Professional Documents
Culture Documents
Drugs To Avoid in Myasthenia Gravis
Uploaded by
papitomalosoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drugs To Avoid in Myasthenia Gravis
Uploaded by
papitomalosoCopyright:
Available Formats
Drug Information Group
1 of 3
http://dig.pharm.uic.edu/faq/myasthenia.aspx
About the
College
Departments
Research
Education
Faculty
Rockford Campus
Alumni
Frequently Asked Questions
Drug Information Group
Department of Pharmacy
Practice
About Us
People
Publications
Contact Us
What drugs should be avoided in myasthenia gravis?
Myasthenia gravis is a rare autoimmune disease occurring in 0.25 to 2 people per 100,000
annually.1,2 Normally, for a synaptic transmission to occur at the neuromuscular junction, an
action potential must initiate depolarization of the presynaptic terminal. Once the presynaptic
terminal has been depolarized, there is an influx of calcium, which causes the release of
acetylcholine from vesicles. The acetylcholine then enters the synaptic cleft and binds to the
postsynaptic acetylcholine receptor (AChR). This interaction then causes a depolarization of
the postsynaptic terminal, which allows the signal to propagate and eventually ends in
stimulation of the muscle. In myasthenia gravis, formation of antibodies directed against the
AChR in the postsynaptic neuron form. The antibodies bind with the AChR, thus making
acetylcholine unable to complex with the AChR. This causes a decrease in the total number of
AChRs and muscle weakness due to diminished neurotransmission to the postsynaptic
membrane. The disease may be limited to the external ocular muscles (a less severe form of
the disease) or may be more generalized, involving muscles of the face, oropharyngeal areas,
upper torso, and proximal extremities. Respiratory paralysis can also occur in very severe
exacerbations. Although the disease is progressive, patients experience intermittent periods
of very active disease and remission.
Several medications are implicated in either inducing or worsening myasthenia gravis.1,3 Four
mechanisms have been described to explain the interaction of these drugs and the disease:
(1) neuronal transmission may be inhibited at the presynaptic terminal; (2) lack of
acetylcholine release (possibly related to inhibition of calcium influx into the presynaptic
terminal); (3) blockade of the postsynaptic AChRs, therefore preventing the binding of
acetylcholine to the postsynaptic AChR; and (4) prevention of action potential transmission
past the postsynaptic terminal secondary to changes in postsynaptic ion permeability.
More than 30 medications have been reported to have an effect on neuromuscular
transmission.1,3 The agents suspected in exacerbations or first presentations of myasthenia
gravis have mainly been published in case reports, therefore, it is difficult to describe a true
incidence with each agent. In addition, questionable temporal relationships or other
confounding factors sometimes make interpretation of the case reports difficult. Nonetheless,
it is prudent to use precaution when using the medications that have been implicated in
myasthenia gravis.
A simple way to remember the drugs that should be used with caution in myasthenia gravis is
the "14 As":4-7
ACTH and corticosteroids
prednisone
Analgesics
narcotics
Anesthetics, local
cocaine, procaine, lidocaine, bupivacaine,
prilocaine
Antacids or laxatives containing magnesium
Maalox, Mylanta
Antiarrhythmics
quinidine, lidocaine, procainamide
Antibiotics
aminoglycosides, quinolones, telithromycin,
azithromycin, erythromycin, clindamycin,
ampicillin, imipenem, vancomycin,
metronidazole
Anticonvulsants
phenytoin
Antihypertensives
beta-blockers, calcium channel blockers
Antimanics
lithium salts
Antipsychotics
chlorpromazine
Antirheumatic
chloroquine
Arthritis agents
penicillamine-induced myasthenia gravis
All neuromuscular blocking agents
Antimalarials
chloroquine, hydroxychloroquine
Approximately 1% to 7% of patients on penicillamine will develop myasthenia gravis.1,3
Penicillamine has been reported to induce the formation of anti-AChR antibodies in 90% of
patients who develop myasthenia gravis while on this agent. While penicillamine is very well
documented to be a cause of myasthenia gravis, there are no reports of it causing an
exacerbation in a patient already diagnosed with myasthenia gravis. Patients who develop
myasthenia gravis while receiving penicillamine typically have a mild form of the disease,
often limited to the extraocular muscles. Initial presentation of the disease varies occurring
from 2 to 12 months after therapy has begun. Most patients have resolution of the disease
within 2 to 6 months following discontinuation.
Interferon alfa has also been implicated as the cause of myasthenia gravis in patients with
leukemia or hepatitis C.3 Rat data suggest the proposed mechanism may be an autoimmune
05/10/2015 20:51
Drug Information Group
2 of 3
http://dig.pharm.uic.edu/faq/myasthenia.aspx
response to the expression of interferon on motor endplates. The onset is from 6 to 9 months,
and it has been reported to last up to 7 months after discontinuation.
Corticosteroids, although a mainstay in the management of moderate to severe myasthenia
gravis, can also cause an exacerbation of muscle weakness.1-3 Patients are generally started
on high doses of prednisone (60 to 100 mg/day) until the disease is in remission, then the
dose is tapered to the lowest possible daily dose, and eventually switched to an every
other-day regimen. Approximately 20% to 50% of patients initiated on high dose prednisone
will have an exacerbation of their disease in the first days to weeks of therapy, which is then
followed by a period of remission.
Overdoses of cholinesterase inhibitors may also exacerbate myasthenia gravis.3 Excessive
doses can result in acetylcholine accumulation, which causes increased bronchial secretions
leading to difficulty swallowing or breathing. It has been suggested that weakness 1 hour after
administration of pyridostigmine could indicate overdose, while weakness 3 or more hours
following a dose could indicate a suboptimal response to therapy.
Aminoglycosides are cited in numerous case reports involving their concomitant use with
neuromuscular blockers.1,3,4 Postoperative respiratory depression was reported in nearly all
cases. Limb or facial weakness has also been reported. Aminoglycosides have also been
documented to exacerbate preexisting myasthenia gravis, and have lead to worsening
symptoms within 1 hour of administration.
Summarized below are various medications that have been associated with exacerbations of
myasthenia gravis.
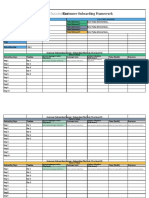
Table 1. Medications to be used with caution in myasthenia gravis.3-7
Drug
Onset (from initiation)
Resolution
Prednisone
1 to 2 weeks
1 to 20 days
Streptomycin
15 min to 1.5 hours
<24 hours
Iodinated contrast media
minutes
2 to 48 hours
Botulinum toxin
minutes
2 weeks
Procainamide
2 days to 2 weeks
12 hours to 10 days
Erythromycin
During infusion; 30 minutes after 2 to 3 days
dose
Ciprofloxacin
4 hours to 2 days
Several days
Ampicillin
12 hours to several days
48 hours
Quinidine
72 hours
48 hours
Lithium
10 days to 3 months
3 to 4 days
Timolol, acebutolol,
propranolol, oxprenolol,
practolol
24 hours to several days
24 hours to 8 weeks
Penicillamine
8 months
6 to 10 months
Chloroquine
1 week 3.5 years
5 days to 14 weeks
Phenytoin
4 to 6 years
2 to 3 months
Imipenem-cilastin
2 days
48 hours
Verapamil
4 days
2 weeks
Trimethaphan
2 to 17 hours
Procaine
7 minutes
Lidocaine
7 minutes
Aprotinin
during infusion
10 to 90 minutes
Levocarnitine
3 weeks
resolved after edrophonium
Several other drugs have been found to worsen myasthenia gravis including telithromycin,
magnesium, oxytocin, neuromuscular blockers, and anticholinergics.3-7 The Myasthenia
Gravis Foundation of America has a resource document for healthcare professionals that
discusses medications that may exacerbate myasthenia gravis (http://www.myasthenia.org
/hp_medicationsandmg.cfm). The document was last updated in January 2007.
In summary, many drugs have been implicated as a cause of myasthenia gravis or disease
exacerbation. Although the literature regarding implicated medications is limited, caution and
close monitoring when prescribing these agents is recommended, especially during an acute
exacerbation.
References
1. Barrons RW. Drug-induced neuromuscular blockade and myasthenia gravis.
Pharmacotherapy. 1997;17(6):1220-1232.
2. Vincent A, Palace J, Hilton-Jones D. Myasthenia gravis. Lancet. 2001;357:2122-2128.
3. Wittbrodt ET. Drugs and myasthenia gravis: an update. Arch Intern Med.
1997;157:399-408.
4. Karcic AA. Drugs that can worsen myasthenia gravis. Postgrad Med. 2000;108(2):25.
5. Pascuzzi R. Myasthenic crisis. Postgrad Med. 2000;107(4):211-222.
6. Yarom N, Barnea E, Nissan J, Gorsky M. Dental management of patients with
myasthenia gravis: A literature review. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 2005;100(2):158-163.
7. Kuczkowski KM. Labor analgesia for the parturient with neurological disease. Arch
Gynecol Obstet. 2006;247(3):41-46.
05/10/2015 20:51
Drug Information Group
3 of 3
http://dig.pharm.uic.edu/faq/myasthenia.aspx
College of Pharmacy | Student Affairs | Academic Affairs | Continuing Education | Office of the Dean | Information Technology
UIC Home | College Phonebook | Course Catalog | Site Map | Contact the College
Copyright 2007 The Board of Trustees of the University of Illinois | Web Privacy Notice
05/10/2015 20:51
You might also like
- Facebook Marketing Research PaperDocument8 pagesFacebook Marketing Research Paperefe8zf19100% (1)
- Digital Marketing ExcelDocument1 pageDigital Marketing ExcelRoHit ShaRmaNo ratings yet
- Business Sales PitchDocument2 pagesBusiness Sales PitchEmphorasoft gmailNo ratings yet
- 2.fabric Inspection Flow ChartDocument1 page2.fabric Inspection Flow ChartMd.Sadequl IslamNo ratings yet
- Drugs and Myasthenia GravisDocument2 pagesDrugs and Myasthenia Gravisskyclad_21100% (1)
- 4 Point SystemDocument5 pages4 Point SystemAdnan QayumNo ratings yet
- Social Media Audit TemplateDocument43 pagesSocial Media Audit Templatesocial.blincNo ratings yet
- Think Outside Square Business Goals Wide Presentation 1Document25 pagesThink Outside Square Business Goals Wide Presentation 1JeamaimaiNo ratings yet
- Emerald Digital MarketingDocument35 pagesEmerald Digital MarketingNguyen Hai LongNo ratings yet
- Streamlined Pipeline ManagementDocument2 pagesStreamlined Pipeline Managementsantsj78No ratings yet
- Winning at Sales in A Buyer-Empowered WorldDocument5 pagesWinning at Sales in A Buyer-Empowered WorldDeta DetadeNo ratings yet
- Step 1: Define Your Stages: Use This Checklist To Help You Get StartedDocument69 pagesStep 1: Define Your Stages: Use This Checklist To Help You Get StartedarifNo ratings yet
- ACELEX Capsule 2mg - Tissue Selective COX-2 Inhibitor CrystalGenomics Acelex NC Jan2016Document26 pagesACELEX Capsule 2mg - Tissue Selective COX-2 Inhibitor CrystalGenomics Acelex NC Jan2016Gihwan KimNo ratings yet
- Daily Sales ReportDocument2 pagesDaily Sales ReportAsprilla Wahyu Dona DonyNo ratings yet
- Online Adult QuestionnaireDocument5 pagesOnline Adult QuestionnaireDiyan UzunovNo ratings yet
- Pharmaceutical Medical Sales Representative in Houston TX Resume Jennifer MillerDocument1 pagePharmaceutical Medical Sales Representative in Houston TX Resume Jennifer MillerJenniferMiller1No ratings yet
- Michael Duntz: Graphic DesignerDocument1 pageMichael Duntz: Graphic DesignerMichael DuntzNo ratings yet
- Seo Copy For 919 MarketingDocument17 pagesSeo Copy For 919 Marketingapi-462894542No ratings yet
- Health Prediction Using Data Mining - Scope DocumentDocument4 pagesHealth Prediction Using Data Mining - Scope DocumentHaris AhmedNo ratings yet
- Sample Policy: Personal Appearance of EmployeesDocument11 pagesSample Policy: Personal Appearance of EmployeesnanajonNo ratings yet
- Karan KapurDocument5 pagesKaran KapurKaran Kapur100% (1)
- F-05 814 Pricing StrategyDocument24 pagesF-05 814 Pricing Strategydinosaur2512No ratings yet
- Customer Onboarding FrameworkDocument3 pagesCustomer Onboarding FrameworkOaga GutierrezNo ratings yet
- VP Director Global Sales in San Diego CA Resume David SilvaDocument2 pagesVP Director Global Sales in San Diego CA Resume David SilvaDavidSilva2No ratings yet
- Exabone PasteDocument4 pagesExabone PasteExabone GmbHNo ratings yet
- Apex Institute of Engineering Department of Ait - Cse: B.E. CSE With Specialization in BDADocument13 pagesApex Institute of Engineering Department of Ait - Cse: B.E. CSE With Specialization in BDARitika MakhariaNo ratings yet
- LinkedIn Content Calendar Excel TemplateDocument31 pagesLinkedIn Content Calendar Excel TemplateSandeep SinghNo ratings yet
- Quotation For: Item Image Description Qty Unite Price AmountDocument22 pagesQuotation For: Item Image Description Qty Unite Price AmountHong VineseNo ratings yet
- Account Based Marketing (Abm) : Logo Name Description Contact Details Accuracy PricingDocument3 pagesAccount Based Marketing (Abm) : Logo Name Description Contact Details Accuracy PricingKUSHAGRA ARORA100% (1)
- Interpret Market Trends and Developments TASk 1Document7 pagesInterpret Market Trends and Developments TASk 1Raí SilveiraNo ratings yet
- Is MP Canada List of Dangerous AbbreviationsDocument1 pageIs MP Canada List of Dangerous AbbreviationsgenbeeNo ratings yet
- Jkbank Phone NoDocument6 pagesJkbank Phone NoVarun KundalNo ratings yet
- Chemlinks Marketing Strategy Edited 2Document14 pagesChemlinks Marketing Strategy Edited 2Insights International100% (1)
- Internet Service Provider Survey 2013Document18 pagesInternet Service Provider Survey 2013Julie StarrNo ratings yet
- Product Demo TemplateDocument9 pagesProduct Demo Templateconnectadasgupta100% (1)
- Medical Sales RepresentativeDocument3 pagesMedical Sales Representativeapi-77860217No ratings yet
- 21 Neurotech Startups To WatchDocument8 pages21 Neurotech Startups To WatchYuan RyanNo ratings yet
- 2 CA - Health Profile - 2014-12-19 PDFDocument9 pages2 CA - Health Profile - 2014-12-19 PDFLiamNo ratings yet
- Health Monitoring Using Mobile Phones: Course:-Mobile Networking Instructor: - Dr. Helmy AhmedDocument40 pagesHealth Monitoring Using Mobile Phones: Course:-Mobile Networking Instructor: - Dr. Helmy AhmedsmritiNo ratings yet
- Duc CV - Marketing ManagerDocument27 pagesDuc CV - Marketing ManagerThang Nguyen100% (1)
- Debt Recovery Agency in IndiaDocument22 pagesDebt Recovery Agency in Indiarecreatecredit CollectionsNo ratings yet
- A System-Wide, Collaborative Purchasing Process: Strategic SourcingDocument8 pagesA System-Wide, Collaborative Purchasing Process: Strategic SourcingPriya SrivastavaNo ratings yet
- B2B - Partner - Brochure PorteaDocument12 pagesB2B - Partner - Brochure PorteaBhagyesh Masurekar100% (1)
- AmcareFamilyPractice New Patient Forms RevisedDocument9 pagesAmcareFamilyPractice New Patient Forms RevisedAmcare Family PracticeNo ratings yet
- Buy Australian MadeDocument60 pagesBuy Australian Madejtact_jtact7649100% (1)
- 10 Usiness-To - Usiness Mistakes: About The AuthorDocument40 pages10 Usiness-To - Usiness Mistakes: About The AuthorkarthickNo ratings yet
- I. SEM (Search Engine Marketing) : What Are The Benefits of Sem?Document6 pagesI. SEM (Search Engine Marketing) : What Are The Benefits of Sem?Aysha ZahidNo ratings yet
- Online Shopping SystemDocument94 pagesOnline Shopping SystemArika Afrin BoshraNo ratings yet
- The Benefits of Social Selling: Design MGZ 6 - 1Document10 pagesThe Benefits of Social Selling: Design MGZ 6 - 1marcaicedoNo ratings yet
- Business Startup Costs TemplateDocument10 pagesBusiness Startup Costs TemplateRandoNo ratings yet
- Surgical & Medical Instruments Industry of Pakistan: An OverviewDocument25 pagesSurgical & Medical Instruments Industry of Pakistan: An OverviewFaisal MasudNo ratings yet
- MODx Cheat SheetDocument47 pagesMODx Cheat SheetYahya NursalimNo ratings yet
- Marketing Plan: Prepared & Submitted By: Boys & Girls Clubs of Greater Any Town Area Marketing CommitteeDocument18 pagesMarketing Plan: Prepared & Submitted By: Boys & Girls Clubs of Greater Any Town Area Marketing CommitteeDaniel Hutapea100% (1)
- PhysiotherapyDocument36 pagesPhysiotherapyOng Siaw YenNo ratings yet
- Usa SetupDocument174 pagesUsa SetupTounsi HurrNo ratings yet
- R01 Revitalife Drip Protocol - UPDATED 9-19-2018Document10 pagesR01 Revitalife Drip Protocol - UPDATED 9-19-2018Eking InNo ratings yet
- Introduction To Mass MailingDocument11 pagesIntroduction To Mass MailingETL LABSNo ratings yet
- Cost Analysis For VR Mock Code Implementation Final Draft Jennifer PDocument25 pagesCost Analysis For VR Mock Code Implementation Final Draft Jennifer Papi-527185509No ratings yet
- Myasthenia GravisDocument4 pagesMyasthenia GravisArlyn MillanesNo ratings yet
- ARDO Amenic - UserInstructions - E - 05-2006Document38 pagesARDO Amenic - UserInstructions - E - 05-2006Moas GabrounNo ratings yet
- CVDocument8 pagesCVJuan Rafael SilvaNo ratings yet
- Cinema Narrative Therapy: Utilizing Family Films To Externalize Children's Problems' Brie Turns and Porter MaceyDocument17 pagesCinema Narrative Therapy: Utilizing Family Films To Externalize Children's Problems' Brie Turns and Porter MaceyRupai SarkarNo ratings yet
- Dance Therapy TortureDocument15 pagesDance Therapy TortureeclatantNo ratings yet
- Sim Scenario 4Document31 pagesSim Scenario 4lilchibaby3161No ratings yet
- 1.D/D of Intraconal Mass 2.D/D of Leucocoria 3.U/S & CT Findings of RB 4.how Will You Manage That CaseDocument15 pages1.D/D of Intraconal Mass 2.D/D of Leucocoria 3.U/S & CT Findings of RB 4.how Will You Manage That CaseMuhammad SharjeelNo ratings yet
- Engaging With Research: Linking Evidence With PracticeDocument2 pagesEngaging With Research: Linking Evidence With PracticeTomáš KrajíčekNo ratings yet
- Parking Placards Reg 3164Document2 pagesParking Placards Reg 3164David BatesNo ratings yet
- Kci Vac Therapy Vtiaf UpdatedDocument2 pagesKci Vac Therapy Vtiaf UpdatedHi BeyoNo ratings yet
- Perspectives of Education in PakistanDocument26 pagesPerspectives of Education in Pakistanmehran school35% (17)
- MFD Part 2 Exam Held in JUST, Jordan On 12-2013Document2 pagesMFD Part 2 Exam Held in JUST, Jordan On 12-2013sohaib197No ratings yet
- PDFDocument13 pagesPDFUlfah Uph UphNo ratings yet
- Diass Course OutlineDocument47 pagesDiass Course OutlineLouise Lean llanitoNo ratings yet
- Vdocuments - MX Standards of Nursing Services AnsapDocument30 pagesVdocuments - MX Standards of Nursing Services AnsapKarl RobleNo ratings yet
- Biopharmaceutics Supplemental NotesDocument19 pagesBiopharmaceutics Supplemental NotesChristine Joy De Ocampo0% (1)
- Alternative Fibromyalgia Pain Management SuggestionsDocument4 pagesAlternative Fibromyalgia Pain Management SuggestionsCinda CrawfordNo ratings yet
- The King's SpeechDocument3 pagesThe King's SpeechAnap LigthNo ratings yet
- Dr. David Rath Medical BoardDocument58 pagesDr. David Rath Medical BoardWews WebStaffNo ratings yet
- NP 5Document14 pagesNP 5Yaj Cruzada100% (1)
- ParenteralDocument10 pagesParenteralDennis SantosNo ratings yet
- Bowlby Attachment TheoryDocument10 pagesBowlby Attachment Theoryfatimapanda100% (1)
- Stretching TherapyDocument95 pagesStretching TherapySpineCare Physiotherapy100% (2)
- Vasculitis Syndrome (VS) : Dr. Julius Roma, SP ADocument45 pagesVasculitis Syndrome (VS) : Dr. Julius Roma, SP ADavid ChristianNo ratings yet
- A Review On LozengesDocument9 pagesA Review On LozengesShakrie AbdullahNo ratings yet
- Klapp MethodDocument7 pagesKlapp MethodRJLeddaNo ratings yet
- I. Approach To Clinical Interviewing and DiagnosisDocument6 pagesI. Approach To Clinical Interviewing and DiagnosisRoci ArceNo ratings yet
- Breathing TherapyDocument8 pagesBreathing Therapyzarrar100% (1)
- Parallel Process in Psychotherapy Supervision PDFDocument5 pagesParallel Process in Psychotherapy Supervision PDFМайя МладеноваNo ratings yet
- Sprains and StrainsDocument15 pagesSprains and StrainsPutri ClaraNo ratings yet
- Direct Decision TherapyDocument9 pagesDirect Decision TherapyzarrarNo ratings yet