Professional Documents
Culture Documents
3.ISCA IRJMedS 2014 046
Uploaded by
Warisatul Imam LubisOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
3.ISCA IRJMedS 2014 046
Uploaded by
Warisatul Imam LubisCopyright:
Available Formats
International Research Journal of Medical Sciences ____________________________________ ISSN 2320 7353
Vol. 2(8), 9-12, August (2014)
Int. Res. J. Medical Sci.
Prevalence of Dermatophytoses in Rural Population of Garhwal Himalayan
Region, Uttarakhand, India
Anup Kainthola, Puneet Gaur, Alkesh Dobhal and Shailendra Sundriyal
Department of Botany and Microbiology, HNB Garhwal University (A Central University), Srinagar, Uttarakhand-246174, INDIA
Available online at: www.isca.in, www.isca.me
Received 23rd July 2014, revised 6th August 2014, accepted 26th August 2014
Abstract
To assess the prevalence and factors contributing in developing dermatophytoses in rural population of Garhwal Himalayan
Region, a cross sectional study of 12 villages was done family to family from 1-Jan-2013 to 28-Aug-2013 and a total of 106
samples were taken into study from subjects who didnt attend OPD and were not receiving any anti fungal treatment.
Samples were tested by potassium hydroxide [KOH] examination. Macroscopic and Microscopic examination of direct
sample and corresponding culture was done to identify the etiologic agent. All of 106 samples were found KOH positive
whereas 74 [69.81 %] samples were culture positive. Amongst culture positive samples, clinical type Tinea capitis was found
predominant with 43.24% prevalence followed by Tinea corporis and Tinea pedis 28.38% and 18.92% respectively. Tinea
cruris was found least with 9.46 % occurrence. Males [64.86%] were more prone to dermatophytoses than females
[35.14%]. A pretested questionnaire, to assess prevalence was designed and data was collected and analyzed.
Keywords: Close contacts with livestock, overcrowding in family and low personal hygiene, bare foot farming were primary
reasons for the development of dermatophytoses. Improving awareness of peoples about the dermatophytoses can minimize
the prevalence of this disease.
Introduction
Methodology
Dermatophytoses, a major public health problem throughout the
world is caused by a group of microorganisms called
Dermatophytes, lesions of which are characterized by circular
disposition, desquamation, alopecia and erythema of the edges1.
There are three genera of dermatophyte, Trichophyton,
Microsporum and Epidermophyton2.
Physiography of the area: The present study was conducted in
the 12 Villages of Joshimath district of Uttarakhand, Garhwal
Himalayan Region namely; Saundari, Badagaon, Dhaak,
Tugaasi, Karchhi, Raigari, Karchhaun, Bhangyul, Ringgi,
Subhhain, Reni, and Merugh, that lies between Latitude
30340 N and Longitude 79340 E and at 3124 msl height.
As the transmittance of the dermatophytoses merely require
contact and low personal hygiene, its occurrence in a
community may become persistent. Keeping in view the fact
that dermatophytoses and other fungal infections are readily
caught by immunocompromised individuals which are
increasing critically at sharp rate3. Frequent incidences of
dermatophytoses have become a serious problem to counter and
manage. Climatic and ambient environmental conditions do
favors the growth of certain dermatophytes4. India is a large
subcontinent with remarkably varied topography. Its climate is
conductive to the acquisition and persistence of dermatophytic
infection.
Collection of Samples: After receiving an informed consent
from each individual included in this study, a total of 106
samples were collected and investigated from those individuals
who were found clinically suspected for dermatophytoses and
were not receiving any antifungal treatment from beginning of
the infection and subjected to mycological examination. To
remove the dirt or other ointments if any, after wiping the
infected areas or lesions with 70% alcohol, Samples from scalp,
nails, foot webs and skin scrapings were collected in pre
sterilized black paper sachet [13x12cm]. Pieces of discolored,
broken nails and scrapings were taken from the advancing
borders and edges of infection with the help of blunt sterile
scalpels were taken.
The present study aims to report the prevalence and distribution
of 4 predominant clinical types of Dermatophytoses and to find
out the parametres contributing in its prevalence in rural
population of Garhwal Himalyan region that dont have access
to the health care facilities due to adverse geographical
locations.
International Science Congress Association
Isolation and culturing of Dermatophytes: Prior to 10% KOH
examination, Samples were made free of any small hairs
aseptically using sterile forcep. All 106 samples collected were
subjected to direct microscopic observation. After confirmation
of fungal elements, samples were streaked on to modified
Sabouraud Dextrose Agar [SDA] plates and slants enriched with
cyclohexamide [0.5 mg/ml], chloramphenicol [0.05 mg/ml] [Hi9
International Research Journal of Medical Sciences ________________________________________________ ISSN 2320 7353
Vol. 2(7), 9-12, August (2014)
Int. Res. J. Medical Sci.
media] and incubated for 5 weeks5. Cultures without any
apparent fungal growth after 5 weeks were treated as Culture
negative and discarded.
All mycological Identifications were done by macroscopic and
microscopic observation of culture isolates by examining the
surface morphology, texture, and pigmentation on the reverse
side of colony6. Lactophenol cotton Blue staining was done for
each culture positive sample to observe mycelial type, conidial
arrangement [macro and micro conidia] to differentiate between
species and genera.
Survey methodology and statistical analysis: In order to
assess the prevalence of dermatophytoses on the basis of age,
sex, education and profession of rural population its
management, a pretested and structured questionnaire was
designed to asses the living standards and other. All individuals
participated in the study were informed and consent was taken
verbally and in written. A value of P < 0.05 was taken as
significant.
Results and Discussion
Amongst 106 samples taken, only 74 (69.81%) were culture
positive and subjected for further investigation. Microscopical
and macroscopical observation suggested the high prevalence of
clinical type Tinea capitis with 43.24% (table 1) followed by
Tinea corporis and Tinea pedis 28.38% and 18.92%
respectively. Tinea cruris was found least with 9.46%
occurrence. We observed that close contacts, over crowding in
family and low personal hygiene were primary regions for the
development of the dermatophytoses.
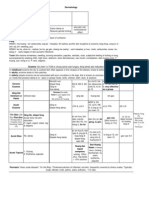
Table-1
Etiology of Dermatophytoses. (P<0.05)
Isolates
Males
Females
Etiological
Agent
No.
%
No.
%
No.
%
Trichophyton
32
43.24 23 71.87 09 28.15
rubrum
Trichophyton
21
28.38 12 57.14 09 42.85
mentagrophytes
Epidermophyton
14
18.92 08 57.14 06 42.85
floccosum
Trichophyton
07
9.46
05 71.42 02 28.57
Verrucosum
Total
74
100
48
64.8
26
35.2
People with habit of bare feet farming, poor hygienic status and
having close contacts with livestock were found to comprise the
major infected group in all (table 2).
Susceptibility by age and gender: Of the 74 culture positive
samples, the dermatophytoses infection was found prominent in
the age group of 20-40 [31.08%] and 40< [28.37%] years [table
2a]. Males were found to be more susceptible to the
dermatophytoses as studied by earlier investigators7-9. Taking
International Science Congress Association
occasional bath and wearing of tight cloths in winter season that
lasts till march in Himalayan region is a major reason for having
such infections. Education however was found as negligible
factor as all educational groups viz. primary and secondary were
infected with nearly equal percent of occurrence.
S.
No.
1
2
3
4
Total
Table-2
Prevalence of dermatophytoses as per Age
Age
No. of
Males
Females
patient(s)
(%)
(%)
1-10
13
8
61.53
5
38.46
10-20
17
11
64.70
6
35.29
20-40
23
15
65.21
8
34.78
>40
21
14
66.66
7
33.33
74
48
64.86
26
35.13
Prevalence of dermatophytoses as per Occupation
Occupation
Farmer
Laborers
House Makers
Students
Total
No. of
patient
(s)
11
9
13
41
74
Males
(%)
Females
(%)
11
9
24
44
100
100
58.53
59.45
13
17
30
100
41.46
40.54
Prevalence of dermatophytoses as per Educational
Qualification
Educational
No. of
Males
Females
Qualification
Patient(s)
(%)
(%)
<5
21
9
42.85
12
57.14
5-10
29
16
55.17
13
44.82
>10
24
15
62.5
9
37.5
Total
74
40
54.05
34
45.94
Discussion: There are reports of emergence of high occurrence
of dermatophytoses from different parts of the world7. Though
on receiving prompt treatment most of the infections are
checked but dwellers of geographically distinct areas those who
are not availing primary facilities like primary health care
centers are always at high risk of persistent infection.
Dermatophytoses if not treated, may sometime go latent and
transmits to the healthy population by all possible ways of
transmission i.e. through sharing of things and close contacts
which in turn leads to the prevalence in symptomatic
carriers10-11. Interior rural population of high altitude regions of
Garhwal Himalayas, thus constitute a privileged site for
epidemiological study of dermatophytoses along with
ascertaining the factors contributing in emergence and
developing of the infection. Occurrence of dermatophytoses
with respect to particular gender has been studied earlier with
different views, which does not come to a significant conclusion
that either of gender is more susceptible to the infection. Some
studies have shown that males are at the higher risk of
acquisition of infection12-15. However, others have reported
females of being more prone4,10,16. Of the 106 samples taken
10
International Research Journal of Medical Sciences ________________________________________________ ISSN 2320 7353
Vol. 2(7), 9-12, August (2014)
Int. Res. J. Medical Sci.
69.81% i.e. 74 were culture positive. High prevalence of
Trichophyton rubrum and Trichophyton mentagrophytes
followed by Epidermophyton floccosum and Trichophyton
verrucosum was found with males [64.86%] being more prone
to the dermatophytoses. Our study reports that species of
Trichophyton genus was responsible of majority of the infection
[71.31%] which is also supported by reports of other
investigators17-19. In this study our findings provide further
evidence for the existence of the strong correlation between
occurrence of dermatophytoses and living standards. Our results
are in good agreement with the earlier studies8,9,20. We observed
that the lack of knowledge about dermatophytoses, carelessness
towards treatment [as it was a general notion that
dermatophytoses doesnt cause serious problems], remoteness
from health care units and low personal hygiene were the
apparent factors for the continuous existence of
dermatophytoses in the community. A value for P to be greater
than 0.05 makes the study statistically significant.
Figure-1
Clinical photographs showing grey scaling with roughness in
hands by T. rubrum
Figure-4
Advancing border of infection of ringworm pattern in Tinea
corporis
Conclusion
The present study indicates the widespread occurrence and
dissemination of dermatophytoses in Garhwal Himalayan region
and suggests for the establishment of healthcare units and
upgrading the beliefs of rural population about dermatophytoses
infection and its consequences. Our study supports the belief
that age group 20-30 years is considered as highly active group
and there are greater chances of interaction between them
leading to dissemination of fungal infections (dermatophytoses)
more rapidly in the community. It was well observed during the
study that level of knowledge about dermatophytoses or other
fungal infections was below average in the local dwellers and
hence further worsened the situation in this part of India. Hence,
an abrupt intervention is needed in the form of upgrading their
knowledge, precautions and need for urgency of treatment.
Acknowledgement
Authors acknowledge the support of rural population of
Garhwal Himalayan region in making the study possible.
References
1.
Lacaz C.S., Porto E. and Martins J.E.C., Micologia medicafungos, actinomycetos e algas de interesse medico, Sarvier
itda, Sao Paulo, (695) (1991)
2.
Pakshir K. and Hashmemi J., Prevalence and etiological
agents of cutaneous fungal infections in milad Hospital of
Teharn, Iran. Indian J.Dermatol. 51, 262264 (2006)
3.
Burkhart C.N., Chang H. and Gottwald L., Tinea corporis
in human immunodeficiency virus positive patients : case
report and assessment of oral therapy, Int. J. Dermatol,
42(10), 839843 (2003)
4.
Anosike J.C., Keke I.R., Uwaezuoke J.C., Anozie J.C.,
Obiukwu C.E. and Nwoke B.E., Prevalence and distribution
of ringworm infection in primary school children in parts of
eastern Nigeria, J. Appl. Sci. Environ. Manage, 9, 2132
(2005)
5.
Irene W. and Richard C., Summerbell, The Dermatophytes.
Clin. Microbiol. Rev., 8, 240249 (1995)
6.
Rippon J.W., The pathogenic fungi and pathogenic
Figure-2
papulosquamous appearance and fissuring in Tinea pedis
Figure-3
Photograph showing broken and weakened hairs in Tinea
capitis
International Science Congress Association
11
International Research Journal of Medical Sciences ________________________________________________ ISSN 2320 7353
Vol. 2(7), 9-12, August (2014)
Int. Res. J. Medical Sci.
actinomycetes, Medical Mycology, WB Saunders,
Philadelphia Sabauraud R. (3rd ed. 1988) (1988)
7.
Patwadhan N. and Dave R., Dermatophytoses in and around
Aurangabad, Indian j. Pathol. Microbiol, 42, 455-462
(1999)
8.
Jain N., Sharma M. and Saxena V.N., Clinico mycological
profile of deramtophytosis in Jaipur, Rajasthan, Indian J.
Dermatol. Venerol. Leprol., 74, 274275 (2008)
9.
Sen S.S. and Rasul E.S., Prevalence of dermatophyte
infection in district Rajkot, Indian J. Med. Microbiol., 24,
7778 (2005)
10. Omar A.A., Ringworm of the scalp in primary school
children in Alexandria: Infection and carriage, East
mediterr. Health J., 6, 961967 (2000)
11. IIkit M., Demhindi H., Yetgin M., Ates a., Turac-Bicer A.
and Yula E. asymptomatic Dermatophyte scalp carriage in
school children in Adana, Turkey. Mycoses. 50, 130 134
(2007)
12. Enweani IB, Ozan CC, Azbonlahor E.E., Ndip R.N.,
Dermato phytoses in school chidren in Ekpoma, Nigeria,
Mycoses, 39, 303-305 (1996)
13. Nweze E.I., Etiology of Dermatophytoses against children
in northeastern Nigeria, Med Mycol, 39, 181-184 (2001)
14. Ajao Ao, Akintunde C., Studies on the prevalence of Tinea
Capitis infection in IIe-Ife, Nigeria, Mycopathologia, 89L,
International Science Congress Association
43-48 (1985)
15. Ogunbiyi Ao and Owoaje E, Ndahi A., Prevalence of skin
disorders in school children in Ibudan, Nigeria, Pediatr
dermatol, 22- 26 (2005)
16. East Innis A., Rainford L., Dunwell P., Barett-Robinson D.,
Nicholson A.M., The changing pattern of Tinea Capitis in
Jamaica, West Indian Med J., 55, 85-88 (2006)
17. Enweani I.B., Graeser Y. and Agbonlahor D., Association
of ABO Blood group and Dermatophytosis in Nigeria, In:de
Hoog S, Ahmed A, Meis J, Vismer H, editors, Proceedings
of the conference, Medical Mycology, The African
Perspective January 25 (2005). Harstenbosch, South Africa.
(Accessed on 2007 mar 26.) (2007)
18. Ezeronye O.U., Distribution of Dermatophytosis in cross
river upstream bank of Eastern Nigeria, In:de Hoog S,
Ahmed A, Meis J, Vismer H, editors. Proceedings of the
conference, Medical Mycology, The African Perspective
2005; January 25. Harstenbosch, South Africa. (Accessed
on 2007 mar 26.) (2005)
19. Sigurgeirsson B., Kristinsson K.G., Jonasson P.S.,
Onychomycosis in Icelandic children, J Eur Acad Dermatol
Venerol. 20, 796-799, (2006)
20. Ranganathan S., Menon T. and Sentamil G.S., Efect of
socio-economic
status
on
the
prevalence
of
dermatophytoses in madras, Indian J. Dermatol. Venerol.
Leprol. 61, 16-18 (1995)
12
You might also like
- Clinicomycological Profile of Superficial Fungal Infections in North IndiaDocument8 pagesClinicomycological Profile of Superficial Fungal Infections in North IndiaasfwegereNo ratings yet
- Iran FungusDocument7 pagesIran FungusHaruka KanataNo ratings yet
- Cox N 2010Document6 pagesCox N 2010Fauzul adzimNo ratings yet
- 35429-Article Text-126139-2-10-20180206Document5 pages35429-Article Text-126139-2-10-20180206Robertus RonnyNo ratings yet
- A Study of Dermatomycoses: Manuscript InfoDocument7 pagesA Study of Dermatomycoses: Manuscript InfoCorry ZalukhuNo ratings yet
- Jurnal TC KohDocument4 pagesJurnal TC KohariefNo ratings yet
- Original Article Paederus Dermatitis in South IndiaDocument6 pagesOriginal Article Paederus Dermatitis in South Indiasoumalya481No ratings yet
- Corporis Was The Most Common Clinical Presentation and Trichopyton Rubrum Was The Most CommonDocument4 pagesCorporis Was The Most Common Clinical Presentation and Trichopyton Rubrum Was The Most CommonaiiaibrahimNo ratings yet
- Admin, Artikel 1Document4 pagesAdmin, Artikel 1Tirza SosantaNo ratings yet
- Prevalence of Dermatophytic Infection in Ahmedabad: Rugved Parmar (116) and Parth Parmar (115) 3Document8 pagesPrevalence of Dermatophytic Infection in Ahmedabad: Rugved Parmar (116) and Parth Parmar (115) 3RugvedNo ratings yet
- Dermatomycological Profile of Patients in A Tertiary Care Hospital of Western MaharashtraDocument2 pagesDermatomycological Profile of Patients in A Tertiary Care Hospital of Western MaharashtraApple IdeaNo ratings yet
- A Clinical and Epidemiological Study of Pityriasis VersicolorDocument5 pagesA Clinical and Epidemiological Study of Pityriasis VersicolornanaNo ratings yet
- Evaluation of Culture Media For The Rapid Isolation of DermatophytesDocument4 pagesEvaluation of Culture Media For The Rapid Isolation of DermatophytesIOSRjournalNo ratings yet
- Emergence of Trichophyton mentagrophytes as a common cause of Tinea CorporisDocument5 pagesEmergence of Trichophyton mentagrophytes as a common cause of Tinea CorporisjmuhilanNo ratings yet
- Incidence and Prevalence of Dermatophytosis in and Around Chennai, Tamilnadu, IndiaDocument6 pagesIncidence and Prevalence of Dermatophytosis in and Around Chennai, Tamilnadu, IndiaYanna RizkiaNo ratings yet
- Geriatric Skin DisordersDocument3 pagesGeriatric Skin DisordersكنNo ratings yet
- Clinical and Microbiological Study of Tinea Unguium in A Tertiary Care CentreDocument7 pagesClinical and Microbiological Study of Tinea Unguium in A Tertiary Care CentreRebeka SinagaNo ratings yet
- Prevalence of Dermatophytic Infection in and Around AhmedabadDocument6 pagesPrevalence of Dermatophytic Infection in and Around AhmedabadRugvedNo ratings yet
- Isolation and Identification of Dermatophytes Causing DermatophytosisDocument15 pagesIsolation and Identification of Dermatophytes Causing Dermatophytosisabznaim420No ratings yet
- Filariasis ReportDocument50 pagesFilariasis ReportMahendra Maharjan100% (2)
- Detection of Dermatophytes in Clinically Normal Extra-Crural Sites in Patients With Tinea CrurisDocument15 pagesDetection of Dermatophytes in Clinically Normal Extra-Crural Sites in Patients With Tinea Crurisracut_khansatraNo ratings yet
- Research Article: Factors Associated With Larval Control Practices in A Dengue Outbreak Prone AreaDocument7 pagesResearch Article: Factors Associated With Larval Control Practices in A Dengue Outbreak Prone AreaJethro BudimanNo ratings yet
- Superficial Fungal Infections: Auroba K. Abbas, PH.D., Zahraa A. Mohammed, M.SC., Imad S. Mahmoud, PH.DDocument3 pagesSuperficial Fungal Infections: Auroba K. Abbas, PH.D., Zahraa A. Mohammed, M.SC., Imad S. Mahmoud, PH.DAnonymous zNUqQaNo ratings yet
- New Horizons in Pharmaceutical & Biomedical SciencesDocument360 pagesNew Horizons in Pharmaceutical & Biomedical SciencesPrema PérezNo ratings yet
- Skin Diseases in Pediatric Patients Attending A Tertiary Dermatology Hospital in Northern Tanzania: A Cross-Sectional StudyDocument4 pagesSkin Diseases in Pediatric Patients Attending A Tertiary Dermatology Hospital in Northern Tanzania: A Cross-Sectional StudyRizna ArianiNo ratings yet
- Profile of tinea corporis and tinea cruris casesDocument6 pagesProfile of tinea corporis and tinea cruris casesMarwiyahNo ratings yet
- MamekDocument5 pagesMamekkamalNo ratings yet
- Patterns of Skin Disease and Prescribing Trends in Rural India Juno J. Joel, Neethu Jose, Shastry C.SDocument6 pagesPatterns of Skin Disease and Prescribing Trends in Rural India Juno J. Joel, Neethu Jose, Shastry C.SHabibur RahmanNo ratings yet
- Lumpy Skin Disease: A Field Manual for VeterinariansFrom EverandLumpy Skin Disease: A Field Manual for VeterinariansNo ratings yet
- Jof 03 00017Document10 pagesJof 03 00017Asterlita RyaneNo ratings yet
- Profile of Tinea Corporis and Tinea Cruris in Dermatovenereology Clinic of Tertiery Hospital: A Retrospective StudyDocument6 pagesProfile of Tinea Corporis and Tinea Cruris in Dermatovenereology Clinic of Tertiery Hospital: A Retrospective StudyRose ParkNo ratings yet
- 273 879 1 PBDocument4 pages273 879 1 PBChasanatul MuwachidahNo ratings yet
- EJMCM - Volume 7 - Issue 11 - Pages 9184-9190Document7 pagesEJMCM - Volume 7 - Issue 11 - Pages 9184-9190Akshay BeradNo ratings yet
- Review Article: Profile of Corneal Ulcer in A Tertiary Eye Care CentreDocument6 pagesReview Article: Profile of Corneal Ulcer in A Tertiary Eye Care CentreNadhila ByantNo ratings yet
- Skin Diseases Among Elderly Attending Out-Patient Dermatologic Clinic, Siriraj HospitalDocument6 pagesSkin Diseases Among Elderly Attending Out-Patient Dermatologic Clinic, Siriraj HospitalenrionickolasNo ratings yet
- Causative Fungi and Treatment Outcome of Dematiaceous Fungal Keratitis in North India. 2019Document7 pagesCausative Fungi and Treatment Outcome of Dematiaceous Fungal Keratitis in North India. 2019Anonymous argZ1ZNo ratings yet
- Skin Diseases of Cattle in the Tropics: A Guide to Diagnosis and TreatmentFrom EverandSkin Diseases of Cattle in the Tropics: A Guide to Diagnosis and TreatmentNo ratings yet
- A Study of Clinical Types of Contact Allergic Dermatitis of Hands and Its Association With AllergensDocument8 pagesA Study of Clinical Types of Contact Allergic Dermatitis of Hands and Its Association With AllergensRika FitriaNo ratings yet
- Prevalence of Oral Submucous Fibrosis The High Natural Radiation Belt of Kerala, South IndiaDocument7 pagesPrevalence of Oral Submucous Fibrosis The High Natural Radiation Belt of Kerala, South IndiaashajangamNo ratings yet
- Clinico-Epidemiological Study of Dermatophytosis in Teaching Hospital of North KarnatakaDocument4 pagesClinico-Epidemiological Study of Dermatophytosis in Teaching Hospital of North KarnatakaAldo NovaNo ratings yet
- Antifungal TestDocument8 pagesAntifungal Testabznaim420No ratings yet
- Pattern of Pediatric Dermatoses in A Tertiary Care Hospital of Western NepalDocument5 pagesPattern of Pediatric Dermatoses in A Tertiary Care Hospital of Western NepalTher RayNo ratings yet
- Rahul Kamble Pediatrics Article 1Document9 pagesRahul Kamble Pediatrics Article 1Rahul KambleNo ratings yet
- Different Approaches To Atopic Dermatitis by Allergists, Dermatologists, and PediatriciansDocument9 pagesDifferent Approaches To Atopic Dermatitis by Allergists, Dermatologists, and PediatriciansyelsiNo ratings yet
- Psoriasis FixDocument4 pagesPsoriasis FixDicky SaputraNo ratings yet
- Makalah Keperawatan AnakDocument4 pagesMakalah Keperawatan AnakAnonymous DOud34bNo ratings yet
- Sciences of Pharmacy Fungal Diseases With Khokon 2024Document14 pagesSciences of Pharmacy Fungal Diseases With Khokon 2024pro-vcNo ratings yet
- J Pak Assoc Dermatol 2013 23 3 295 299Document5 pagesJ Pak Assoc Dermatol 2013 23 3 295 299Latifah Amalia ZatiNo ratings yet
- Fungal - HIVDocument4 pagesFungal - HIVFrankly VRHNo ratings yet
- Duduyemi 2019Document7 pagesDuduyemi 2019kikiNo ratings yet
- Epidemiology of dermatophytoses in TunisiaDocument6 pagesEpidemiology of dermatophytoses in TunisiasantiNo ratings yet
- Investigation of Intertriginous Infections and Their Clinical PresentationsDocument7 pagesInvestigation of Intertriginous Infections and Their Clinical PresentationsKiki FatmawatyNo ratings yet
- Resume Thai Report JournalDocument2 pagesResume Thai Report JournalsigitNo ratings yet
- Research Article: Cutaneous Mycoses Among Rice Farmers in Anambra State, NigeriaDocument6 pagesResearch Article: Cutaneous Mycoses Among Rice Farmers in Anambra State, NigeriakamalNo ratings yet
- Fungal Spectrum in Otomycosis Patients: OriginalarticleDocument4 pagesFungal Spectrum in Otomycosis Patients: OriginalarticleWilga HabibburahmanNo ratings yet
- Community Knowledge, Practice and Prevalence of Brucellosis in Livestock Owners in Northern Red Sea Region, EritreaDocument20 pagesCommunity Knowledge, Practice and Prevalence of Brucellosis in Livestock Owners in Northern Red Sea Region, EritreaWeal AlhaidaryNo ratings yet
- Tinea KorporisDocument3 pagesTinea Korporishaprisia winaNo ratings yet
- Identification of Hookworm Species in Stool By Harada Mori Culture MethodDocument2 pagesIdentification of Hookworm Species in Stool By Harada Mori Culture MethodMeenachi ChidambaramNo ratings yet
- Bindari Et Al 2012 Prevalence Mange Katmandu PDFDocument5 pagesBindari Et Al 2012 Prevalence Mange Katmandu PDFjulian satriaNo ratings yet
- Clinico-Microbiological Study of Pyodermas: Research Article Janardhan. B, Prasad - GK, Nandeshwar - AJ and Vidyavathi.NDocument5 pagesClinico-Microbiological Study of Pyodermas: Research Article Janardhan. B, Prasad - GK, Nandeshwar - AJ and Vidyavathi.NradiNo ratings yet
- IcdDocument180 pagesIcdFitri MoraNo ratings yet
- Chinese Medicine InfoDocument28 pagesChinese Medicine Infopeter911xNo ratings yet
- Rapid Real-Time PCR for Diagnosing Tinea InfectionsDocument7 pagesRapid Real-Time PCR for Diagnosing Tinea InfectionsSiti Bellia Arafah XndNo ratings yet
- Fungal ClassificationDocument109 pagesFungal ClassificationMirza Shaharyar BaigNo ratings yet
- Mycology Viva With AnswerDocument8 pagesMycology Viva With AnswerKumar KPNo ratings yet
- Eritrasma 2012Document17 pagesEritrasma 2012Ammar HasyimNo ratings yet
- Week 1 MCQ VMPFDocument25 pagesWeek 1 MCQ VMPFZainab_Wajih_2544100% (1)
- Tinea CapitisDocument9 pagesTinea CapitisadityakafiberkahsmgNo ratings yet
- DaseqwDocument57 pagesDaseqwChiNo ratings yet
- Classification of Fungi PDFDocument2 pagesClassification of Fungi PDFSajjad Hossain ShuvoNo ratings yet
- ICD 10 CodeDocument241 pagesICD 10 CodeZoe RinaNo ratings yet
- Traditional Home Remedies of GuyanaDocument15 pagesTraditional Home Remedies of GuyanaAaronJosiahNo ratings yet
- The Diagnosis and Management of Tinea CapitisDocument4 pagesThe Diagnosis and Management of Tinea CapitisKeyla Kehara PutriNo ratings yet
- Fungus Infections of the Skin and Nails: Causes, Symptoms and TreatmentsDocument5 pagesFungus Infections of the Skin and Nails: Causes, Symptoms and TreatmentsRoyNo ratings yet
- JamurDocument89 pagesJamurTriana AmaliaNo ratings yet
- DermatologyNotes OCRDocument164 pagesDermatologyNotes OCRPJ100% (1)
- اسكيمات لتشخيص و علاج بعض أمراض الجلديةDocument11 pagesاسكيمات لتشخيص و علاج بعض أمراض الجلديةsalamredNo ratings yet
- Summer Diseases and Its PreventionDocument6 pagesSummer Diseases and Its PreventionJithin M Krishna EzhuthachanNo ratings yet
- Dermatophyte Infections in CairoDocument5 pagesDermatophyte Infections in CaironevinNo ratings yet
- Fungal Skin InfectionsDocument31 pagesFungal Skin InfectionsCareyTranNo ratings yet
- ICD 10 - Chapter 1 Certain Infectious and Parasitic DiseasesDocument16 pagesICD 10 - Chapter 1 Certain Infectious and Parasitic DiseasesHuseikha VelayazulfahdNo ratings yet
- Introduction To MycologyDocument66 pagesIntroduction To MycologyHerlinaNababanNo ratings yet
- Mycopedis 2017Document110 pagesMycopedis 2017Ahmed RadwanNo ratings yet
- Fungal Infections Tinea Pedis and OnychomycosisDocument7 pagesFungal Infections Tinea Pedis and OnychomycosisAshraf AboNo ratings yet
- Assessing The IntegumentaryDocument73 pagesAssessing The IntegumentaryHelena Meurial HilkiahNo ratings yet
- KohDocument5 pagesKohNanny HerwantoNo ratings yet
- Tinea corporis causes and differential diagnoses under 40 charactersDocument4 pagesTinea corporis causes and differential diagnoses under 40 charactersHardiyanti HermanNo ratings yet
- Maintain Salon SafetyDocument83 pagesMaintain Salon SafetyRosMa WaEi100% (1)
- MycologyDocument9 pagesMycologyibti100% (1)