDra Sandra VèlezNo ratings yet
- SeizureDocument10 pagesSeizureRomeo ReyesNo ratings yet