Professional Documents
Culture Documents
Feeding Difficulties in Infants and Young Children
Uploaded by
Argadia YuniriyadiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Feeding Difficulties in Infants and Young Children
Uploaded by
Argadia YuniriyadiCopyright:
Available Formats
I N T E G R AT I V E M E D I C I N E
Feeding Difficulties in Infants and Young Children:
Tailor Interventions to Match Child Behaviours
Editorial:
Glenn Berall, MD, FRCPC
Chief of Pediatrics, North York General Hospital
Assistant Professor of Paediatrics, Division of Gastroenterology, Hepatology and Nutrition
University of Toronto
Toronto, Ontario
Miami Summit, June 2009 Feeding difficulties in infants and young children are highly prevalent and pediatricians
need to pay close attention to parental complaints in order to identify and categorize the chief problem and tailor
interventions accordingly. This report presents an expert categorization of feeding difficulties and appropriate
consequent treatments. Parental education and reassurance is often sufficient to resolve many feeding issues;
however, providing a nutritionally balanced supplement may help correct malnutrition and ease parental anxiety.
Feeding difficulties in infants and young children are among
the most prevalent complaints encountered in the average
pediatric practice today. Estimates of their prevalence vary but
in physically normal children, 50% to 60% of surveyed parents
report feeding difficulties with their young children, while 25%
to 35% meet criteria for specific difficulties such as food refusal
and selective eating. The consequences of an untreated feeding
difficulty can include failure to thrive, nutritional deficiencies,
impaired parent/child interactions and chronic aversion with
socially stigmatizing mealtime behaviour. As well, a feeding
difficulty can be a sign of an underlying organic disorder such
as eosinophilic esophagitis. It is therefore important to identify
the type of feeding difficulty present.
Categorization of Feeding Difficulties
In pediatrics, a variety of terms are used to categorize
different feeding difficulties, with a resulting lack of common
understanding. To that end, an attempt to apply a single
categorical description has been made by a diverse group
of experts and presented at a meeting in Miami, Florida by
Dr. Benny Kerzner, Professor of Pediatrics, The George
Washington University, Washington, DC; Thomas Linscheid,
PhD, Clinical Associate Professor of Pediatrics, Ohio
State University School of Medicine, Columbus; pediatric
gastroenterologist Dr. Russell J. Merritt, Childrens Hospital
Los Angeles, California; and Dr. Irene Chatoor, Childrens
National Medical Center and Professor of Psychiatry, George
Washington University.
Patients were placed into one of the following seven
categories, each with differing features and treatments:
1. Infants with poor appetite because of organic causes.
2. Those with poor appetite due to parental misperception.
3. Those with poor appetite who are otherwise vigorous.
4. Poor appetite in an apathetic or withdrawn child.
5. Children who display highly selective food behaviours.
6. Infants with colic that interferes with feeding.
7. Infants or children who fear feeding.
Interventional Strategies
Situating a childs feeding behaviour into one of the proposed
seven categories helps determine interventional strategies.
1. Children may have poor appetite or refuse food because of an
underlying organic cause and it is critical to systematically
exclude organic causes of poor appetite. If an organic cause is
suspected, then the appropriate investigations must be carried
out to determine the diagnosis and guide treatment. Signs that
would make one suspect underlying organic causes include
but are not limited to dysphagia; recurrent chest symptoms
or pathology; failure to thrive; feeding interrupted by pain,
regurgitation or chronic vomiting; diarrhea or blood in stool;
neurodevelopmental anomalies; atopy and eczema; chronic
cardiorespiratory disease; or signs of neglect.
2. For children with poor appetite due to parental misperception,
parents need to be educated about what they can realistically
expect in terms of their childs growth and nutritional needs
for their age. They also need to understand basic feeding
principles and apply them consistently during feedings.
Reassurance is often all that is needed to improve the
situation. If not, and parental anxiety remains high, then a
balanced nutritional supplement may be considered in order
to allay parental fears and reduce the likelihood that they will
use force or coercion to get their child to eat.
3. Children with poor appetite who are otherwise vigorous are
often more interested in playing than in feeding, are alert,
active and inquisitive but rarely show signs of hunger or
interest in feeding, and are felt by some experts to have
infantile anorexia. Typically, this behaviour occurs during
transition from spoon to self-feeding between 6 months and
3 years of age.
As discussed by Drs. Linscheid and Chatoor, treatment
of poor appetite in a child who is fundamentally vigorous
should promote the childs appetite by increasing hunger
and satisfaction from eating. Principles here include no
grazing between meals, only water; three meals a day plus
an afternoon snack; no distractions during feeding; discrete
mealtimes not longer than 30 minutes; and the use of timeout
to discourage disruptive feeding behaviours. If growth is
faltering, practitioners may recommend parents feed the
child high-calorie foods or use a 30 kilocalories-per-ounce
nutritionally balanced supplement, optimally given after the
dinner meal to least impact on appetite.
4. Poor appetite in a child who is withdrawn and depressed
may be a sign of neglect. If practitioners observe no signs
of smiling, babbling or eye contact between the infant and
caregiver during examination, the child could be at risk for
substantial weight loss and malnutrition and may require
inpatient admission to improve the feeding environment.
Consider socioeconomic circumstances, psychoneurosis in
the mother and neurological problems in the child.
5. Children who consistently refuse specific foods because of
taste, texture, smell or appearance, or who become visibly
anxious if asked to eat foods to which they are averse, often
have additional sensory difficulties. They are upset by loud
noises or they dislike the sensation of sand or grass under
their feet. Highly selective food intake or what Dr. Chatoor
calls sensory food aversion goes beyond normal resistance
to the introduction of new foods and, depending on the foods
refused, may result in deficits of some essential dietary
nutrients. In these circumstances, parents should be taught
to tempt the child with food, not foist it upon them. Parents
should themselves consume new foods without offering the
food to the child, although they can try leaving the food
within the childs reach as toddlers are often more willing
to try new foods if they feel in control. Reassuring the
parent can be helpful. Again, the diet may be supplemented
with a nutritionally balanced product to redress the risk of
micronutrient deficiencies.
6. In infants under the age of 3 months, colicdefined as
inconsolable crying not responsive to usual interventions
and with no obvious pathologycan be problematic because
infants may fail to calm down enough to feed successfully.
If the crying disrupts feeding, mothers often try to feed
infants more frequently, fearing the infant is crying because
they are hungry. Strategies to improve infants with colic
include feeding in a quiet room with dim lights and white
noise, giving the infant a warm bath to break the crying
cycle, swaddling the infant to comfort them or possibly using
kangaroo-style skin-to-skin nursing. Mothers with colicky
infants need to get adequate rest and support and fathers need
to get involved in the feeding and caring of the infant. At the
same time, infants may cry because of pain and discomfort
from feeding and practitioners need to differentiate possible
triggers for crying including food sensitivity, constipation or
gastroesophageal reflux.
7. Fear of feeding is rare, but if a child cries at the sight of food
or the bottle or resists feeding by crying, arching or refusing
to open their mouths, they may have what Dr. Chatoor refers
to as post-traumatic feeding disorder, possibly the result of
a frightening feeding experience such as choking. Parental
education is again key here. If a child fears the bottle, parents
can offer a sippy cup or spoon instead. Parents should also try
to feed the child when they are half asleep and relaxed rather
than when wide awake and stressed at the sight of food. Once
they have succeeded, they will begin to realize that they can
feed their child successfully.
Practical Tips
Anthropomorphic measurements clearly help distinguish
infants and children who are failing to thrive because of poor
appetite. It is also important for practitioners to assess parental
anxiety. If parents perceive that their child is not feeding
well, they may feel pressured to resort to coercive feeding
practices which can be detrimental and can exacerbate feeding
disorders. Acknowledgement of parental anxiety and providing
reassurance, information and a plan of action are helpful in this
regard. However, the specific approach taken depends upon the
category of feeding difficulty.
Summary
Feeding difficulties are very common in young children and they
have the potential to compromise nutrition, growth and cognitive
development. Pediatricians therefore need to pay close attention
to parental complaints about feeding difficulties to determine
the category of feeding difficulty and tailor their interventions
accordingly. This particular attempt to categorize feeding difficulties
in infants and children may serve as a guide in this regard.
To view an electronic version of this publication along with related slides if available, please visit www.mednet.ca/2009/ho10-001e.
2009 Health Odyssey International Inc. All rights reserved. Integrative Medicine Report is an independent medical news reporting service providing educational updates
reflecting peer opinion from accredited scientific medical meetings worldwide and/or published peer-reviewed medical literature. Views expressed are those of the participants and
do not necessarily reflect those of the publisher or the sponsor. Distribution of this educational publication is made possible through the support of Abbott Nutrition Canada under
written agreement that ensures independence. Any therapies mentioned in this publication should be used in accordance with the recognized prescribing information in Canada. No
claims or endorsements are made for any products, uses or doses presently under investigation. No part of this publication may be reproduced in any form or distributed without
written consent of the publisher. Information provided herein is not intended to serve as the sole basis for individual care. Our objective is to facilitate physicians and allied health
care providers understanding of current trends in medicine. Your comments are encouraged.
Health Odyssey International Inc.
132 chemin de lAnse, Vaudreuil, Quebec J7V 8P3
A member of the Medical Education Network Canada group of companies
HO10-001E ML
You might also like
- Pcsmanual Current PDFDocument355 pagesPcsmanual Current PDFArgadia YuniriyadiNo ratings yet
- Analgesic Effect of Breast Milk Versus Sucrose For Analgesia During Heel LanceDocument32 pagesAnalgesic Effect of Breast Milk Versus Sucrose For Analgesia During Heel LanceArgadia YuniriyadiNo ratings yet
- Safety and Efficacy of Vinyl Bags in Prevention of Hypothermia of Preterm Neonates at BirthDocument3 pagesSafety and Efficacy of Vinyl Bags in Prevention of Hypothermia of Preterm Neonates at BirthArgadia YuniriyadiNo ratings yet
- Skin Integrity Guideline - FinalDocument13 pagesSkin Integrity Guideline - FinalArgadia YuniriyadiNo ratings yet
- Histiocytosis: BackgroundDocument26 pagesHistiocytosis: BackgroundArgadia YuniriyadiNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Module 9 Eng Health PDFDocument80 pagesModule 9 Eng Health PDFVivica MorenoNo ratings yet
- Acute Respiratory Infections Daryl Joel Dumdum, M.DDocument5 pagesAcute Respiratory Infections Daryl Joel Dumdum, M.DJoan LuisNo ratings yet
- Compilation of MacromineralsDocument3 pagesCompilation of MacromineralsJustin AncogNo ratings yet
- 04-Nutrition COURSE PLANDocument5 pages04-Nutrition COURSE PLANPNT EXAM 2016No ratings yet
- Haccp: (Hazard Analysis Critical Control Point)Document79 pagesHaccp: (Hazard Analysis Critical Control Point)Sinta Wulandari100% (1)
- Care CWS Helen Keller Report07Document8 pagesCare CWS Helen Keller Report07Syamsul ArdiansyahNo ratings yet
- Final Revised Draft Dropout Study Report by Dr. Dawood Shah January 9 2019 (Flag B)Document83 pagesFinal Revised Draft Dropout Study Report by Dr. Dawood Shah January 9 2019 (Flag B)Khawaja SabirNo ratings yet
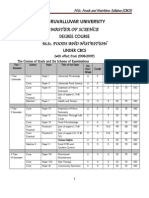
- M.sc. Foods and NutritionDocument43 pagesM.sc. Foods and NutritionGeetha Arivazhagan0% (1)
- The Role of Aquaculture in Improving The Livelihoods of Rural CommunitiesDocument4 pagesThe Role of Aquaculture in Improving The Livelihoods of Rural CommunitiesKIU PUBLICATION AND EXTENSIONNo ratings yet
- Latest Pediatrics Multiple Choice Questions and Answers - All Medical Questions and AnswersDocument4 pagesLatest Pediatrics Multiple Choice Questions and Answers - All Medical Questions and AnswersAbdul Ghaffar Abdullah90% (10)
- Nutrition Powerpoint Week 2Document20 pagesNutrition Powerpoint Week 2Shaira Kheil TumolvaNo ratings yet
- Lesson 3 Nutritional AssessmentDocument84 pagesLesson 3 Nutritional AssessmentJake ArizapaNo ratings yet
- World HungerDocument5 pagesWorld Hungerveneficus08No ratings yet
- Who Will Feed Us Questions For The Food and Climate CrisesDocument34 pagesWho Will Feed Us Questions For The Food and Climate Criseshtsmith35801No ratings yet
- Nourishing MillionsDocument236 pagesNourishing MillionsAtay UltramanNo ratings yet
- Class 9th: CH 4 Food Security in India EconomicsDocument25 pagesClass 9th: CH 4 Food Security in India EconomicsPankaj KumarNo ratings yet
- Narrative Report Siga-Indicator 3docxDocument12 pagesNarrative Report Siga-Indicator 3docxMylene Solis Dela Pena100% (7)
- How Do Barangay Nutrition Committees Contribute To Better Nutrition?Document20 pagesHow Do Barangay Nutrition Committees Contribute To Better Nutrition?Angelito CortunaNo ratings yet
- Food Security and Vision 2025Document38 pagesFood Security and Vision 2025madihaNo ratings yet
- Getaneh Et Al-2019-BMC PediatricsDocument11 pagesGetaneh Et Al-2019-BMC Pediatricszegeye GetanehNo ratings yet
- Answers To Module 2 of Urban Geography 3Document26 pagesAnswers To Module 2 of Urban Geography 3Johanisa DeriNo ratings yet
- Health Teaching PlanDocument8 pagesHealth Teaching Planrain َNo ratings yet
- 1 s2.0 S2666149722000202 MainDocument6 pages1 s2.0 S2666149722000202 MainALEXANDRE SOUSANo ratings yet
- Diet and FoodDocument2 pagesDiet and Foodneon333100% (2)
- Clup Final'08Document568 pagesClup Final'08Mae Elizabeth PugarinNo ratings yet
- FNCP PrioritizationDocument10 pagesFNCP PrioritizationSteven ConejosNo ratings yet
- Nutrition EducatorDocument13 pagesNutrition EducatorDarsan P NairNo ratings yet
- Beating Cancer With Nutrition - Optimal Nutrition Can Improve The Outcome in Medically-Treated Cancer Patients (PDFDrive)Document556 pagesBeating Cancer With Nutrition - Optimal Nutrition Can Improve The Outcome in Medically-Treated Cancer Patients (PDFDrive)Muhammad Mawardi Abdullah100% (12)
- Ajol File Journals - 475 - Articles - 141517 - Submission - Proof - 141517 5605 376681 1 10 20160805Document17 pagesAjol File Journals - 475 - Articles - 141517 - Submission - Proof - 141517 5605 376681 1 10 20160805myblackconfidentladiesNo ratings yet
- 08 Chapter-5Document114 pages08 Chapter-5Lamico Dellavvoltoio100% (1)