Professional Documents
Culture Documents
10 5923 J Surgery 20140301 03 PDF
Uploaded by
JacobMsangOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 5923 J Surgery 20140301 03 PDF
Uploaded by
JacobMsangCopyright:
Available Formats
International Journal of Surgical Research 2014, 3(1): 15-18
DOI: 10.5923/j.surgery.20140301.03
V-Y Advancement Flap for Reconstruction of Defects
after Excision of Basal Cell Carcinoma of the Face
Waleed Elnahas1,*, M. T. Hafez 1, Reda A. Younis2, Loai Elbassiony2, Mohamed A. Hegazy1
1
Surgical Oncology Unit, Mansoura Oncology Center, Mansoura University
2
Plastic Surgery Department, Mansoura University
Abstract Background: Basal cell carcinoma (BCC) is the most common skin cancer. After excision of BCC on the face,
the options of treatment for a skin defect are variable. Many surgeons prefer to use a local flap rather than a skin graft or free
flap for small- or moderately-sized circular defects. We have evaluated the versatility of V-Y perforator flap for
reconstruction of skin defects after excision of BCC of the face. Methods: All of the patients were pathologically diagnosed
with basal cell carcinoma (BCC), Thirty-seven patients underwent V-Y advancement flap repair over the period between
September 2011 and May 2013. We evaluated the postoperative complications in the form of flap loss either partial or
complete, wound dehiscence, hematoma, seroma and wound infection. The cosmetic outcome and patient satisfaction was
evaluated at 6 months after surgery. Results: There were 30 men and 7 women. The ages ranged from 51to 69 years with a
mean age of 60 years. The causes were BCC in all cases. The tumor locations were the face in all patients. All of the flaps
survived apart from only one case in which there was partial flap loss. Postoperative recovery was usually rapid. Conclusions:
The V-Y advancement flap is preferably used for small and medium size facial defects. Its advantages are less scarring and
superior aesthetic results as compared with other local flap methods.
Keywords Surgical flaps, BCC, Face reconstructive surgical procedures, V-Y flap
1. Introduction
Basal cell carcinoma (BCC) is the most common skin
cancer with significant local tissue invasion and morbidity.[1]
Since long time the conventional treatment option is surgical
excision with free safety margins. The narrower the free
surgical margin, the higher the recurrence rate.[2] Soft tissue
defects due to tumor excision are important medical and
cosmetic issues. Because of a rise not only in tumor
incidence, but also in patients expectations regarding their
quality of life after surgery, the need for functionally and
esthetically high-quality reconstruction is now greater than
ever.[3] Compared with skin grafts and free flaps, primary
closure and local flap are advantageous because less scar
tissue is formed following reconstruction, the use of similar
adjacent tissue provides cosmetic benefits, and they do not
have the risk of donor site morbidity.[4] V-Y advancement
flap is a flap in which the incision is shaped like a V and after
closure like a Y, partially or totally detached, to lengthen a
localized area of tissue to gain access to structures
underneath or to be used in repairing defects in an adjacent
part of the body. In this study we evaluate the use of v-y
* Corresponding author:
waleedelnahas@yahoo.com (Waleed Elnahas)
Published online at http://journal.sapub.org/surgery
Copyright 2014 Scientific & Academic Publishing. All Rights Reserved
advancement flap in covering defects after basal cell
carcinomas excision of the face.[5]
2. Patients and Methods
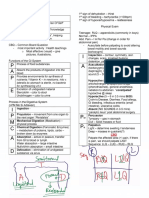
Figure 1. preoperative design and detection of preoperative perforators by
hand Doppler
Over the period between September 2011 and May 2013,
thirty-seven patients of basal cell carcinoma of the face were
included in this study at surgical oncology unit, Mansoura
oncology center and plastic department, Mansoura
University. There were 30 males and 7 females. Age of the
Waleed Elnahas et al.: V-Y Advancement Flap for Reconstruction of
Defects after Excision of Basal Cell Carcinoma of the Face
16
patients was ranged from 51 to 69. Patients with extensive co
morbidity were excluded from this study. Sites of basal cell
carcinoma in the face were summarized in table 1.
Preoperative design and detection of the perforators within
the flap by hand Doppler was performed. (Fig. 1).
Table (1). Demographic data
Tumor diameter
Age
Sex
Tumor Sites
From 12 mm to 44 mm, mean 28 mm
From 51 to 69 years , mean 60 Years
Male: 30 Cases
Female: 7 Cases
Forehead: 11 cases
Cheek: 16 cases
Side of nose: 10 cases
The flap was designed so it was at least twice the length of
the width of the flap. Wide local excision with three
dimensional safety margins was carried out and was guided
by intraoperative frozen section in all patients prior starting
the reconstructive procedure. Any infiltrated margin was
dealt immediately by re-excision. A triangular incision is
made from the edges of the wound and carried down to
subcutaneous fat. Undermining is carried out laterally. Some
undermining of the leading edge may be necessary to
enhance flap mobility and to avoid tethering of the base of
the flap or significant wound tension. Undermining
performed away from the perforators detected preoperatively.
Once mobilized, the flap is brought into position using a skin
hook and an absorbable key suture is placed in the middle of
the leading edge of the advancing triangular flap, followed
by additional absorbable sutures at the corners of the leading
edge. The incisions are then closed in 2 layers, in a Y shaped.
And a compression dressing is applied to prevent hematoma
formation beneath the flap. We evaluated the postoperative
complications in the form of flap loss either partial or
complete, wound dehiscence, hematoma, seroma and wound
infection.All patients were evaluated 6 months after surgery
for cosmetic outcome and classified according to patient
judgment as excellent, good, fair and poor. (Fig 2 and fig 3.)
3. Results
The tumor diameters varied from 12 to 44 mm (mean, 28
mm). All patients were treated under general anesthesia. We
did not apply any algorithm to select a unilateral or bilateral
V-Y advancement flap, and thus, the choice was made after
considering the defect location, skin condition, and expected
scarring. Complete flap survival was achieved in 36 cases
(97%). There was a case of partial flap necrosis of the
forehead and healed by secondary intention. There was
wound dehiscence encountered in two cases due to wound
infection, which were managed by antibiotics, frequent
dressings then secondary sutures. There was no hematoma,
or seroma occurred. (Table 2) Bilateral flaps were used in 5
cases of the forehead while in the other 32 cases unilateral
flap was used. All of the patients had excellent skin coverage.
No recurrence at the primary tumor site was detected during
the follow-up period, which ranged from 6 months to 26
months. Aesthetic results were deemed excellent in 20
patients (55%), while 13 patients shows good results (35%)
and 4 patients were fair result (10%). The color and texture
matches were aesthetically good and the contour was distinct
in all patients.
Figure 2. preoperative marking, early post operative results and results after 6 month a case of basal cell carcinoma of the forehead
International Journal of Surgical Research 2014, 3(1): 15-18
17
Figure 3. preoperative, early postoperative and 6 month after surgery of a case of basal cell carcinoma of the side of the nose
Table (2). Postoperative complications
Post operative complications
Partial flap loss
Complete flap loss
wound dehiscence
Sex
Percentage
3%
0%
5%
hematoma
0%
Seroma
0%
Wound infection
5%
4. Discussion
In this study, all cases were basal cell carcinoma of the
face planned for excision with three dimensional safety
margins and reconstruction.
Appropriate margins for malignant tumors depend on the
cancer type, tumor size, tumor irregularity, and time elapsed
from onset. In cases of basal cell carcinoma, an appropriate
excision margin would be 2 to 5 mm from the tumor,
whereas in cases with a small-sized lesion of <2 cm in
diameter, it would be approximately 4 mm. On the other
hand, in cases with a lesion of >2 cm in diameter or with a
substantial delay after onset, the margin would be 1 cm, and
in recurrent cases, it would be >1 cm. (1, 2). In our study, we
used mean safety margins of 3 mm, and all margins were
proved to be free by intraoperative frozen section.
A number of different techniques have been described for
reconstruction of the face defects after excision of malignant
tumors. To date, there are no clear criteria for the selection of
one or the other technique.[6]
Four methods are used to reconstruct soft tissue defects
after the surgical excision of skin tumors: primary closure,
skin graft, local and free flaps. The most important factors to
be considered for reconstruction are defect location and
shape.[7]
Primary closure is the most commonly used method to
treat soft tissue defects. In the reconstruction of primary
closure for circular defects, a dog-ear had been considered
the standard approach. To avoid dog-ears, an elliptical
excision would be needed that would include adjacent
normal tissue. As a result, it would create a longer scar than
the defect. Therefore, primary closure may not be
appropriate for use in the facial region from a cosmetic
perspective.[8]
Skin grafting is usually performed when defects are large
and unsuitable for primary closure or a local flap. However,
skin grafts are less desirable due to the color differences
between the donor and recipient sites and scarring. Therefore,
in patients with small-to-medium defects, a local flap rather
than a skin graft is preferred.[9]
Various local flap methods can be used, the application of
which are dependent on skin tissue status and skin defect
location.[4] In practice, the optimal method for a local flap
depends initially on the surgeon's preference. Rotational
flaps are used frequently, but although the procedure is
straightforward, it has the disadvantages of leaving large
elliptical scars, requiring the resection of a large amount of
normal skin tissue, and causing anatomical deformities of the
adjacent structures. In particular, in younger patients,
rotational flaps exert excessive tension on the face, where
there is no redundant skin, and leave obvious scars.
Advancement flaps are used when the patient is in overall
good health and the defect is free of tumor and obvious
infection. Flaps should match thickness, color, and texture of
excised skin. Resultant scars should fall in relaxed
skin-tension lines.
We used V-Y advancement flaps with a unilateral or
bilateral pedicle to reconstruct soft tissue defects after the
surgical excision of skin tumors of the face. This method
involves the transfer of a V-shaped flap to the defect site and
converting it to a Y-shaped flap using a random pattern flap
involving dermal plexus and subdermal plexus, which are
Waleed Elnahas et al.: V-Y Advancement Flap for Reconstruction of
Defects after Excision of Basal Cell Carcinoma of the Face
18
connected by a subcutaneous perforating artery arising from
the muscle.[10] We identified the subcutaneous perforator
by hand Doppler preoperative in all cases to ensure adequate
blood supply. Many authors including Dufourmentel and
Talaat have previously described the subcutaneous pedicled
V-Y flap,[11] who have coined the term "kite flap", which
also refers to cases in which the skin island overlies the
orbicularis oculi muscle for defects of the medial canthus
and lower lid. The flap is optimally designed so that the
common limb of the Y falls into the boundary with
neighboring aesthetic regions or within a natural crease, fold,
or wrinkle.
The advantages of the V-Y advancement flap are the
preservation of sensation and length, and good soft tissue
coverage. Tension, however, is the primary problem
encountered with this flap, especially with larger defects.
The point of maximum tension occurs where the gap of the
defect is greatest, which is in the mid portion of the defect.
The need for a tension-free closure is highlighted in a variety
of sources. If a tension-free closure is not achieved, the flap
is at risk for necrosis.[12]
The V-Y advancement flap is particularly useful when a
structure or region requires lengthening or release from a
contracted state. When a skin tumor is present on the margin
of an aesthetic unit, excellent cosmetic outcomes can be
obtained using a V-Y advancement flap. In elderly patients,
by identifying redundant skin areas, we have transferred
bilateral flaps after adjustment for size. Thus, by using V-Y
advancement flaps we have achieved excellent cosmetic
outcomes in the facial region.[3]
Scar widening is related to ongoing tension. According to
geometric analysis, compared with a pivot flap that includes
a rotational flap and transpositional flap, the V-Y
advancement flap provides much less tension, which reduces
the risk of hypertrophic changes and scar widening in the
long term.[13]
Furthermore, because a V-Y flap also creates a smaller
dead space, it presents lower risks of postoperative
complications such as seroma and hematoma.
Another disadvantage is scar revision for stigmata of a
V-Y advancement flap. Although abnormal scar formation,
such as a hypertrophic scar or widening scar, occurs less
often with V-Y flaps than with the other flap methods, the
stigmata is not linear; it is of a rhomboidal shape. Therefore,
it is very difficult to correct the scar by making it
invisible.[3]
Although there are various methods for reconstructing
skin defects created by skin tumor resection, we believe that
the V-Y advancement flap produces good treatment
outcomes in cases with small-to-medium defects.
5. Conclusions
The V-Y advancement flap is preferably used for small
and medium size facial defects. Its advantages are less
scarring and superior aesthetic results as compared with
other local flap methods.
REFERENCES
[1]
Rhodes LE, de Rie M, Enstrom Y, Groves R, Morken T,
Goulden V, et al. Photodynamic therapy using topical methyl
aminolevulinate vs surgery for nodular basal cell carcinoma:
results of a multicenter randomized prospective trial.
Archives of dermatology. 2004;140(1):17-23. Epub
2004/01/21.
[2]
Katz KH, Desciak EB, Maloney ME. The optimal application
of surgical adhesive tape strips. Dermatologic surgery:
official publication for American Society for Dermatologic
Surgery[et al]. 1999;25(9):686-8. Epub 1999/09/22.
[3]
Strauch B, Fox M. VY bipedicle flap for resurfacing the nasal
supratip region. Plastic and reconstructive surgery.
1989;83(5):899-903. Epub 1989/05/01.
[4]
Kwon KH, Lee DG, Koo SH, Jo MS, Shin H, Seul JH.
Usefulness of v-y advancement flap for defects after skin
tumor
excision.
Archives
of
plastic
surgery.
2012;39(6):619-25. Epub 2012/12/13.
[5]
Valdatta L, Mortarino C, Thione A, Buoro M. Modified
deepithelialized bilateral triangular VY flaps for the
correction of posttracheostomy scar. Plastic and
reconstructive surgery. 2005;115(1):351-3; author reply 3.
Epub 2004/12/29.
[6]
Mosterd K, Krekels GA, Nieman FH, Ostertag JU, Essers BA,
Dirksen CD, et al. Surgical excision versus Mohs'
micrographic surgery for primary and recurrent basal-cell
carcinoma of the face: a prospective randomised controlled
trial with 5-years' follow-up. The lancet oncology.
2008;9(12):1149-56. Epub 2008/11/18.
[7]
Chiummariello S, Del Torto G, Iera M, Alfano C. The use of
local flaps in the one-step nose reconstruction after cancer
resection. Annali italiani di chirurgia. 2013;84. Epub
2013/07/10.
[8]
Schubert J.[Local flaps for the closure of facial defects]. Hno.
2013;61(5):433-46. Epub 2013/05/08. Defektdeckung mittels
Nahlappenplastiken im Gesicht.
[9]
Pepper JP, Baker SR. Local flaps: cheek and lip
reconstruction. JAMA facial plastic surgery. 2013; 15(5):
374-82. Epub 2013/09/21.
[10] RC R. Fingertip injuries. In: McCarthy JG, editor. Plastic
Surgery. Philadelphia: Saunders; 1990. p. 447798.
[11] Dufourmentel C TS. The kite flap. In: JT H, editor.
Transactions of the Fifth International Congress of Plastic and
Reconstructive Surgery; Melbourne1971. p. 11234.
[12] RA W. Treatment options for distal tip amputations. In:
Strickland JW GT, editor. The Hand. second ed. Philadelphia:
Lippincott Williams and Wilkins; 2005. p. 32338.
[13] Onishi K, Maruyama Y, Hayashi A, Inami K. Repair of scalp
defect using a superficial temporal fascia pedicle VY
advancement scalp flap. British journal of plastic surgery.
2005;58(5):676-80. Epub 2005/06/01.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Catatan Harian Seorang Mahasiswa KedokteranDocument14 pagesCatatan Harian Seorang Mahasiswa KedokteranJacobMsangNo ratings yet
- Contoh Pidato Bahasa Inggris Tentang Perpisahan Sekolah Dan ArtinyaDocument3 pagesContoh Pidato Bahasa Inggris Tentang Perpisahan Sekolah Dan ArtinyaJacobMsangNo ratings yet
- The 4 Main Phases of Wound HealingDocument2 pagesThe 4 Main Phases of Wound HealingJacobMsangNo ratings yet
- Clinical Anatomy of The Vulva, Vagina, Lower Pelvis, and PerineumDocument20 pagesClinical Anatomy of The Vulva, Vagina, Lower Pelvis, and PerineumJacobMsangNo ratings yet
- Scar RemovalDocument3 pagesScar RemovalJacobMsangNo ratings yet
- When Organs Fail One by OneDocument6 pagesWhen Organs Fail One by OneJacobMsangNo ratings yet
- Anatomical Steps of ThyroidectomyDocument7 pagesAnatomical Steps of ThyroidectomyJacobMsangNo ratings yet
- Craniotomy VS CraniectoyDocument1 pageCraniotomy VS CraniectoyJacobMsangNo ratings yet
- Nonunion of The Fractured ClavicleDocument18 pagesNonunion of The Fractured ClavicleJacobMsangNo ratings yet
- Video PemeriksaanDocument8 pagesVideo PemeriksaanJacobMsangNo ratings yet
- Wrist Ganglion: Definition and PathologyDocument8 pagesWrist Ganglion: Definition and PathologyJacobMsangNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Phrasal Verb PracticeDocument2 pagesPhrasal Verb PracticeganaNo ratings yet
- Part III Internal Medicine Examination AnswersDocument91 pagesPart III Internal Medicine Examination AnswersFırat GüllüNo ratings yet
- My Hands The Body Is Painful / Do ROM Actions Done With MyDocument3 pagesMy Hands The Body Is Painful / Do ROM Actions Done With MyHanip Little-FaqotNo ratings yet
- 8 Heirs of Spouses Remedios R. Sandejas and Eliodoro P. Sandejas vs. LinaDocument9 pages8 Heirs of Spouses Remedios R. Sandejas and Eliodoro P. Sandejas vs. LinaBerNo ratings yet
- 2018 Chapter 3-1 2018 Introduction To Industrial Higiene & Occupational Health PDFDocument59 pages2018 Chapter 3-1 2018 Introduction To Industrial Higiene & Occupational Health PDFLove StrikeNo ratings yet
- Headache and Joint PainDocument13 pagesHeadache and Joint PainJosiah Noella BrizNo ratings yet
- How To Achieve SuperhealthDocument24 pagesHow To Achieve SuperhealthJulian Williams©™No ratings yet
- Nursing Skills (Vital Signs) PDFDocument48 pagesNursing Skills (Vital Signs) PDFkhizer hayatNo ratings yet
- Value of Home Care SECUREDDocument25 pagesValue of Home Care SECUREDRichard HutasoitNo ratings yet
- LCB Surgical Technique - 2022 Update v3Document24 pagesLCB Surgical Technique - 2022 Update v3Samuel SalvadorNo ratings yet
- 1 66th WHA Provisional AgendaDocument6 pages1 66th WHA Provisional AgendaRenzo R. GuintoNo ratings yet
- Ulcerative ColitisDocument30 pagesUlcerative ColitisAndika SulistianNo ratings yet
- OMG 6 Sains TG 5 - Bab 01Document15 pagesOMG 6 Sains TG 5 - Bab 01Azizah EmbongNo ratings yet
- Acute Purulent Diseases of Fingers and HandDocument23 pagesAcute Purulent Diseases of Fingers and Handluckyswiss7776848No ratings yet
- Crick PrsentationDocument28 pagesCrick Prsentationalka mehraNo ratings yet
- IM-Module B Summarized Notes (IBD)Document69 pagesIM-Module B Summarized Notes (IBD)DeepbluexNo ratings yet
- Hea LLG: 18 Sign of Dehydration - ThirstDocument22 pagesHea LLG: 18 Sign of Dehydration - ThirstMhae TabasaNo ratings yet
- Metabolic Encephalopathies in The Critical Care Unit: Review ArticleDocument29 pagesMetabolic Encephalopathies in The Critical Care Unit: Review ArticleFernando Dueñas MoralesNo ratings yet
- A To Z Orthodontics - Vol 9 - Preventive and Interceptive OrthodonticsDocument37 pagesA To Z Orthodontics - Vol 9 - Preventive and Interceptive OrthodonticsĐạt HuỳnhNo ratings yet
- Autoimmune Abnormalities of Postpartum Thyroid DiseasesDocument8 pagesAutoimmune Abnormalities of Postpartum Thyroid DiseasesIpan MahendriyansaNo ratings yet
- PNLE Prep.Document23 pagesPNLE Prep.Darnell Adrian EstobioNo ratings yet
- Health and H BehaviorDocument69 pagesHealth and H BehaviorDawud AsnakewNo ratings yet
- Fundamentals of Nursing10-19Document19 pagesFundamentals of Nursing10-19escolarNo ratings yet
- 0226.OPWDD Letter From MembersDocument2 pages0226.OPWDD Letter From MembersZacharyEJWilliamsNo ratings yet
- Language and The BrainDocument8 pagesLanguage and The BrainAntonio GoqueNo ratings yet
- Revision 1 English Open LetterDocument9 pagesRevision 1 English Open Letterapi-441660843No ratings yet
- MNT-Dislipidemia-Unja 20022019 PDFDocument48 pagesMNT-Dislipidemia-Unja 20022019 PDFAnonymous o3Q3QXENo ratings yet
- Importance of Espresso Coffee Machine ParametersDocument10 pagesImportance of Espresso Coffee Machine ParametersOssian89No ratings yet
- Evidence-Based Decision Making in Dentistry - Multidisciplinary Management of The Natural DentitionDocument143 pagesEvidence-Based Decision Making in Dentistry - Multidisciplinary Management of The Natural DentitiontayabakhanNo ratings yet
- 756 1754 1 PBDocument2 pages756 1754 1 PBmiayt2006No ratings yet